Intro to Clinical Sciences Phase2a
0.0(0)
Card Sorting
1/289
Earn XP
Description and Tags
Last updated 2:24 PM on 3/17/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
290 Terms
1
New cards
Which type of inflammation is primarily associated with neutrophils?
Acute inflammation
2
New cards
What is chronic inflammation?
Slow or sequel to acute, long term inflammation involving B&T lymphocytes (plasma cells) and macrophages
3
New cards
Which cell type lives for 1-3 days?
Neutrophil polymorphs
4
New cards
Which cell types are involved in inflammation?
Neutrophil polymorphs
Macrophages
Lymphocytes
Endothelial cells
Fibroblasts
Macrophages
Lymphocytes
Endothelial cells
Fibroblasts
5
New cards
What is the approximate life-span of a macrophage?
weeks-months
6
New cards
What are the 5 cardinal signs?
1. rubor (redness)
2. calor (heat)
3. tumor (swelling)
4. dolor (pain)
5. loss of function
2. calor (heat)
3. tumor (swelling)
4. dolor (pain)
5. loss of function
7
New cards
What are the 3 stages of acute inflammation?
Change in vessel calibre (wider space for same no. cells)
Increased vascular permeability
Formation of fluid exudate
Increased vascular permeability
Formation of fluid exudate
8
New cards
What is inflammation?
A local physiological response to tissue injury
9
New cards
What is margination?
Stage in neutrophil action where neutrophils move to the plasmatic zone near the endothelium due to loss of fluid
10
New cards
Define granuloma
Aggregate of epitheloid histiocytes
(small area of chronic inflammation characterised by a collection of macrophages in a histological horse shoe shape)
(small area of chronic inflammation characterised by a collection of macrophages in a histological horse shoe shape)
11
New cards
What is meant by the term 'pavementing' in neutrophil action?
Neutrophils adhere to the endothelium and "roll"
12
New cards
The term used to describe neutrophils moving through walls of venules and veins into the extravascular space is...
Emigration
13
New cards
What is diapedesis?
The migration of blood cells (R&W) into the extravascular space in inflammation
14
New cards
What are the possible outcomes of inflammation?
1) resolution - complete return to normal
2) suppuration - pus formation
3) organisation (repair) - necrosis, regrowth, scarring
4) progression - chronic inflammation
2) suppuration - pus formation
3) organisation (repair) - necrosis, regrowth, scarring
4) progression - chronic inflammation
15
New cards
What are the benefits of acute inflammation?
- dilution of toxins to be carried away in lymphatics
- entry of antibodies
- useful for drug transport to site eg. antibiotics to bacteria
- fibrin formation
- delivery of nutrients and oxygen from increased fluid flow
- stimulation of immune response by fluid exudate entering lymphatics
- entry of antibodies
- useful for drug transport to site eg. antibiotics to bacteria
- fibrin formation
- delivery of nutrients and oxygen from increased fluid flow
- stimulation of immune response by fluid exudate entering lymphatics
16
New cards
What are the negatives of acute inflammation?
- digestion of normal tissues by enzymes
- swelling in bad areas eg. brain, epiglottis
- inappropriate responses eg. hypersensitivity reactions, autoimmune
- swelling in bad areas eg. brain, epiglottis
- inappropriate responses eg. hypersensitivity reactions, autoimmune
17
New cards
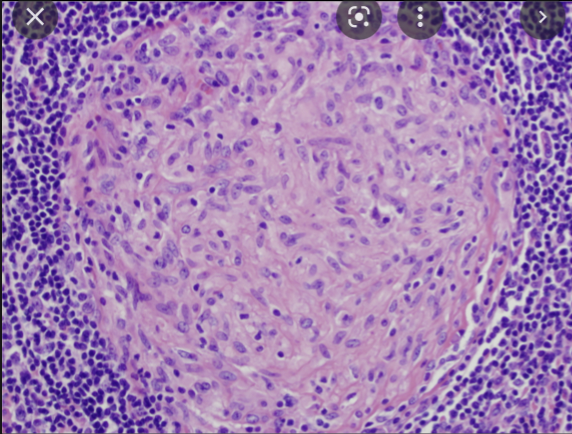
What is shown?
Granuloma
18
New cards
What is the clinical significance of raised Angiotensin-Converting-Enzyme in the blood?
