NURS 3083 Pharmacology Final
1/146
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
147 Terms
Pharmacokinetics (ADME) is the impact of the body on the drug and pharmacodynamis is the impact of the drug on the body. What does ADME stand for?
The four major pharmacokinetic processes are
1.Drug absorption – IV drugs bypass this!
2.Drug distribution
3.Drug metabolism
Drug excretion- Kidneys & Intestines
When describing pharmacodynamics, we look at selectivity, onset, peak, duration, & trough. State the meaning of Peak & Trough?
Peak
The time it takes for a drug to reach its maximum therapeutic response
Trough
Lowest Blood level
What oral prep provides the fastest absorption?
Liquid, Elixers, & Syrups
When giving medications to newborns, state 2 challenges that must be considered in respect to ADME?
In comparing pharmacokinetics of elderly and pediatrics, elderly organ are degenerating & peds organs are immature leading to similar problems.
Absorption – Variable depending on surface.
Distribution – dec. due to dec. albumin levels.
Metabolism – dec. Hepatic function low.
Excretion – dec. Renal reduced
The ADME effects during Pregnancy are Absorption & Distribution (GI) motility dec. = prolonged transit & inc. absorption of med, Metabolism- increased, Excretion – Renal blood flow doubles (Inc. GFR) = leading to what type of changes in medication dosing?
increased dosing
Describe ADME in relation to the Elderly?
Absorption – Gastric Ph less acidic or increased
Distribution – less body water, inc. Fat content & protein binding sites reduced.
Metabolism – Liver blood flow dec. & dec. production of protein.
Excretion – GFR dec. & the # of intact nephrons are dec.
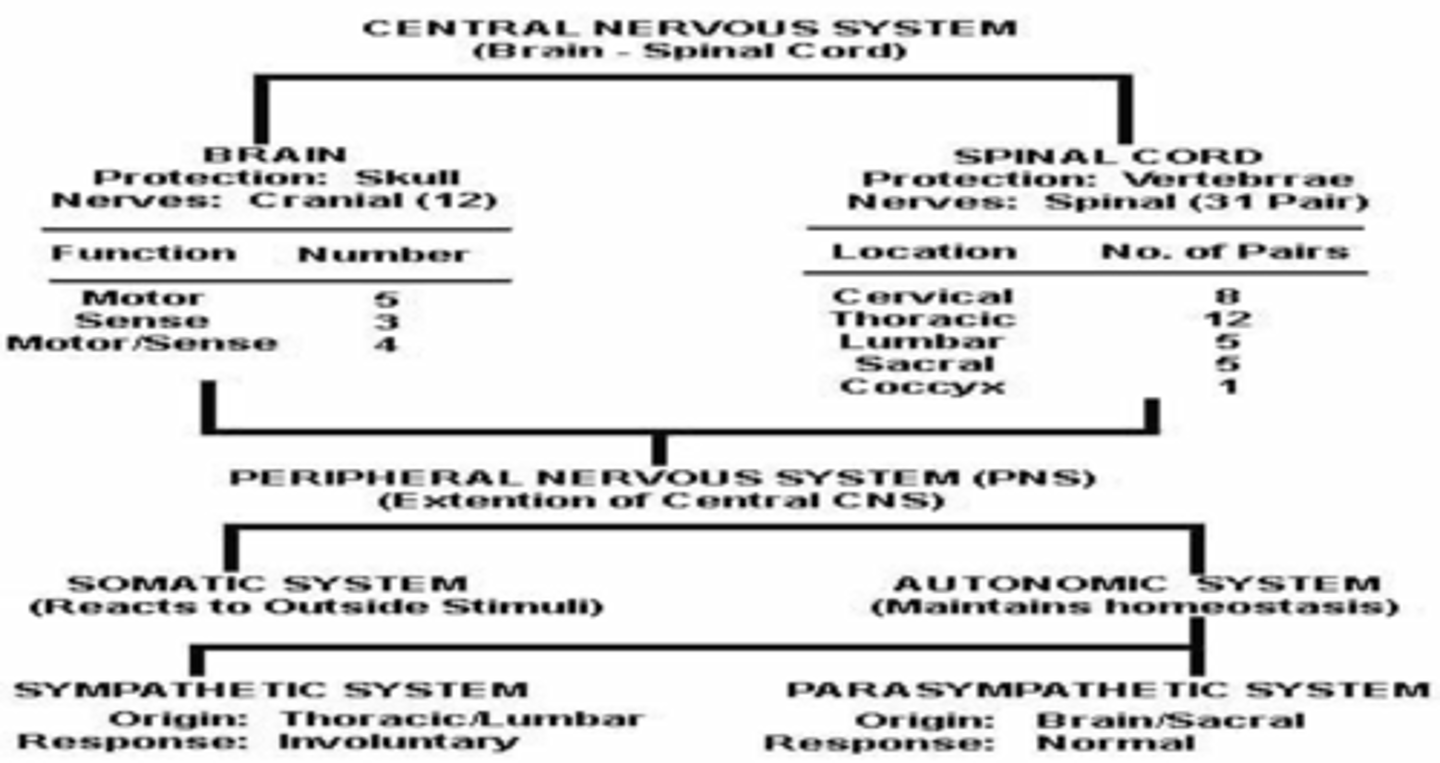
Sympathetic & Parasympathetic Nervous System.
