Chemistry BOC 7th ed. : Key Terms & Definitions for Medicine
1/375
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
376 Terms
Following overnight fasting, hypoglycemia in adults is defined as a glucose of:
a. ≤70 mg/dL (≤3.9 mmol/L)
b. ≤60 mg/dL (≤3.3 mmol/L)
c. ≤55 mg/dL (≤3.0 mmol/L)
d. ≤45 mg/dL (≤2.5 mmol/L)
c. ≤55 mg/dL (≤3.0 mmol/L)
Diagnosis of hypoglycemia in non-diabetic adults. If blood glucose levels are measured while the person is experiencing those symptoms and found to be ≤45 mg/dL (≤2.5 mmol/L) in a woman ≤55 mg/dL (≤3.0 mmol/L) in a man.
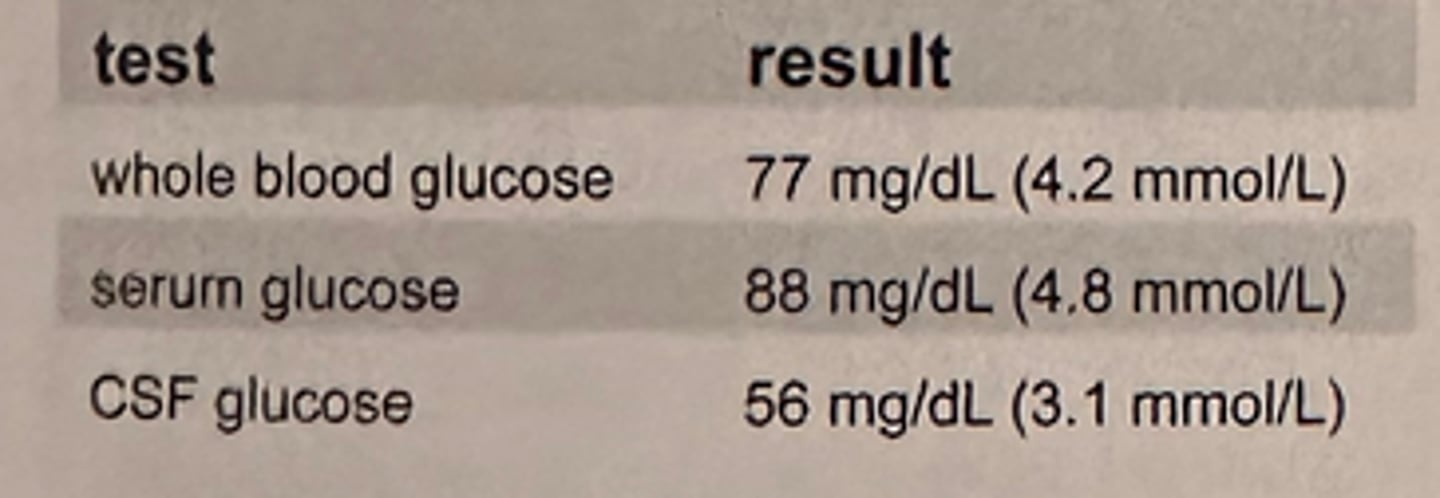
The results shown in the table are from a 21-year-old patient with a back injury who appears otherwise healthy:
The best interpretation of these results is that:
a. the whole blood and serum values are expected but the CSF value is elevated
b. the whole blood glucose value should be higher than the serum value
c. all values are consistent with a normal healthy individual
d. the serum and whole blood values should be identical
c. all values are consistent with a normal healthy individual
Fasting whole blood is 10-15% lower than plasma glucose
The preparation of a patient for standard glucose tolerance testing should include:
a. a high carbohydrate diet for 3 days
b. a low carbohydrate diet for 3 days
c. fasting for 48 hours prior to testing
d. bed rest for 3 days
a. a high carbohydrate diet for 3 days
GTT diet preparation. Perform in the AM after 3 days of unrestricted diet containing at least 150 g of carbohydrates/day.
If a fasting glucose is 90 mg/dL, which of these 2-hour postprandial glucose results would most closely represent normal glucose metabolism?
a. 55 mg/dl (3.0 mmol/L)
b. 100 mg/dl (5.5 mmol/L)
c. 180 mg/dl (9.9 mmol/L)
d. 260 mg/dl (14.3 mmol/L)
b. 100 mg/dl (5.5 mmol/L)
Normal 2-hour postprandial value should return to approximately fasting state at 2 hours postprandial
A healthy person with a blood glucose of 80 mg/dL (4.4 mmol/L) would have a simultaneously determined CSF glucose value of:
a. 25 mg/dL (1.4 mmol/L)
b. 50 mg/dL (1.4 mmol/L)
c. 100 mg/dL (1.4 mmol/L)
d. 150 mg/dL (1.4 mmol/L)
b. 50 mg/dL (1.4 mmol/L)
CSF glucose is ~60% of blood glucose
A 25-year-old man became nauseated and vomited 90 minutes after receiving a standard 75g carbohydrate dose for an oral glucose tolerance test. The best course of action is to:
a. give the patient a glass of orange juice and continue the test
b. start the test over immediately with a 50 g carbohydrate dose
c. draw blood for glucose and discontinue test
d. place the patient in a recumbent position, reassure him and continue the test
c. draw blood for glucose and discontinue test
GTT is discontinued when the patient vomits the glucose solution; however, the partial information is useful
CSF for glucose assay should be:
a. refrigerated
b. analyzed immediately
c. heated 56 degrees Celsius
d. stored at room temperature after centrifugation
b. analyzed immediately
Glycolysis may occur more quickly on glucose in CSF due to presence of bacteria or cells so it should be analyzed immediately.
Which of these 2-hour postprandial glucose values demonstrates unequivocal hyperglycemia diagnostic for diabetes mellitus?
a. 160 mg/dL (8.8 mmol/L)
b. 170 mg/dL (9.4 mmol/L)
c. 180 mg/dL (9.9 mmol/L)
d. 200 mg/dL (11.0 mmol/L)
d. 200 mg/dL (11.0 mmol/L)
A glucose level of ≥200 mg/L gives an unequivocal diagnosis of diabetes mellitus postprandially
Serum levels that define hypoglycemia in preterm or low birth weight infants are:
a. the same as adults
b. lower than adults
c. the same as a normal full-term infant
d. higher than a normal full-term infant
b. lower than adults
Age effect on glucose and hypoglycemia in infants is determined at much lower levels. Neonates have lower glucose levels than adults. Additionally, the serum levels that define hypoglycemia is lower in preterm infants when compared to full term infants
A 45-year-old woman has a fasting serum glucose concentration of 95 mg/dL (5.3 mmol/L) and a 2-hour postprandial glucose concentration of 105 mg/dL (5.8 mmol/L). The statement which best describes this patient's fasting serum glucose concentration is:
a. normal; reflecting glycogen breakdown by the liver
b. normal; reflecting glycogen breakdown by skeletal muscle
c. abnormal; indicating diabetes mellitus
d. abnormal; indicating hypoglycemia
a. normal; reflecting glycogen breakdown by the liver
Glucagon breaks down glycogen after an individual has fasted to prevent a rapid decline in the blood glucose
Pregnant women with symptoms of thirst, frequent urination or unexplained weight loss should have which of the following tests performed?
a. tolbutamide test
b. lactose tolerance test
c. epinephrine tolerance test
d. glucose tolerance test
d. glucose tolerance test
A 2-step method for determining gestational diabetes is recommended
In the fasting state, the arterial and capillary blood glucose concentration varies from the venous glucose concentration by approximately how many mg/dL (mmol/L)?
a. 1 mg/dL (0.05 mmol/L) higher
b. 5 mg/dL (0.27 mmol/L) higher
c. 10 mg/dL (0.55 mmol/L) higher
d. 15 mg/dL (0.82 mmol/L) higher
b. 5 mg/dL (0.27 mmol/L) higher
In fasting state, arterial/capillary glucose concentration is 2-5 mg higher than venous blood
The conversion of glucose or other hexoses into lactate or pyruvate is called:
a. glycogenesis
b. glycogenolysis
c. gluconeogenesis
d. glycolysis
d. glycolysis
Which of the following values obtained during a glucose tolerance test is diagnostic of diabetes mellitus?
