PT 714 MDT & Mobilization with Movement Lecture 2025 [Autosaved]
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
What is Mechanical Diagnosis & Therapy (MDT)
Examination and intervention classification-based approach
Utilizes repeated movements in addition to single movements
Rapidly identifies fast/slow/non-responders
Focuses on the patient and their potential to self-manage and recover their previous level of function
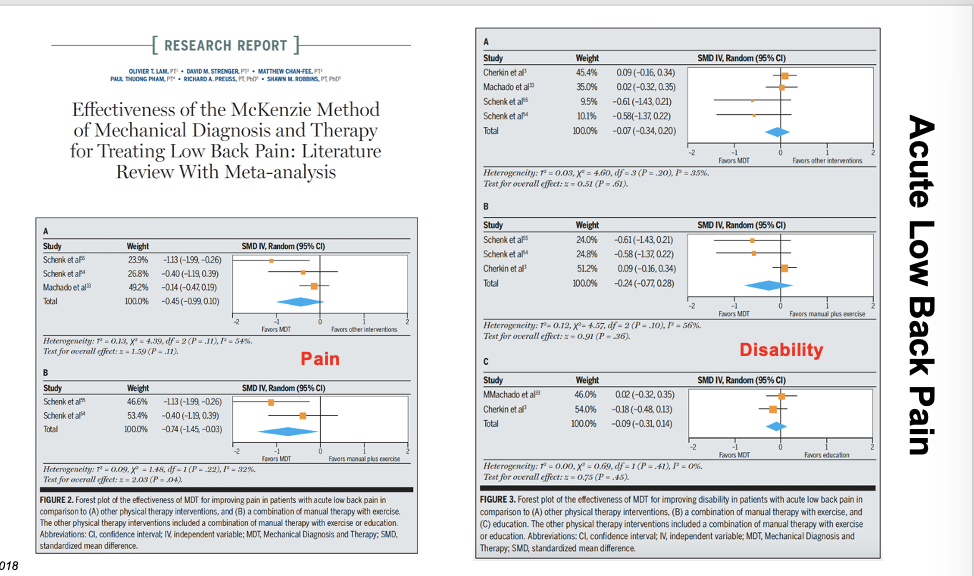
effectiveness of Mckezie method on acute low back pain
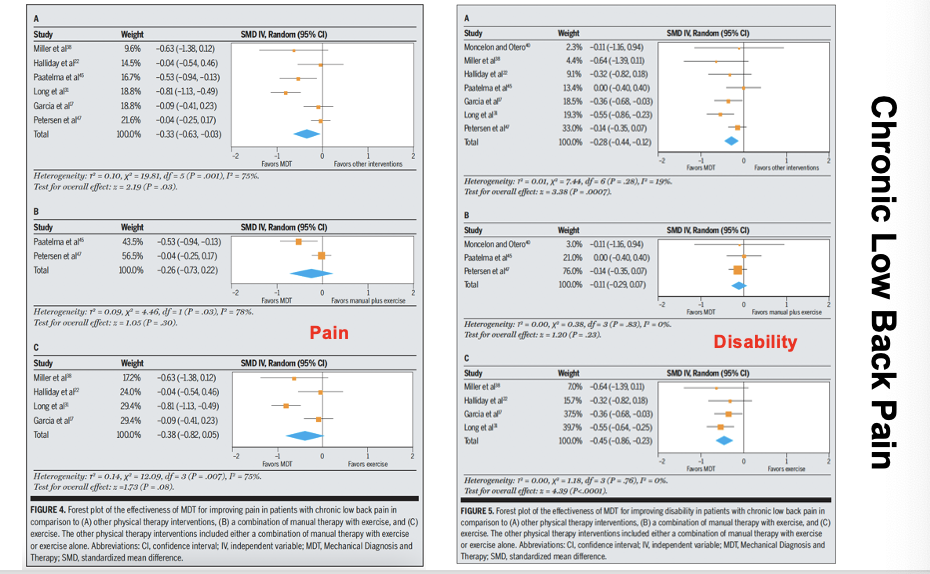
effectiveness of Mckezie method on chronic low back pain
Examination: repeated movement testing
In addition to standard orthopedic exam
Response to repeated end-range movements
NOT a ROM test
Proceed from loaded to unloaded position
Drives classification
Directional preference
Centralization
