Geri E2 Study Guide
1/136
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
137 Terms
What is the pathophysiology of pressure injuries?
Soft tissue compression → microvascular occlusion → ischemia & hypoxia (~3-4 hrs)
Friction → breaks skin surface; shearing forces → separates DEJ → dec tissue perfusion; moisture → further tissue breakdown
What are the 4 most susceptible bony prominences?
Sacrum (MC), heels, greater trochanter, ischial tuberosity
What normal changes are seen in elderly skin?
Thinning dermis & decreased vascularity, decreased elastin, loss of SC fat, decreased dermal-epidermal turnover
What must be included when assessing a pressure injury and documenting the description?
Assess (weekly): location, class/stage, size, base tissues, exudates, odor, edge/perimeter, pain, eval for infx
Document: location (extremity, nearest bony prominence, anatomical landmark)
What should you never do when staging a wound?
Back stage → should never be restaged at a lesser stage

What stage pressure injury?
intact skin with localized area of non blanchable erythema
does NOT include purple or maroon discoloration
± edema, induration, warmth
heal: tissue regeneration
Stage I

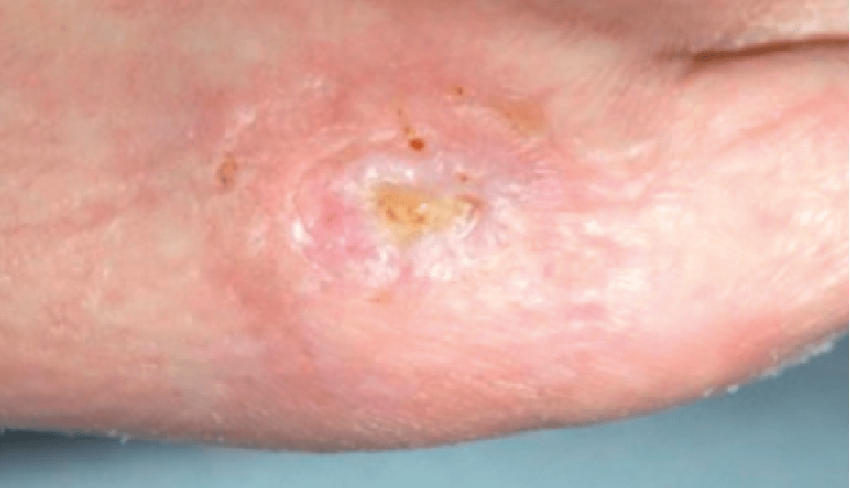
What stage pressure injury?
partial thickness skin loss that does not go deeper than dermis
NO SC tissue exposure; no granulation tissue, slough or eschar present
can include intact or ruptured blisters
heal: tissue regeneration
Stage II

What stage pressure injury?
full thickness skin loss that extends into SC tissue
no fascia, muscle, tendon, ligament, or bone is exposed
epibole - rolled wound edges
heal: scar formation & contraction
Stage III

What stage pressure injury?
Full thickness skin loss with extensive destruction exposing muscle, tendon, cartilage or bone
tissue necrosis; slough & eschar may be visible; epibole, undermining & tunneling often occur
heal: scar formation and contraction
Stage IV
What is a reliable predictive indicator of pressure injury healing?
20% reduction in wound size over 2 weeks

What stage pressure injury?
persistent localized area of nonblanchable deep red or purple skin
intact or non-intact
can also present as blood filled blisters
caused by damage to underlying soft tissues
Deep tissue pressure injury (DTPI)

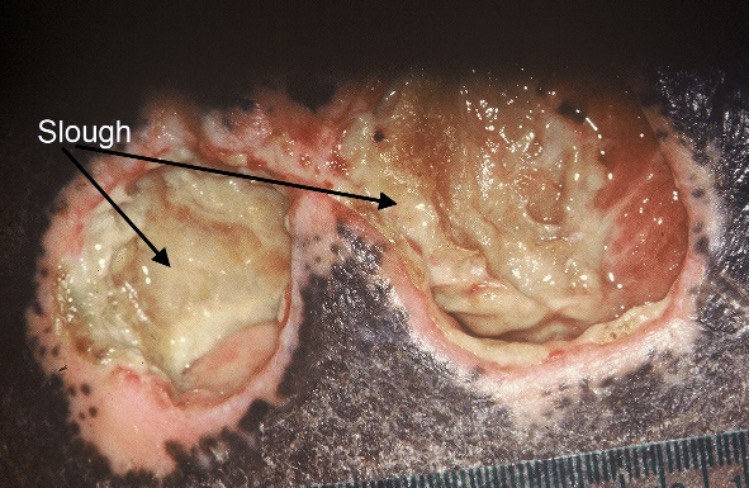
What stage pressure injury?
