ETC8363-2020 BCCCP-Acute Cardiac Care
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
114 Terms
What is the new chain of survival?
CAB
Chest compressions
Airway
Breathing.
Why are chest compressions so important?
Provide intrathoracic pressure and direct compressions to heart leading to perfusion and oxygenation to brain and myocardium.
What is the rate of chest compressions?
Depth?
100-120 compressions per min.
2-2.4 inches (and allow recoil)
How often should people giving chest compressions switch?
(keep switch < 10 seconds)
q 2 min or
after 5 cycles of 30 compressions : 2 ventilations.
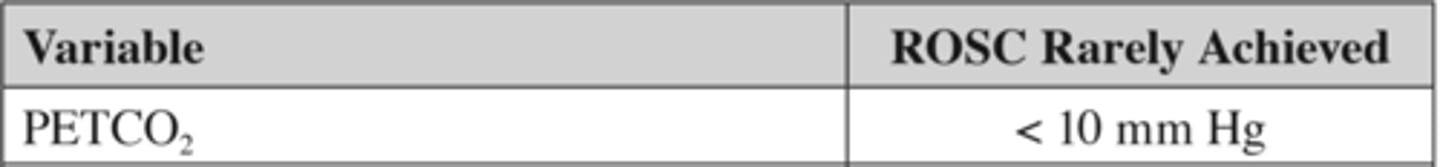
ROSC is RARELY achieved when PETCO2 is?
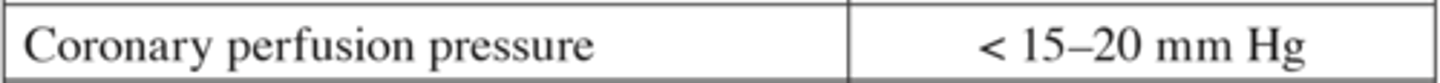
ROSC is RARELY achieved when Coronary Perfusion Pressure is?
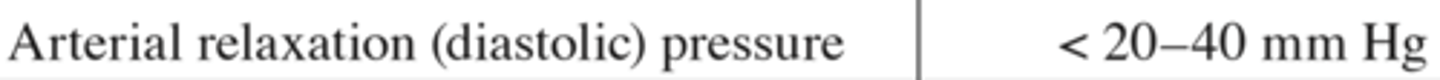
ROSC is RARELY achieved when Arterial Relaxation (Diastolic) Pressure is?
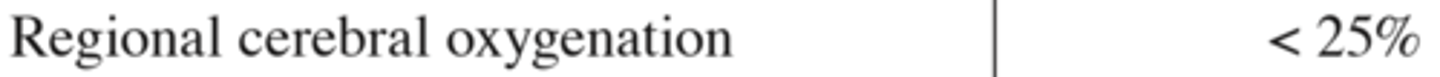
ROSC is RARELY achieved when Regional Cerebral Oxygenation is?
ROSC is RARELY achieved when Scvo2 is?
What is Cricoid Pressure?
technique of applying pressure to the victims cricoid cartilage to push trachea posteriorly and compress esophagus to prevent aspiration.

True or False:
You should perform abdominal thrusts to people who have any type of foreign body airway obstruction (FBAO)
No, if the patient is coughing then it is considered a MILD FBAO hence they may clear it by themselves.
If you ask them if they are choking and grasp their throat, cough silently, have stridor, or resp diff. then its a SEVERE FBAO then you would give abdominal thrusts.
During SEVERE FBAO a person goes unresponsive. What should be done?
Place person on floor and begin CPR.
Chest compressions actually provide greater airway pressure to dislodge substance. before giving ventilation check mouth for object.
True/False:
You can finger sweep a person if they have SEVERE FBAO?
No, if the object is not visible do not finger sweep
Why are rescue breaths important? what is their purpose?
maintain oxygenation and remove carbon dioxide
During a code how many breaths per minute are being given?
1 breath q 5-6 seconds (10-12 breaths/min) until advanced airway is placed.
what is the rate of chest compressions to breaths/ventilation?
provide the 30:2 compression-to-ventilation ratio
After advanced airway is placed then switch over to 1 ventilation q 5-6 seconds (10-12 breaths / min)
What is more damaging low minute ventilation or excessive ventilation?
Low min vent: can maintain oxyenation due to reduced CO
Excessive Vent: causes gastric inflation, aspiration, regurgitation, decreased survival.
True/False:
Anytime there is a bagmask available use it to prevent transmission of illness?
FALSE, single healthcare CPR should NEVER use bag mask to give breaths. always do mouth-mouth or mouth to barrier.
for single layperson CPR: hands-only CPR is recommended.
