Tricuspid Valve Disease and Pulmonary Disease
1/181
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
182 Terms
How many leaflets are found on the tricuspid valve?
Three. These are known as the anterior, the posterior, and the septal.
Does the TV open earlier or later than the MV? When does it close in relation to the MV?
TV opens earlier than the MV and closes after the MV.
What is the normal orifice of the TV?
7-9 cm²
Do right heart events last shorter than left heart events?
No, right heart events last longer than left side events.
Why do right heart events last longer than left?
Because inspiration causes a change in the intra—abdominal pressure with a resultant of an increase in blood flow to the heart and through the TV.
Blood velocities of the TV are lower than all the other velocities through the other valves. Why is this? (2)
The valve opening is the largest of any heart valve.
Right-sided pressures are lower than left heart pressures.
What is the area of the MV?
4-6 cm²
What is the area of the Ao V?
3-5 cm²
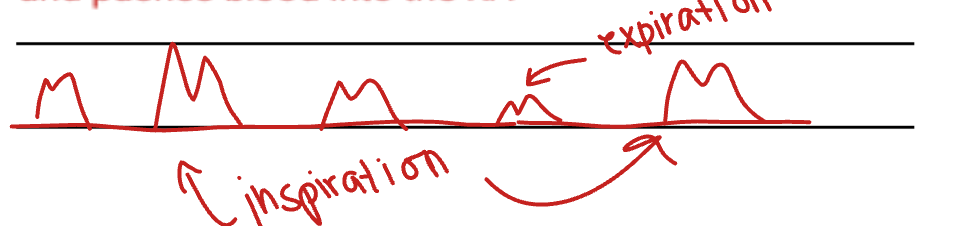
Because inspiration affects the intra-abdominal pressures, thus causing an increase in blood flow to the heart, we see what difference when we apply Doppler?
The inspirations when the TV opens are much taller and brighter. The expirations are smaller and darker. This is because when you breathe in, more blood goes into the right heart because the diaphragm goes down, which increases in intra-abdominal pressure in the cavity. This causes the IVS to collapse and pushes blood into the RA.
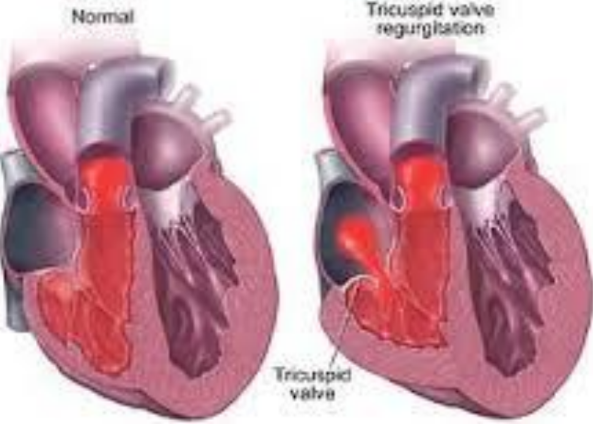
What is tricuspid regurgitation (TR)?
The backflow of blood from the RV back into the RA in systole.
Is TR common to find in patients?
Yes. Trace to mild TR is a common finding in 93% of patients.
TR can be of what three types?
Acute
Chronic
Intermittent (dependent on breathing - specifically inspiration)
What is the physiology associated with TR?
Backflow of blood from the RV, across the TV, into the RA in systole
And increase in RA size and pressure
Increase in IVC, hepatic veins, SVC, and neck veins
TR is usually well tolerated in the absence of what?
Pulmonary Hypertension.
What is the normal RA pressure?
5
What is the normal RV pressure?
25/5
What is the normal LA pressure?
10
What is the normal LV pressure?
110//10
What is the normal Ao pressure?
120/80
Is TR usually a primary lesion?
No. It is usually paired with other pathology.
TR is usually secondary to what issues? (3) Addtionally, what are these all precursors for? (1)
Pulmonary hypertension
RV failure
RV infarction
These are precursors to lung disease.
What are the causes of TR? (11)
Rheumatic heart disease
Infective endocarditis
Iatrogenic-pacemaker wire (doesn’t allow TR to close properly because a wire it running through it)
Congenital-Ebstein’s Anomaly
Connective Tissue Disease
Carcinoid Heart Disease
Trauma
TVP associated with MVP
Systemic Lupus
Tumor
Papillary muscle dysfunction and ruptured chordae
What is a typical clinical finding associated with TR?
Right heart failure
What are the other clinical findings associated with TR?
Renal failure
Weight loss, cachexia (wasting), cyanosis, jaundice
Hepatomegaly (enlarged liver)
Jugular venous distention
Arrhythmia (atrial fibrillation)
Arrhythmia - atrial fibrillation, occurs whenever what happens?
One (or more) of the chambers are stretched.
What is the auscultation like when there is TR?
High pitched blowing sound in systole which increases with inspiration (Rivero-Carvallo’s sign).
What is Rivero-Carvallo’s sign?
When breathing in (inspiration) causes TR to appear worse.
