Respiratory System
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
Functions of Respiratory System
Provides for gas exchange
Regulates blood pH
Contains receptors for smell
Filters inspired air
Produces vocal sounds
Excretes small amounts of water and heat
Classification of Respiratory System Components
according to:
Structure:
Upper Respiratory System
Nose
Nasal Cavity
Pharynx
Lower Respiratory System
Larynx
Trachea
Bronchi
Lungs
Function:
Conducting Zone
Nose
Nasal Cavity
Pharynx
Trachea
Bronchi
Bronchioles
Terminal Bronchioles (end point)
Respiratory Zone
Respiratory Bronchioles
Alveolar Ducts
Alveolar Saccules (Sacs)
Pulmonary Alveoli
Note: Conducting zone filters, warms, moistens, passes air into respiratory zone; Respiratory zone is where gas exchange occurs
Related Branches of Medicine
Otorhinolaryngology:
diagnosis and treatment of ear, nose, throat disease
ENT
Pulmonology:
specializes in diagnosis and treatment of lung diseases
Nose
External Nose:
visible section of the nose
Bony Framework
nasal bones + frontal bone + maxillae (upper jaw)
Cartilaginous Framework
hyaline cartilage + fibrous connective tissue
External Nares/Nostrils
Internal Nose:
nasal cavity inside skull
Lateral Walls
walls formed from bone
Nasal Cavity
space in skull above oral cavity
Internal Nares
two openings from internal nose into pharynx
also called choanae
Olfactory Epithelium
External Nose Functions
Functions of Interior Structures:
Warming of Air
Moistening of Air
Filtering Incoming Air
Detecting olfactory stimuli
Modifying speech vibrations
as they pass through large, hollow, resonating chambers
Internal Nose
a large cavity in anterior aspect of skull
lies inferior to nasal bone
lies superior to oral cavity
Lateral Walls:
formed by:
Maxilla bone (upper jaw)
Ethmoid bone (at root of nose)
Lacrimal bone (eye socket)
Palatine bone (part of hard palate)
Inferior nasal conchae bones
Nasal Cavity:
Vestibule
entrance of nasal cavity; just after nostrils
lined with skin w/ hair follicles, sweat glands, sebaceous glands
filters out large dust particles
Nasal Septum
vertical partition
divides nose equally into left and right
anterior: hyaline cartilage
posterior: bone
Conchae
different from choanae
also called nasal turbinates
three pairs of bony projections
superior, middle, and inferior conchae
increases surface area
Internal Nares:
choanae
posterior to nasal cavity; opens into nasopharynx
Olfactory Epithelium:
also called olfactory receptors
superior portion of nasal cavity
Airflow Process in Nose
Air enters nostrils/external nares →
air passes through vestibule →
air is warmed by blood in capillaries as it whirls around conchae and meatuses →
mucus moistens air and traps dust →
cilia move mucus/trapped dust towards pharynx (where it can then be swallowed/spit)
Pharynx
muscular tube-like structure
connects nasal cavity + mouth to esophagus + larynx (voice box)
begins at internal nares
reaches until cricoid cartilage
Location:
posterior to nasal + oral cavity
superior to larynx
anterior to cervical vertebrae
Regions:
Nasopharynx:
immediately after nasal cavity; upper part
Oropharynx
led into from oral cavity; middle part
below nasopharynx
Laryngopharynx/Hypopharynx
bottom part
below both cavities
Pharynx Functions
conducts air from nasal cavity + mouth to larynx and trachea (breathing)
conducts food + liquid from oral cavity to esophagus (swallowing)
provides resonating chamber for speech production
houses tonsils
part of immune system, fight infections
Nasopharynx
uppermost part of pharynx
situated behind nasal cavity
passageway for air only
posterior wall contains pharyngeal tonsil
also called adenoid tonsil
lined with ciliated pseudostratified columnar epithelium
traps and removes dust + foreign matter
has 5 openings
2 internal nares
2 openings that lead into the auditory tubes
1 opening into oropharynx
Functions:
accepts air from nasal cavity
gathers clusters of mucus with dust particles
cilia proper mucus downwards towards laryngopharynx
shares some air with Eustachian Tubes (auditory tube)
balances air pressure between pharynx and middle ear
Oropharynx
located behind oral cavity
has only one opening, the fauces (opening from the mouth)
contains palatine and lingual tonsils
common passageway for food and air