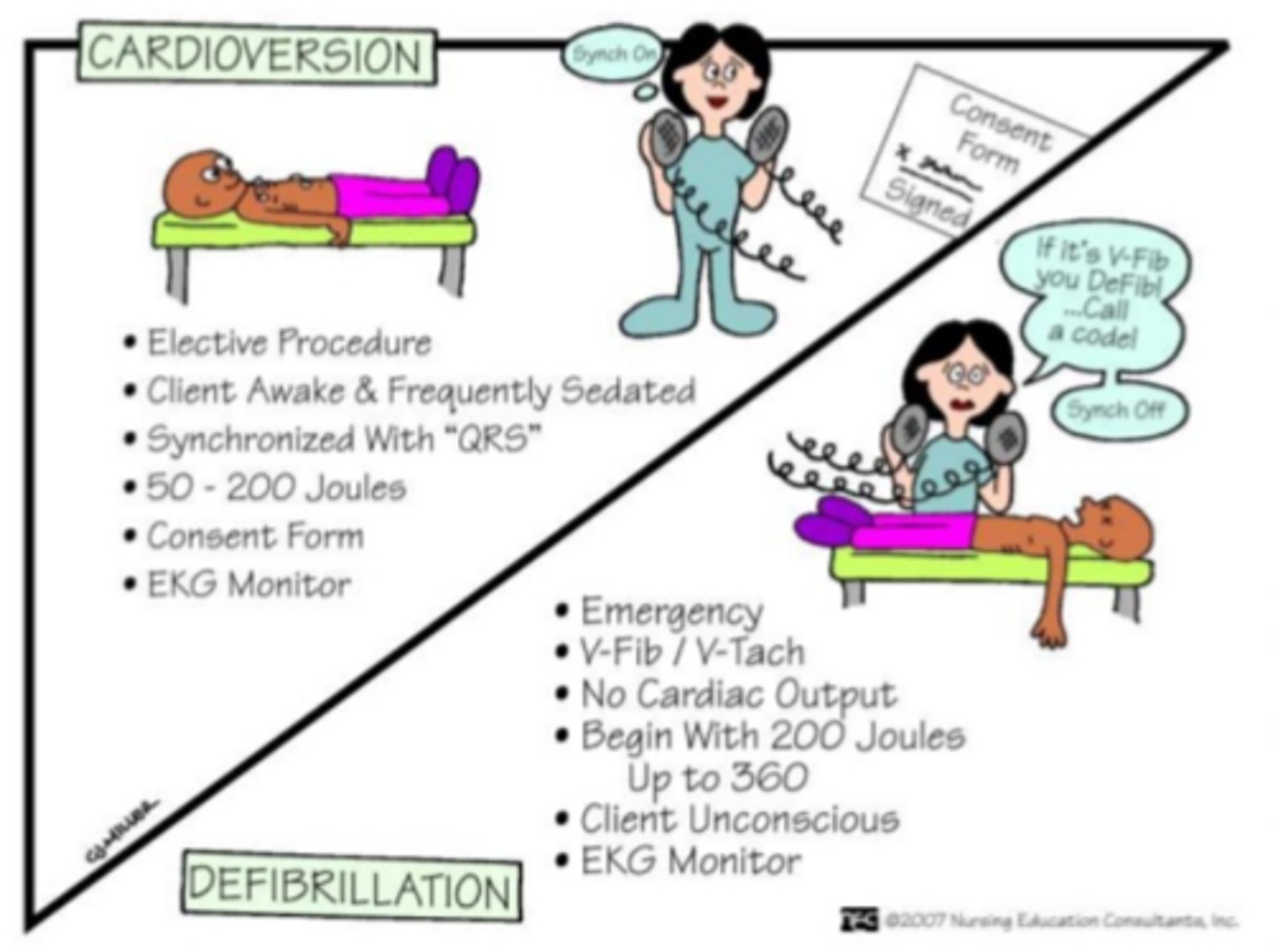
what is the definition of a SUCCESSFUL defibrillaton?
termination of arrhythmia >5 seconds after shock is delivered.
What is the most common rhythm in WITNESSED out-of-hosp sudden cardiac arrest (SCA)?
Why is that important?
Ventricular Fibrillation.
Early defibrillation of VF is crucial because survival diminishes rapidly over time. VF most commonly progresses to asystole.
What 3 things must happen within moments of VF SCA to increase the likelihood of survival?
1. Activate EMS ( emergency medical services)
2. CPR
3. Shock delivery (TX of CHOICE in VF)
((This was asked several times. ))
How are pacing, defibrillation, and cardioversion different?
pacing is for symptomatic bradycardia/arrythmias.
True or false:
Chest compression should stop while defibrillator is being obtained?
FALSE:
chest compression done while defibrillator is obtained SIGNIFICANTLY improves survival
What happens to the heart when VF is present for more than a few minutes?
How does that affect CPR ?
Myocardium is depleted of oxygen and energy substrates (ATP)
CPR: oxygenates and provides ATP until shock is delivered. CPR also PROLONGS/delays VF from progressing into asystole.
When are survival rates the highest in regards to VF, Shock, CPR, and onset of arrest?
VF Survival rates are highest when CPR + early defibrillation occur within 3-5 min of arrest.
What is the recommended Biphasic defibrillator joules for VF cardiac arrest?
200 J or manufacturers recommendations which is also ~200J
What is the correlation between min after arrest vs % survival
For every 1 minute after collapse = survival DECREASES 7-10%.
What is the optimal biphasic shock energy?
Has not been determined. Between 120-200J.
if repeat shock warranted begin at last Joule and increase.
In OUT-of-Hospital what is the best time from from collapse to intubation for better odds of survival?
Intubation within 13 min is associated with better survival
What is the most reliable and objective way to ensure, confirm, and monitor correct endotracheal tube placement?