localized areas of tissue necrosis covered with slough (viscous fibrinous dead tissue that is yellowish) or eschar (dead tissue that is dry, dark scab)
base of ulcer not visible & can’t properly assess depth
Unstageable
How should wound size be assessed?
length (head to toe), width (edge to edge, perpendicular), & depth (straight in) in cm
How should undermining or tunneling of a pressure injury be assessed?
Clock concept → 12 o’clock is in direction of patients head, 6 towards feet; note where it starts, ends, depth, and location of deepest point
What is tunneling?
Extension of wound into fascial planes that results in a narrow passageway along the base of the wound
What is undermining?
Dead space is caused by erosion under the wound edges (large wound w/ small opening); less extensive
What is eschar/necrosis?
Black, brown or tan devitalized tissue that adheres to the wound bed or edges & may be firmer or softer than surrounding skin

What is slough?
Soft, moist avascular tissue that adheres to the wound end in strings or thick clumps; may be white, yellow, tan, or green
What is granulation?
Pink/red moist tissue comprised of new blood vessels, collagen fibers, & fibroblasts; surface is shiny & moist w/ granular appearance

What is epithelium?
New pink & shiny tissue/skin that grows in from the edges or as islands on the wound surface
What is the criteria for documenting the amount of exudate associated with a wound?
None: base & dressing dry
Slight: small amount in center of dressing
Moderate: contained w/in the dressing
Copious: extends beyond dressing onto clothing or bed linen (concern for infx)
What is serous exudate?
Thin, watery, clear, or straw colored
What is serosanguinous exudate?
Thin, pale red to pink
What is purulent exudate?
Thick, opaque, tan, yellow to green & may have offensive odor
What is critical colonization?
Multiplication of organisms w/o invasion but interfering with wound healing, wound is stagnate w/o obvious signs of infection
When would you be concerned about critical colonization?
Signs of infection are present or when wound fails to heal
*testing → Semi-quantitative swab, Quantitative bx (gold standard but $$ & invasive), ABI - compares perfusion pressures
What stage of wound healing?
bleeding stops, balance between coagulants, vasoconstriction, formation of plt plug, clot retraction, fibrinolysis
Hemostasis
What stage of wound healing?
wound formation-6 days
redness, swelling, warmth, pain, phagocytosis, GF stimulation
Inflammation
What stage of wound healing?
4-24 days
angiogenesis, granulation formation, epithelialization, collagen synthesis, contraction of wound edges
Proliferation
What stage of wound healing?
21-2 yrs
scarring period, reorganization of collagen, tensile strength improves (up to 80%)
Remodeling
What healing phase do chronic wounds primarily remain in?
Inflammatory phase
How can you best optimize wound environment?
Encourage adequate perfusion & protect from pressure & friction, manage comornid conditions, encourage protein, calorie dense foots & fluids unless CI, dietary consult, manage pain, saline soln irrigation 4-15 psi, protect skin w barrier products, prevent or tx infx, debridement
What is the removal of nonviable tissue to remove growth medium, control & prevent infx, define extent of wound & stimulate healing process?
Debridement
What kind of debridement is not recommended as it is nonselective, causes repeated trauma to the wound bed, & is frequently painful?
Wet to dry dressing mechanical debridement (saline soaked, allowed to dry, then tear off)
What should treatment include for stage 1 & 2 pressure injury?
Encourage adequate perfusion & protect further tissue damage & friction
What should stage III pressure injury treatment include?
Debridement to promote granulation & contraction (epithelialization)
What should stage 4 pressure injury treatment include?
More aggressive debridement (surgical) to promote granulation & contraction (epithelialization)
What is rotational sensation made worse by moving head?