lined with nonkeratinized stratified squamous epithelium
same as GI tract because also part of GI tract
Laryngopharynx
also called hypopharynx
lowest part of pharynx
situated behind the larynx (voice box)
common pathway for food and air
leads to esophagus, involved in swallowing process/deglutition
lined with stratified squamous epithelium
protects against mechanical/chemical irritation
begins at level of hyoid bone
opens into esophagus (inferiorly) and larynx (anteriorly)
Larynx
also called voice box
short passageway, connects laryngopharynx to trachea
pathway for air to travel when breathing
in the middle of the neck
anterior to esophagus
anterior to C4-C6 cervical vertebrae
Wall is composed of 9 cartilages
Epiglottis
Thyroid
Cricoid
Arytenoid (2)
Cuneiform (2)
Corniculate (2)
Epiglottis
primarily composed of elastic cartilage
large, leaf-shaped
closes the glottis
glottis = vocal cords + rima glottidis (the space between the cords)
when swallowing, larynx rises which pushes the leaf portion closed
prevents entry of food into larynx
“leaf” portion is superior, broad, unattached, and free to move up and down (like flap or trap door)
Thyroid Cartilage
also called the Adam’s Apple
largest cartilage in larynx
anterior region of neck, just below thyroid gland
shield-shaped, consists of two plate-like structures (laminae)
meet in the midline to form front portion of larynx
provide structural support and protection
house and protect the vocal cords
role in controlling tension of vocal cords
crucial for speech production
Cricoid Cartilage
ring of hyaline cartilage
forms inferior wall of larynx
serves as a landmark for making an emergency airway (cricothyrotomy)
Arytenoid Cartilage
small, triangle shaped segments of hyaline cartilage
situated at the upper, back edge of the cricoid cartilage
influence changes in tension and position of vocal cords
important for production of vocal sounds
Corniculate Cartilage
horn-shaped pieces of elastic cartilage
located at the apex of each arytenoid cartilage
supporting structure for the epiglottis
Cuneiform Cartilage
anterior to corniculate cartilage
club-shaped elastic cartilage
support the vocal folds
support the lateral aspects of the epiglottis
Structures of Vocal Production
Ventricular Folds
false vocal cords
superior to vocal folds
have protective function; cover the true vocal cords
hold breath against pressure when brought together
Vocal Folds
true vocal cords
inferior to ventricular folds
thicker and longer in males (due to androgens)
vibrate slowly
bands of elastic ligament stretch within
when air passes through them, sound is made
Rima Glottidis
space between vocal folds
Rima Vestibuli
space between ventricular folds
Laryngeal Sinus
lateral expansion of middle portion of laryngeal cavity
Laryngitis
inflammation of the larynx
Common Causes:
respiratory infection
irritants
Hoarseness or Loss of Voice:
potential consequence of laryngitis
caused by inflammation of vocal cords
can be permanent due to chronic inflammation (ex: due to smoking)
Laryngeal Cancer
almost exclusively found in smokers
Symptoms:
hoarseness
pain on swallowing
pain radiating to ear
Treatment:
radiation therapy
surgery
laryngectomy
surgical removal of larynx
leaves a hole in the throat
patient unable to speak without device afterwards
patients can no longer breathe normally (epiglottis removed)
must breathe through stoma (hole in neck)
Trachea
also called windpipe
tubular passageway for air
anterior to esophagus
extends from larynx to superior border of fifth thoracic vertebra (T5)
composed of 16-20 incomplete hyaline rings (C-Shaped)
C-Shaped Rings:
incomplete ring allows for slight expansion of esophagus into trachea when swallowing
semi-rigid support; prevents trachea from collapsing inwards
Tracheal Wall Layers:
from deep to superficial
mucosa
ciliated pseudostratified columnar epithelium
lamina propria of elastic and reticular fibers
submucosa
areolar connective tissue
seromucous glands and ducts
cartilaginous layer (hyaline)
adventitia (areolar connective tissue)
Tracheal Obstruction
Causes:
collapse of cartilage rings due to crushing injury to chest
inflammation of mucus membrane
accidental inhalation of foreign objects (ex: small toys, food particles, etc.)