Granulomas secrete ACE Marker of other granulomatous diseases such as TB, parasitic infections (if eosinophil is raised), sarcoidosis, leprosy, syphilis, Crohn's disease
19
New cards
What is a caseating granuloma?
Cheese-like necrosis
found in TB, fungal infections
found in TB, fungal infections
20
New cards
What are non-caseating granulomas?
Granulomas formed by inflammatory conditions (sarcoidosis, chron) or foreign objects
21
New cards
What happens in resolution of acute inflammation?
The initiating factor is removed, the tissue is either undamaged or can regenerate
eg. a bone after a break
eg. a bone after a break
22
New cards
What happens in the organisation of acute inflammation?
the initiating factor is still present
the tissue is damaged and unable to regenerate
the damaged tissue is replaced by fibrous tissue (mainly collagen) forming a scar
the tissue is damaged and unable to regenerate
the damaged tissue is replaced by fibrous tissue (mainly collagen) forming a scar
23
New cards
Name an example of a tissue and condition that cannot be resolved, only organised
heart after myocardial infarction
brain after cerebral infarction
spinal cord after trauma
brain after cerebral infarction
spinal cord after trauma
24
New cards
What is the difference between exudate and transudate?
Exudate - high protein, increased vascular permeability, formed in inflammation
transudate - low protein, normal permeability, normal circumstances
transudate - low protein, normal permeability, normal circumstances
25
New cards
Give 5 types of cell capable of regeneration
Hepatocytes
Osteocytes
Pneumocytes
Blood cells
Gut and skin epithelial cells
Osteocytes
Pneumocytes
Blood cells
Gut and skin epithelial cells
26
New cards
Why do blood clots not constantly form?
1) laminar flow (blood travels in the centre of arterial vessels)
2) endothelial cells are not sticky if healthy
2) endothelial cells are not sticky if healthy
27
New cards
Define thrombosis
The formation of a solid mass from blood constituents in an intact vessel
28
New cards
Define embolism
A blocked blood vessel caused by an embolus such as a clot or air bubble
29
New cards
What is ischaemia?
reduced blood flow to a tissue without other implications
30
New cards
What is infarction?
Ischaemic necrosis of tissue
31
New cards
What are the causes of thrombosis?
1. change in blood flow (stasis)
2. change in blood constituents (hyper coagulability)
3. change in the vessel wall (endothelial damage)
32
New cards
What is the most common cause of a venous thrombosis?
stasis
33
New cards
What is the most common cause of an arterial thrombosis?
Atheroma
34
New cards
What are the different types of embolism?
venous thromboembolism
pulmonary embolism
systemic embolism
infective emboli
fat embolism
gas embolism
amniotic embolism
tumour
foreign
pulmonary embolism
systemic embolism
infective emboli
fat embolism
gas embolism
amniotic embolism
tumour
foreign
35
New cards
What happens to a thrombus?
1. the body dissolves and clears it
2. organised into a scar by macrophages
3. capillaries grow into the thrombus and fuse later, vessel is recanalized
4. death
5. embolism
2. organised into a scar by macrophages
3. capillaries grow into the thrombus and fuse later, vessel is recanalized
4. death
5. embolism
36
New cards
Explain primary plug formation in haemostasis
1. damaged endothelium exposes collagen to the inter vascular space
2. vasospasm: endothelin-1 release causes vasoconstriction
3. platelet adhesion: platelets glycoprotein 1b receptor bind to collagen via von-willebrand-factor
4. platelet activation: platelets release platelet dense granules with ADP, thromboxane, Clotting factors and activates other platelet.