*never continuous for more than a few weeks bc CNS will adapt
Vertigo
What is the sensation of near-fainting, feeling of faintness or lightheadedness?
*sign of decreased cerebral perfusion
Pre-syncope
What is the feeling of imbalance or being unsteady when standing or walking?
*usually from visual or proprioceptive system abnormalities
Disequilibrium
What is the sudden, transient loss of postural tone and consciousness with spontaneous full recovery (not due to trauma)?
Syncope
What condition?
MC peripheral vestibular disorder
inner ear: canalithias (calcium debris / loos otoconia) w/in semicircular canal → endolymph movement → sensation of spinning
brief spells (5-15s) associated with positional change- turning, rolling over, bending)
BPPV
What maneuver is used to treat BPPV?
Epley
How can you differentiate positional vertigo or BPPV from postural syncope (dizziness upon standing d/t lower BP)?
Maneuvers that change head position but don’t lower BP → lying down, rolling over in bed, bending neck to look up
What condition?
idiopathic inner ear disorder: increased endolymphatic pressure for unknown reason
aural fullness, tinnitus, vertigo, sensorineural hearing loss
*dx w/ audiometry
Meniere’s disease
What stage of Meniere’s disease?
sudden unpredictable vertigo
hearing loss & tinnitus only during vertigo, normal between attacks
Early
What stage of Meniere’s disease?
vertigo attacks less severe
hearing loss & tinnitus becomes worse
periods of remission
Middle
What stage of Meniere’s disease?
less frequent vertigo
hearing loss & tinnitus becomes worse
problems with balance
Late
What are treatment options for Meniere’s disease?
Salt restriction, diuretics, vestibular suppressants during acute attacks
Severe: surgery, endolymphatic decompression, vestibular nerve resection, labyrinthectomy
What condition?
MC brain tumor associated with dizziness
Unilateral cochlear sx (tinnitus, hearing loss) predominate over dizziness
Acoustic neuroma
What are the MCC of pre syncope?
Tachy/bradyarrhythmia, aortic outflow obstruction, orthostatic hypotension, vagal stimulation, postural changes, prost-prandial hypotension
Does Ramsay hunt, Meniere’s disease, or BBPV present with clumsiness of the extremities?
No
What factors are associated with disequilibrium?
Proprioceptive disorders- peripheral neuropathies; cataracts, macular degeneration, RA, OA, weakness, deconditioning after prolonged illness, CVA, parkinsons, cerebellar disorders
What medication classes are most associated with dizziness in the elderly?
*use of ≥3 meds = dizziness RF
Aminoglycosides (gentamicin), NSAIDs, CV or hypertensive drugs, psychotropic meds
How should you evaluate dizziness & elicit the patient’s description of their sx?
Encourage use of their own words, describe specific sensations such as spinning, imbalance / unsteadiness, or fainting, pay attention to exacerbating or precipitating factors (head position, time of day)
Which provocative test of the vestibular system?
diagnoses BPPV
positive:
paroxysmal vertigo along with rotary nystagmus,
latency 1-2s bt completion of maneuver and onset of vertigo and nystagmus,
fatigability (dec in intensity of vertigo and nystagmus with repeated testing)
Dix hallpike
Which provocative test of the vestibular system?
Ask pt to fixate on examiners nose -> rotate pts head rapidly 10° to the left or right
Normal = eyes remain fixed on target w/o saccade
Vestibular deficit =eyes move away from the target along with head, followed by corrective saccade (jerking movement) back to the target
Head thrust test
Which provocative test of the vestibular system?
Draw circle on floor and ask pt to stand in the center -> blindfold pt and ask to take a few steps forward as if walking on a straight line with outstretched arms -> no body sway
In UL vestibular lesion or acoustic neuroma: body will sway >30 degrees toward affected side
***difficult for elderly population with weakness, gait disorders
Fukuda stepping test
What other than provocative tests should always be performed on a physical exam when evaluating dizziness?
BP & pulse supine and after standing 1-2 min, cardiac exam, observe balance & gait (timed up & go), hearing & vision tests
if suspected vertebrobasilar infarction → cranial nerves
If dizziness is longstanding, lasting more than several months, what other conditions should you be considering?