a. 2-hour specimen = 150 mg/dL (8.3 mmol/L)
b. fasting plasma glucose = 126 mg/dL (6.9 mmol/L)
c. fasting plasma glucose = 110 mg/dL (6.1 mmol/L)
d. 2-hour specimen = 180 mg/dL (9.9 mmol/L)
b. fasting plasma glucose = 126 mg/dL (6.9 mmol/L)
A fasting glucose of ≥126 is diagnostic of diabetes mellitus
Monitoring long-term glucose control in patients with adult onset diabetes mellitus can best be accomplished by measuring:
a. weekly fasting 7am serum glucose
b. glucose tolerance testing
c. 2-hour postprandial serum glucose
d. HbA1C
d. HbA1C
HbA1c represents average glucose over time and is the best predictor
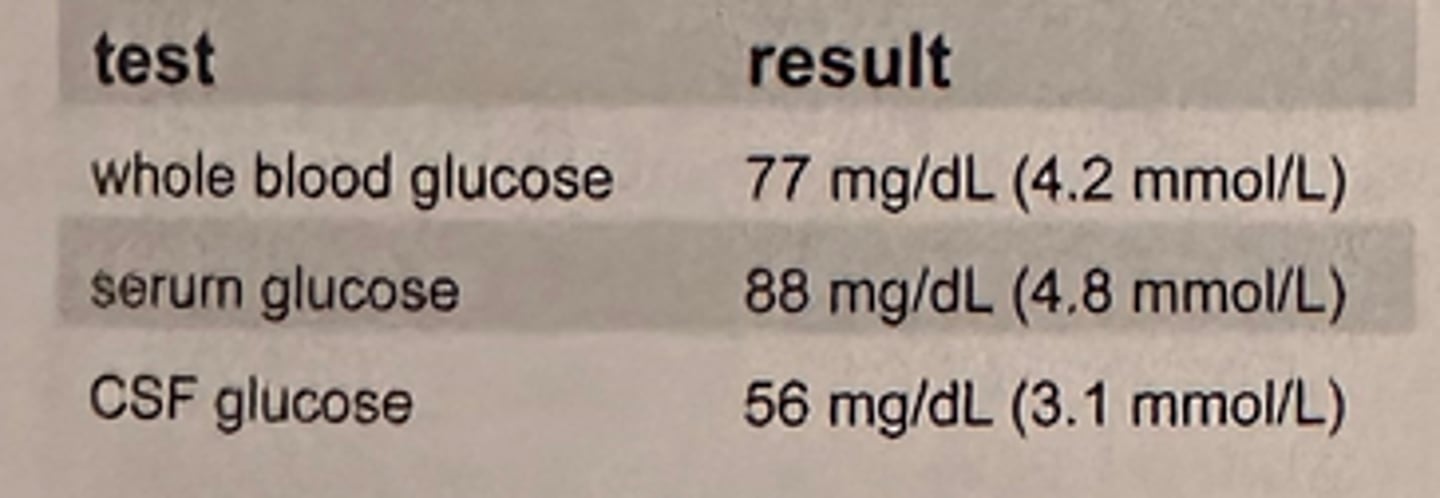
c. improving state of metabolic control as indicated by fructosamine
Fructosamine is a glycated protein which may be used in place of HbA1c in patients with hemoglobin variants. There is not agreement on the clinical utility of fructosamine.
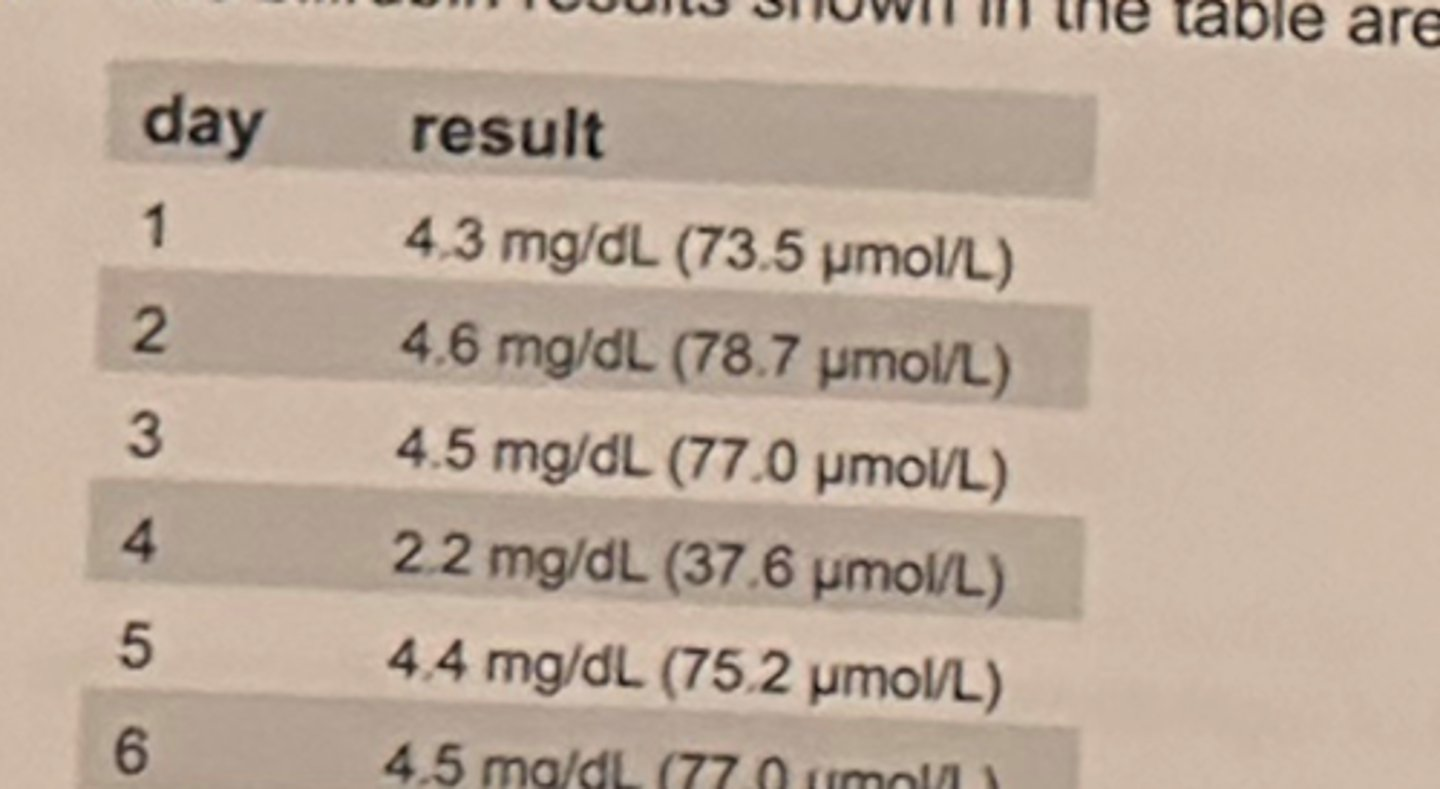
A patient with type 1, insulin-dependent diabetes mellitus has the results shown in the table.
After reviewing these test results, the technologist concluded that the patient is in a :
a. "steady state" of metabolic control
b. state of flux, progressively worsening metabolic control
c. improving state of metabolic control as indicated by fructosamine
d. state of flux as indicated by the fasting glucose level
Total glycosylated hemoglobin levels in a hemolysate reflect the:
a. average blood glucose levels of the past 2-3 months
b. average blood glucose levels for the past week
c. blood glucose level at the time the sample is drawn
d. HbA1C level at the time the sample is drawn
a. average blood glucose levels of the past 2-3 months
The rate of formation of glycated hemoglobin is directly proportional to the concentration of glucose in the blood, therefore the glycated hemoglobin concentration is an average for glucose values over the preceding 8 to 12 weeks
Which of these glycosylated hemoglobins is recommended by the ADA guidelines for testing diabetic patients?
a. HbA1a
b. HbA2
c. HbA1b
d. HbA1c
d. HbA1c
HbA1c is the major fraction of glycated hemoglobin
A patient with hemolytic anemia will:
a. show a decrease in glycated Hb value
b. show an increase in glycated Hb value
c. show little or no change in glycated Hb value
d. demonstrate an elevated HbA1
a. show a decrease in glycated Hb value
Glycated hemoglobin is directly related to the life of RBCs as it is the average glucose values over the lifespan of a RBC, approximately 120 days
In using ion-exchange chromatographic methods, falsely increased levels of Hgb A1c might be demonstrated in the presence of:
a. iron deficiency anemia
b. pernicious anemia
c. thalassemia
d. HbS
d. HbS
HbS & HbC yield falsely decreased levels in ion exchange chromatography methods.
An increase in serum acetone is indicative of a defect in the metabolism of:
a. carbohydrates
b. fat
c. urea nitrogen
d. uric acid
a. carbohydrates
Increase in ketones is found when there is a decreased use of carbohydrates, such as in diabetes
An infant with diarrhea is being evaluated for a carbohydrate intolerance. His stool yields a positive copper reduction test and a pH of 5.0. It should be concluded that:
a. further tests are indicated
b. results are inconsistent - repeat both tests
c. the diarrhea is not due to carbohydrate intolerance
d. the tests provided no useful information
a. further tests are indicated
Copper reduction reaction detects many reducing substances
Blood samples are collected at the beginning of an exercise class and after 30 minutes of aerobic activity. Which of the following would be most consistent with the post-exercise sample?
a. normal lactic acid, low pyruvate
b. low lactic acid, elevated pyruvate
c. elevated lactic acid, low pyruvate
d. elevated lactic acid, elevated pyruvate
d. elevated lactic acid, elevated pyruvate
After strenuous exercise, lactate and pyruvate may increase due to increased carbohydrate metabolism in the skeletal muscle
What is the best method to diagnose lactase deficiency?
a. H2 breath test
b. plasma aldolase level
c. LD level
d. D-xylose test
a. H2 breath test
Diagnosis of lactase deficiency by H2 breath test based on bacteria acting on unabsorbed disaccharides
The different water content of erythrocytes and plasma makes true glucose concentrations in whole blood a function of the:
a. hematocrit
b. leukocyte count
c. erythrocyte count
d. erythrocyte indices
a. hematocrit
Glucose is measured in the water of the sample and not the cells. Water content is much higher in plasma than in whole blood so Hct, the ratio of cells to plasma, affects glucose result. Glucose is ~11% lower in whole blood due to presence of RBCs in the sample that displace the water. If the leukocyte count is high and serum or plasma is not separately from blood cells quickly, glucose will be consumed and falsely lower.
In a specimen collected for plasma glucose analysis, sodium fluoride:
a. serves as a coenzyme of hexokinase
b. prevents reactivity of non glucose reducing substances
c. precipitates proteins
d. inhibits glycolysis
d. inhibits glycolysis
Sodium fluoride exerts its preservative action by inhibiting the enzyme systems involved in glycolysis and thus prevents red or white blood cells from consuming the glucose and falsely lowering the amount in the first few minutes. It will not protect glycolysis in the first hour. It does not react in the hexokinase method wither enhancing or inhibiting activity nor does it react with non-glucose reducing methods
Which of these serum constituents is unstable if a blood specimen is left standing at room temperature for 8 hours before processing?
a. cholesterol
b. triglyceride
c. creatinine
d. glucose
d. glucose
Glucose decreases at a rate of 5-7% per hour in whole blood at room temperature. Glycolysis will continue until the specimen is processed by centrifugation, and serum and plasma are separated from the cellular components of blood. Cholesterol, triglycerides and creatinine are not as unstable in serum left at room temperature over an 8-hour period.