cancerous tumors that protrude into airway
Management:
Tracheostomy:
operation, creates opening in trachea
short, longitudinal, incision inferior to cricoid cartilage
metal/plastic tracheal tube inserted into hole
Intubation:
tube inserted through mouth or nose; guided downwards through larynx & trachea
tube displaces blockages; also allows air to pass through
mucus causing obstruction may be suctioned out using tube
Bronchi
consists of right primary and left primary bronchi
right bronchi is more vertical, shorter, and wider
as such, an inhaled object is more likely to enter and lodge in the right primary bronchus
left and right primary bronchus enter left and right lung respectively
also contain incomplete hyaline cartilage rings
Carina:
also called tracheal carina
ridge/cartilaginous projection
point where trachea bifurcates into left and right primary bronchi
widening/distortion of carina is indicative of carcinoma
Path from Trachea to Bronchi Composition and Histology
Note:
approaching bronchi (downwards), cartilage decreases, smooth muscle increases
cartilage plates also tend to replace incomplete cartilage rings going downwards
approaching trachea (upwards), cartilage increases, smooth muscle decreases
Pathway:
Trachea → Primary Bronchi → Secondary Bronchi → Tertiary Bronchi → Bronchioles → Terminal Bronchioles
Pathway Histology:
From Trachea to Tertiary: ciliated pseudostratified columnar epithelium
Large Bronchioles: ciliated simple columnar epithelium with some goblet cells
Small Bronchioles: ciliated simple cuboidal epithelium with no goblet cells
Terminal Bronchioles: non-ciliated simple cuboidal epithelium
Bronchi Branches
left primary bronchi → left lung; right primary bronchi → right lung
upon entering lungs; divide into secondary (lobar) bronchi (one for each lobe)
right lung = 3 lobes
left lung = 2 lobes
Lobar bronchi further branch into tertiary (segmental) bronchi
supply specific segments within the lobes
10 in each lung, despite different lobe count
which then branch into bronchioles, which branch further repeatedly
eventually branch into terminal bronchioles
Lungs
paired, cone-shaped organs
located in thoracic cavity; protected by ribcage
pair is separated by heart and other structures in mediastinum
Right Lung:
consists of three lobes
Upper/Superior
Middle
Lower/Inferior
thicker, broader, but shorter than left lung
Left Lung:
consists of two lobes
Upper/Superior
Lower/Inferior
10% smaller than right lung
Note: if one lung collapses, the other may still function
Pleural Membrane
a double layer of serous membrane that encloses and protects each lung
Parietal Pleura:
superficial
lines the walls of the thoracic cavity
Visceral Pleura:
deep
covers the lungs
Pleural Cavity:
small space between the pleurae
contains a small amount of lubricating fluid that is secreted by the membranes
Related Conditions:
Pleuritis:
also called pleurisy
inflammation of pleura
Pleural Effusion:
abnormal accumulation of fluid in the pleural cavity
may be caused by persisting inflammation
Pneumothorax:
presence of air or gas in pleural cavity
Causes:
surgical opening of chest
stab or gunshot wounds
air accumulation can cause partial/complete collapse of lung
air takes space; presses down on lung causing collapse
Hemothorax:
presence of blood in pleural cavity
treatment: evacuation of blood from pleural space
Thoracentesis:
treatment method used to remove excess fluid/air from thoracic cavity
needle is inserted anteriorly through 7th intercostal space (space between ribs)
if inserted anywhere inferior to 7th, risk of accidentally hitting diaphragm
Lungs: Surface Anatomy
Base:
broad, concave surface
rests on diaphragm
extends downwards to level of the rib cage
can be felt just above costal margin