Vertebrobasilar ischemia, cerebellar infarct/hemorrhage, Acoustic neuroma, Parkinsons, Peripheral neuropathy secondary to DM, B12 deficiency, cervical degenerative arthritis, spondylosis
What other tests can be considered in the evaluation of chronic dizziness?
Check hct, glucose, eleytes, renal function, vit B12, folic acid, thyrotropin
Audiometry if cochlear sx, EKG if cardiac cause, MRI, CT, vestibular function tests
What is the pathophysiology of syncope?
Reflexes are less responsive: dec ability to increase HR to sympathetic stimulation, inc sensitivity to effects of dehydration & vasodilators
Reduced baroreflex control of HR, arterial vasoconstriction, dec LV compliance, dec GFR
What comorbidities affect postural responses?
DM → high sugar → more urination = less water (dehydrated)
What drugs impair postural reflexes?
Vasodilators, antidepressants, alpha blockers, BBs, TCAs
The following syncopal episode is associated with what cause?
Prior: occurs in any position, sudden onset, < 5 second warning
During: flaccid tone, absent or faint pulse, blue ashen skin, incontinence (rare)
Recovery: rapid & complete
Arrhythmia
The following syncopal episode is associated with what cause?
Prior: second-minutes warning, precipitant present, N, diaphoresis, visual changes, can be aborted if pt lies flat
During: motionless, relaxed tone, slow faint pulse, pale, dilated reactive pupils
Recovery: fatigue, N, diaphoresis, no retrograde amnesia
Vasovagal
The following syncopal episode is associated with what cause?
Prior: occurs in any position, no warning or prodrome
During: rigid tone, rapid pulse, elevated BP, tonic eye deviation, frothing at mouth, incontinence
Recovery: slow, incomplete, disorientation, focal neurological findings
Seizure
How should a carotid pulse exam be performed when evaluating syncope?
Only with continuous EKG & resuscitation equipment available; delayed upstroke & low volume may indicate aortic stenosis
*CI with carotid bruit, CVD, recent MI
Why is obtaining an ECG in individuals experiencing syncope important? What syncopal conditions can an ECG uncover?
Important to r/o cardiac cause, especially in asx patients; assess for MI, conduction abnormalities, pre-excitation, sinus bradycardia, prolonged QT
What are the treatment options for syncope caused by significant ventricular tachyarrhythmias?
Implant defibrillator or medical therapy
What are the treatment options for syncope caused by bradyarrhythmias?
Pacemaker
What are the treatment options for syncope caused by symptomatic SVTs?
Medical therapy or electrophysiology ablation
What are the treatment options for syncope caused by orthostatic hypotension?
Adjust meds, ensure adequate volume, conservative measures (stockings, squatting, sleeping in head up position, avoid excessively warm environments, activities associated with straining)
What are the treatment options for vasovagal syncope?
Avoid triggers, medical therapy somewhat controversial (BB, clonidine, paroxetine, midodrine)
What are the treatment options for syncope caused by carotid sinus hypersensitivity?
Avoid stimulating factors (tight collars, rapid neck movements), pacemakers
What are the treatment options for syncope caused by postprandial hypotension?
Lie down for 30-60 min after meals, frequent small meals, slow rise from sitting position, avoid alcohol, high carb meals, exercise after meals, & antihypertensives during / near meal time
Describe the sympathetic and parasympathetic control of normal micturition.
Sympathetic: causes the proximal urethral smooth muscle to contract (T11-L2), controls urine storage, inhibits detrusor contraction, inc sphincter contraction
Parasympathetic: causes the bladder smooth muscle (detrusor) to contract (nerves S2-S4), controls voiding, induces sphincter relaxation
What are age related urinary tract changes that occur and what do they result in?
Detrusor muscle function declines, fibrosis of bladder wall, & heightened sensitivity to NTs
Results in: reduced bladder capacity, detrusor instability, reduced urinary flow rate, reduced voided volume, inc post void residual
What are transient causes of urinary incontinence?
Delirium
Infection
Atrophic vaginitis or urethritis
Pharmaceuticals
Psychological problems
Excessive urine output
Restricted mobility
Stool impaction
What are the 4 major types of urinary incontinence?