Directional Preference vs Centralization
Directional preference
One direction makes symptoms “better”
One direction makes symptoms “worse”
Usually the opposite direction
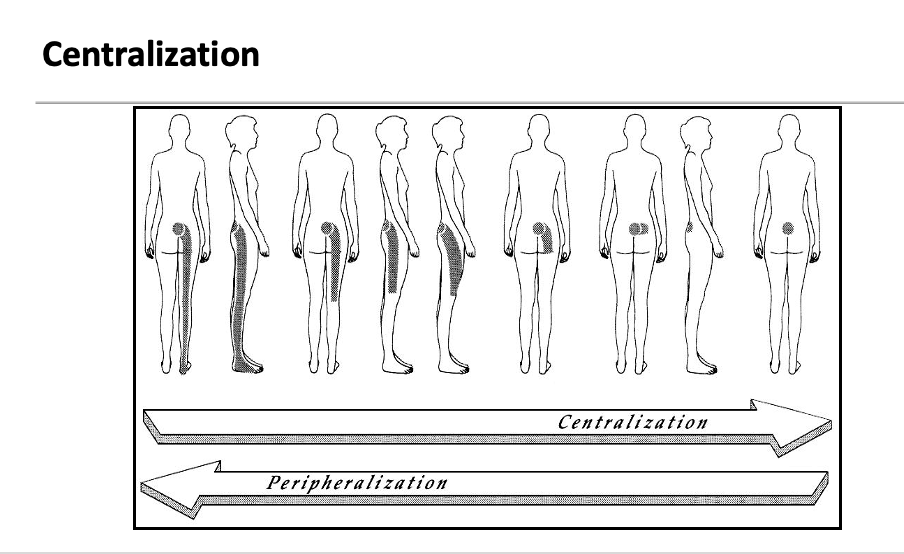
Centralization
A subset of directional preference
Unique definition
Might have a directional preference without centralization/peripheralization
Definition of centralization
with repeated motion or sustained positions, pain moves from distal to proximal and remains there
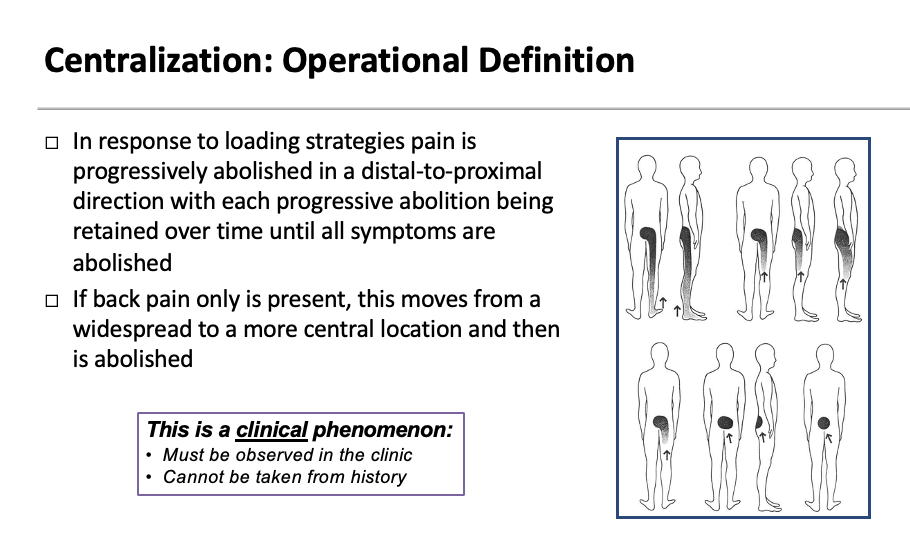
Centralization: Operational Definition
In response to loading strategies pain is progressively abolished in a distal-to-proximal direction with each progressive abolition being retained over time until all symptoms are abolished
If back pain only is present, this moves from a widespread to a more central location and then is abolished