One international unit of enzyme activity is the amount of enzyme that will, under specified reaction conditions of substrate concentration, pH and temperature, cause utilization of substrate at the rate of:
a. 1 mol/min
b. 1 mmol/min
c. 1 micromol/min
d. 1 nanomol/min
c. 1 micromol/min
In 1961, the enzyme commission recommended the adoption of an international unit (IU) of enzyme activity. The IU was defined as the amount of enzyme that would convert 1 micromol of substrate per minute under standard conditions.
1 IU = 1 micromol/min
In spectrophotometric determination, which of the following is the formula for calculating the absorbance of a solution?
a. (absorptivity x light path)/concentration
b. (absorptivity x concentration)/light path
c. absorptivity x light path x concentration
d. (light path x concentration)/absorptivity
c. absorptivity x light path x concentration
A= abc is mnemonic for Absorbance = absorptivity x light path x concentration
The most specific method for the assay of glucose in all body fluids utilizes:
a. hexokinase
b. glucose oxidase
c. glucose-6-phosphatase
d. glucose dehydrogenase
a. hexokinase
Hexokinase is the method most specific to both forms of glucose and the basis for the reference method and should be the method of choice for urine due to fewer interferences. Glucose oxidase/peroxidase method is the second most specific method mainly due to potential interferences in the peroxidase step and is commonly employed in automated methods as well as dipstick screening methods in routine urinalysis. Glucose dehydrogenase is suitable for POCT devices .
Which of the following is an example of glucose-specific colorimetric method?
a. alkaline ferricyanide
b. glucose oxidase
c. hexokinase
d. o-toluidine
b. glucose oxidase
Other distractors are not glucose-specific methods.
Hexokinase is specific for other isomers of glucose.
Ferricyanide was a nonspecific method for reducing substances method
o-toluidine is a condensation method and reacts w/ HgB (found in feces), mannose and other sugars as well as glucose so not specific. It was used in the past for CSF glucose methods.
Increased concentrations of ascorbic acid inhibit chromogen production in which of the following commonly-used glucose methods?
a. ferricyanide
b. ortho-toluidine
c. glucose oxidase (peroxidase)
d. hexokinase
c. glucose oxidase (peroxidase)
Ascorbic acid interferes with the peroxidase step. This is a limitation of the glucose oxidase (peroxidase) reaction making it not as specific overall, as the hexokinase method. Other sugars react in the o-toluidine method but ascorbic acid is not generally thought to interfere significantly. The ferricyanide method is affected by many substances since it is nonspecific for reducing substances so ascorbic acid would also interfere but it is an obsolete method.
In the Hexokinase method for glucose determinations, the actual end product measured is the:
a. amount of hydrogen peroxide produced
b. NADH produced from the reduction of NAD
c. amount of glucose combined with bromcresol purple
d. condensation of glucose with an aromatic amine
b. NADH produced from the reduction of NAD
The principle of the hexokinase method is the production of NADPH from NADP in a coupled enzymatic reaction involving hexokinase, ATP and glucose-6-phosphate dehydrogenase and NADP. Hydrogen peroxide is produced in the first step of the coupled glucose oxidase/peroxidase method. O-toluidine condenses glucose with an aromatic amine. Bromcresol purple binds with albumin to form a spectrophotometric product.
At midmorning, blood glucose levels fall and stimulate the secretion of which hormone?
a. cortisol
b. epinephrine
c. glucagon
d. insulin
c. glucagon
Glucagon is released in fasting states and increases blood glucose levels by increasing glycogenolysis from the liver and increasing glyconeogenesis.
Deficiency of this enzyme is the most frequent cause of galactosemia:
a. glucose-6-phosphatase
b. galactose-1-phosphate uridyl transferase
c. glacatokinase
d. uridine diphosphate 4 epimerase
b. galactose-1-phosphate uridyl transferase
The deficiency of galactose-1-phosphate uridyl transferase, which causes Type 1 glycogen storage disease, is the most common form of galactosemia.
High levels of which lipoprotein class are associated with decreased risk of accelerated atherosclerosis?
a. chylomicrons
b. VLDL
c. LDL
d. HDL
d. HDL
High-density lipoprotein (HDL) is the smallest and most dense lipoprotein. Its role in lipid metabolism involves removing cholesterol from the peripheral cells and transporting it to the liver for further metabolism. Because of these actions, HDL is thought to be anti-atherogenic. Increased levels of LDL, VLDL, and chylomicrons are associated with atherosclerosis.
The most consistent analytical error involved in the routine determination of HDL is caused by:
a. incomplete precipitation of LDL
b. coprecipitation of HDL and LDL
c. inaccurate protein estimation of HDL
d. a small concentration of apoB-containing lipoproteins after precipitation
d. a small concentration of apoB-containing lipoproteins after precipitation
Serum HDL has been routinely measured indirectly by a 2-step procedure.
Precipitation of all the non-HDL lipoprotiens with a polyanion-divalent cation combination reagent and centrifugation to obtain the supernatant containing only HDL.
The cholesterol bound to HDL is measured as HDL.
One challenge regarding the method has been the selection of a precipitating reagent that would precipitate the ApoB containing lipoproteins. Dextran sulfate with magnesium has proven to be very effective.
If the LDL is to be calculated by the Friedewald formula, what are the 2 measurements that need to be carried out by the same chemical procedure?
a. total cholesterol and HDL
b. total cholesterol and triglyceride
c. triglyceride and chylomicrons
d. apolipoprotein A and apolipoprotein B
a. total cholesterol and HDL
LDL cholesterol = Total cholesterol- (HDL-cholesterol + Triglyceride/5
(indirect, not valid for triglycerides over 400 mg/dL)
In the indirect measurement of LDL using the Friedewald equation, values are needed for the total chol, HDL chol and trig.
Because LDL and HDL are measured based on their cholesterol content, it is necessary to determine the total cholesterol and HDL cholesterol using the same cholesterol procedure following the precipitation step in the HDL method.
The chemical composition of HDL corresponds to:
a. triglyceride 60%, cholesterol 15%, protein 10%
b. triglyceride 10%, cholesterol 45%, protein 25%
c. triglyceride 5%, cholesterol 15%, protein 50%
d. triglyceride 85%, cholesterol 5%, protein 2%
c. triglyceride 5%, cholesterol 15%, protein 50%
High-density lipoprotein (HDL) is the smallest and most dense of the lipoproteins. This is evidenced by its lipid content of 20% and protein concentration of 50%.
In familial hypercholesterolemia, the hallmark finding is an elevation of:
a. low-density lipoproteins
b. chylomicrons
c. high-density lipoproteins
d. apolipoprotein A1
a. low-density lipoproteins
Familial hypercholesterolemia is a genetic condition = inc serum chol lvls.
In homozygotes and heterozygotes, the elevated chol is associated with an inc LDL level.
The lack or deficiency of the LDL receptors prevents the metabolism of LDL cholesterol, resulting in an increased LDL level.
Premature atherosclerosis can occur when which of the following becomes elevated?
a. chylomicrons
b. prostaglandins
c. low-density lipoproteins
d. high-density lipoproteins
c. low-density lipoproteins
Atherosclerosis is characterized by a thickening and hardening of the arterial walls by cholesterol
Transportation of 60-75% of the plasma cholesterol is performed by:
a. chylomicrons
b. very low-density lipoproteins
c. low-density lipoproteins
d. high-density lipoproteins
c. low-density lipoproteins
LDL transports about 70% of the total plasma cholesterol.
HDL transports a smaller portion of the cholesterol through reverse-cholesterol transport from peripheral cells.
Chylomicrons and VLDL transport triglycerides.
Which of the following diseases results from a familial absence of high density lipoprotein?
a. Krabbe disease
b. Gaucher disease
c. Tangier disease
d. Tay-Sachs disease
c. Tangier disease
Tangier disease results from a defect in the catabolism of Apo A-I, an essential apoprotein for HDL.
In homozygotes, the plasma level for HDL is ~ 0. It is a rare autosomal disorder. The reduced HDL levels result from increased HDL catabolism.
Other more common causes of hypoalphalipoproteinemia include LCAT deficiency and mutations of the APOA-1 gene.