Clinical and objective measures. (physical assessment of chest and epigastrium)
End-tidal CO2 detector
Continuous waveform capnography
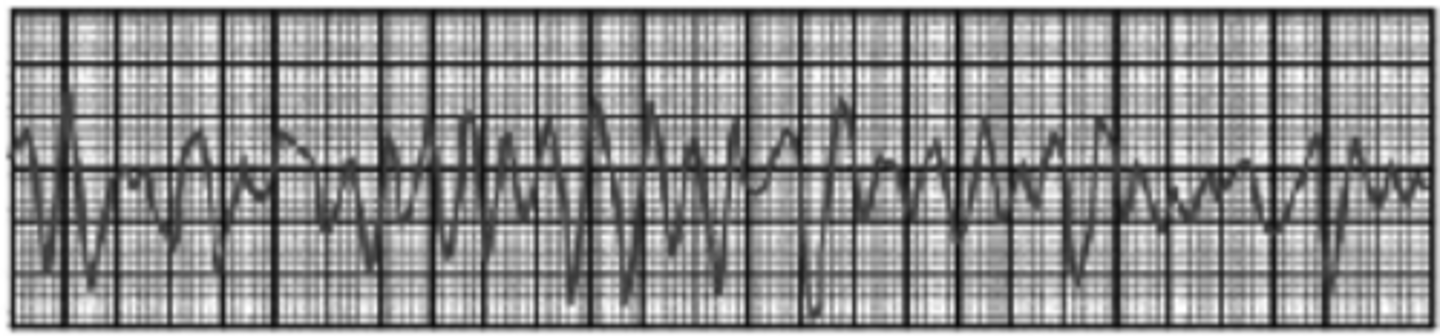
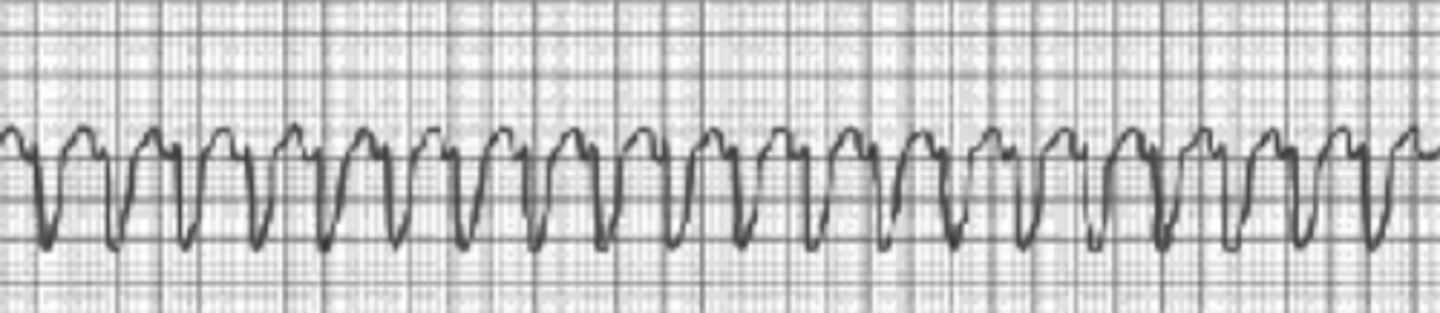
Classify VF, asystole, PEA, and Pulseless VT as either
Shockable or Non-Shockable
Shockable: VF pVT
Non-Shockable: Asystole PEA
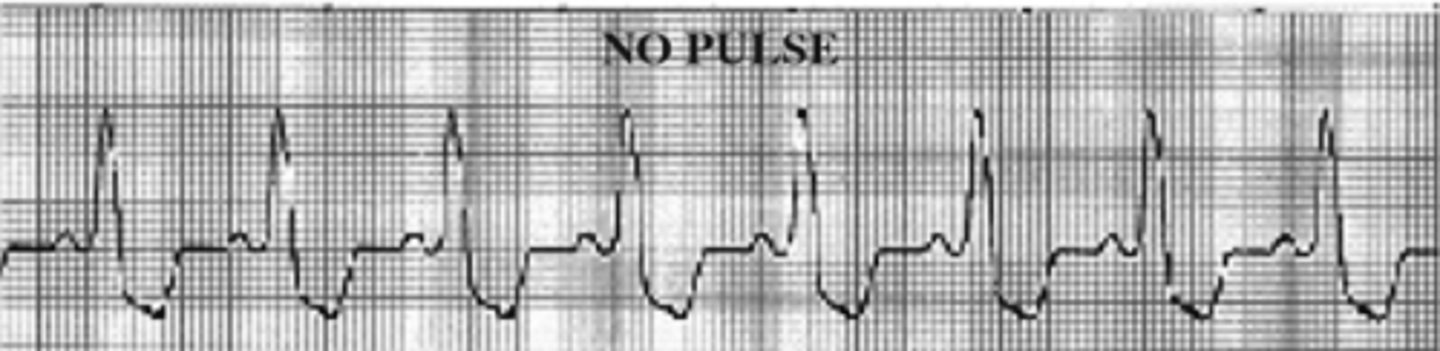
VF EKG
pVT EKG
PEA EKG
What is the ONLY therapy that increases the rate of ROSC or survival to hospital discharge?
Defibrillation ONLY IN VF and pVT.
Medication only increase rate of ROSC and hospital admission.