This is a clinical phenomenon:
Must be observed in the clinic
Cannot be taken from history
_______
You have to see it – not just take their word
It also must stay in that area – if it reverts back immediately its not centralizing – should only go back with different motion like flexion
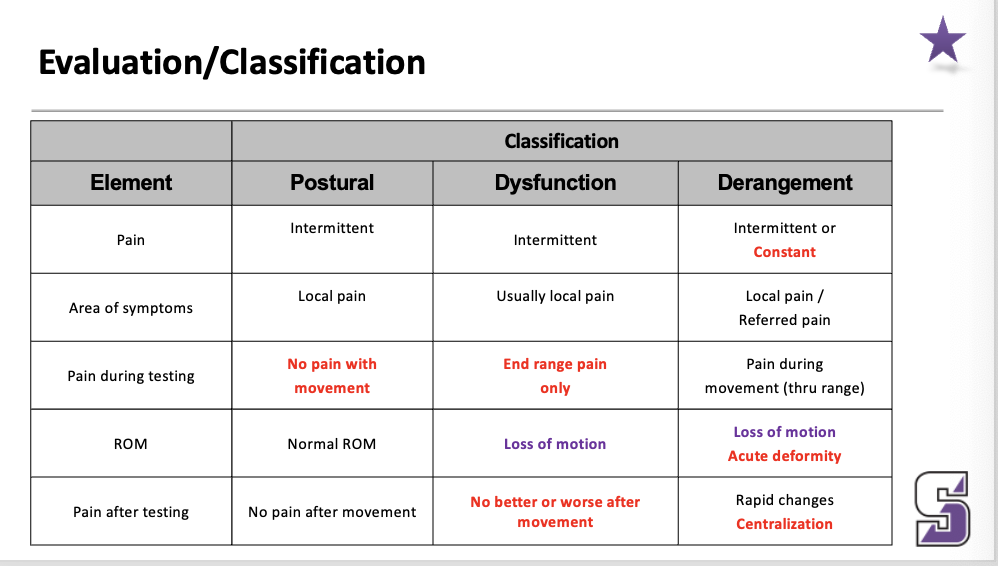
Evaluation/Classification (postural vs dysfunction vs derangement)
____
Postural- named for aggravating static or sustain posture Dysfunction- direction of restriction and pain provacation is the same, if you can’t flex and flexion causes you pain…then you are a flexion dysfunction
Derangement- based on conceptual model of disc; named for the direction in which the NP is shifted in the disk.
Pproblems with a disc typically come from repeated ans sustained flexion – so you do repeated extension to get the fluid back into the disc since it’s a jelly doughnut
