PMY3304- PSYCHOSIS, SCHIZOPHRENIA AND BIPOLAR DISORDER
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
54 Terms
What is schizophrenia?
Most common psychotic disorder, often develops in young adulthood (tends to emerge earlier in males than females), increased risk of premature mortality, a lot of misinformation and negative attitudes
What are the positive symptoms of schizophrenia?
Hallucinations, delusions, disorganised speech, thought disorder, catatonic behaviour (more info about symptoms in slide notes)
What are the negative symptoms of schizophrenia?
Emotional blunting, reduced speech, loss of motivation, self-neglect, social withdrawal
What is catatonic behaviour?
Psychomotor activity that is grossly exaggerated or retarded (slowed down)
What symptoms are seen more, positive or negative?
Negative symptoms are seen more prominently when the positive symptoms are treated
What are the main areas affected by schizophrenia?
Cognitive symptoms, affective symptoms, loss of insight
We will often see cognitive defects, attention, decision making, planning or sequencing, problem solving issues (all higher executive functions)
What is the loss of insight associated with schizophrenia?
Inability to recognise/understand that they are suffering from a condition
What are some other psychotic disorders?
Schizoaffective disorder (symptoms of schizophrenia and a mood disorder- depressed or maniac- are equally prominent, drug induced psychosis- substance induced and usually remits within a month of cessation of use, persistent delusional disorder- most pervasive symptom is delusion
Is there a genetic risk for schizophrenia?
7.5 fold increased risk of psychotic disorders if patient has schizophrenia
What are the social and environmental risk factors of schizophrenia?
- Stressful life events, including childhood adversity
- Family heritage (increased risk is south Asian and black populations)
- Migration (especially from developing country)
- Urban living
- Cannabis and other substance use- amphetamines, ketamine
- Medication use- high dose CCS
- Early life factors
- Exposure to toxoplasma gondii- parasite
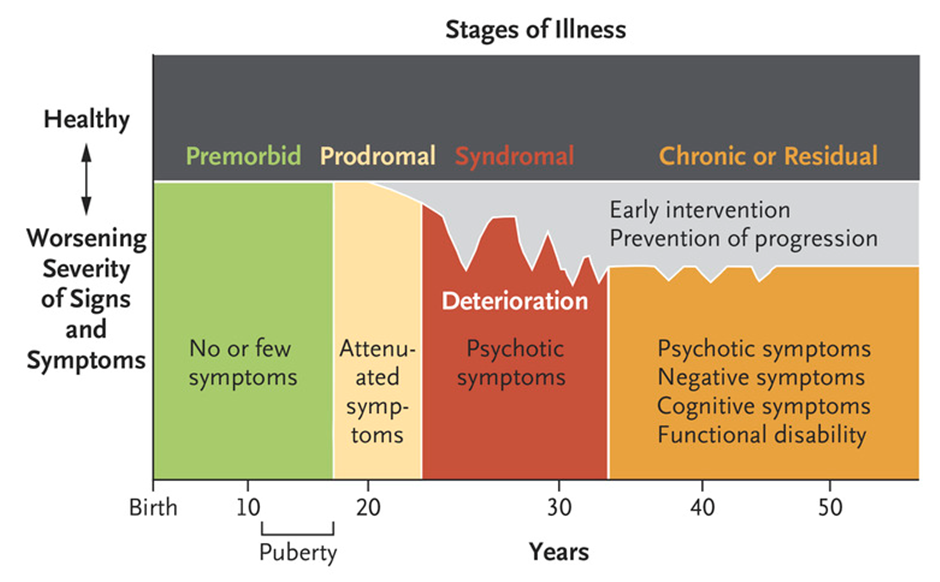
What is the course and prognosis of psychosis?
what are the complications with schizophrenia?
- Premature death, increased risk of suicide, increased risk of certain physical disorders e.g. CV disease, T2D, smoking related illnesses, cancer, infections
- Social exclusion- impairs the person’s ability to learn, work and maintain relationships
- Substance misuse- up to one third of people with schizophrenia misuse drugs- huge risk to persons physical health e.g. blood borne viruses and hepatitis
How is schizophrenia managed?
- Assess risk of self harm to self and/or others
- Refer for specialist assessment- secondary care team maintain responsibility for at least first 12 months
- Treat co-existing anxiety disorders, depression, emerging personality disorders, or substance misuse
- Therapeutic trial of oral antipsychotic- family intervention for relatives who live/ in close contact with patient, individual CBT, art therapies may be offered, particularly to help with negative symptoms
What are the different kinds of antipsychotics?