Apex:
rounded, superior portion
extends above clavicle into root of neck
can be palpated (examined by touch) just above medial third of clavicle
Cardiac Notch:
notch on the left lung
where the heart rests along the lung
anterior and inferior; can be palpated along left border of the sternum
Costal Surface:
surface of lungs that lays against the ribs
matches round curvature of the ribs
Mediastinal (Medial) Surface:
contains hilum
structure where bronchi, blood and lymph vessels, and nerves enter and exit
Fissures:
divide the lobes
Right Lung:
Oblique: separates upper and middle
Horizontal: separates middle and lower
Left Lung:
Oblique: separates upper and lower
Lungs: Lobes and Segments
Right Lung = 3 Lobes
Left Lung = 2 Lobes
each lobe gets its own secondary bronchus
Right Lobe gets superior, middle, and inferior secondary bronchi
Left Lobe gets superior and inferior secondary bronchus
Secondary Bronchi give rise to tertiary bronchi
there are 10 in each lung, irrespective of how many lobes they have
each tertiary bronchus supplies a bronchopulmonary segment
branch into bronchioles
Bronchopulmonary Segments:
also called pulmonary segments
both a functional and anatomical unit of the lung
supplied by a tertiary bronchus
surrounded by connective tissue septa
have own segmental veins that drain into the pulmonary veins
contain small compartments called lobules
Lungs: Lobules
small, discrete, pyramid shaped unit
surrounded by elastic connective tissue
contains:
1 lymphatic vessel
1 arteriole
1 venule
1 terminal bronchiole branch
terminal bronchioles then branch into smaller respiratory bronchioles
which then subdivide into several alveolar ducts
Lungs: Alveoli
Alveoli:
tiny, ballon-like structures
where gas exchange takes place
around 300 million in the lungs
provides surface area of 70 m2
Alveolar Sac:
clusters of alveoli in the lungs
2 or more alveoli that share an opening
terminal ends of the respiratory tree
responsible for majority of gas exchange
Alveolar Ducts:
connect respiratory bronchioles to alveolar sacs
Alveolar Wall:
consists of two types of alveolar epithelial cells
Type I:
extremely flat, thin
predominant; form most of wall
main site of gas exchange
Type II:
interspersed among Type I cells
secrete alveolar fluid
keeps surface between air and cells moist
produce surfactant
reduce alveolar fluid surface tension
reduces tendency of alveoli to collapse
also called septal cells
also contain alveolar macrophages (dust cells)
wandering phagocytes
remove fine dust, particles, other debri
Alveolar Fluid:
thin layer of fluid; lines inner surface of alveoli
maintains proper function; facilitates gas exchange
Composition:
water
surfactant
electrolytes
proteins
immune cells
Respiratory Membrane
the membrane through which gas must diffuse in gas exchange
allows rapid diffusion of gasses between lungs and blood
includes alveolar and capillary walls
Consists of four layers:
Alveolar Wall (with Type I and II cells)
Epithelial Basement Membrane
Capillary Basement Membrane
Endothelial Cells of Capillaries
Aqours Third Years being Precious

Basic Respiration Processes
Pulmonary Ventilation:
also called breathing
the inhalation and exhalation of air
between the alveoli and the environment
External Respiration:
also called pulmonary respiration
involves gas exchange between alveoli and pulmonary capillaries of the respiratory membrane
blood is oxygenated, and loses CO2
Internal Respiration:
also called tissue respiration
the exchange of gasses between systemic capillaries and tissue cells
blood loses oxygen and gains CO2
Pulmonary Ventilation
air flows between atmosphere and lungs due to pressure differences
pressure created by contraction and relaxation of respiratory muscles