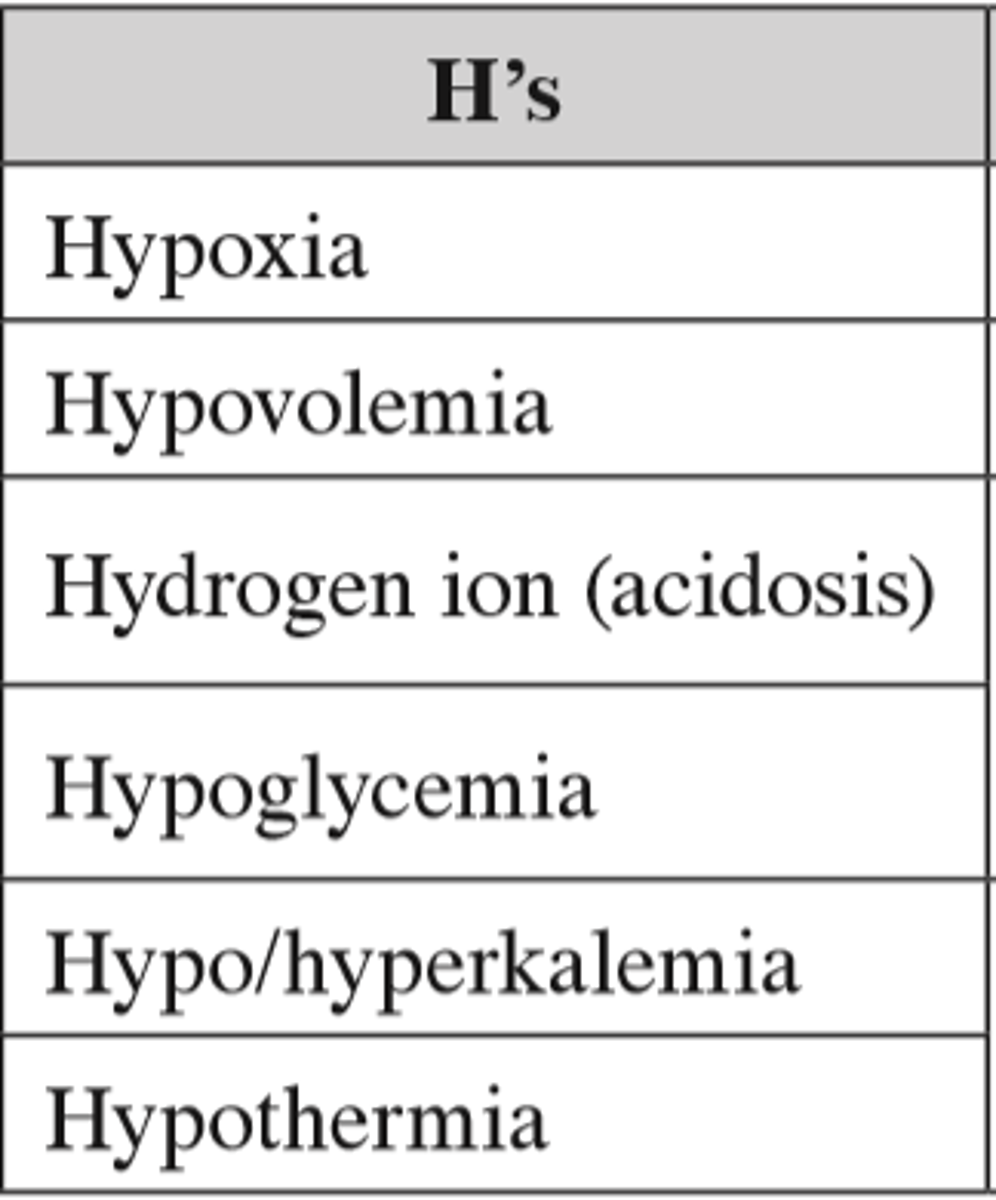
What are the H's in regards to treatable causes of arrest H's & T's
Hypoxia/ volemia/ glycemia/thermia
hypo/hyper-kalemia
Hydrogen ions ( acidosis)
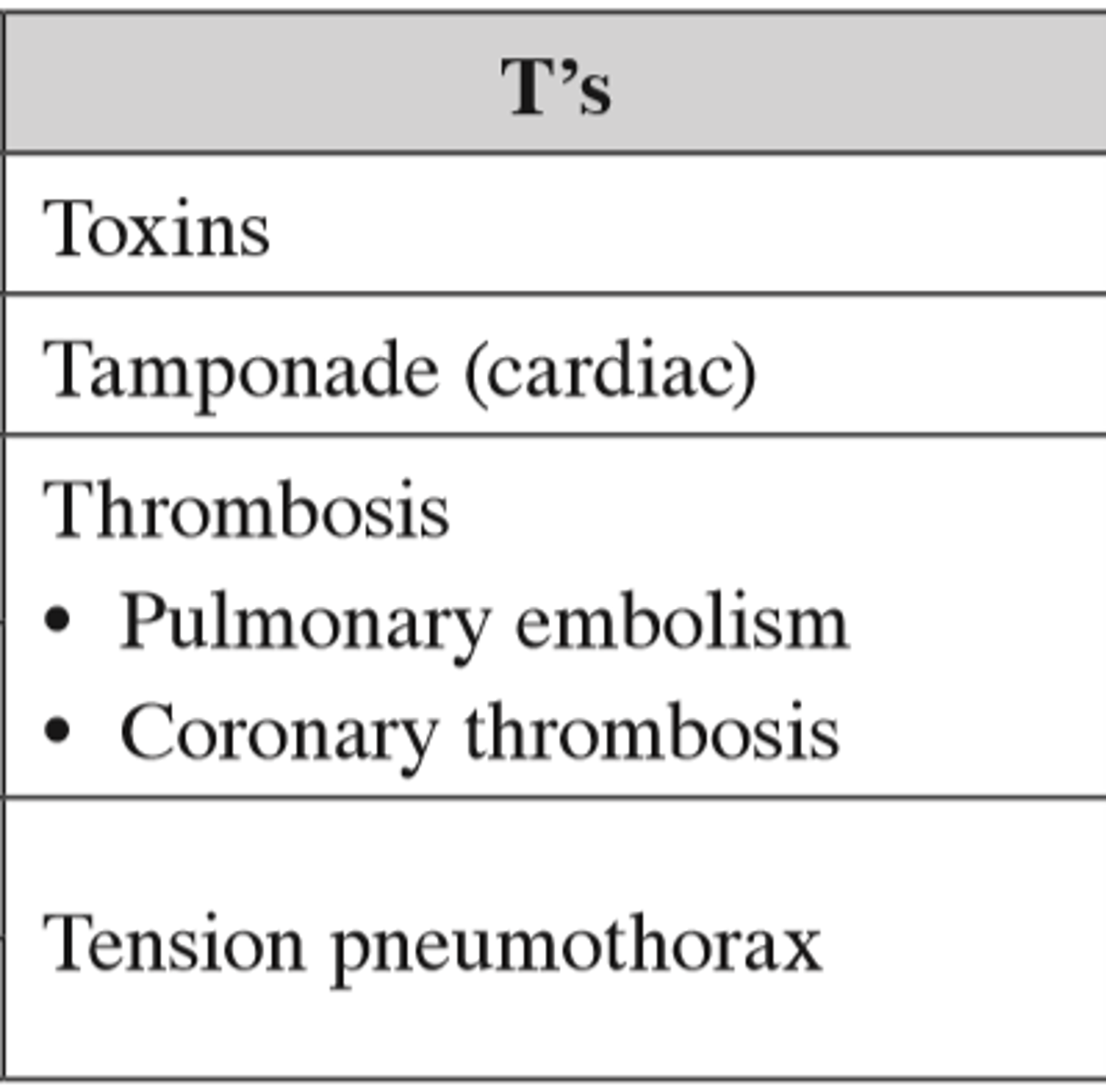
What are the T's in regards to treatable causes of arrest H's & T's
What medications can be given via the endotracheal tube?
Naloxone
Atropine (removed from VF algorithm for PEA/asystole)
Vasopressin
Epinephrine
Lidocaine
True of False:
When the AED alerts "CHARGING" everyone should stop compressions and step back?