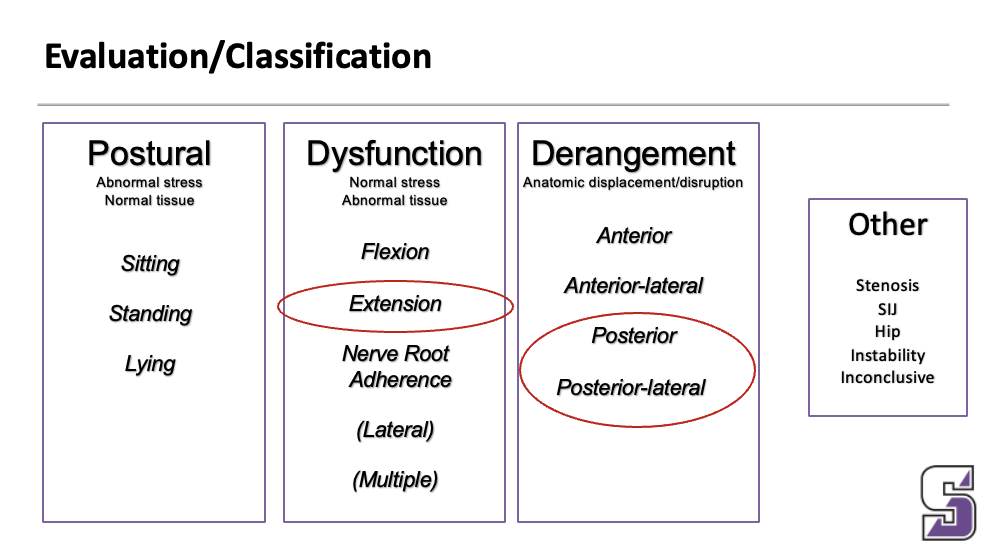
Evaluation/Classification
Ignore the postural one
Derangement: pain all the way through the movement – lateral shift as example
Derangement changes quickly, dysfunction does not
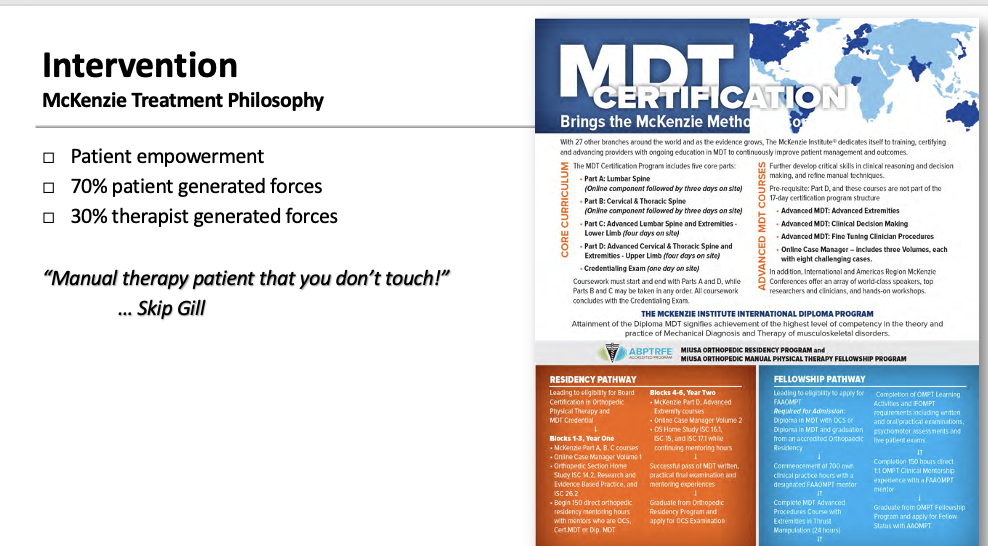
Intervention: McKenzie Treatment Philosophy
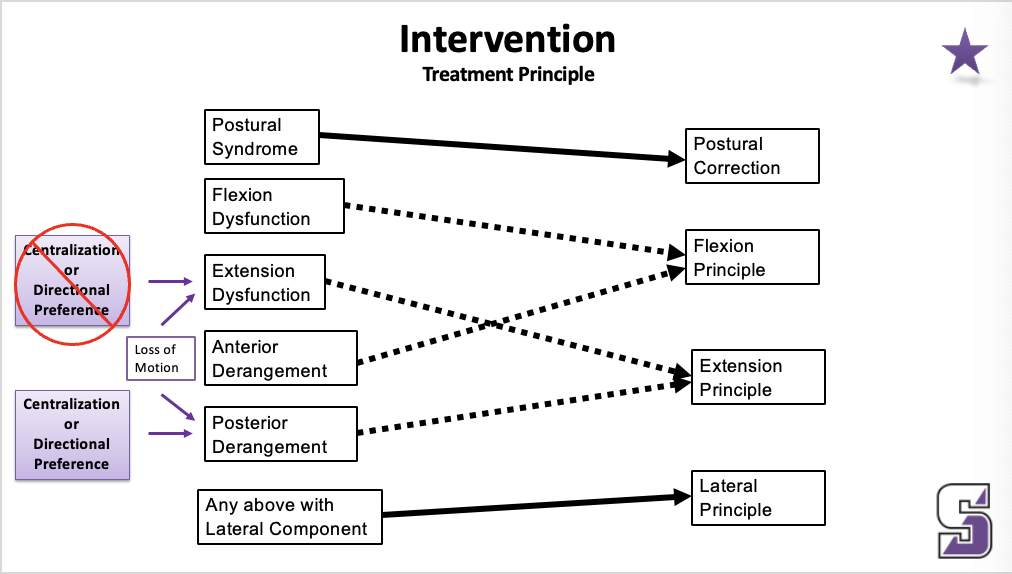
Intervention: treatment principle
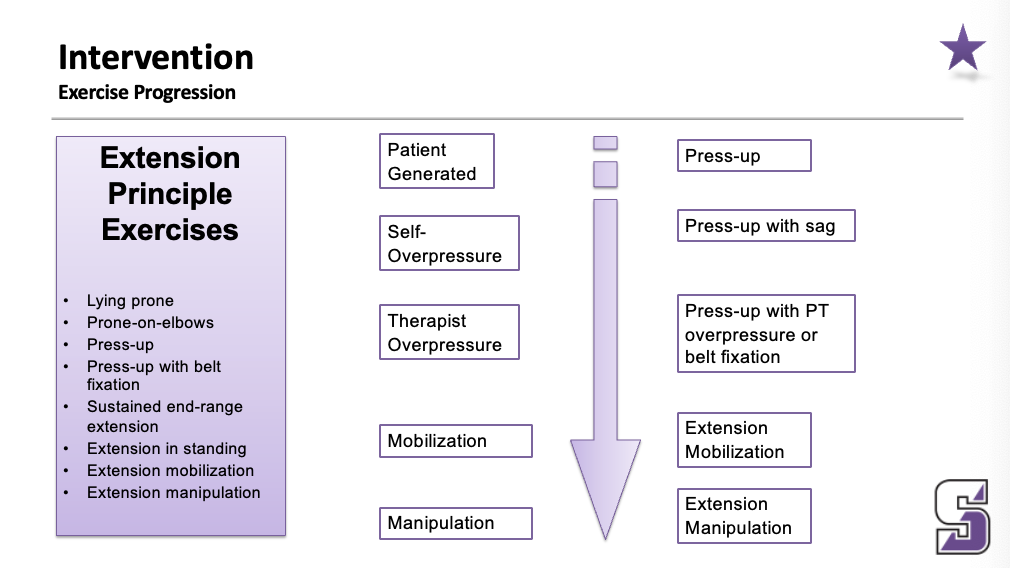
Intervention: exercise progression
____
Postural- named for aggravating static or sustain posture
Dysfunction- direction of restriction and pain provocation is the same, if you can’t flex and flexion causes you pain…then you are a flexion dysfunction
Derangement- named for the direction in which the NP is shifted in the disk…use posterior derangement…someone walks into the room bent over, how did that happen and how do we fix it?