Urge (MC): leakages with or before urge to void; overactive bladder ± incontinence, nocturia, urinary frequency
Stress: leakage with inc intra-abdominal pressure in absence of bladder contraction
Overflow: continuous leakage, dribbling, incomplete emptying, bedwetting, elevated PVR
Functional: physically unable to toilet in timely fashion despite intact function
*can also have mixed
What type of incontinence is caused by detrusor overactivity, which leads to an overactive bladder? What nonpharm treatment have been associated with high rates of satisfaction (equal to or better than bladder relaxant agents)?
Urge incontinence
Bladder training, biofeedback, pelvic muscle exercises
What are the primary causative mechanisms associated with stress incontinence?
Weak pelvic floor muscles (urethral hypermobility, genuine stress incontinence, episodic leakage w/ inc intra-abd pressure)
Intrinsic sphincter deficiency (ctrauma, scarring from anti-incontinence surgery in women, prostatectomy in men, continual leakage may occur while sitting or standing)
What population is overflow incontinence MC in? What causative mechanisms are associated with it?
Men; outlet obstruction & detrusor overactivity (smooth muscle damage, peripheral neuropathy, damage to spinal cord or bladder nerve)
*inadequate emptying PVR = 200 mL
What are SEs of antimuscarinics?
oxybutynin (gold standard), tolterodine, tropism, darifenacin, solifenacin, fesoterodine
Dry mouth, blurry vision, constipation, dental caries, ulceration of gums & tooth decay, cognitive
take effect w/in 1st month
Which antimuscarinic is renally cleared and needs dose reduction in renal insufficiency?
(all others have interactions with CYP3A4 & 2D6 except this one)
Trospium
What SEs are seen with beta-3 adrenergic agonists (Mirabegron)?
***more favorable tolerability rate than antimuscarinics
Constipation/diarrhea, HA, dizzy, Nausea, Tachycardia, HTN, UTI
can take 4-8 weeks
What are the treatment options for overflow urinary incontinence?
Tx underlying cause if obstruction or constipation, reduce or stop RX that impairs detrusor contractility or increases urethral tone, intermittent clean catheter, protective garments (last resort)
What concerns are associated with intermittent and indwelling catheterization?
Significant morbidity: polymicrobial bacteriuria, nephrolithiasis, urolithiasis, epididymitis, chronic renal inflammation, pyelonephritis
bacteriuria is universal in catheterized patients (dont tx in absence of clear sx of infx, dont routinely culture or reculture after UTI rx)