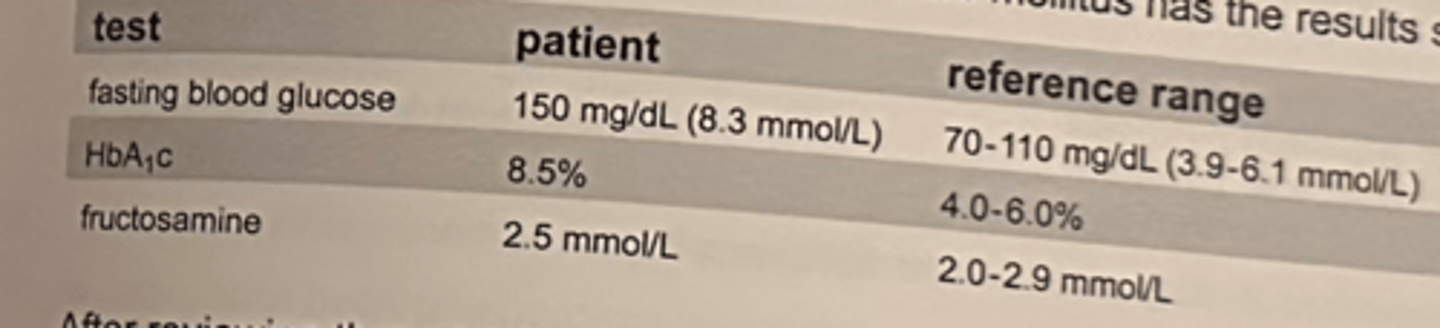
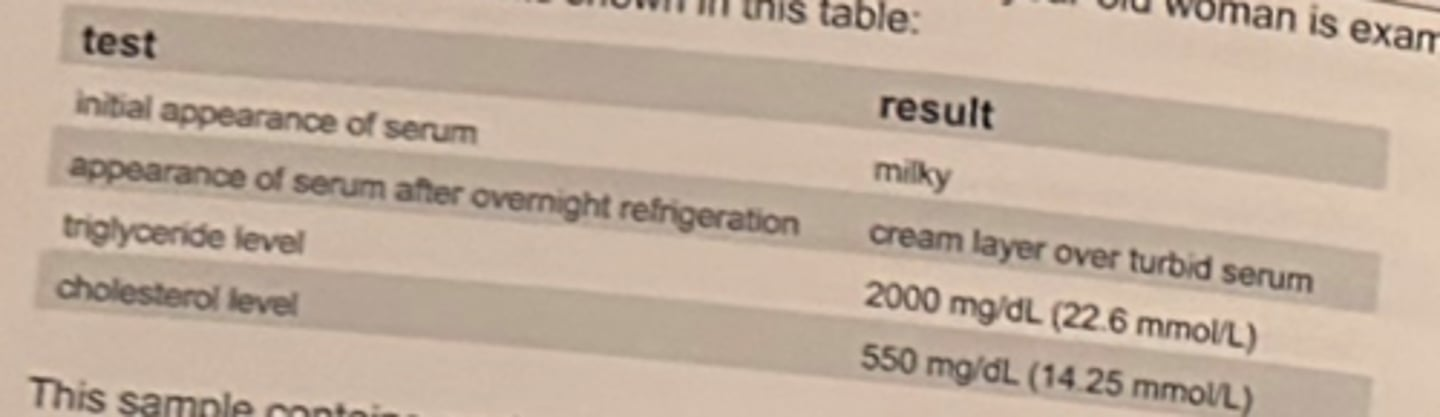
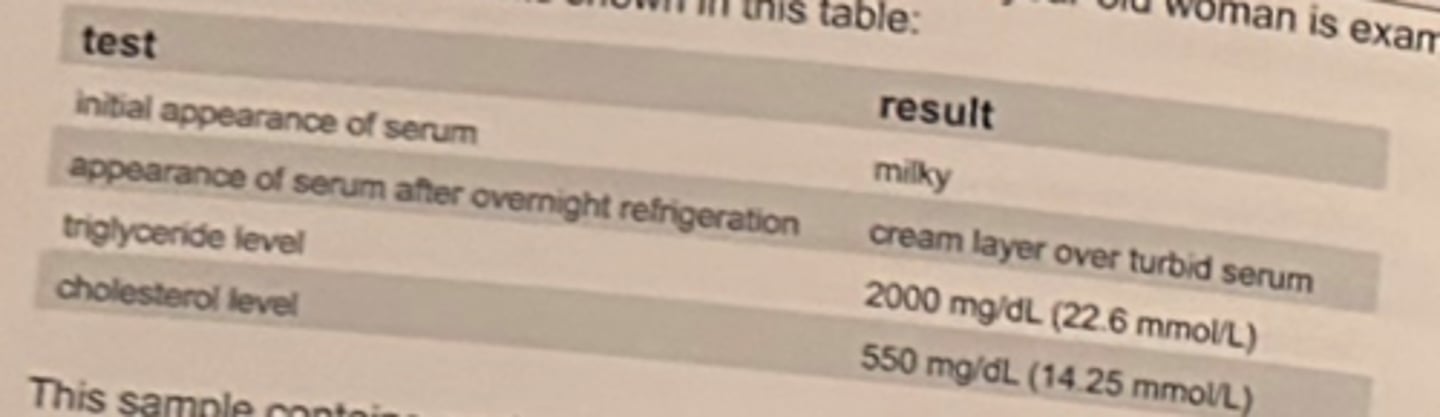
A 1-year-old girl with a hyperlipoproteinemia and lipoprotein lipase deficiency has the lipid profile results shown in the table.
A serum specimen from this patient that is refrigerated overnight would most likely appear:
a. clear
b. cloudy
c. creamy layer over cloudy serum
d. creamy layer over clear serum
d. creamy layer over clear serum
accumulation of chylomicrons is evident in blood samples of patients with familial chylomicronemia syndrome (FCS), which is sometimes known as lipoprotein lipase deficiency (LPLD), or Fredrickson type 1 hyperlipoproteinemia. Lipid analysis using overnight refrigeration involves incubating the sample at 4 C overnight.
The chylomicrons which have the lowest density of the lipoproteins, present as a thick homogenous cream layer and may be observed floating at the plasma surface.
= familial hyperchylomicronemia due to deficiency in lipoprotein lipase activity which is responsible for breaking down triglycerides.
Which of the following lipid results would be expected to be falsely elevated on a serum specimen from a non-fasting patient?
a. cholesterol
b. triglyceride
c. HDL
d. LDL
b. triglyceride
Food intake can cause a transient increase in the triglyceride level by 50%.
The LDL and HDL levels may be decreased depending on the fat content of the meal.
Total cholesterol does not usually change significantly after a meal.
A 9-month old boy from Israel has gradually lost the ability to sit up, and develops seizures. He has an increased amount of a phospholipid called GM2-ganglioside in his neurons, and he lacks the enzyme hexosaminidase A in his leukocytes. These findings suggest:
a. Neimann-Pick disease
b. Tay-Sachs disease
c. phenylketonuria
d. Hurler syndrome
b. Tay-Sachs disease
Tay-Sachs disease is a rare inherited disorder characterized by the near-total deficiency of the enzyme N-acetyl-beta-hexosaminidase A. The enzyme is responsible for the hydrolysis of the beta (1,4)-glycosidic bond between N-acetylgalactosamine and galactose in GM2 ganglioside. Neimann-Pick disease and Hurler syndrome are lysosomal disorders as is Tay-Sachs. Phenylketonuria results from an absent enzyme, but is an inborn error of metabolism.
Apolipoprotein A1 is the major component of which lipoprotein?
a. chylomicrons
b. HDL
c. LDL
d. VLDL
b. HDL
Apolipoprotein A1 acts as a receptor site on HDL
The lipoprotein that transports cholesterol away from the tissues is:
a. HDL
b. IDL
c. LDL
d. VLDL
a. HDL
HDL serves to transport cholesterol away from the tissues and provides protection against cardiac disease.
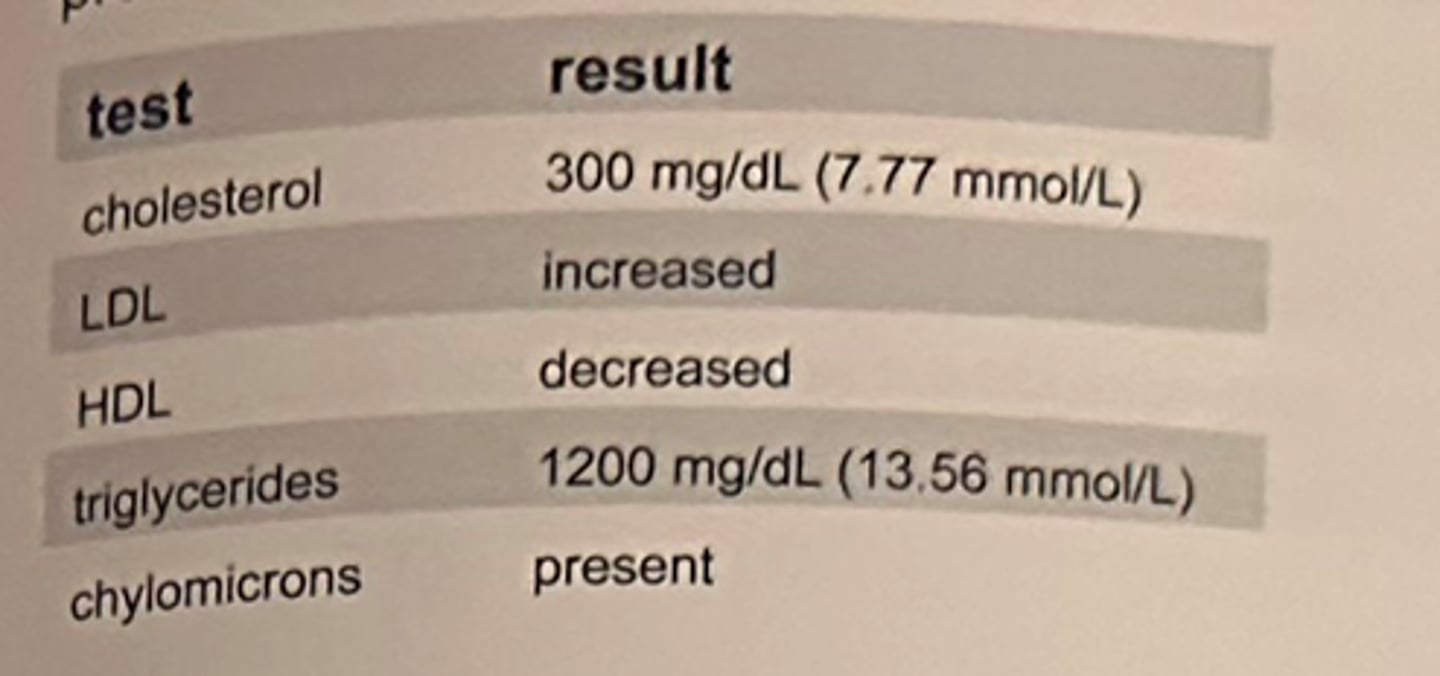
A fasting serum sample from an asymptomatic 43-year-old woman is examined visually and chemically with the results shown in the table.