False: When AED is charging compressions should still be done up until the shock is going to be delivered. This is because compressions deliver oxygen to heart and unloads ventricles which both increases likelihood of a perfusing rhythm will return after shock.
True or false:
Anti-arrhythmics increase survival to discharge?
False:
NO evidence that anti-arrythmics increase survival to discharge.
When is amiodarone given? (where does it fall in the timing of therapy? )
CONSIDERED for "Refractory" VF/ pVT
(unresponsive to 3 shocks, CPR, and vasopressor)
What is the dose of Amiodarone?
Pulseless: 300mg IV Push
Pulse obtained: 150mg IVPB over 15min.
(over 15min if pulse is present because of polysorbate 80 and benzyl alcohol solvents in amiodarone may cause bradycardia and hypotension)
When is Lidocaine given?
for defibrillator refractory VF/pVT ONLY when amiodarone is on back order or cannot be obtained.
What is the dose of Magnesium to terminate Torsades de Pointes?
Magnesium 1-2g in 10ml of D5% or sterile water IV/IO only one dose.
What is the main treatment for PEA/Asystole
CPR, epi, and treating reversible causes
Mainstay treatment: high quality CPR & reverse causes.
Epi should be given ASAP (stepwise increase mortality if epi withheld > 4 min in asystole/PEA)
Why is central administration better than peripheral IVs, IO, or via endotracheal tube administrations?
Central administration of meds result in....
Higher peaks/concentration of medications
faster onset
standardized dosing
ease of use (when compared to IO or ET)
Often what is a cause of PEA arrest?
Hypoxia, hence in PEA placement of airway and oxygen delivery should be of utmost importance.
But this is not true for ALL arrests. a large proportion of adult cardiac arrests are caused by CARDIOVASCULAR not respiratory events. If pt on room air/nasal canula and suddenly loses pulse then it wasn't due to hypoxia. moreso CV arrest.
True/False:
During cardiac arrest using sodium bicarb is the mainstay treatment to restore acid/base status?
False: to restore acid/base status HIGH quality chest compressions and ventilation/oxygenation are best practice.
Sodium bicarb shows no benefit or poor outcome when used. if not needed may actually inactivate epi.
When is Sodium Bicarb useful?
TCA OD
Bicarb Wasting illnesses causing metabolic acidosis
Hyperkalemia
When using catecholamines in a pt with acidosis.
(acidosis blunts catecholamine response)
When is calcium used during a code?
Not really well studies but you can use if the pt exhibits tetany or seizures.
When is dextorse used during a code?
only if they are hypoglycemic. Other than that dextrose has been shown to cause higher rates of mortality and worsen neurological outcomes.
Describe the post-cardiac arrest care- INITIAL
1. Optimize Hemodynamics:
MAP: 65-100, CVP: 8-12, SCVo2: > 70%, UO: >1/kg/hr, and normal lactate level.
2. Transfer pt to unit that provides ECG, TTM
3. ID and treat reversible causes.
Who is a candidate for Target Temperature Management (TTM)?
ANY pt with ROSC who does not follow commands (comatose) after cardiac arrest
application can be made to all pts with cardiac arrest INDEPENDENT of rhythm.
Why would we want to put someone into TTM?
TTM improves neurologic recovery in pts after cardiac arrest. (guideline recommended, good studies to back up)
Best results happen when TTM is done within 2 hrs of ROSC but can also be done up to 8 hrs after arrest.
True/False:
when putting someone into TTM, 33C is better than 36C?
33C vs 36C have shown no difference regarding outcomes between both temperatures.
TTM, what is the temp we aim for?
Duration of TTM?
33-36*C (moreso to the 36*C side)
At least 12 hrs, (optimally minimum of 24 hrs)
True/false:
You can use a oral or axillary thermometer to gauge a TTM pt?
False, temperature needs to be from central/core via esophageal, bladder, or pulmonary route.
What confers poor neurological outcome if present within 72hrs of TTM?
Sepsis
Myoclonus
Seizures
Hypoglycemia
what is the most common complication of hypothermia and why?
when does it occur ?
what do we do about it?
Shivering, can increase metabolic heat production by 600%.
Normally without meds shivering stops at temp < 33.5*C.
We give medication to decrease shivering threshold.
What do we give for shivering?
APAP 650mg q4-6hrs4
Buspirone 30mg q12hrs
Clonidine
Magnesium sulfate
Meperidine !! possible seizures in decreased GFR!!
Precedex/ Propofol / Paralytics
When a pt is under TTM (target therapy management) what is the most reliable monitoring method?
Clinical monitoring or Continuous EEG.
NOT TRAIN OF 4s
aside from neurological also renal function should be closely monitored with Sr concentrations.
Neurologically what do we need to look out for in pts undergoing TTM?
Sedation / Analgesia (RASS of -3 to -5)
Seizures ( Benzos, Phenytoin, Barbs, Valproic, Propofol
ICP ( if due to ROSC= TTM attenuates ICP but major increase in ICP may happen when rewarming. )
Cardiac complications during TTM?
Arrhythmias: VF/VT/Afib. ( life threatening= start rewarming, but slight brady is normal)
ECG observation: PR, QRS, QT prolongation
Hemodynamics: Dec CO and fluid shifts
Is a pt more likely to have HYPER or HYPO-glycemia in TTM?
What is the goal in TTM?
HYPERglycemia because cold temperatures decrease insulin production. Hence, BG rises.
Insulin drip might be needed to maintain BG<180
Renally what do we look out for in pts in TTM?
Decreased renal blood flow (urine output may increase at the beginning due to cold diuresis but not true UP)
Electrolyte shifts (K, PO4, Na, Ca) but all revert back to normal upon rewarming so be careful when correcting.
True or false:
TTM causes hyper coagulability?
No the opposite, pt is more prone to bleeding.
the cold temperature does not allow coagulation factors to work properly (or platelet function) hence ACTIVELY bleeding pts should not be cooled.
How long does the rewarming phase take?
how many *C should be increased per hr?
takes 8 hrs
0.3-0.5*C increase / hr.