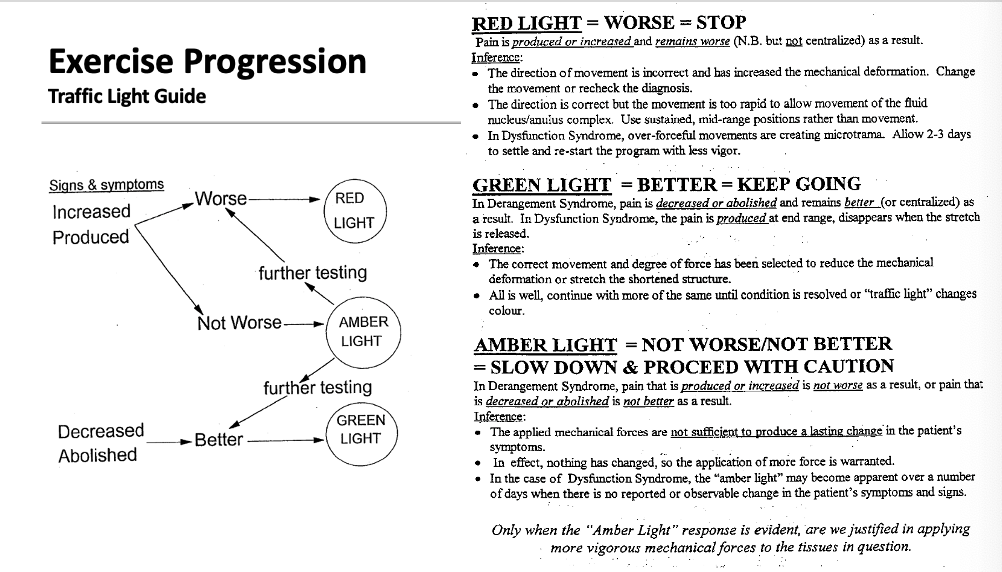
Exercise progression: traffic light guide
Intervention
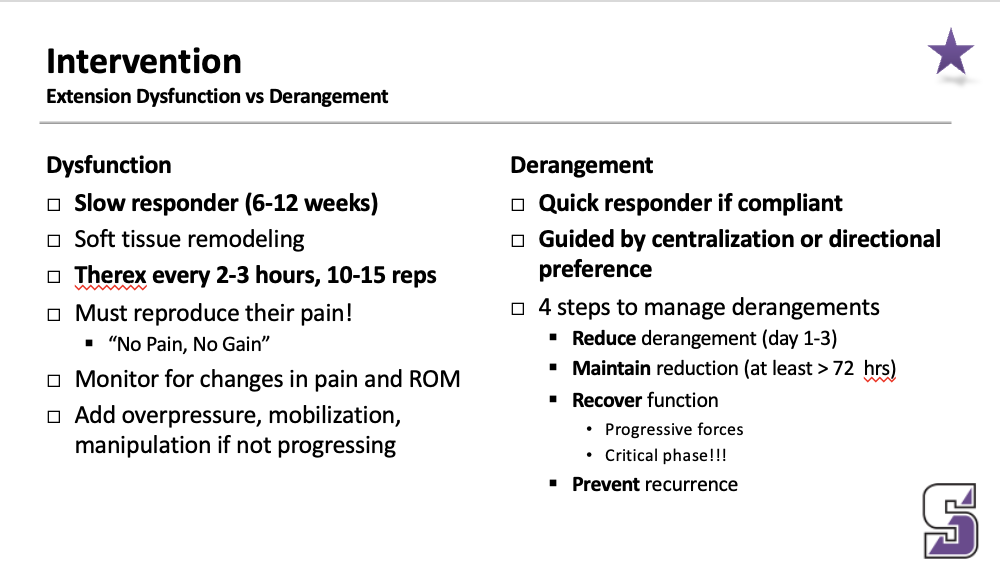
Extension Dysfunction
Slow responder (6-12 weeks)
Soft tissue remodeling
Therex every 2-3 hours, 10-15 reps
Must reproduce their pain!