The sample contains predominantly:
a. chylomicrons, alone
b. chylomicrons and very low-density lipoproteins (VLDL)
c. very low-density lipoproteins (VLDL) and low-density lipoproteins (LDL)
d. high-density lipoproteins (HDL)
b. chylomicrons and very low-density lipoproteins (VLDL)
Mixed hyperlipoproteinemia or type V hyperlipoproteinemia occurs primarily in adulthood and is characterized by markedly elevated TRIGs, elevated VLDL and chylomicrons.
Because of the markedly increased triglyceride level, the specimen integrity is MILKY, and overnight refrigeration shows a creamy layer over turbid serum due to the chylomicrons and triglycerides.
Chylomicrons are present in which of the following dyslipidemias?
a. familial hypercholesterolemia
b. hypertriglycerdemia
c. deficiency in lipoprotein lipase activity
d. familial hypoalphalipoproteinemia
c. deficiency in lipoprotein lipase activity
Lipoprotein lipase hydrolyzes triglycerides and chylomicrons during normal lipid metabolism. A deficiency in lipoprotein lipase results in markedly increased serum chylomicrons and triglycerides.
The function of the major lipid components of the very low-density lipoproteins (VLDL) is to transport:
a. cholesterol from peripheral cells to the liver
b. cholesterol and phospholipids to peripheral cells
c. exogenous triglycerides
d. endogenous triglycerides
d. endogenous triglycerides
In the endogenous pathway for lipid metabolism, the hepatocytes can synthesize triglycerides from carbohydrates and fatty acids. The triglycerides are packaged in VLDL, and ultimately delivered to the circulation in that form. Exogenous triglycerides are transported primarily by chylomicrons. HDL transports cholesterol from peripheral cells to the liver. LDL transports cholesterol and phospholipids to peripheral cells.
Turbidity in serum suggests elevation of:
a. cholesterol
b. total protein
c. chylomicrons
d. albumin
c. chylomicrons
Elevated levels of chylomicrons in serum or plasma will result in a turbid specimen. The large size of the chylomicron will reflect the light, causing a turbid appearance.
A lipemic serum is separated and frozen at -20°C for assay at a later date. One week later, prior to performing an assay for triglycerides, the specimen should be:
a. warmed to 37°C and mixed thoroughly
b. warmed to 15°C and centrifuged
c. transferred to a glycerated test tube
d. discarded and a new specimen obtained
a. warmed to 37°C and mixed thoroughly
Frozen samples should be allowed to thaw slowly at room temperature (22°C) or in a 37°C water bath and should then be mixed thoroughly before analysis.
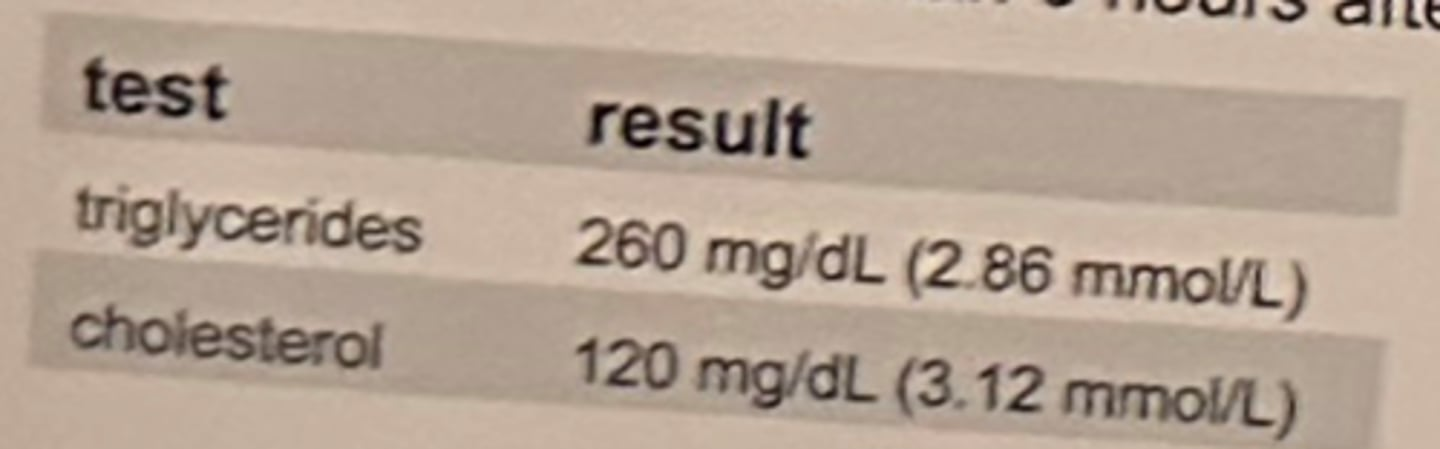
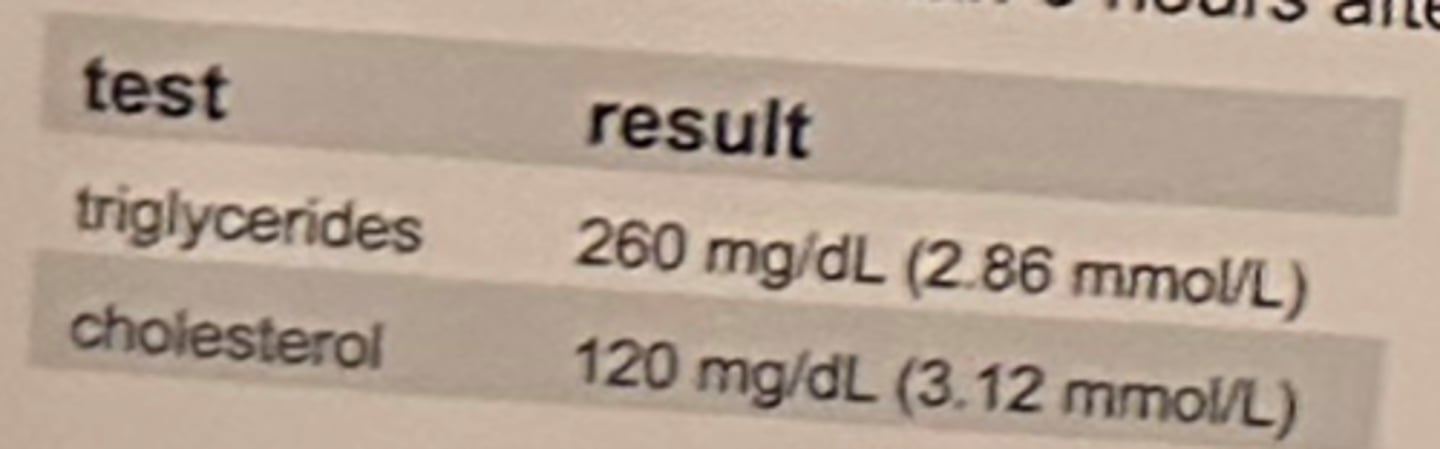
As part of a hyperlipidemia screening program, the results shown in the table are obtained from a 25-year-old woman 6 hours after eating.
Which of the following is the best interpretation of these results?
a. both results are normal, and not affected by the recent meal
b. cholesterol is normal, but triglycerides are elevated, which may be attributed to the recent meal.
c. both results are elevated, indicating a metabolic problem in addition to the non-fasting state
d. both results are below normal despite the recent meal, indicating a metabolic problem.
b. cholesterol is normal, but triglycerides are elevated, which may be attributed to the recent meal.
A high-fat diet increases the serum concentrations of triglycerides. Fasting overnight for 10-14 hours is the optimal interval for fasting around which to standardize blood collections including lipids.
Blood is collected in a serum separator tube on a patient who has been fasting since midnight. The time of collection is 7 am. The lab test that should be recollected is:
a. triglycerides
b. iron
c. LD
d. sodium
a. triglycerides
Triglycerides are affected by recent ingestion (<8 hour) of food. Fasting overnight for 10-14 hours is the optimal interval for fasting around which to standardize blood collections
including lipids. Iron is subject to circadian rhythm and is best analyzed on a specimen drawn in the morning, however a specific time of fasting is not as critical. LD and sodium are not affected by recent ingestion of food.
Which of the following is the formula for calculating absorbance given the percent transmittance (%T) of a solution?
a. 1-log(%T)
b. log(%T)/2
c. 2xlog(%T)
d. 2-log(%T)
d. 2-log(%T)
Because of the following relationship is true, A = light stopped and T = light passed through, A and T are inversely related. They are also logarithmically related, because the absorption of light is a logarithmic function. A =-log (I/I0) = log(100%)-log(%T). Log of 100%=2.
The substance that is measured to estimate the serum concentration of triglycerides by most method is:
a. phospholipids
b. glycerol
c. fatty acids
d. pre-beta lipoprotein
b. glycerol
There are several enzymatic methods for measuring serum triglyceride. The first step of the coupled reactions involves the hydrolysis of triglyceride by lipase to produce glycerol and fatty acids. Glycerol is a reactant in 1 of 2 enzymatic sequences for the final measurement of triglycerides. Fatty acids are not easily measured. Pre-betalipoprotein is the source of a large portion of endogenous triglycerides, but is not produced in enzymatic methods of triglyceride analysis. Phospholipids are separate from triglycerides although similar. They contain 2 esterified fatty acids and a phospholipid group such as choline on the glycerol molecule Thus, they are more complex than triglycerides and not a by-product of enzymatic hydrolysis with lipase.