CNS: Parkinson’s disease is a neurodegenerative disorder of the extrapyramidal system disrupting the regulation of voluntary movements. The treatment goal is increased control of voluntary movement, what is the treatment med of choice?
Levodopa + Carbidopa *only lipid soluble agents cross the BBB & it may take months to see a response to treatment.
Review on/off phenomenon, Drug Holiday, & Adverse effects: N/V, postural hypotension
What is on/off phenomenon?
tx wears off & motor symptoms return before its time for the next dose
What is a Drug Holiday?
10 days stop medication - under supervision in the hospital
What are the AE of Levadopa-Carbidopa?
N/V, postural hypotension
Dilantin (Phenytoin) is an antiepileptic agent used for partial and tonic-clonic seizures. The adverse effects are Nystagmus, sedation, Ataxia, & GINGival hyperplasia. What are the therapeutic and toxic drug levels?
Therapeutic 10-20 mcg/ml & Toxic – 30-50 mcg/ml.
*Never stop any of these drugs abruptly, they must be weaned
On the WHO analgesic ladder for pain treatment, Step 1 is mild pain with nonopiods such as NSAIDS & Tylenol, Step 2 mild to moderate pain add opioid such as oxycodone & hydrocodone, Step 3 moderate to severe pain add morphine or fentanyl + adjuvant (amitriptyline). Name 2 S/E’s of Morphine and the antagonists for overdose?
Resp. depression, *Coma,* Pinpoint pupils, *Constipation, * Hypotension. Overdose= Naloxone (Narcan)
Remember Opiods are more effective on a fixed schedule.*
What pain medications are most effective on a fixed schedule?
Opioids
Under treatment of pain is a major concern – the goal should be to have a pain level reduced to a level agreed upon by both the patient and provider. Using the acronym A,B,C,D,E state the pain management strategy?
ASK about pain regularly
–Assess pain systematically
•BELIEVE the patient and family in their reports of pain and what relieves it
•CHOOSE pain control options appropriate for the patient, family, and setting
•DELIVER interventions in a timely, logical, coordinated fashion
•EMPOWER patients and their families
–Enable patients to control their treatment to the greatest extent possible
Calcium Channel Blockers are (Very Nice Drugs) Verapamil (Calan) (constipation), Amlodipine (Norvasc) (flushing & reflex tachycardia), & Diltiazem – (constipation, flushing, & Heart block). They promote vasodilation by preventing Calcium ions from entering the cells. What are they used to treat – Name 1?
Angina pectoris, HTN, & Cardiac dysrhythmias (A-Fib, A-flutter, & SVT)
Angiotensin-Converting Enzyme (ACE) Inhibitors – reduce levels of Angiotensin II & increase levels of bradykinin, they are used to treat HTN, Heart failure, MI, & DM nephropathy. State 2 side effects?
*1st dose hypotension, *Cough, *HA, *Hyperkalemia (use cautiously with K+ sparing diuretics), & *Angioedema – edema of tongue, glottis, & pharynx.
*Prils *Review ARB’s mechanism of action???
What is ARB's mechanism of action?
block action on angiotensin II (block the vasoconstriction effects)
Hypertension is preferred to be treated with lifestyle changes 1st but what is the #1 medical regimen (2 classes)?