What is the goal PaCO2 and PetCO2 for pts under TTM?
PaCO2 si 40-45mmHg
partial pressure of carbon dioxide
PetCO2= 35-40 mmHg
Postapneic End-Tidal Carbon Dioxide
Dose for Epi/ Norepi and the difference?
0.03-0.3 mcg/kg/min
Both alpha and beta but norepi more alpha
Epi used for symptomatic bradycardia (since it has more B1 activity than norepi)
Norepi used more in volume-resuscitated pts.
Norepi 1st line for septic shock.
Phenylephrine dose and when is it used?
0.3- 3 mcg/kg/min
(pure alpha agonist)
used in volume resuscitated pts
AVOID in low CO
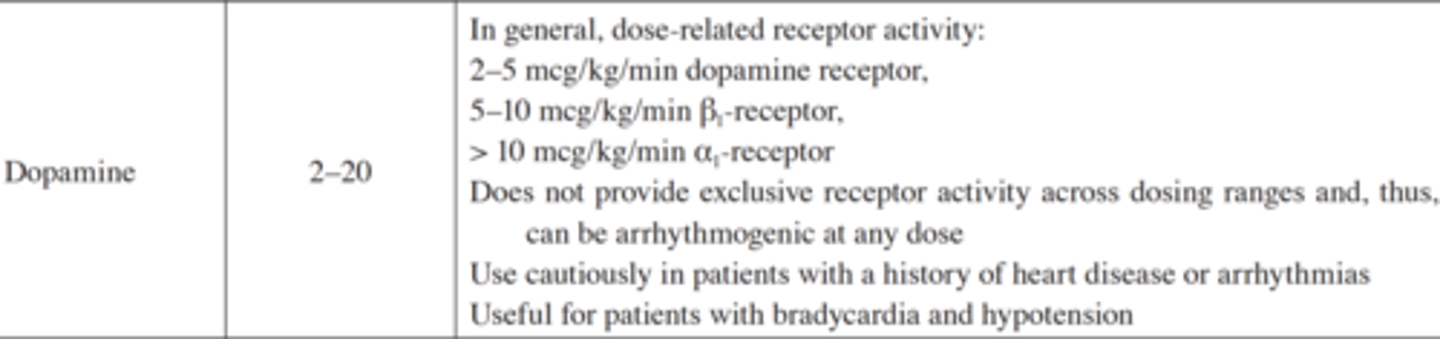
Dopamine dosing?
2-5 hits dopamine receptors
5-10 Beta receptors
>10 Alpha receptors
Mostly for bradycardia and hypotensive pts
(may cause arrhythmias use caution in these pts.)
Dobutamine dosing?
used for low CO at dose of 2-20 mcg/kg/min
more tachycardia (than milrinone)
less systemic & pulmonary vasodilation (than milrinone)
Dopamine/dobutamine/milrinone= caution in arrythmias
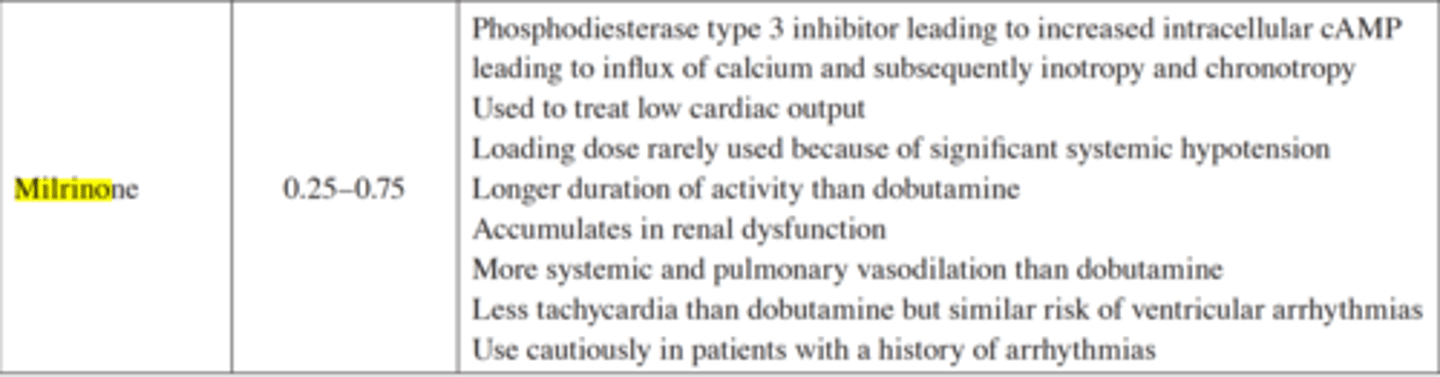
Milrinone dosing
0.25-0.75 mcg/kg/min ( lasts longer than dobutamine)
for iono/chronotropy
treats low CO
bad to give in renal dysfunction
Less tachy than dobutamine. but more systemic/pulmonary vasodilation.
Dopamine/dobutamine/milrinone= caution in arrythmias
What is the glucose range we aim for in TTM?
144-180 mg/dL
True or false :
Prognostication can be made at any time when pt is under TTM?
False, prognostication must be delayed 72 hrs after rewarming ( or 72 hrs after ROSC)
What is the difference between hypertensive URGENCY vs Emergency?
Urgency:
SBP > 180Hg or DBP >110mmHg + NO organ dysfunction.
Emergency:
SBP > 200mmHg or DBP > 120mmHg + organ damage ( kidney, HF exa, obtundation, LIVER ENZYME INCREASE and changes in vision)
What is the formula for MAP?
Average pressure in arteries during one cardiac cycle.
MAP= 1/3 SBP + 2/3 DBP
How do you treat hypertensive urgency?
Lower BP within 24-48hrs using ORAL medications
(does not require ICU stay)
How do you treat hypertensive EMERGENCY?
Admit to ICU and give IV medications (nitroprusside) to a goal of .....