Which of the following methods for quantitation of high-density lipoprotein is most suited for clinical lab use?
a. Gomori procedure
b. homogeneous
c. column chromatography
d. agarose gel electrophoresis
b. homogeneous
The high-volume HDL method is homogenous or direct. This method uses antibodies or complexing agents, such as cyclodextrin, to mask or consume non-HDL cholesterol lipids but does not require a separation step.
The indirect (2-3 step) method required separates pre-treatment and centrifugation to remove interferants and non-HDL cholesterol lipids. The Gomori procedure has been used with acid phosphatase or uric acid but is more currently associated with trichrome histological staining of muscle tissue.
Column chromatography is a purification step prior to separation by ultracentrifugation, a research method for lipoprotein separation.
Agarose gel electrophoresis has been used historically for separation of lipoproteins including HDL but is tedious, laborious and not used routinely.
Hemoglobin A1c represents:
a. valine substitution for glutamine at the 6th position of the beta chain of hemoglobin
b. ketone formation due to hydrolysis of the alpha and beta C-terminus forming an abnormal hgb
c. glycosylation of valine in the polypeptide N-terminus of the polypeptide chains of hemoglobin
d. glucose reduction in the presence of oxygen at the N-terminus of the polypeptide chains of hgb
c. glycosylation of valine in the polypeptide N-terminus of the polypeptide chains of hemoglobin
HbA1c is the addition of glucose (glycation) to the N-terminal valine of the B-chain
HbA.
The principle of the occult blood test depends
a. coagulase ability of blood
b. oxidative power of atmospheric oxygen
c. hydrogen peroxide in hemoglobin
d. peroxidase-like activity of hemoglobin
d. peroxidase-like activity of hemoglobin
Hemoglobin has endogenous peroxidase activity that is capable of oxidizing guaiac in the presence of hydrogen peroxide to a blue product
A breakdown product of hemoglobin is:
a. lipoprotein
b. bilirubin
c. hematoxylin
d. Bence Jones protein
b. bilirubin
Hemoglobin metabolism breakdown product is bilirubin
Hemoglobin S can be separated from hemoglobin D by:
a. electrophoresis on a different medium and acidic pH
b. hgb A2 quantitation
c. electrophoresis at higher voltage
d. Kleihauer-Betke acid elution
a. electrophoresis on a different medium and acidic pH
Agarose electrophoresis at ph 6.4 using a citrate buffer will separate H6S from 45D
On electrophoresis at alkaline pH, which of the following is the slowest migrating hemoglobin?
a. HbA
b. HbS
c. HbC
d. HbF
c. HbC
At alkaline pH, hemoglobins migrate according to electrical charge with HbH moving the fastest (closest to the anode) and HbC moving the slowest
The hemoglobin that is resistant to alklai (KOH) denaturation is:
a. A
b. A2
c. C
d. F
d. F
Fetal hemoglobin may be quantitated using NaOH or KOH based on the principle that it is resistant to alkali denaturation
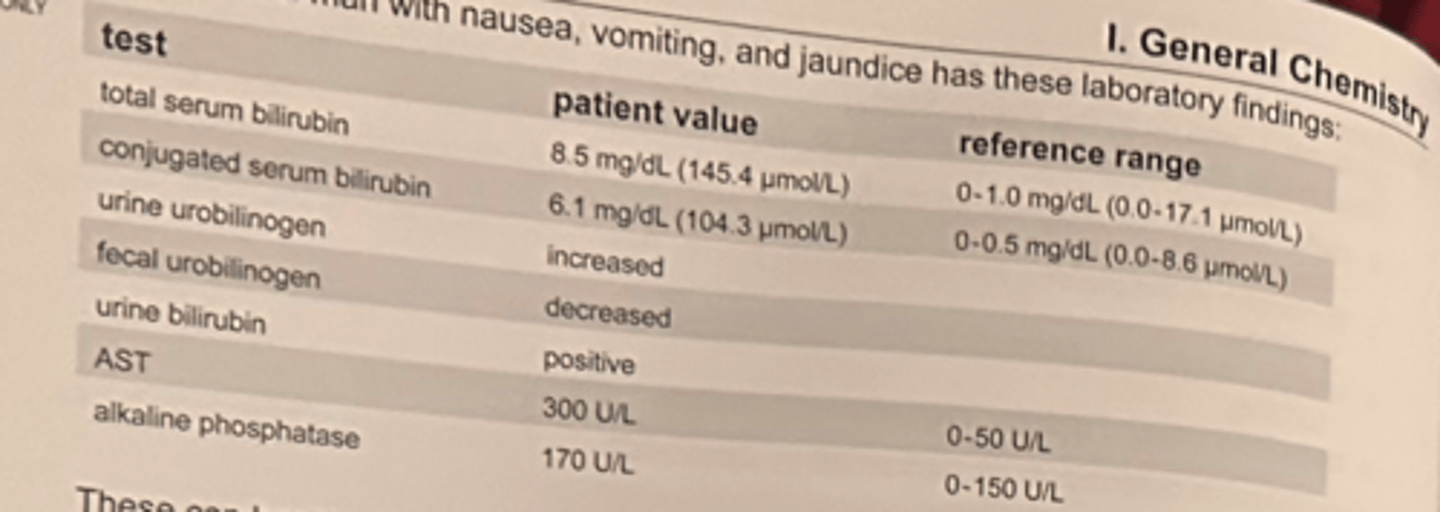
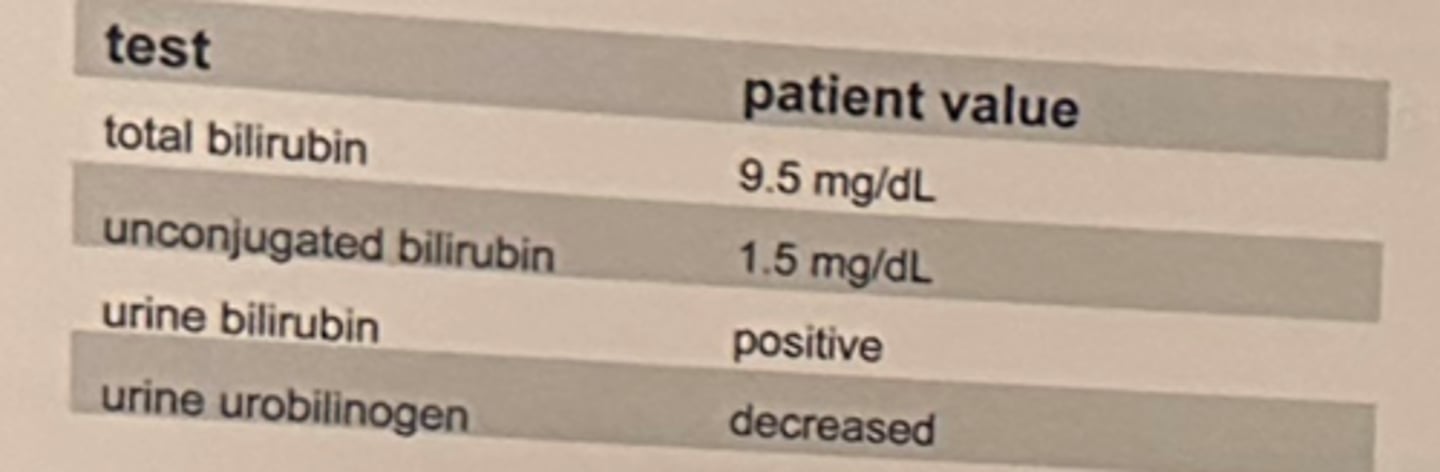
The bilirubin results show in the table are obtained on a patient.
Given the controls are within range each day, what is a probable explanation for the result on day 4?
a. no explanation necessary
b. serum, not plasma, was used for testing
c. specimen had prolonged exposure to light
d. specimen was hemolyzed
c. specimen had prolonged exposure to light
Light-exposed bilirubin is reduced by intestinal microbes to form urobilinogen
Urobilinogen is formed in the:
a. kidney
b. spleen
c. liver
d. intestine
d. intestine
Unconjugated bilirubin is reduced by intestinal microbes to form urobilinogen.
In bilirubin determinations, the purpose of adding a concentrated caffeine solution or methyl alcohol is to:
a. allow indirect bilirubin to react with color reagent
b. dissolve conjugated bilirubin
c. precipitate protein
d. prevent any change in pH
a. allow indirect bilirubin to react with color reagent
principle of diazo reaction with unconjugated bilirubin; reaction with caffeine solution or methyl alcohol makes the unconjugated bilirubin soluble, allowing it to react with the diazo reagent
If the total bilirubin is 3.1 mg/dL (53.0 micromol/L) and the conjugated bilirubin is 2.0 mg/dL (34.2 micromol/L), the unconjugated bilirubin is:
a. 0.5 mg/dL (8.6 micromol/L)
b. 1.1 mg/dL (18.8 micromol/L)
c. 2.2 mg/dL (37.6 micromol/L)
d. 5.1 mg/dL (87.2 micromol/L)
b. 1.1 mg/dL (18.8 micromol/L)
total bilirubin = (direct) conjugated bilirubin + (indirect) unconjugated bilirubin = 3.1 - 2.0 = 1.1
The principle of the tablet test for bilirubin in urine or feces is:
a. reaction between bile and 2,4-dichloronitrobenzene to make a yellow color
b. liberation of oxygen by bile to oxidize orthotolidine to make a blue-purple color
c. chemical coupling of bile with a diazonium salt to make a brown color
d. chemical coupling of bilirubin with a diazonium salt to make a purple color
d. chemical coupling of bilirubin with a diazonium salt to make a purple color
In urine, conjugated bilirubin is reacted with diazo tablet to form a purple color
Ten heparinized plasma samples were assayed for bilirubin by 1) Jendrassik-Grof method on analyzer 1, and by 2) the Evelyn-Malloy method on analyzer 2, in a method comparison study. The results were all 10 - 20% higher from analyzer 2 most likely because:
a. caffeine-benzoate stabilizer in analyzer 2 prevented falsely decreased results as found in analyzer 1
b. fibrinogen in the plasma samples caused falsely decreased results in the Jendrassik-Grof method
c. alcohol reagents in method 2 cause precipitation of proteins and increased background turbidity
d. hemolysis caused greater interference in method 1 than in method 2
c. alcohol reagents in method 2 cause precipitation of proteins and increased background turbidity
Jendrassik-Grof (method 2) is not affected by turbidity because it uses a serum blank
Serial bilirubin determinations performed by Jendrassik-Grof are charted below.