“No Pain, No Gain”
Monitor for changes in pain and ROM
Add overpressure, mobilization, manipulation if not progressing
Intervention
Extension Derangement (4 steps to manage derangements)
Quick responder if compliant
Guided by centralization or directional preference
4 steps to manage derangements
Reduce derangement (day 1-3)
Maintain reduction (at least > 72 hrs)
Recover function
Progressive forces
Critical phase!!!
Prevent recurrence
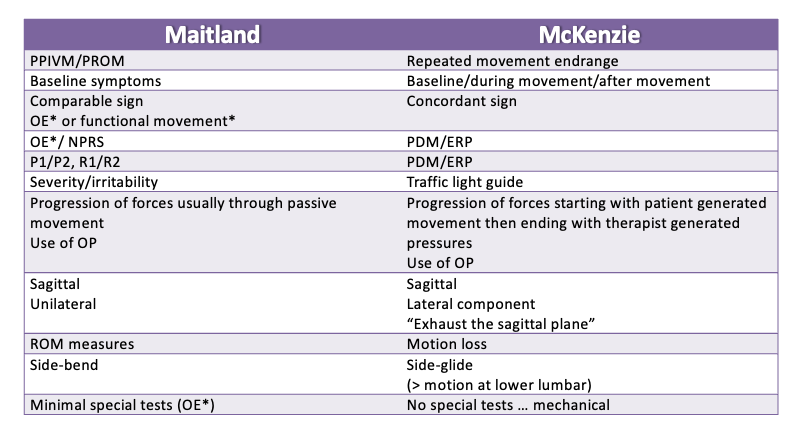
Maitland vs McKenzie interventions
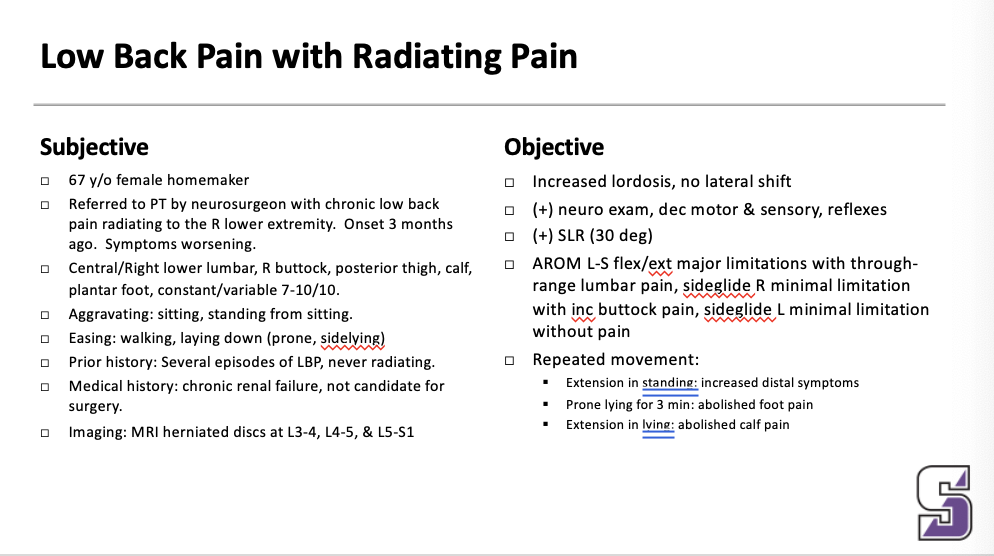
Case:
MDT classification
Is centralization or a directional preference present?