How should catheters be cared for?
Change about once a month (can be longer in absence of UTI) or every 7-10 days if recurrent blockage; Proph abx if short term; Keep long term care residents with catheters in separate rooms from each other
Patient has worsening urinary retention that has not yet progressed to complete retention (“overflow incontinence”). He has a midline mass emanating from suprapubic area that is dull on percussion. Portable US shows ~600 ml of urine. What is the next best step?
Insert foley Cath; if bladder volume is confirmed, leave catheter in and refer for further evaluation
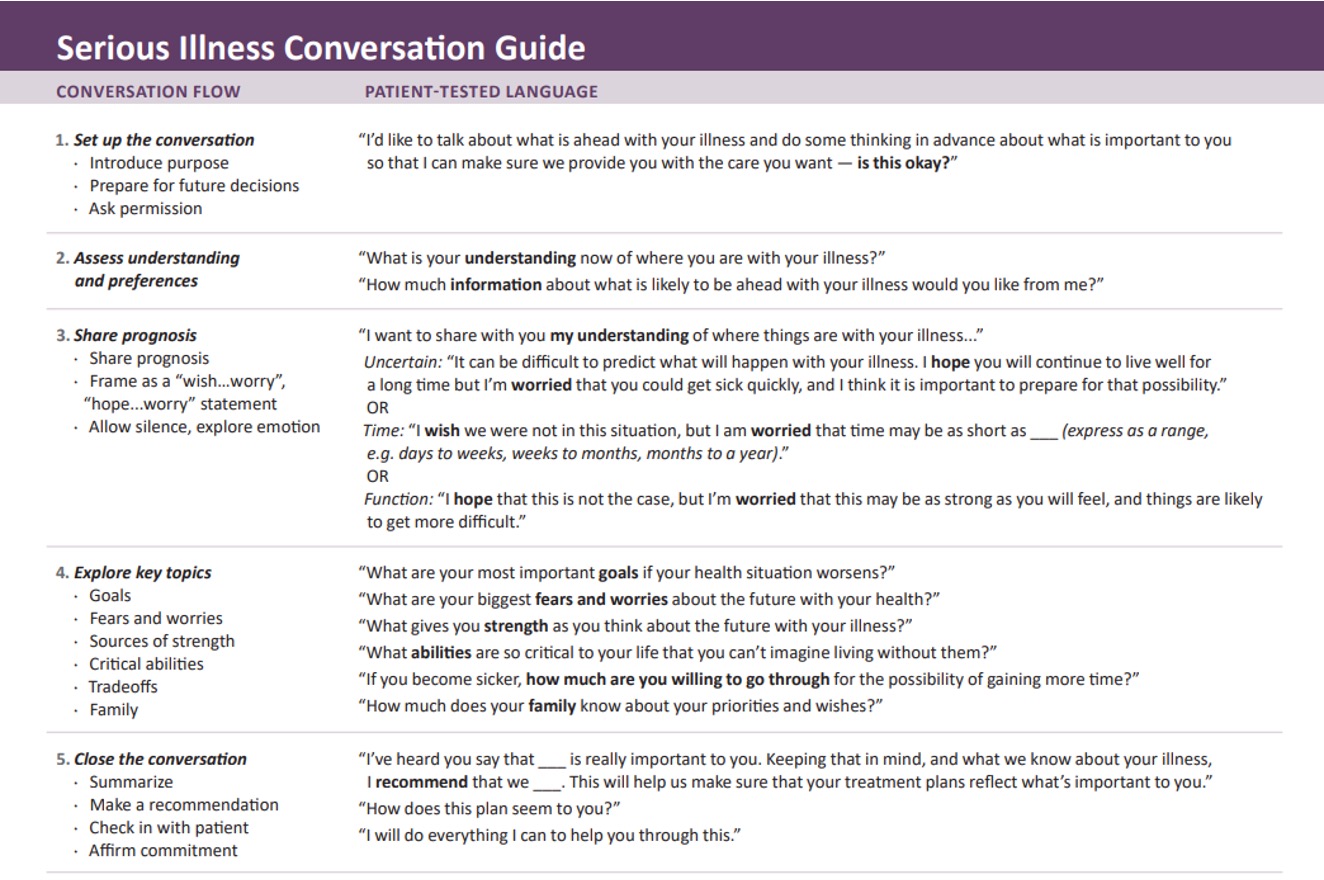
What protocol provides an approach for difficult discussions?
SPIKES → setting, perception/perspective, invitation, knowledge, empathy/emotion, summary/strategy
What is the main goal of palliative care?
Patient-family centered care → improve QOL for people suffering from severe illness
What conditions are palliative care appropriate diagnoses?
ALS, Parkinson’s dz, HIV/AIDS, Dementia/Alzheimer’s, CHF III+, stroke, advanced liver disease, COPD/emphysema/ILD/IPF, failure to thrive (BMI < 18), Malignancy (solid tumor, hematologic)
Palliative care or hospice?
end of life (or disease trajectory)
reduce suffering
prognosis ≤ 6 mos
Hospice
Palliative care or hospice?
at time of diagnosis
maximize QOL
improve function
reduce suffering
allow control for pts/family
Palliative care
What must an individual's life expectancy be before insurance covers hospice benefits? If the criteria are met, what percentage of care is covered by most insurance companies?
≤ 6 mos to live; covers 100% of care
What are the pitfalls and challenges of palliative care and how can they be avoided?
biggest - starting discussion too late or not at all; rushed conversation or expecting family to make dramatic decisions; delivering too much info & pressuring for decisions too quickly, conversation bias (should, shouldn’t, can’t)
avoid w/ advanced care planning or remap mnemonic? idek
How is cancer pain best managed in palliative care?
Pure opioid agonists → Codeine, Hydrocodone, Morphine, Hydromorphone, Fentanyl, Oxycodone, Oxymorphone
*meperidine & propoxyphene not recommended
What should be used for refractory chemo-induced nausea (also treats loss of appetite)?
Liquid Marinol (cannabis)
How is constipation best managed in palliative care?
Adequate fiber, encourage bowel pattern, inc fluid intake & exercise
1st line: bulk laxatives
2nd: osmotic laxatives