Typical antipsychotics (first generation) and contemporary atypical antipsychotics (have many different actions and targets- second generation). First gen usually inhibit dopaminergic neurotransition, second gen usually have serotonin receptor action
Give some examples of 1st generation antipsychotics
- Benperidol
- Chlorpromazine
- Flupentixol
- Haloperidol
- Levomepromazine
- Periciazine
- Perphenazine
- Pimozide
- Sulpiride
- Trifluoperazine
- Zuclopenthixol
Give some examples of second generation antipychotics
- Amisulpride
- Aripriprazole
- Clozapine
- Clozapine
- Olanzapine
- Paliperidone
- Quetiapine
- Risperidone
What are the antipsychotic depot injections that can be given and when would they be given?
They are used for maintenance therapy when adherence to oral treatment is unreliable, they are administered every 1-4 weeks
- Aripriprazole
- Flupentixol decanoate
- Fluphenazine decanoate
- Haloperidol
- Olanzapine embonate
- Paliperidone
- Pipotiazine palmitate
- Risperidone
- Zuclopenthixol decanoate
What is the first line antipsychotic for schizophrenia?
There is no first line, need to consider the patient, any co-morbidities, other medications, and what side effects the patient would be more prepared to put up with
How is clozapine initiated?
Won’t be initiated in primary care- is a second generation anti-psychotic, response can be quite variable- dosing and dosing interval will need to be adjusted according to response
What are extrapyramidal symptoms?
Drug induced movement disorders that are caused as side effect of anti-psychotic medication
Acute dystoria- tongue protrusion, torticollis (occurs within hours to days of beginning treatment)
Pseudoparkinsonism- shuffling gait, tremor, cogwheel rigidity (days to weeks after beginning treatment) akathisia e.g. compelling urge to tap one’s feet (days to weeks after starting treatment)
Tardive dyskinesia- grimacing, excessive blinking, lip smacking (months to years of treatment)
Extra-pyramidal symptoms are dose related and more likely to occur with first generation agents
What can sometimes help with extrapyramidal symptoms?
Antimuscarinics can be helpful, they wouldn’t be prescribed prophylactically only if symptoms occur
What are some other adverse effects of antipsychotics?
Weight gain
- More frequent with second gen drugs like clozapine and olanzapine
Hyperprolactinaemia
- Sexual dysfunction, reduced bone mineral density, menstrual disturbances, breast enlargement, galactorrhoea
- Dopamine inhibits prolactin release
- First generation agents are more likely to cause hyperprolactinaemia
Sexual dysfunction
- Risperidone, haloperidol, olanzapine
Cardiovascular
- Tachycardia, arrhythmias, hypotension
- QT-interval prolongation with pimozide
Hyperglycaemia and diabetes
- Diabetes risk increased in all patients with schizophrenia who take antipsychotics
Neuroleptic malignant syndrome
- Rare but potentially fatal
- Discontinuation essential for at least 5 days, preferably longer
Where is clozapine managed?
- Managed exclusively in secondary care- patient, prescriber, supplying pharmacist must be registered with patient monitoring service- takes several days to do this
What are potential side effects with clozapine?
- Neutropenia and potentially fatal agranulocytosis, requires frequent monitoring of FBC
- Fatal myocarditis and cardiomyopathy reported
- Intestinal peristalsis- causes constipation, intestinal obstruction, faecal impaction, paralytic ileus, seek immediate medical advice before taking next dose if constipation develops
When can clozapine be diagnosed?
- Two different anti-psychotics must be trialed, 1st and 2nd gen before clozapine can be prescribed
What is bipolar disorder?
- Characterised by episodic depressed and elated moods and increased activity (hypomania or mania)
What is a manic episode?
- Abnormally and persistently elevated, expansive, or irritable mood lasting at least 1 week. Includes psychotic features such as delusions or hallucinations
What is a hypomanic episode?
Not severe enough to cause marked impairment in social or occupational functioning or necessitate hospitalisation. No psychotic features
What is a depressive episode?
Period of at least 2 weeks, depressed mood or loss of interest or pleasure in nearly all activities
What is the difference between bipolar 1 vs bipolar 2 disorder?
- Bipolar 1 has at least one episode of extreme mania lasting more than a week, depression tends to be milder than other types, some experience no depression, increased energy, talking extremely quickly, euphoria
- Bipolar 2 has symptoms of hypomania (a milder form of mania) lasting at least 4 days, at leasat one depressive episode broken up by periods of hypomania, feelings of hopelessness, fatigue, irritable and anxious
What is the epidemiology of psychiatric disorders?