Derangement or dysfunction
MDT intervention
Exercise: prone press ups
Frequency per day: every hour
Sets/repetitions: 2x10
Education: avoid flexion and sitting for long periods of time – you can use a lumbar roll to get lordosis when sitting:
Centralization because of the “abolished” calf pain
Derangement because of the rapid change
If it was a dysfunction the sx would come back as soon as you stop
Can do bridges because it is an extension based
Mulligan Concept
Developed in the 1980’s by Brian Mulligan, a physical therapist from New Zealand
Based on the work of Kaltenborn, Maitland, and Paris
Uses NAGS, SNAGS, and MWMS … articular techniques with neuromuscular effects
Pain-free techniques
Immediate improvement in pain/function
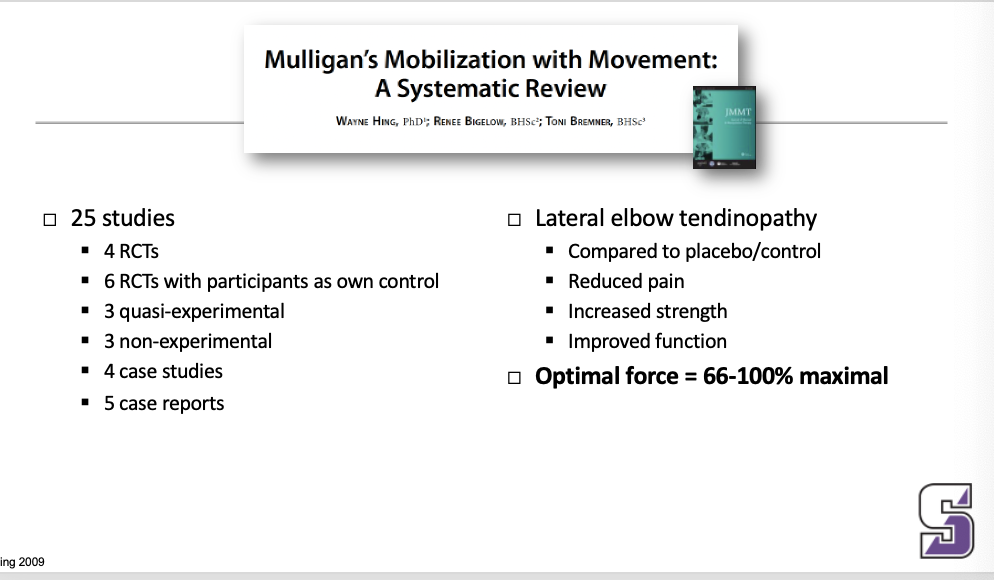
Avoid injections at the muscle tendon – tendonopathy is not inflammation
It is time for clinicians to finally update themselves on the nature of tendinopathy and to embrace, along with medical educators, that corticosteroid injections for tennis elbow worsen the long-term outcomes of patients. Corticosteroid injections should not be used to treat most patients with tennis elbow with symptom duration of less than 12 months.
Terminology (NAGS, MWM, SNAGS, SMWAMS)
Natural Apophyseal Glides (NAGS): passive accessory mobilizations which can be applied to facet joints between C2 and T3; glide one facet on its neighbor
Mobilizations With Movements (MWM): sustained repositioning of one articular surface on its neighbor while a movement or function is performed
Sustained Natural Apophyseal Glides (SNAGS): combination of sustained facet glide with movement; a SNAG is a MWM
Spinal Mobilizations With Arm Movements (SMWAMS): sustained transverse glide to spinous process of a vertebra is applied while the restricted peripheral joint is mobilized actively or passively
KEY Principles: PILL
If a PILL response is not achieved, do not use the technique!