Air moves from high to low pressure
into lungs when pressure is greater in atmosphere
out of lungs when pressure is greater in lungs
relies on inhalation and exhalation
Inhalation
also called breathing in or inspiration
an active process, involving muscular contraction
lung pressure is decreased by increasing the lung volume
accomplished via contraction of diaphragm and external intercostals
Diaphragm
a dome-shaped skeletal muscle
while ordinarily involuntary, can be made voluntary
forms the floor of the thoracic cavity
most important muscle for respiration
accounts for about 75% of air that enters the lungs during quiet breathing
normally curved, but contraction flattens it
increases vertical volume of thoracic cavity
Normal Quiet Inhalation:
descends about 1 cm
generates pressure difference of 1-3 mmHg
inspires about 500 mL of air
Forceful Inhalation:
ex: due to physical activity
descends about 10 cm
generates pressure difference of 100 mmHg
inspires about 2-3 L of air
External Intercostals
muscle between the ribs
contraction elevates the ribs
increases anteroposterior and lateral diameters of the chest cavity
increases chest cavity volume
responsible for about 25% of air that enters the lungs during breathing
Intrapleural and Alveolar Pressure
Intrapleural Pressure:
as thoracic cavity expands, parietal pleura is pulled outwards
the visceral pleura is pulled alongside it, which also pulls the lungs
Pressure between the two Pleural Layers:
before inhalation: 756 mmHg
after inhalation: 754 mmHg
Alveolar Pressure:
also called intrapulmonic pressure
as lung volume increases, the pressure within the lungs decreases
Pressure Inside Lungs:
before inhalation: 760 mmHg
after inhalation: 758 mmHg
Atmospheric Pressure is 760 mmHg (1 atm)
Pressure of Lungs during Exhalation:
Intrapleural: 756 mmHg
Alveolar: 762 mmHg
Specific numbers will not be asked for in exam
Accessory Muscles of Inhalation
participate only during forceful inhalation
increase the size of the thoracic cavity (by increasing diameter)
Sternocleidomastoid: elevate the sternum
Scalene Muscles: elevate the first two ribs
Pectoralis Minor Muscles: elevate the third, fourth, and fifth ribs
Exhalation
also called breathing out or expiration
a more passive process
due to pressure differences, and higher pressure in lungs
elastic recoil of muscles reduce volume of thoracic cavity
no muscular contraction is involved
simply due to natural tendency spring back after being stretched
diaphragm relaxes = dome moves up
external intercostals relax = ribs depressed
resulting alveolar pressure: 762 mmHg
Forceful Breathing:
exhalation becomes active during forceful breathing only
requires contraction of muscles of exhalation
Abdominal Muscles
attached to the ribs
move inferior ribs downwards
compresses abdominal visceral
Internal Intercostals
pulls the ribs inferiorly
Factors that Affect Pulmonary Ventilation
Surface Tension of Alveolar Fluid
Compliance of the Lungs
Airway Resistance
Surface Tension of Alveolar Fluid
due to secretions of Type II alveolar cells
produces thin layer of alveolar fluid
coats the luminal surface of the alveoli
fluid surface tension pulls alveoli in (tries to minimize surface area)
tension allows alveoli to assume the smallest possible diameter (without collapsing)
in inhalation, surface tension must be overcome to expand lungs
in exhalation, surface tensions accounts for 2/3 of the lung’s elastic recoil which decreases lung volume
Surfactant in Alveolar Fluid:
reduces surface tension
prevents alveolar collapse at the end of each exhalation
reduces pressure needed for subsequent alveolar inflation
Surface Tension Related Conditions
Respiratory Distress Syndrome (RDS):
breathing disorder in premature neonates
since lungs are the last organ to develop