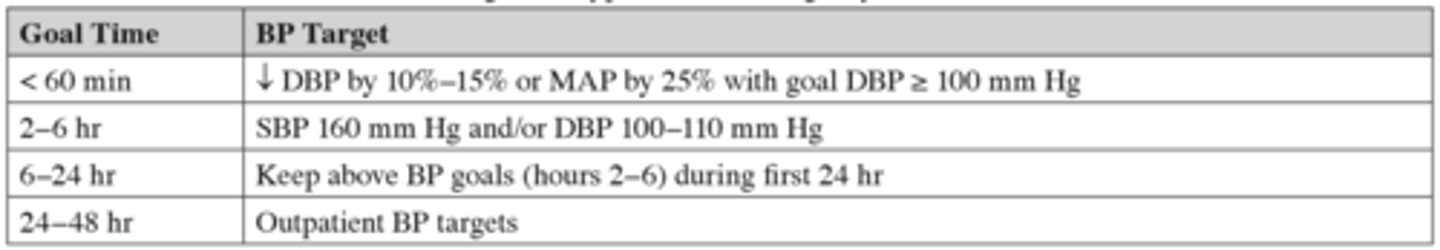
Why do we target 25% decrease in MAP within the 1st hour in hypertensive EMERGENCY?
We only want 25% decrease in MAP within first 60 min because we want to maintain cerebral perfusion (blood flow autoregulation).
Anything more than 25% will induce ischemia due to lack of cerebral perfusion.
In what situations/diseases do we need to follow a set % decrease in MAP or BP according to their severity?
Acute Aortic Dissection:
Goal HR < 60 & SBP < 100 mmHg ASAP!!! ( 5-10 min)
Hypertensive EMERGENCY: MAP decrease by 25% within 1 hr.
Acute Ischemic Stroke: the goal is to reduce MAP by
10-20% over 24hrs.
Intracerebral Hemorrhage: parameters depend on pt.
What is the formula for Cerebral Perfusion Pressure (CPP)?
CPP= MAP - ICP
True or false:
Initial Blood Pressure measurement does not matter when dealing with a pt who has Intracranial hemorrhage?
FALSE: Higher blood pressure + Intracranial hemorrhage = worse outcomes
(hematoma expansion, neurological deterioration, death, or inability to perform activities of daily living after hemorrhage)
If a pt has an Intracerebral Hemorrhage but NO ICP what is out goal SBP?
BP reductions in pts WITHOUT ICP goal SBP is < 140mmHg-160mmHg have been shown benefit regarding functional recovery.
In pts WITH intracerebral hemorrhage with extreme elevations in BP ( > 220mmHg) , or large Hematomas, or those with elevated ICP what is the recommended level of therapy?
What are the parameters (SBP, MAP, and time frame)
Aggressive MAY be considered but the MODEST reduction is recommended.
SBP< 180mmHg or MAP < 130mmHg over 24hrs.
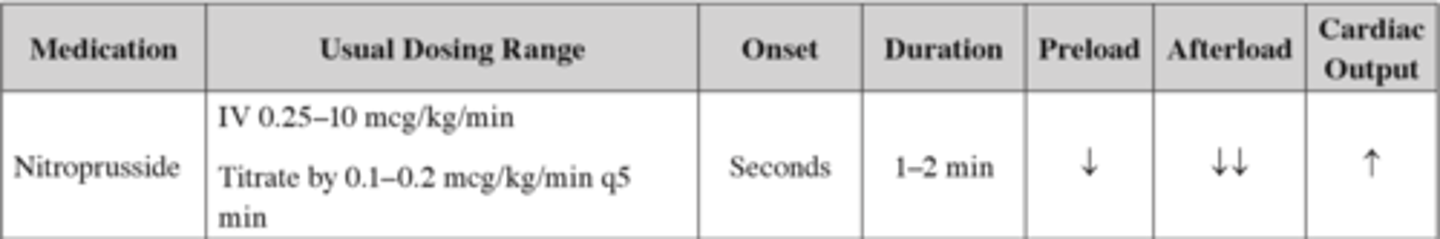
What is the drug of choice for a hypertensive EMERgency
Nitroprusside.
works rapid and does not need to be adjusted for renal or hepatic deficiencies.
Who do you not use Nitroprusside in?
Pts who......
do not have an Arterial line
Have ICP ( may cause coronary steal)
Have Myocardial Ischemia/Infarction.