Thiazide diuretics (HCTZ) & Beta Blocker (propanolol – Inderal)
*Less effective in african americans, give carefully in asthmatics, & always check a pulse prior.
What HTN medication should be given with caution to DM patients and why?
Propranolol because it may mask signs of hypoglycemia
Vasodilator used for its selective dilationof arterioles, used to treat essential HTN & HTN crisis, with the side effect of reflex tachycardia & the rare S/E of Systemic Lupus Erythematosus (LUPUS
Hydralazine (Apresoline)
*Sodium Nitroprusside (Nitropress) fastest acting - used for HTN emergencies. S/E:Hypotension & Cyanide poisoning.
Digoxin (Lanoxin) is a cardiac glycoside which has a positive inotropic action on heart therefore increasing myocardial contractility. Name 3 nursing measures important to monitor in your newly diagnosied CHF pt. taking digoxin?
*Cardiac monitor & Apical HR. *K+ levels between 3.5-5meq/ml. *Assess for A-V Block. *Monitor for anorexia, N/V, fatigue & visual disturbances.
What is used to treat digoxin toxicity?
Digibind
Anticoagulants such as Heparin & Warfarin (coumadin) – disrupt the coagulation cascade & thereby suppress production of fibrin – preventing venous thrombus. Heparin’s effects are monitored by aPTT levels (60-80 sec) and overdose is treated with Protamine Sulfate. Name the mechanism of action of coumadin and what are overdoses treated with?
decrease prothrombin activity & prevents use of vit. K by the liver & Vitamin K.
*Don’t forget Low-molecular wt. Heparins like lovenox – Fixed dosing, cheaper, & NO bloodwork.
*Review Antiplatelets – ASA & Thrombolytics – Streptokinase.
Most frequently prescribed loop diuretic and most effective in producing the greatest urine output. Therapeutic use includes treatment of CHF, Edematous states, & HTN. Name that drug?
Furosemide (Lasix) or Demadex.
This drug is a thiazide diuretic with the mechanism of action in the distal convoluted tubule, 1st line drug to treat HTN, same side effects as Lasix. Name this drug?
Hydrochlorothiazide (HydroDiuril) HCTZ or Xaroxolyn.
High-Ceiling loop diuretics have the following adverse effects of Hypotension leading to tachycardia & Hypokalemia, name 2 others?
Ototoxicity (if given too fast IVP), Hyperglycemia, Hyperuricemia, Potentiates drug interactions such as Digoxin & K-sparing diuretics.
Spironolactone (Aldactone) blocks aldosterone in the distal nephron leading to K+ retension and Increased excretion of sodium & H2O. Name one significant adverse effect?
Hyperkalemia.
*Remember to use with caution with ACE inhibitors*
Nursing Interventions for diuretic dosing include:Take med in AM or before 1400, may take with food to reduce GI upset. Name 2 more Patient Education tips:
monitor BP, Pulse & weight for effects, Weigh daily, Rise slowly to standing postion, observe for signs of dehydration (light headedness, dizzy, thirst, confusion), monitor FSBS
Resp. Acidosis is caused by retention of CO2 secondary to hypoventilation with the treatment of sodium bicarbonate. State the cause & treatment of Respiratory alkalosis?
Hyperventilation & rebreathe CO2-laden expired breath (brown paper bag).
A common practice when converting the patient from oral to inhaled steriods?
taper the pills gradually.
2 Main drug classes used in the treatment of Asthma?
Anti-Inflammatory agents & Bronchodilators
We know the most effective drug for relief of acute bronchospasms is nebulized albuterol (bronchodilator) with the S/E of tachycardia, nervousness, angina, & tremors. So what is the long-term control fixed schedule drug in this class?
Salmeterol (Serevent Diskus) or Foradil Aerolizer.
Anti-inflammatory or Inhaled Glucocorticoids such as QVAR or Azmacort used prophylactically and to suppress inflammation in asthma. State 2 common side effects?
Oropharyngeal candidiasis, Dysphonia – hoarseness & speaking difficulty, and promotes bone loss.