5. aggregation: ADP dependent expression of glycoprotein IIb/IIIa, + ADP P2Y12 receptor activates glycoprotein IIb/IIa on platelets bind to fibrinogen creating crosslinks, platelets are aggregated
37
New cards
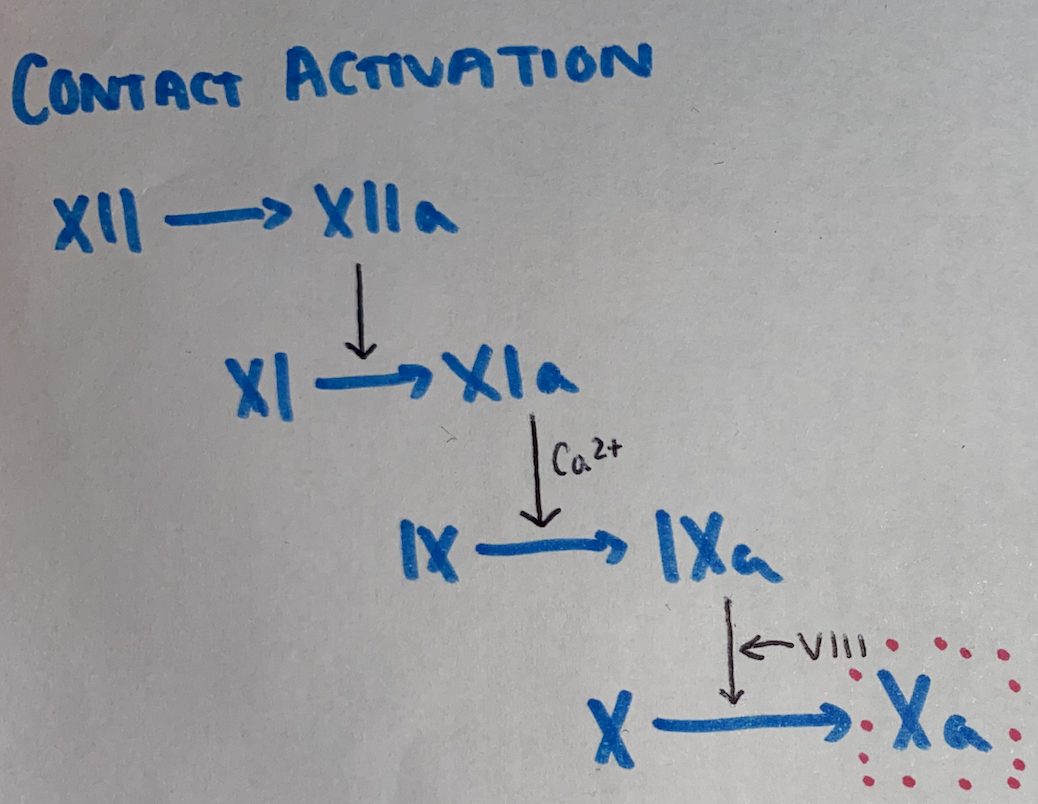
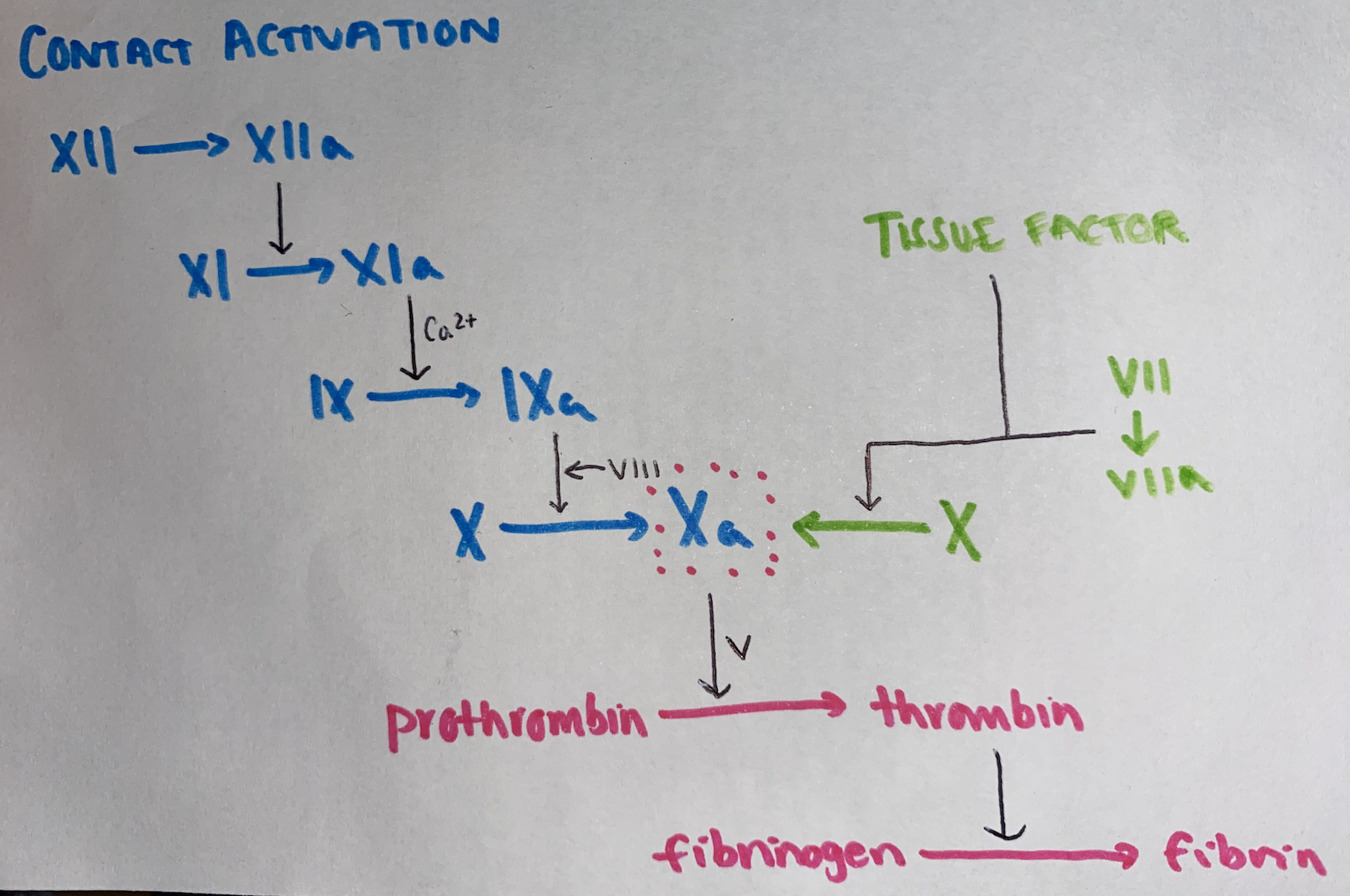
Intrinsic pathway of secondary plug in haemostasis
contact activation
XII -> XIIa
XI -> XIa
IX -> IXa + VIIIa
X -> Xa
common pathway
XII -> XIIa
XI -> XIa
IX -> IXa + VIIIa
X -> Xa
common pathway
38
New cards
Extrinsic pathway of the secondary platelet plug
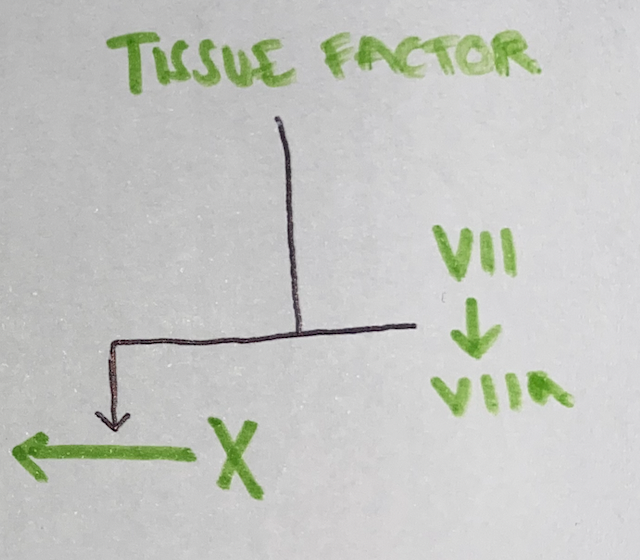
39
New cards
Secondary plug formation in hemostasis
40
New cards
Define congenital disease
Disease which is present at birth
41
New cards
Compare inherited and acquired disease
inherited - inherited genetic abnormality
acquired - caused by non-genetic environmental factors
acquired - caused by non-genetic environmental factors
42
New cards
An increase in the size of a tissue due to increase in the size of constituent cells is
hypertrophy
43
New cards
what is hyperplasia?
Increase in the size of a tissue due to increase in the number of the cells
44
New cards
What is metaplasia?