Nitroprusside (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
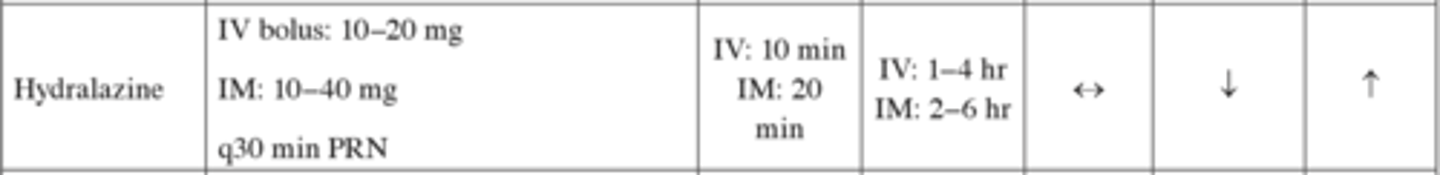
Hydralazine (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
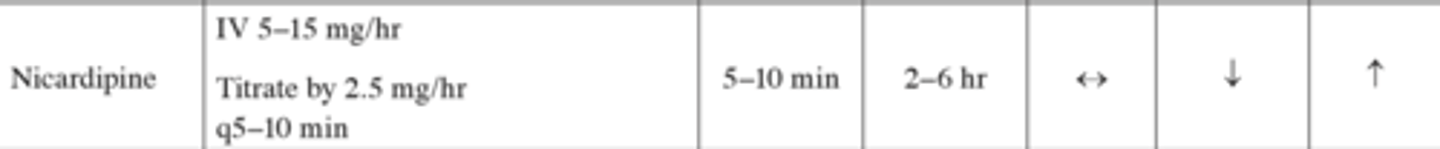
Nicardipine (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
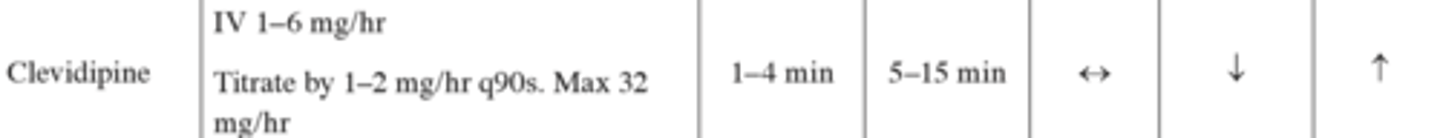
Clevidipine (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
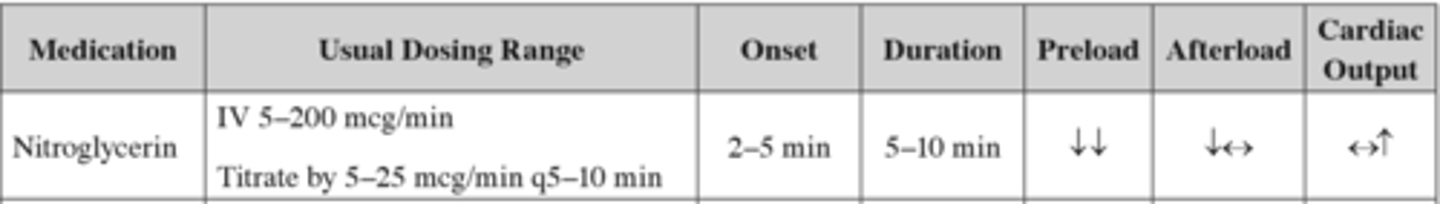
Nitroglycerin (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
Esmolol (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects

Metoprolol (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects

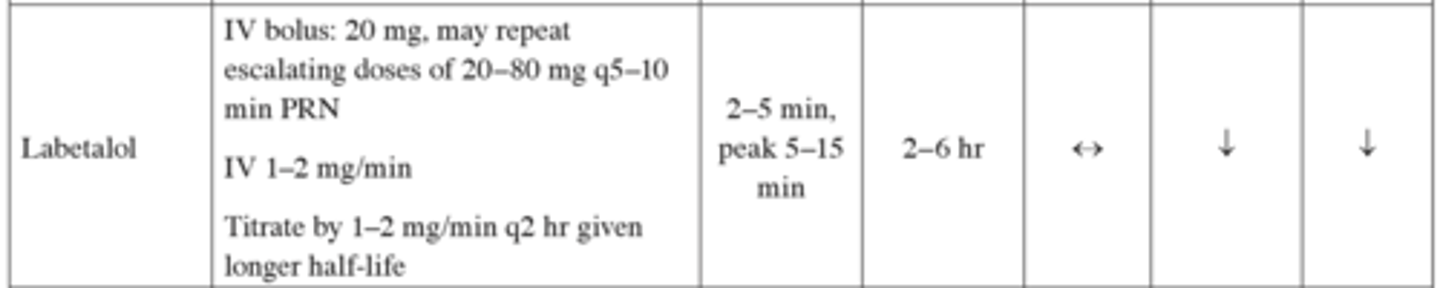
Labetalol(for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
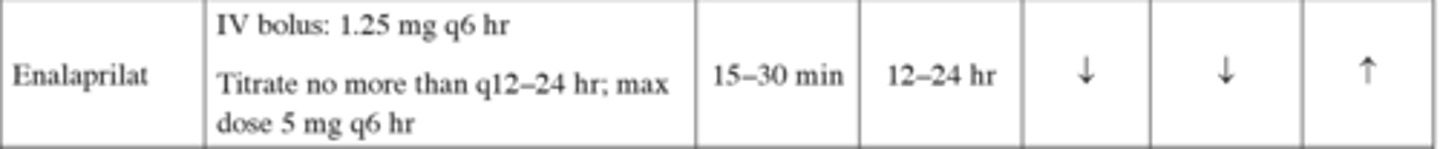
Enalaprilant (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
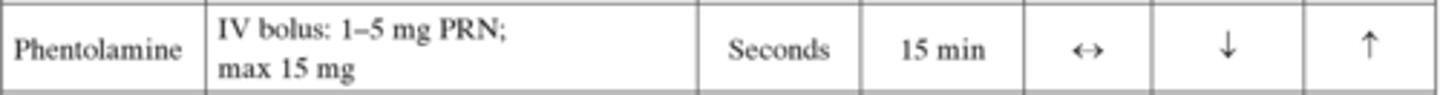
Phentolamine (for hypertensive EMERgencies)
Indication?
Dose
Onset
Duration
Preload/Afterload/CO effects
Use in catecholamine-induced hypertensive emergency
(pheochromocytoma)
competitively inhibits α-adrenergic receptors.
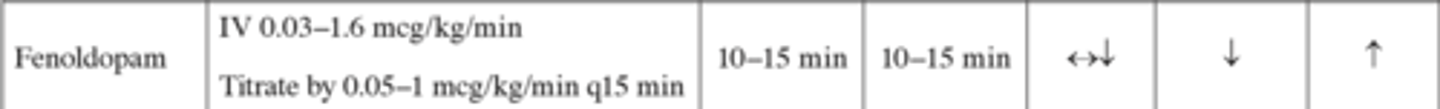
Fenoldopam (for hypertensive EMERgencies)
Dose
Onset
Duration
Preload/Afterload/CO effects
Special Considerations using Nitroprusside?
cyanide and thiocyanate poisoning if on drip for > 72 hrs or running drip at >3mcg/kg/min.
Accumulation can be worse in liver/kidney insufficiency but we still give due to emergency
Can still be given despite the above for first 24hrs, since the benefit of reducing BP outweighs risk of poisoning.
Special Considerations using hydralazine?
Indicated for pregnant pts.
may cause prolonged hypotension
reflex tachy
lupus-like syndrome.