Cromolyn (Intal) – acts to stabilize the cytoplasmic membrane mast cells (suppresses inflammation) NOT a bronchodilator, used for prophylaxis of asthma. State 2 patient education tips regarding the use of this med?
Routine use or scheduled dosing – not for emergencies.
15 min. prior to exercise for most beneficial effect.
Therapeutic effects may take several weeks
Name one drug class used to treat allergic rhinitis and its mechanism of action and common drug?
1. Anticholinergic – blocks muscarinic receptors in the bronchi (bronchial dilation) = Atrovent (Ipratropium Bromide)
2. Oral antihistamines – H1 receptor antagonists = Chlor-Trimeton & Benadrly
3. Intranasal Glucocorticoids –supress inflammation = Rhinocort, Flonase
4. Intranasal Cromolyn – Srpress release of histamine 1= NasalCrom
5. Sympathomimetics (oral/nasal) – Activate alpha-1 in nasal blood vessels = vasoconstriction=reduce stuffiness= Afrin or Sudafed.
Expectorants stimulate the flow of secretions making the cough more productive. Name that drug
Guaifenesin (Mucinex)
This is infused Intravenously to treat Hyperkalemia?
Infusion of Insulin & Glucose (which promotes uptake of K+ by the cells) or Sodium bicarbonate
Chemotherapy Drugs are more toxic to tissue in?
High growth fraction (Not in G0 phase)
Chemotherapy will be the most effective for a neoplastic tumor if the malignancy is?
growing rapidly! (High growth fraction)
A female client receives an antineoplastic drug for the treatment of breast cancer. The nurse observes for adverse reactions and takes the client’s vital signs routinely (Temp). What is the primary rationale for the nurse’s actions?
changes in vital signs can indicate an infection as a result of bone marrow depression (neutropenia).
Most serious complication of Chemotherapy?
Neutropenia (loss of neutrophils) = Infection
When a patient receiving chemo is at the highest risk for infection and experiencing the lowest neutrophil count between days 10-14 is a period called?
Nadir
3 modalities to treat cancerous solid tumors?
Irradiation, Surgery, & Debulking
Name one of the major drugs that should be considered in the plan of care for a client diagnosed with Peptic Ulcer Disease (PUD)?
Antacids (short term), Histamine 2 receptor antagonist, Proton pump inhibitors, Antibiotics.
A common Histamine (H2) – receptor Antagonists (Antisecretory agents) – Blocks receptors and decreases acid secretion. Used for GERD & treat and prevent ulcers.
Tagamet or Zantac
Common classification that inhibits gastric acid pump of the parietal cells?
Omeprazole (Prilosec)
This drug class neutralizes gastric acid by buffering hydrochloric acid, increasing tone of the LES, & increasing resistance to irritation.
Antacids
Remember to review antacid contents with specific disease process.
Regarding Laxatives, Go-lytely acts within 4 hours, bulk forming metamucil acts within 24-48 hours (like dietary fiber), the time frame for fecal softeners (Colace or Surfak) is?
1-3 days
Prokinetic agents (Propulsid & Reglan) act by?
Increases lower esophageal sphincter pressure and peristalsis (increasing emptying time)
Serum test performed for routine diabetes evaluation?
Hgb A1C.
Lispro (Humalog) Rapid acting onset 15 min., Regular Insulin (Humulin R) slower acting onset 30-60 min., NPH Intermediate acting onset 60-120 min, Lantus long acting peakless with a duration of 24 hours: Name the medication that is most like Regular Insulin in an inhaled form?
Exubera.
Regular Insulin is the only Insulin that can be given via 2 different routes, Name the routes?
SQ & IV.
Sulfonylurea Oral Hypoglycemic Agents such as Glucotrol & DiaBeta act by?
stimulate the release of insulin by Beta cells of the pancreas.
**Don’t forget to check for Sulfa allergies**
Biguanides such as metformin (Glucophage) acts by decreasing glucose production via liver and Inc. uptake by cells. Glitazones (Actos & Avandia) decrease glucose by reducing insulin resistance by the cells therefore inc. uptake. Both have the dec. S/E of hypoglycemia, which one has an additive effect and what is it?
metformin (Glucophage) and the additive effect of dec. LDL & inc. HDL.
*Don’t forget to monitor liver function test & encourage Avandia users to use birth control
3 life saving IV measures used for treating Acute Diabetic Ketoacidosis – please name them?