The change in differentiation of a cell from one fully-differentiated type to a different fully differentiated type
45
New cards
Give an example of normal metaplasia in the body
Change from respiratory epithelium in the trachea to simple squamous in the alveoli
46
New cards
pre-malignant cells changing morphology is known as
dysplasia
47
New cards
decrease in the size of an organ or tissue
atrophy
48
New cards
Give 3 physiological examples of hyperplasia
- bone marrow production of erythrocytes at high altitude
- breast tissue at pregnancy/puberty
- thyroid in puberty/pregnancy
- breast tissue at pregnancy/puberty
- thyroid in puberty/pregnancy
49
New cards
Give an example of pathological hyperplasia
Grave's disease
Prostate with age and excess oestrogen
Prostate with age and excess oestrogen
50
New cards
What are the pathological causes of hypertrophy?
- arterial walls in hypertension
- RV from pulmonary valve stenosis, hypertension or septal defects
- LV from aortic valve stenosis or systemic hypertension
- RV from pulmonary valve stenosis, hypertension or septal defects
- LV from aortic valve stenosis or systemic hypertension
51
New cards
Give an example of physiological hyperplasia and hypertrophy
uterine smooth muscle in puberty and pregnancy
52
New cards
When is atrophy considered normal?
- thymus in early adulthood
- fetus
- genitals, mandible, cerebrum, lymphoid tissues in the elderly
- fetus
- genitals, mandible, cerebrum, lymphoid tissues in the elderly
53
New cards
When is atrophy considered pathological?
- loss of blood supply
- loss of innervation
- pressure eg. pressure sores, tumours
- lack of nutrition
- lack of, or hormonal stimulation
- decreased function eg. fracture
- loss of innervation
- pressure eg. pressure sores, tumours
- lack of nutrition
- lack of, or hormonal stimulation
- decreased function eg. fracture
54
New cards
The use of topical corticosteroids can cause what?
skin atrophy
55
New cards
What is the difference between apoptosis and necrosis?
Apoptosis: programmed cell death, non-inflammatory, sometimes pathological
Necrosis: traumatic unexpected cell death, inflammatory, always pathological
Necrosis: traumatic unexpected cell death, inflammatory, always pathological
56
New cards
Explain the intrinsic pathway of apoptosis
BAX & BAK proteins promote apoptosis by signalling the mitochondria to release cytochrome C which activates caspases which cause cell death
57
New cards
Explain the extrinsic pathway of apoptosis
Fas-Ligand & Fas or TNF-a & TNF-R
activate initiator caspases
activates caspases
cell death
activate initiator caspases
activates caspases
cell death
58
New cards
Which proteins inhibit apoptosis?
Bcl-2 and Bcl-xl
59
New cards
Explain the cytotoxic pathway of apoptosis
if a cytotoxic T cell binds to a membrane, it releases Granzyme B which allows perforin to enter the cell and activate caspases
60
New cards
Give an example of necrosis from ischaemia
fingers in frostbite
avascular necrosis in scaphoid fractures
pancreatitis
caseous necrosis in TB
avascular necrosis in scaphoid fractures
pancreatitis
caseous necrosis in TB
61
New cards
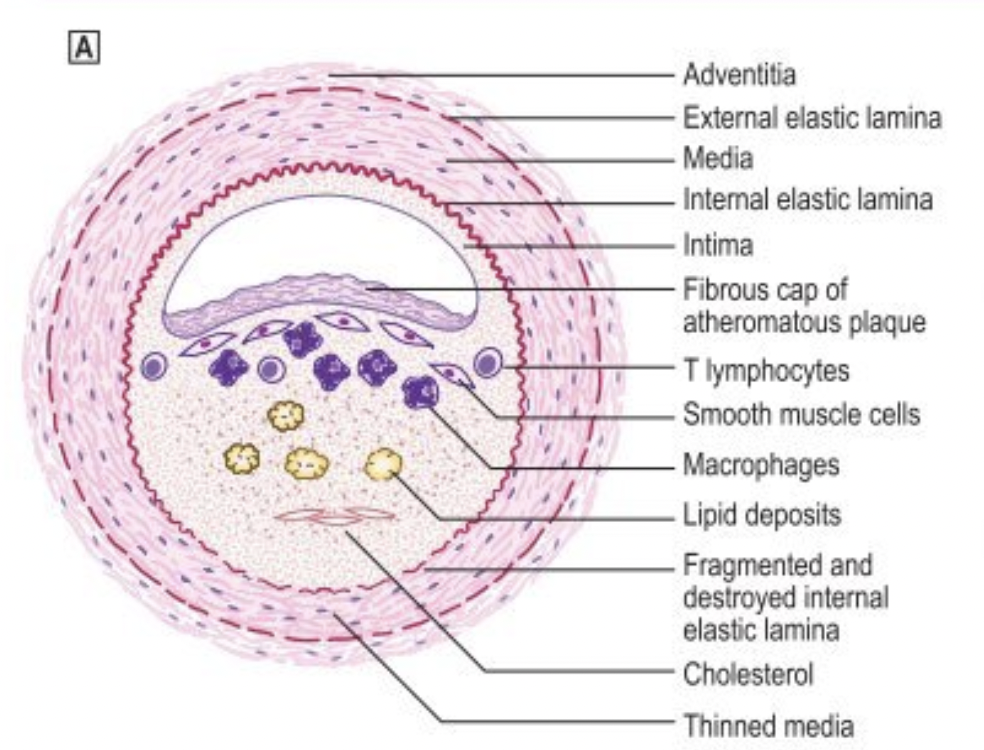
What is atherosclerosis?
