6.0 Clostridiodes difficile C.diff
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
20 Terms
Clostridiodes difficile C diff
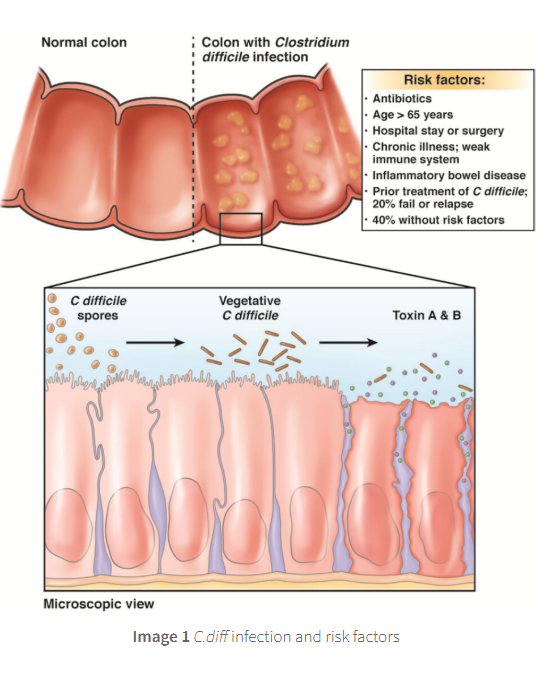
gram positive spore forming anaerobic bacteria that
thrives without oxygen
and can survive externally to the host as spores
c diff releases 2 toxins A + B
which damages the colons lining and triggers inflammation and diarrhoea
in the gut good microbes are protective from C diff colonisation
however using broad spectrum antibiotics and gastric acid supression can lead to an imbalance in this protection allowing C diff to overgrow and cause disease
the orgnaism is carried asymptomaticalled, colonised in up to 5% od healthy adults
clinically significant disease almost always follows disruption of the protective gut microbiota
watch video😛
infected or colonised patients shed spores via faeces
spores survive routine cleaning and are resistant to alcohol hand rub,
soap and water must be used by staff members for appriroate hand hygine
alongside protective personal equipment PPF including gloves n aprons
patients admitted to hospital with C diff infecitions CDI are isolated within side rooms to limit spead to other patients
transmission is faecal-oral and amplified in environemnts where patients share bathrooms, equpirment or stadd like hospiutals and long term care facilities
spores can persist on surfaces for months and transmission may occur when apprioriate cleaning standards are not followed
prevention through environmental cleaning and disinfection is vital, chlorine containing cleaning product are required
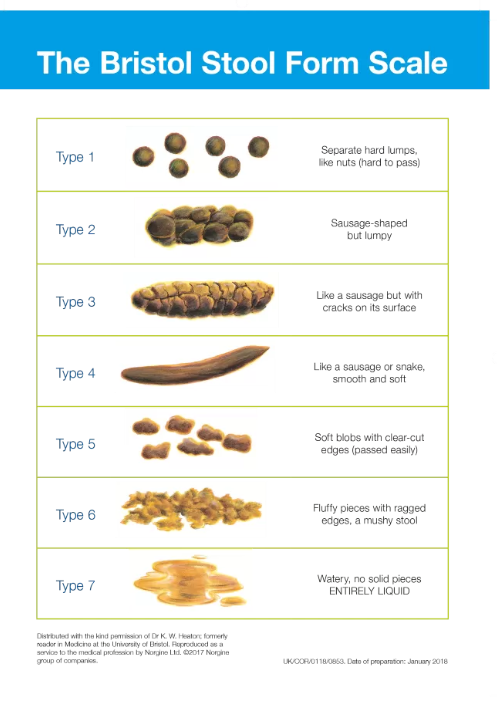
typical symptoms
watery diarrhoea, type 6-7
lower abdominal cramping
low grade fever
STINKYYYYYYYYYY DOOKIE
labratory clues
raised white-cell count
severe cases, raised serum creatine from dehydration
severe disease
profuse diarrhoea with raised white cell count
significant abdominal tenderness or distension
lactate > 2mmol L-1
fulminant/life threatening colitis
hypotension or shock
toxic megacolon or bowel perforation
potential progression to sepsis and miltiorgan failure
complications
dehdyration
toxic megacolon
bowel perforation
sepsis
dehdyration
can lead to significant fluid and electrolyte loss resulting in dehydration which can cause dangerously low blood pressure in severe cases n kidney failure
toxic megacolon
rare condition occurs when the colon becomes enlarged and unable to expel gas and stool
life threating as the colon can rupture and bacteria can enter the blood stream leading to sepsis
required emergency surgery
bowel perforation
c diff/ toxic megacolon can damage the lining of the colon causing a hole to form
leading to peritonisis a danger infection of the abdominal cavity
caused by bacteria leaking from the colon
sepsis
a life threatening condition where the body’s response to infection damages its own tissue organs
risk factors
Recent or prolonged antibiotic therapy (especially clindamycin, cephalosporins, fluoroquinolones, carbapenems)
aged 65+
Hospitalisation or long‑term care facility stay
Proton pump inhibitor (PPI) or H₂‑blocker use
immunosuppression (e.g., corticosteroids, chemotherapy, HIV infection, organ transplant drugs)
Gastrointestinal surgery or manipulation (including feeding tubes, colectomy, or endoscopic procedures)
Previous C. difficile infection