since lungs are not needed as fetus
lack of surfactant causes surface tension to increase
leads to alveoli not remaining open
greater effort is needed per inhalation
Symptoms:
tachypnea (high respiratory rate)
nasal flaring
harder breathing = more pressure per breath
causes nostrils to widen
a sign of use of accessory muscles
grunting during exhalation
blue skin color
intercostal, subcostal, or subxiphoid retractions
muscles pull back farther
skin is also pulled towards the ribs
can see outline of ribs as a result
Diagnosis:
clinical examination +
chest radiographs +
blood tests
Management:
for mild: O2 support
for severe: intubate, give surfactant
surfactant available as intratracheal solution
Compliance of the Lungs
stretchiness of lung and chest walls
highly compliant = can expand easily
low compliance = lungs resist expansion
related to elasticity and surface tension
lungs normally have high compliance
elastic fibers in lung are easily stretched
surfactant reduces surface tension
Conditions Where Compliance is Decreased:
Pulmonary Tuberculosis (scarring of lung tissue)
Pulmonary Edema
Surfactant Deficiency
Paralysis of Intercostal Muscles (impedes lung expansion)
Airway Resistance
airflow depends on both pressure difference and resistance
walls of airway (bronchioles): offer some resistance to normal flow in and out of lungs
Airway Diameter:
high determinant of resistance
regulated by contraction/relaxation of smooth muscle in airway
large diameter = decreased resistance
small diameter = increased resistance
Related Conditions:
Obstructive Lung Diseases:
Bronchial Asthma
smooth muscle constricts
alveolar wall is thickened and inflamed
fluid secretion increases
COPD
Breathing Patterns
Eupnea:
normal pattern; quiet breathing
shallow, deep, or combined shallow and deep breathing
unlabored and effortless
Costal Breathing:
shallow (chest) breathing
upward & outward movement of the chest due to contraction of external intercostal muscles
Diaphragmatic Breathing:
deep (abdominal) breathing
outward movement of the abdomen due to contraction and descent of diaphragm
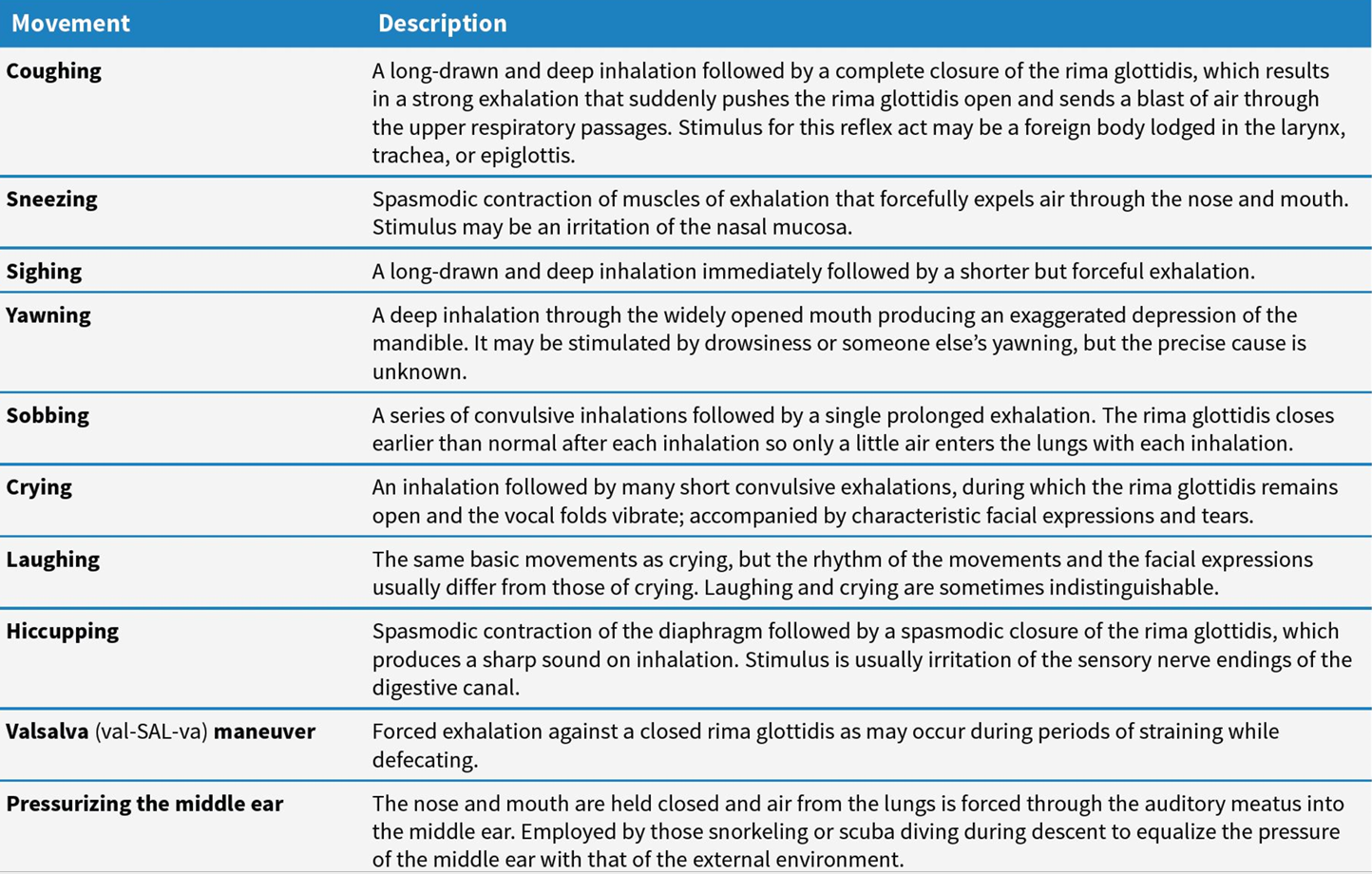
Modified Breathing
Tidal Volume (TV)
volume of each tide of respiration (every quiet/normal breath)
in one normal inhale/exhale
around 500 mL
350 mL - reaches the respiratory zone
150 mL - only reaches the conducting zone (the anatomic dead space)
Inspiratory Reserve Volume (IRV)
volume that can be inhaled on maximal inspiration (after tidal volume)
after a normal inhalation, you can inhale even more
around 3.1 L
deep breath = 500 mL (TV) + 3.1 L (IRV)
note: values in textbook are based on Caucasian individuals
Expiratory Reserve Volume (ERV)
volume that can be exhaled on maximal expiration after tidal volume
after quiet inhalation (TV) you can exhale even more
around 1.2 L
note: lungs are never empty of air; not collapsed and stay patent
FEV1
test for forced expiratory volume in 1 second
in one second, inhale as hard and blow as hard as you can into a tube
then will check how much volume you exhaled
changes in obstructive diseases
useful in COPD monitoring
Residual Volume
even at maximum exhalation, some air is still left in
prevents collapse of lungs; also still allows gas exchange when breathing out
around 1.2 L
though tends to be slightly more than ERV
Lung Capacities
comparison of the volumes
Inspiratory Capacity (IRC):
how much you can breathe in
Tidal Volume + Inspiratory Reserve Volume
Functional Residual Capacity (FRC)
total amount of air that is available for gas exchange after quiet exhalation
hence, functional, because it still participates in gas exchange
Expiratory Reserve Volume + Residual Volume
Vital Capacity (VC)
Inspiratory Reserve + Tidal Volume + Expiratory Reserve