disease of the arteries in which fatty plaques develop on their inner walls
62
New cards
Risk factors for atherosclerosis
- increasing age
- smoking
- unhealthy high fat diet
- sedentary lifestyle
- obese/overweight
- excessive alcohol use
- hypertension
- hypercholesterolemia (family or self)
- diabetes
- family history
- south asian, African, african-caribbean descent
- smoking
- unhealthy high fat diet
- sedentary lifestyle
- obese/overweight
- excessive alcohol use
- hypertension
- hypercholesterolemia (family or self)
- diabetes
- family history
- south asian, African, african-caribbean descent
63
New cards
Treatments for atherosclerosis
statins
antihypertensives
low-dose aspirin (reduce platelet aggregation medicines)
anti-platelet
surgery
antihypertensives
low-dose aspirin (reduce platelet aggregation medicines)
anti-platelet
surgery
64
New cards
What does an atheromatous plaque look like when fully developed?
a lesion with a lipid core and fibrous cap covered by arterial endothelium
65
New cards
what are the clinical manifestations of atherosclerosis?
1. progressive lumen narrowing causing ischemia eg. angina
2. acute atherothrombotic occlusion eg. plaque rupture
2. acute atherothrombotic occlusion eg. plaque rupture
66
New cards
What can detect DNA damage to trigger apoptosis?
p53 protein
67
New cards
Describe and explain the time course of atherosclerosis
birth - none
late teen/early 20s - fatty streaks
30s-50s established plaques
40s-80s complications of plaques
late teen/early 20s - fatty streaks
30s-50s established plaques
40s-80s complications of plaques
68
New cards
Why is there a limit on how many times a cell can divide?
Hayflick limit
At each cell division, the telomere region at the end of chromosomes shorten until its no longer possible to divide and replicate
cancer cells can produce telomerase enzymes thus maintain their telomere region and continue to divide
At each cell division, the telomere region at the end of chromosomes shorten until its no longer possible to divide and replicate
cancer cells can produce telomerase enzymes thus maintain their telomere region and continue to divide
69
New cards
What factors can cause damage to a cell for it to die?
- DNA mutation
- cross linking of proteins
- loss of control of calcium influx
- mitochondrial damage
- loss of DNA repair mechanisms
- time dependent activation genes
- telomere shortening
- accumulation of toxins (from metabolism)
- free radicals
- cross linking of proteins
- loss of control of calcium influx
- mitochondrial damage
- loss of DNA repair mechanisms
- time dependent activation genes
- telomere shortening
- accumulation of toxins (from metabolism)
- free radicals
70
New cards
What are the effects of ageing in skin?
wrinkling (dermal elastosis) from UV-B
71
New cards
How does age affect the eyes?
cataracts from UV-B
72
New cards
What are the effects of ageing on bone?
Osteoporosis - loss of bone matrix in women after menopause
73
New cards
What are the effects of ageing on the brain?
Dementia
74
New cards
How does age affect muscle?
Sarcopaenia (loss of muscle)
75
New cards
How does age affect hearing?
Deafness
hair cells do not divide so will die if damaged and not be replaced
hair cells do not divide so will die if damaged and not be replaced
76
New cards
What are the causes of acute inflammation?
- microbial infections
- hypersensitivity reactions
- physical agents (trauma, temperature)
- chemicals
- bacterial toxins
- tissue necrosis
- hypersensitivity reactions
- physical agents (trauma, temperature)
- chemicals
- bacterial toxins
- tissue necrosis
77
New cards
What is suppuration?