Day Collected Assayed Result
1 7 AM 8 AM 14.0 mg/dL (239.4 pmol/L)
2 7 AM 6 PM 9.0 mg/dL (153.9 pmol/L)
3 6 AM 8 AM 15.0 mg/dL (256.5 pmol/L)
The best explanation for the results is:
a: sample on day 2 has mild hemolysis and hemoglobin deterioration
b: sample on day 2 has exposure to light
c: sample on day 2 shows normal day to day variation
d: reagent deterioration is evident on day 3
b. sample on day 2 has exposure to light
Light-exposed bilirubin is reduced 30-50% per hour, while hemolysis my interfere depending on the method
In the liver, bilirubin is converted to:
a. urobilinogen
b. urobilin
c. bilirubin-albumin complex
d. bilirubin diglucuronide
d. bilirubin diglucuronide
Bilirubin is conjugated with glucuronic acid to produce bilirubin diglucuronide
In which of the following disease states is conjugated bilirubin a major serum component?
a. biliary obstruction
b. hemolysis
c. neonatal jaundice
d. erythroblastosis fetalis
a. biliary obstruction
Intrahepatic biliary atresia in the newborn can also cause conjugated hyperbilirubinemia, while in the adult it is likely due to biliary obstruction or hepatitis.
Kernicterus is an abnormal accumulation of bilirubin in:
a. heart tissue
b. brain tissue
c. liver tissue
d. kidney tissue
b. brain tissue
Definition of kernicterus: High concentrations of unconjugated bilirubin that passes the immature blood-brain barrier of the newborn
In which of the following conditions does decreased activity of glucuronyl transferase result in increased unconjugated bilirubin and kernicterus in neonates?
a. Gilbert disease
b. Rotor syndrome
c. Dubin-Johnson syndrome
d. Crigler-Najjar syndrome
d. Crigler-Najjar syndrome
There are several forms of Crigler-Najjar syndrome, but they each result in abnormal metabolism of bilirubin due to absence or deficiency of UDP-glucronyltransferase
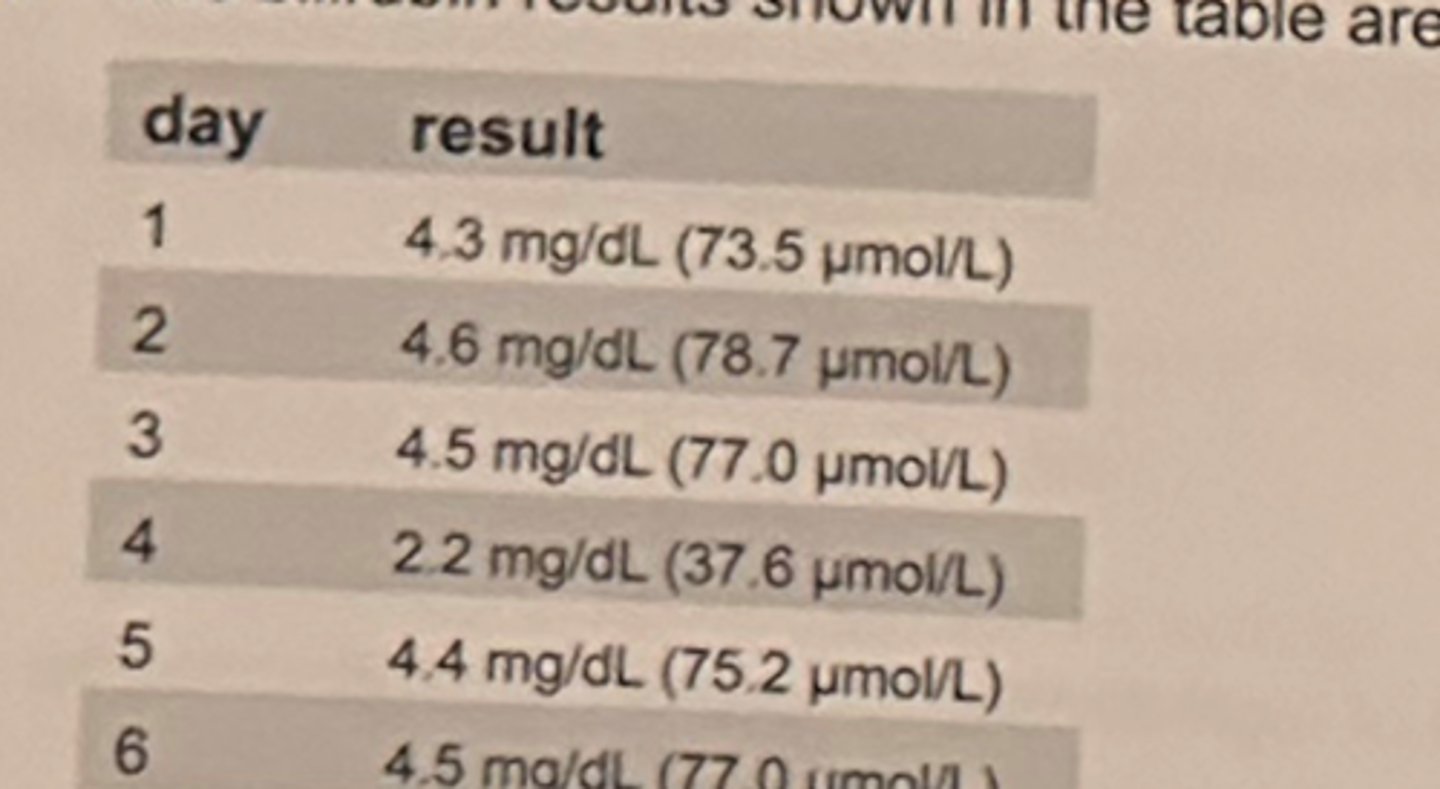
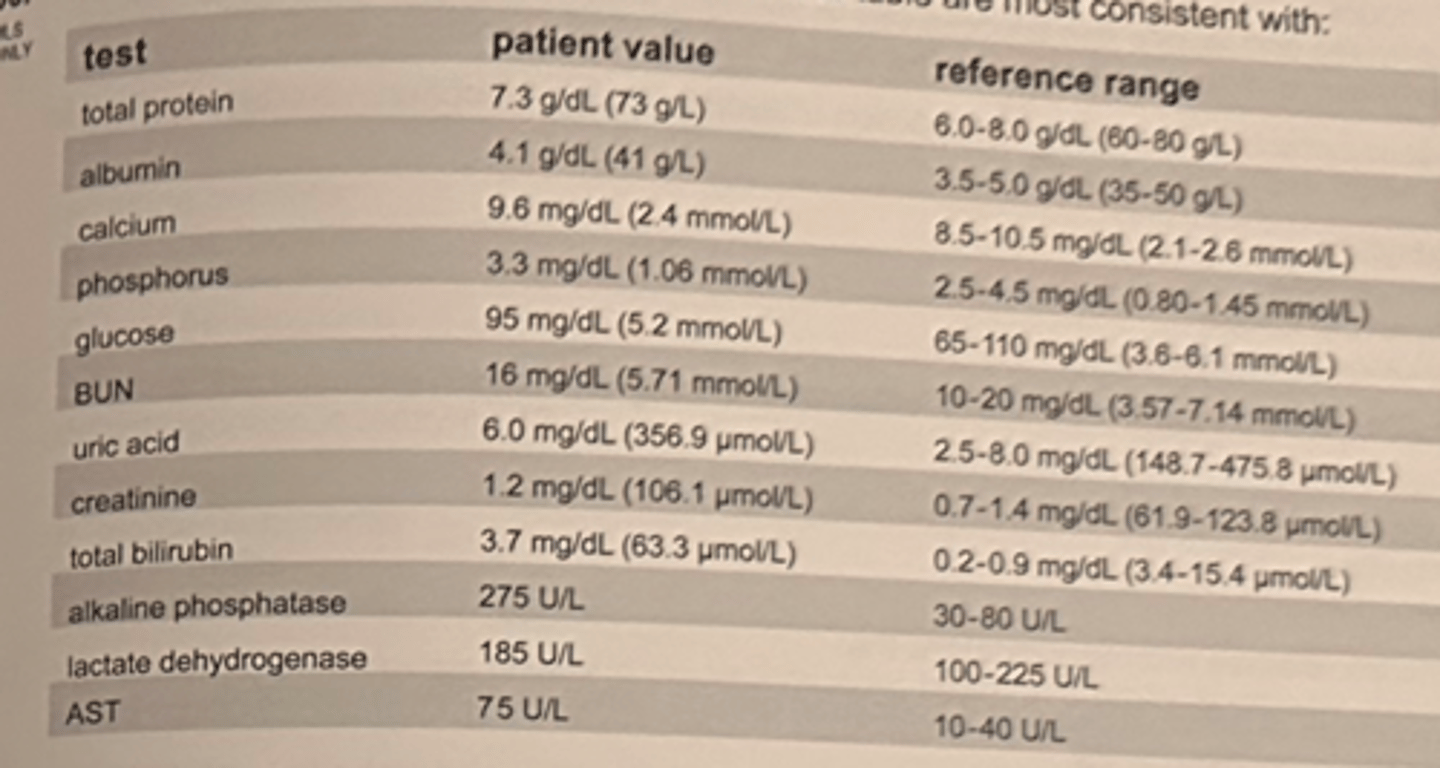
c. conjugated hyperbilirubinemia, probably due to hepatocellular disease
The results point to hepatocellular disorder and high elevated AST but near normal alkaline phosphatase, typical of acute hepatitis
A 21-year-old man with nausea, vomiting, and jaundice has the lab findings in the table.