the total amount of air the lungs can accommodate
Total Lung Capacity:
around 6 L
Minute Ventilation:
total amount of air inspired and expired every minute
Normal Respiratory Rate: 12 breaths per minute (12-20 usually)
Formula: (Breaths/Minute) x (Liter/Breath)
or in other words: Respiratory Rate x Tidal Volume
Alveolar Ventilation:
total amount of air reaching the respiratory zone every minute
External Respiration
exchange of gas between alveoli and pulmonary capillaries
Goal: convert Deoxy blood → Oxy blood
Flow of Oxygen:
alveoli to pulmonary capillaries
105 mmHg → 40 mmHg (alveoli has higher oxygen partial pressure)
flows from high to low (alveoli has higher because it just flowed in)
Flow of Carbon Dioxide:
Pulmonary Capillaries → Alveoli
45 mmHg → 40 mmHg
higher in body because it produces it
Internal Respiration
exchange of gas between systemic capillaries and tissue cells
Flow of Oxygen:
Systemic Caps → Tissue Cells
100 mmHg → 40 mmHg
Flow of CO2:
tissue cells → Systemic Caps
45 mmHg → 40 mmHg
Factors Affecting Pulmonary and Systemic Gas Exchange
difference of partial pressure of gasses
similar to concentration gradient in diffusion
surface area available for gas exchange
diffusion distance
molecular weight and solubility of gasses
lower MW and more lipophilic can diffuse through membranes better
Note: partial pressure is contribution of that specific gas to the total pressure of the gas mixture
relative to gas concentration
Partial Pressure Difference
larger pressure difference = faster diffusion of gas
Affected by the Following:
Altitude:
high altitudes decrease pressure difference due to thinner air
Exercise
increases respiratory rate and decreases blood oxygen
increases pressure difference
Morphine (Anesthesia)
decreases respiratory input
slow ventilation = less gas
Surface Area for Gas Exchange
larger surface area = faster rate of diffusion
alveoli: around 70 m2 surface area
Emphysema:
part of COPD
destruction of alveolar walls
decreases surface area = slower rate of gas exchange
Diffusion Distance
higher diffusion distance = slower rate of diffusion
respiratory membrane originally very thin; makes diffusion easy
however conditions may increase distance:
Pulmonary Edema
Molecular Weight of Gas
the lower the MW = faster rate of diffusion
MW of O2 is less than CO2
as such, O2 should diffuse faster (if only considering MW)
O2 diffuses across the membrane about 1.2 times faster than CO2
Solubility of Gasses
higher solubility = faster rate of diffusion
Solubility of CO2 is higher than of O2
solubility of CO2 in respiratory fluids is about 24 times greater than O2
Net effect: net outward CO2 is around 20x more rapid than inward O2
Conditions:
Emphysema: causes hypoxia and hypercapnia
Oxygen-Hemoglobin Dissociation Curve
some gasses dissolve in the blood, but most travel via hemoglobin
X Axis: PO2 (partial pressure of Oxygen)
Y Axis: Percent saturation of Hemoglobin
As O2 increases, saturation should increase
Follows sigmoidal curve; blunts near the end
More linear at the center
fully saturated hemoglobin means all hemoglobin is converted to “oxyhemoglobin”
partially saturated means mixture of oxyhemoglobin and reduced hemoglobin
Oxygen Transport
around 98.5% of O2 in blood is hemoglobin bound
1.5% dissolved in plasma
Resting Condition: only 25% O2 unloads fro Hb and is used by tissue
rest is in reserve
Factors Affecting Hb affinity for O2:
partial pressure of O2
Acidity; Partial pressure of CO2
Temperature
BPG
O2 Transport Factors
PO2
most important factor that determines how much O2 binds to Hb
higher PO2 = Higher binding
same as the disassociation curve
Acidity:
as acidity increases, affinity for Hgb for O2 decreases
acidity comes from CO2 (that becomes carbonic acid)