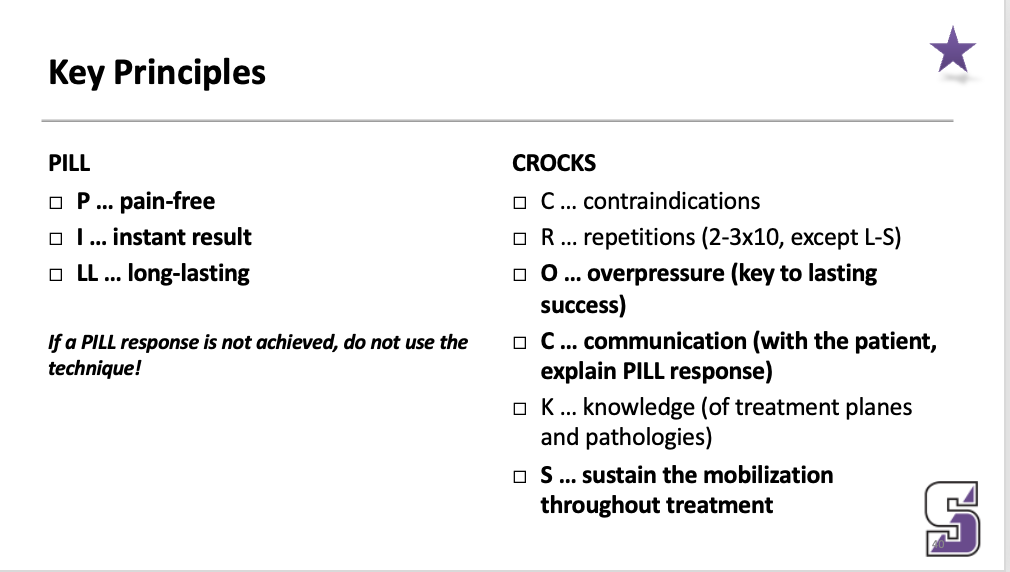
KEY Principles: CROCKS
C … contraindications
R … repetitions (2-3x10, except L-S)
O … overpressure (key to lasting success)
C … communication (with the patient, explain PILL response)
K … knowledge (of treatment planes and pathologies)
S … sustain the mobilization throughout treatment
Key principles
Mobilization w/ Movement: Mulligan Concept
Mobilization w/ Movement: combined movement to add dosage
key principles advantages vs disadvantages
Advantages:
Pragmatic approach with often immediate results
Focus on performance in weight-bearing (functional)
Emphasis on eventual self-performance
Combination of physiologic (osteokinematic) and accessory (arthrokinematic) motion
Techniques are pain-free and safe
Disadvantages
Techniques may not adhere to the biomechanics of the joint
Does not attempt to identify anatomic cause of impairment
Key Principles: indications
Painful restrictions of spinal and peripheral joint mobility
Commonly seen orthopedic conditions include:
Mechanical neck pain
Headache
Subacromial shoulder pain
Lateral epicondylitis
Hip pain (FAI/OA)
Patellofemoral pain
Ankle sprain/pain
Mobilization with Movement
Procedure
Identify pain producing movement
Apply passive accessory glide to the joint at approximately 50-75% of maximal force
Spine (SNAG): start at most symptomatic level
Extremity: usually a plane perpendicular to the joint axis
Patient actively performs previously restricted or painful motion (or active muscle contraction) while the PT maintains the accessory glide
Mobilization with Movement
Procedure if symptoms remain or worsen…
If symptoms remain or worsen …
Change direction of force
Change location of force (spinal level, patellofemoral vs tibiofemoral vs proximal tib-fib)
Ensure consistent glide is provided throughout the entire range
MWM not indicated
Mobilization with Movement
Procedure - if pain improved but not eradicated
If pain improved but not eradicated, fine-tune the glide (pressure, angle, et cetera)
_____
If pain improved but not eradicated, fine-tune the glide (pressure, angle, et cetera)
If asymptomatic, perform ten repetitions of the previously symptomatic movement
Re-test movement without the glide being applied
If not symptomatic …
Perform more repetitions of glide with movement
Pain-free over-pressure at end of range
Teach patient how to replicate the technique at home
Tape the joint in the desired position
Mobilization with Movement
Procedure - if asymptomatic
If asymptomatic, perform ten repetitions of the previously symptomatic movement
_____
If pain improved but not eradicated, fine-tune the glide (pressure, angle, et cetera)
If asymptomatic, perform ten repetitions of the previously symptomatic movement
Re-test movement without the glide being applied
If not symptomatic …
Perform more repetitions of glide with movement
Pain-free over-pressure at end of range
Teach patient how to replicate the technique at home
Tape the joint in the desired position
Mobilization with Movement
Procedure - if not symptomatic
Perform more repetitions of glide with movement
Pain-free over-pressure at end of range
Teach patient how to replicate the technique at home
Tape the joint in the desired position
____
If pain improved but not eradicated, fine-tune the glide (pressure, angle, et cetera)
If asymptomatic, perform ten repetitions of the previously symptomatic movement
Re-test movement without the glide being applied
If not symptomatic …
Perform more repetitions of glide with movement
Pain-free over-pressure at end of range
Teach patient how to replicate the technique at home
Tape the joint in the desired position
pain free
long-lasting
overpressure (key to lasting success)