IV NS replacement, IV Potassium additive, & IV Insulin.
*IV Bicarbonate also important
Name 2 exams used to diagnosis TB?
Chest X-ray & Sputum Cx.
TB treatment plan used to prevent emergence of resistant organisms aside from strict compliance?
use of 2 or meds.
Common but unusual adverse effect seen with the use of Rifampin (Rifadin)?
Discoloration of body fluids (Red-orange, sweat, saliva, & tears)
Drug regimen for Tuberculosis consists of: Induction phase: 2 months – daily therapy
INH (Isoniazid) *peripheral neuropathy*
Rifampin
Pyrazinamide *watch for liver damage*
Ethambutol
What drugs are in the continuation phase for 4 months?
Isoniazid (INH) & Rifampin. *Daily or biweekly
A broad spectrum antifungal agent Amphotericin B (Fungizone) is considered highly toxic ranging from infusion reaction (fever, chills, nausea, HA) to a more severe complication?
renal damage or Nephrotoxicity
**Monitor Urine output & infuse 1000ml NS along with med infusion**
A common anti-viral drug Acyclovir (Zovirax) used to treat Herpes simplex & Varicella zoster has several side effects. State 2 important patient education interventions to provide upon discharge?
Important to educate on the need to use condoms even when no lesions. Nephrotoxicity reduced by infusing hydration during infusion and 2 hours after.
Be aware of possible GI upset & Vertigo.
Name the drug class that has the most common cause of drug allergies, is a bactericidal, and remains the drug of choice for many infections?
Penicillins.
*Review all classess of penicillins ie: narrow or broad.
What are narrow spectrum PCN (penicillinases sensitive +/-)?
Pencillin G (IM)
Penicillin V (PO)
Amoxicillin (PO)
What are narrow spectrum PCN (pencillinase resistant +)?
Nafcillin
Oxacillin
What are broad spectrum PCN (aminopenicillins +/-)?
ampicillin/Sulbactam
Amoxicillin /clavulanate
What are extended spectrum PCN (antipseudomonal PCN -)?
Piperacillin/tazobactam
This is the most widely used drug class of antibiotics with a similar structure to penicillin, toxicity is low, common names are Ancef, Keflex, Rocephin, and should be used with caution with severe PCN allergies.
Cephalosporins.
A common Bacteriostatic (suppress bacterial growth but do not kill), absorption is effected by calcium, milk and iron supplements, and is the primary treatment for Rickettsial diseases such as Rocky Mountain spotted fever?
Tetracycline.
*Remember it’s effects on the bone & teeth and the potential risk of super infections!
What are AE of Tetracyclines?
N/V/D, yellowing or brown discoloration of the teeth, supress bone growth, hepatic toxicity, renal toxicity, photosensitivity, superinfection (c-diff, staph bowel infection, over growth of candida)
Vancomycin is the big gun! Given IV, it is used to treat MRSA with the adverse effects of Ototoxicity when plasma levels exceed 30, Red man syndrome, & thrombophlebitis. What disorder does Vancomycin treat when given PO?
pseudomembraneous colitis.
Aminoglycosides – bactericidal, often referred to as the MYCINS, include drugs such as Gentamicin & Tobramycin. This drug class can cause serious injury to the inner ear (ototoxicity) and Kidney (Nephrotoxicity) – Name one nursing measure that can be performed to prevent this?
measure serum peaks & troughs.
Sulfonamides – Trimethoprim/Sulfamethoxazol (TMP/SMZ) Bactrim or Septra are the 1st line treatment for UTI’s, name 3 educational interventions your patient’s should be aware of while taking these meds?
Avoid prolonged sun exposure – wear sunscreen (you may experience a rash or photosensitivity)
Crystalluria – must drink 8-10 glasses of water.
Drug interactions – intensifies effects of coumadin, dilantin & Sulfonylureas (DM meds) often leading to hypoglycemia.
This amount of Insulin is produced naturally by the body each day?
approximately 120 units.
Name the rare side effect of the drug Ciprofloxacin (Cipro) that is the drug of choice for anthrax?