- Prevalence rates similar in males and females
- Common in younger age groups
- One of the most heritable psychiatric disorders
- Environmental triggers- early life stresss, maternal death before child reaches 5, childhood trauma/abuse, emotional neglect/abuse, cannabis use, cocaine exposure
What is the prognosis of bipolar disorder?
- Relapse is common, especially when treatment adherence is poor (average of 10 episodes in lifetime, and recovery may or may not be complete during episodes)
- Progressive deficits in cognition and functioning
- Associated with other psychological and physical illnesses like anxiety disorder, alcohol and substance misuse, ADHD, CV disease, hypertension, T2D, dyslipidaemia, metabolic syndrome, obesity
- Higher mortality among people with bipolar disorder
How is mania associated with bipolar disorder managed?
- Trial of oral antipsychotic (haloperidol, olanzapine, quetiapine, or risperidone)
- If first antipsychotic is not tolerated/ineffective, second antipsychotic offered.
- If second line antipsychotic is ineffective, lithium or sodium valproate may be added.
- Antidepressant medication is usually tapered and discontinued
How is depression associated with bipolar disorder managed?
- Quetiapine alone, or
- Fluoxetine combined with olanzapine, or
- Olanzapine alone, or
- Lamotrigine alone
How is relapse prevented with bipolar disorder?
- Continue current treatment for mania, or
- Start long term treatment with lithium, or
- If lithium is not effective, valproate may be added to lithium treatment
- If lithium is poorly tolerated, valproate alone or olanzapine alone may be considered
Psychological therapies can also be offered
Secondary care usually monitor person for at least first 12 months or until condition stabilised
What can occur with higher doses of olanzapine?
Photosensitisation- avoid sunlight- can be a problem with a lot of anti-psychotics, check when counselling
Why is caution needed with IM use of olanzapine?
- Acute myocardial infarction, bradycardia, recent heart surgery, severe hypotension, sick sinus syndrome, unstable angina
What extra monitoring is required with olanzapine?
- More frequent monitoring of blood lipids and weight, every 3 months for the first year and then yearly
what should be done if the person taking olanzapine is taking other antimanic drugs?
Reduce olanzapine dose gradually over at least 4 weeks
How long does it take for the full prophylactic effect of lithium to take effect?
May take 6-12 months
Why should lithium be prescribed by brand name?
There are differences in bioavailability, as there are two salts – lithium carbonate and lithium citrate which are not dose equivalent
What is the aim plasma level of lithium?
Aim to achieve a plasma level of 0.6-1.0mmol/L, to achieve this therapeutic drug monitoring is required- lithium has a narrow therapeutic window/index
What are the potential side effects with lithium?
Signs of intoxication = withdrawal of treatment
GI disturbances, visual disturbances, polyuria, muscle weakness, fine tremor increasing to coarse tremor, CNS disturbances, abnormal reflexes, myoclonus, incontinence, hypernatraemia
Why should abrupt discontinuation of lithium be avoided?
Increases risk of relapse, decrease dose gradually over 4 week period (preferably 3 months)
What are the interactions with lithium?
Interacts with diuretics, NSAIDs, carbamazepine
What is the risk with long term use of lithium?
Thyroid disorders and mild cognitive and memory impairment
What patient/carer counselling should be carried out with lithium?
- Report signs and symptoms of lithium toxicity, hypothyroidism, renal dysfunction, and benign intracranial hypertension
- Maintain adequate fluid intake and avoid dietary changes which alter Na intake
What two forms are valproate available as?
Semisodium valproate (Depakote)- licensed for treatment of acute mania
Sodium valproate (epilim) and valproic acid (convulex)- both unlicensed for treatment of bipolar disorder
Can valproate be used in pregnancy?
No, there is a high teratogenic risk, must not be used during pregnancy in patients with bipolar disorder
Are there many interactions with valproate?
Highly protein bound (94%), interactions!
What should the patient be advised with valproate?
- Advise patient/carer how to recognise signs/symptoms of blood disorders, liver disorders and pancreatitis
- Seek immediate medical help if these develop
When should lamotrigine be prescribed with caution?
- Prescribe with caution if myoclonic seizures or Parkinson’s disease
What is a risk with lamotrigine use?
Skin rash, prompt evaluation needed and lamotrigine withdrawn immediately
Small risk of suicidal thoughts and behaviour, alert to mood changes, distressing thoughts, or feelings about suicide or harming themselves at any point during treatment
What are the key interactions with lamotrigine?
CNS depressants, carbamazepine, phenytoin, primidone, oestrogens, progestogens, desmopressin, ritonavir, valproate