that way, oxygen releases when and where CO2 is high
called the Bohr Effect
increase in H+ can cause O2 to unload
binding of O2 can cause H+ to unload from Hgb
Hemoglobin also acts as a blood buffer
Partial Pressure of CO2:
high CO2 decreases affinity of Hgb for O2
this is in addition to the H+ effects
related to H+ levels
2,3-Bisphosphoglycerate (BPG)
decreases affinity of Hgb for O2
a product of metabolism
helps unloading of O2 in target tissues
important factor in maternal-fetal circulation
Fetal Hemoglobin (Hb-F)
higher affinity for O2 than any other hemoglobin
can carry up to 30% more O2 than adult Hgb
CO2 Transport
Dissolved CO2:
around 7%
diffuses out of blood into alveoli (because it is more lipophilic)
Carbamino Compounds
CO2 + Hgb → Reversible binding (Carbaminohemoglobin)
accounts for 23% of CO2
Bicarbonate:
70% of CO2
produced by action of carbonic anhydrase
Movement of HCO3 into blood plasma from RBC causes chloride shift
Haldane Effect:
lower amount of Hb-O2, the higher amount of CO2-carrying capacity of blood
as O2 leaves; frees up space for CO2
allows it to be picked up and carried out of the body
Respiratory Center
group of neurons that send the impulse for respiratory muscle contraction
2 principal areas
Medullary Respiratory Center
Pontine Respiratory Center
Medullary Respiratory Center
has two groups:
Dorsal Respiratory Group
important for normal/quiet respiration
Ventral Respiratory Group
pre-Botzinger complex (pacemaker of normal respiration)
important for forceful respiration
Pathway:
DRG activates VRG; which activates forceful respiration
accessory muscles of inhalation contract
or DRG triggers diaphragph
follow rest from ppt later
Pontine Respiratory Group
in midbrain
formerly called the pneumotaxic area
active during inhalation and exhalation
modifies basic rhythm generated by VRG for
Cerebral Cortex in breathing
breathing can be made voluntary
enables activities like holding breath, swimming, avoiding irritating gasses
holding breath eventually limited by buildup of CO2 and H+
when high enough, DRG takes over
instinct will force breathing
if fought against, you will pass out
fainting → loss of conscious control → DRG will still take over
hypothalamic impulses can also alter breathing pattern
ex: crying, laughing
note: this is also how drowning works; DRG kicks in while still underwater
Chemoreceptor Regulation
chemoreceptors for CO2, H+, and O2
provides input to respiratory center
Central Chemoreceptors:
present in medulla oblongata
are sensitive to H+ and PCO2
vigorous response to even slight increase in PCO2
Peripheral Chemoreceptors:
in aortic bodies or carotid arteries
more sensitive to PO2, H+ and PCO2
uniquely sensitive to O2, activates when PO2 is less than 00 mmHg
Brain concerned with CO2, body concerned with O2 I guess
Negative Feedback:
Decreased PO2 → DRG activation → Hyperventilation
Hypocapnia/Hypocarbia → DRG activation → sets moderate pace of breathing
Breathing into a bag
during hyperventilation = excess CO2 exhalation = alkalinity
breathing into bag recycles some CO2
effective for mild cases
if caused by more serious case (ex: renal disease) though probably won’t be enough
Hypoxia
deficiency of O2 at the tissue level
Hypoxic Hypoxia:
caused by low PO2 in arterial blood
ex: due to high altitude, obstruction, fluid in lungs
Anemic Hypoxia:
due to too little functioning hemoglobin; causes decreased O2 transport → insufficient O2
ex: due to hemorrhage, anemia, carbon monoxide poisoning, etc.
Ischemic Hypoxia:
blood flow to tissue is reduced (due to block, usually)
despite PO2 and oxyhemoglobin levels being normal
Histotoxic Hypoxia:
blood delivers normal O2 to tissues, but they are unable to use it
due to some toxic agent
ex: cyanide poisoning