Tendon Rupture. *Achilles
How do beta blockers work? (metoprolol & propranolol)
prevent stimulation of sympathetic nervous system
inhibit action of catecholamines norepi and epi at beta adrenergic receptors
*non selective blocks beta 1 and beta 2 receptors (propranolol)
*
What do you need to teach your pt about beta blockers?
do not give to pt w/asthma or COPD
educate s/s of hypoglycemia
educate on taking BP, keep a log, monitor HR
do not stop taking aburptly
if taking antacid take 1-2 hours after beta-blocker
What AE when using beta blockers?
hypotension, bradycardia (because they decrease HR), palpations, hypoglycemia with insulin use, brochospasm
How do calcium channel blockers work? (verapamil diltiazem)
block calcium access to cells causing decrease in contractility, conductivity of the heart thru AV node, & demand for oxygen
What do you teach your patient about calcium channel blockers?
postural hypotension (get up slowly), call dr if experience signs of edema (ankles/feet), avoid grapefruit juice, increase dietary fiber and fluid to minimize constipation, call dr if experience slow HR, SOB, or wt gain
What are the AE of calcium channel blockers?
decrease BP, bradycardia, may precipitate AV block, HA, constipation, nausea, peripheral edema
How do ACE inhibitors work? (captopril)
decrease peripheral vascular resistance w/out increasing cardiac output, cardiac rate, & cardiac contractility and also improves CO
What do you teach your pt about ACE inhibitors?
educate about hypotension and get up slowly, take your first dose at HS (prevent orthostatic hypotension), s/s angioedema, if develop cough call DR, monitor K+ level (can cause hyperkalemia), avoid K+ supplements and K+ containing salts, WBC done q 2 weeks fr 1st 3 mos & monitor for neutropenia, be aware NSAIDS decrease the effectiveness
How do ARBs work? (end in sartan)
affect the end result of RAAS--blocks activation of angiotensin II receptor type 1
dilate vessels (decrease BP), decrease secretion of aldosterone
**Pt that develop a cough taking ACE inhibitors can be switched to ARB b/c it does not have the cough as SE
How does digoxin work?
increase myocardial contractile force which causes increase cardiac output, depresses SA node, reduces conduction of the impulse thru AV node, slows HR
What do you teach your pt taking digoxin?
s/s of digoxin toxicity, eat foods high in K+, s/s of hypokalemia (muscle weakness), how to measure HR and call DR < 60 or >100
What are the AE of Digoxin?
cardiac dysrhythmias, hypokalemia, bradycardia (sign of toxicity)N/V, HA, dizziness, visual disturbances,(blurred, yellow vision, halos around dark objects), fatigue, DO NOT double up with missed doses,
How does low molecular weight heparin work? (lovenox , heparin)
reduce formation of fibrin in the coagulation cascade, prevent thrombin & further clot growth
What do you teach your pt about low molecular weight heparin?
can increase bleeding, report s/s of bleeding ,lovenox – Fixed dosing, cheaper, & NO bloodwork.
What are AE of low molecular weight heparin?
hemorrhage, hematuria, epistaxis, ecchymosis, bleeding gums, thrombocytopenia, hypotension
How do bulk forming laxatives work?
cause H2O to be retained in stool
What complications could occur with bulk forming laxatives?
esophageal obstruction, gas formation, intestinal obstruction or impaction
DO NOT USE W/PT WHO MAY HAVE GI OBSTURCTION OR IMPACTION
How do osmotic laxatives work? (MOM, Fleets)
hypertonic compounds draw H2O into the bowel causing peristalsis
Who should not take osmotic laxatives?
pt w/ undiagnosed abdominal pain & pt w/ renal impairment
can cause acute renal failure in high risk pts (kidney disease, taking drugs that alter renal function like ACE, ARBs, & diuretics)
How do surfactant laxatives work? (docusate sodium / colace)
wetting agent - draw H2O into the stool to soften
What type of patient is surfactant laxatives appropriate for?
best for cardiac pt because they are non irritating and no bulking , no straining
How do stimulant laxatives work? (bisacodyl/ducolax, Senna/Ex Lax)
act directly on the bowel via nerve stimulation
What type of patient is stimulant laxatives appropriate for?
no indication to avoid on specific pt
What is PUD?
peptic ulcer disease
- may occur in esophagus, stomach, or upper part of duodenum
- open sore in lining of stomach or duodenum