An outcome of acute inflammation. Pus is formed and leads to scarring
78
New cards
What are the causes of chronic inflammation?
Resistance of infective agent
Endogenous materials eg. necrotic tissue
Exogenous tissues eg. asbestos
Autoimmune conditions
granulomatous disease
transplant rejection
Endogenous materials eg. necrotic tissue
Exogenous tissues eg. asbestos
Autoimmune conditions
granulomatous disease
transplant rejection
79
New cards
neoplasm
A lesion resulting from autonomous abnormal growth of cells
80
New cards
Tumour
any abnormal swelling in or on a part of the body
81
New cards
Cancer
uncontrolled proliferation of cells that arise from virtually any cell type in the body
82
New cards
Carcinogenesis
The transformation of normal cells to neoplastic cells through permanent genetic alterations or mutations
83
New cards
What is angiogenesis?
The growth of new blood vessels
84
New cards
Define exophytic
growth outwards from an epithelial surface (characteristic of benign tumours)
85
New cards
What is meant by endophytic?
Growth inwards from an epithelial surface (characteristic of malignant)
86
New cards
What is meant by the term histogenesis?
the specific cell or origin of a tumour
87
New cards
What is the difference between oncogenic and carcinogenic?
oncogenic: tumour/neoplasm causing agent
carcinogenic: malignant neoplasm causing agent
carcinogenic: malignant neoplasm causing agent
88
New cards
What do tumours secrete for angiogenesis?
Vascular endothelial growth factor (VEGF)
89
New cards
A grade 2 cancer is...
moderately differentiated
cells look abnormal and grow faster than normal
cells look abnormal and grow faster than normal
90
New cards
If the cancer has grown in size, but not spread, what numerical classification would it be?
3
91
New cards
What is TNM cancer staging?
T - size 1-4
N - lymph nodes 0-3
M - metastases 0 or 1
N - lymph nodes 0-3
M - metastases 0 or 1
92
New cards
what are the features of a benign tumour?
- slow growing
- localised
- well defined capsule
- exophytic growth
- localised
- well defined capsule
- exophytic growth
93
New cards
what are the features of a malignant tumour?
- not contained
- cause angiogenesis
- cancerous
- rapid growth
- consists of different cell types
- endophytic
- ulceration
- cause angiogenesis
- cancerous
- rapid growth
- consists of different cell types
- endophytic
- ulceration
94
New cards
How is cancer graded?
1 well differentiated - cells resemble normal cells, not rapidly growing
2 moderately differentiated - look abnormal, grow faster than normal cells
3 poorly differentiated - look abnormal, grow/spreads aggressively
2 moderately differentiated - look abnormal, grow faster than normal cells
3 poorly differentiated - look abnormal, grow/spreads aggressively
95
New cards
numerical classification of cancer
0 - cancer in situ no spread
1 - cancer is small hasn’t spread elsewhere
2 - cancer has grown, no spread
3 - cancer is larger and may have spread to surrounding tissues/lymph nodes
1 - cancer is small hasn’t spread elsewhere
2 - cancer has grown, no spread
3 - cancer is larger and may have spread to surrounding tissues/lymph nodes
96
New cards
What 5 types of cancer can spread to bone?
Breast
Lung
Thyroid
Kidney
Prostate
(BLT KP)
Lung
Thyroid
Kidney
Prostate
(BLT KP)
97
New cards
How can benign tumours cause clinical issues?
pressure on structures
obstruction
hormone production
anxiety & stress
obstruction
hormone production
anxiety & stress
98
New cards
How do tumours spread?
1. hematogenous spread (blood)
2. lymphatic system
3. transcoelomic (into body cavities through peritoneal, pleural, pericardial, subarachnoid)
2. lymphatic system
3. transcoelomic (into body cavities through peritoneal, pleural, pericardial, subarachnoid)
99
New cards
What are the exceptions to usual tumour nomenclature?
Hepatoma/hepatocellular carcinoma
Melanoma (malignant from melanocytes)
Mesothelioma (malignant of mesothelial cells)
Melanoma (malignant from melanocytes)
Mesothelioma (malignant of mesothelial cells)
100
New cards
malignant tumour of adipocytes
liposarcoma