These can best be explained as representing:
a. unconjugated hyperbilirubinemia, probably due to hemolysis
b. unconjugated hyperbilirubinemia, probably due to toxic liver damage
c. conjugated hyperbilirubinemia, probably due to hepatocellular disease
d. conjugated hyperbilirubinemia, probably due to hepatocellular obstruction
A stool specimen that appears black and tarlike should be tested for the presence of:
a. occult blood
b. fecal fat
c. trypsin
d. excess mucus
a. occult blood
Bleeding from upper GI causes digested blood to appear as dark and tarry in feces. Mucus and fecal fat may be visible in feces as an oily appearance.
What substance gives feces its normal color?
a. uroerythrin
b. urochrome
c. urobilin
d. urobilinogen
c. urobilin
Bile pigments (uro-, meso-, stercobilin) are found in feces. The precursors are urobilinogens, which are oxidized to form the bile pigments.
A condition in which erythrocyte protoporphyrin is increased is:
a. acute intermittent porphyria
b. iron deficiency anemia
c. porphyria cutanea anemia
d. acute porphyric attack
b. iron deficiency anemia
The definitive diagnosis for hereditary coproporphyria (HCP) is a markedly increased:
a. urine delta-aminolevulinic acid (ALA)
b. urine porphobilinogen (PBG)
c. fecal coproporphyrin III
d. erythrocyte protoporphyrin
c. fecal coproporphyrin III
A fresh urine sample is received for analysis for "porphyrins" or "porphyria" without further information or specifications. Initial analysis should include:
a. porphyrin screen and quantitative total porphyrin
b. quantitative total porphyrin and porphobilinogen screen
c. porphyrin and porphobilinogen screen
d. porphobilinogen screen and ion-exchange analysis for porpobilinogen
c. porphyrin and porphobilinogen screen
Which of the following enzyme of heme biosynthesis is inhibited by lead?
a. delta-aminolevulinate dehyratase
b. porphobilinogen synthase
c. uroporphyrinogen synthase
d. bilirubin synthetase
a. delta-aminolevulinate dehyratase
In amniotic fluid the procedure used to detect hemolytic disease of the newborn is:
a. measurement of absorbance at 450nm
b. creatinine
c. lecithin/sphingomyelin ratio
d. estriol
a. measurement of absorbance at 450nm
Hemoglobin S can be separated from hemoglobin D by which of the following methods?
a. citrate agar gel electrophoresis at pH 5.9
b. thin-layer chromatography
c. alkali denaturation
d. agarose gel electrophoresis at pH 8.4
a. citrate agar gel electrophoresis at pH 5.9
Before unconjugated bilirubin can react with Ehrlich diazo reagent, which of the following must be added?
A. acetone
B. ether
C. distilled water
D. caffeine
D. caffeine
The most widely used methods for bilirubin measurement are those based on the:
a. Jaffe reaction
b. Schales and Schales method
c. 8-hydroxyquinoline reaction
d. Jendrassik-Grof method
d. Jendrassik-Grof method
In the Evelyn-Malloy method for the determination of bilirubin, the reagent that is reacted with bilirubin to form a purple azobilirubin is:
a. dilute sulfuric acid
b. diazonium sulfate
c. sulfobromophthalein
d. diazotized sulfanilic acid
d. diazotized sulfanilic acid
In the Jendrassik-Grof method for the determination of serum bilirubin concentration, quantitation is obtained by measuring the green color of:
a. azobilirubin
b. bilirubin glucuronide
c. urobilin
d. urobilinogen
a. azobilirubin
In the Jendrassik-Grof reaction for total bilirubin, alkaline tartrate is added to:
a. form diazo bilirubin, a reddish chromogen
b. eliminate many spectrophotometric interferences
c. act as an accelerator
d. react with delta-bilirubin
b. eliminate many spectrophotometric interferences
a. prehepatic
The lab results shown in the table are obtained on a patient suspected have liver disease.
The type of jaundice would be classified as:
a. prehepatic
b. viral hepatic
c. cirrhotic hepatic
d. post hepatic
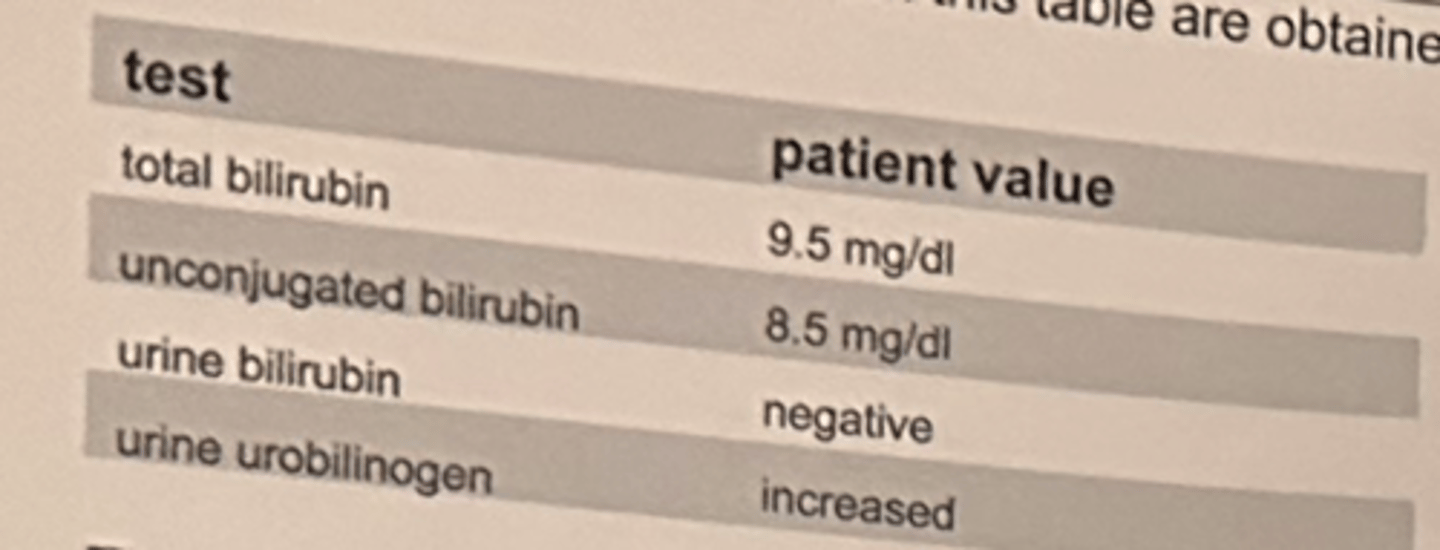
d. posthepatic
The lab results shown in the table are obtained on a patient suspected to have liver disease.
The type of jaundice would be classified as:
a. prehepatic
b. viral hepatic
c. cirrhotic hepatic
d. posthepatic
A quantitative measurement of urobilinogen uses the following reagent:
a. diazo
b. DMSO
c. Erhlich
d. Ferric chloride
c. Erhlich
c. common bile duct stone
The results the biochemical profile shown in the table are most consistent with:
a. viral hepatitis
b. hemolytic anemia
c. common bile duct stone
d. chronic active hepatitis
The most specific enzyme test for acute pancreatitis is:
a. acid phosphatase
b. trypsin
c. amylase
d. lipase
d. lipase
Which of the following enzymes are used in the diagnosis of acute pancreatitis?
a. amylase (AMS)
b. aspartate aminotransferase (AST)
c. gamma-glutamyl transferase (GGT)
d. lactate dehydrogenase (LD)
a. amylase (AMS)
Which of the following enzymes catalyzes the conversion of starch to glucose and maltose?
a. malate dehydrogenase (MD)
b. amylase (AMS)
c. creatine kinase (CK)
d. isocitric dehydrogenase (ICD)
b. amylase (AMS)
Which of the following sets of results would be consistent with macroamylasemia?
a. normal serum amylase and elevated urine amylase values
b. increased serum amylase and normal urine amylase values
c. increased serum and urine amylase values
d. normal serum and urine amylase values
b. increased serum amylase and normal urine amylase values
In acute pancreatitis, the following results would be expected:
a. LD isoenzyme 1 elevates higher than LD isoenzyme 2 within 72 hours
b. lipase elevates within 4-8 hours of an attack, peaks at 24 hours and normalizes in 48 hours
c. amylase and lactate rise successively in the first 24 hours and stay elevated 4 days
d. amylase and lipase elevate in a few hours, but amylase normalized within 3 days
d. amylase and lipase elevate in a few hours, but amylase normalized within 3 days
What enzyme is measured in the reaction of maltoheptaose-nitrophenol producing glucose fragments and 4-nitrophenol?
a. amylase
b. hexokinase
c. pyruvate kinase
d. alkaline phosphatase
a. amylase
Aspartate amino transferase (AST) is characteristically elevated in diseases of the:
a. liver
b. kidney
c. intestine
d. pancreas
a. liver