Is TR usually well tolerated for years?
Yes.
What are some medical treatments for TR? (3)
Digitalis
Diuretics
Sodium restriction
What is digitalis?
A drug that makes your heart contract more.
What are some surgical interventions that can be used to help treat TR?
Annuloplasty or RV replacement (bioprosthetic).
What is bioprosthetic?
Something that is made out of body tissue.
Which is more of an issue, acute TR or chronic TR?
Acute TR because it occurs suddenly. Chronic TR occurs slowly. If it continues to remain minor then it is virtually unproblematic. If it continues to worsen, then action must be taken.
What are the 2-D findings of TR? (7)
Anatomic basis for the presence of TR
RVVO
Paradoxical IVS motion and/or flattening of the IVS
D shaped LV during diastole
Dilated RA, RV, TV annulus > 3.4 cm in systole and > 3.2 in diastole
Dilated IVC (normal < 2.1 cm) - IVC should decrease in side with inspiration or sniff test
TVP associated with MVP (checking other valves for regurge).
Why does the LV turn into a D shape in diastole when there is TR?
Because there is an increase in RA and RV pressure. The size of the RA and RV is going to cause flattening of the IVS and the IAS. This increase in size and pressure of the RV pushes against the IVS, thus making it bow to the right.
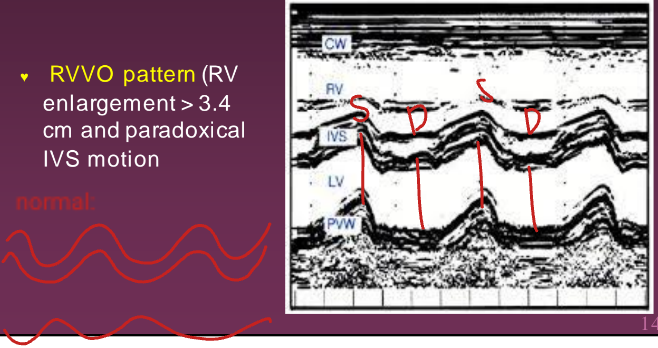
What are the M-mode findings of TR?
The RVVO pattern. This shows the RV is dilated (> 3.4 cm) and has paradoxical IVS motion (abnormal).
What are some CW Doppler findings with the presence of TR?
Using the peak TR to assess the severity of TR. It can also be used to estimate the RVSP because leak back into the RA is related to the pressure in the RV. Estimating the PA systolic pressure in the absence of pulmonary stenosis (PS) can also be done..
What is the normal RVP?
25/5 mmHg
Estimation of what is required when there is TR?
RAP.
What is the method of choice for diagnosing TR?
Doppler.
What percentage of patients have trace to mild TR?
93%
What is the IVC collapsibility index?
The index indicating how much the IVC is collapsing.
Why does the IVC collapsibility index important with TR?
Because the IVC is a highly compliant vessel and so we can assess it to determine pressures in the RA, thus allowing us to determine if a patient has TR or not.
The caliber and respiratory response of the IVC reflects which “sided” hemodynamics?
Right sided hemodynamics (which should be < 2.1 cm)
During inspiration, there is normally an increase or decrease in venous return to the right heart? What does this result in?
Increase. Results in a decreased pressure within the IVC and a decrease in blood volume within the IVC resulting in the collapse of the diameter of the IVC. (During expiration, the reverse occurs).
When can the normal inspiratory collapse of the IVC become diminished or absent?
When flow to the right heart is impeded by increased right side filling pressures and dilatation of the IVC or the hepatic veins may occur.
Maximal size and the degree of collapse of the IVC during respiration is a useful indicator of what?
RAP.
What is the normal size of the IVC?
< 2.1 cm.
If the IVC does not collapse with respiration, what can be used to hopefully enhance the effect inspiration should have on the IVC?
The Sniff Test.
What is the Sniff Test?
Where the patient takes a big sniff in to create a sudden decrease in intrathoracic pressure and a reduction in the diameter of the IVC.
Dilatation of the IVC with normal RAP can be seen in what types of patients?
Athletes and those who are mechanically ventilated. (Should be considered when estimating RAP)
What is the normal RV and pulmonary artery systolic pressure range?
15 to 30 mmHg.
A normal IVC size (< 2.1 cm) which has a collapsibility index of 50% has what pressure range in RA?
0-5 mmHg (go with 3 mmHg). NORMAL
A dilated IVC size (> 2.1 cm) which a greater than 50% collapsibility index has what pressure in RA?
6 to 10 mmHg (8 mmHg). MILD-MODERATE
A dilated IVC (> 2.1 cm) with less than 50% collapsibility index has what pressure in their RA?
10 to 15 mmHg. MODERATE
A dilated IVC (> 2.1 cm) with no collapsing of the IVC during inspiration has a RA pressure of what?
> 15 mmHg. VERY SEVERE.
How is RVSP calculated using Bernoulli and RAP?
RVSP = 4 (V)² + RAP (where V = TR peak velocity which can be found using CW, and RAP which can be determined when looking at the IVC)
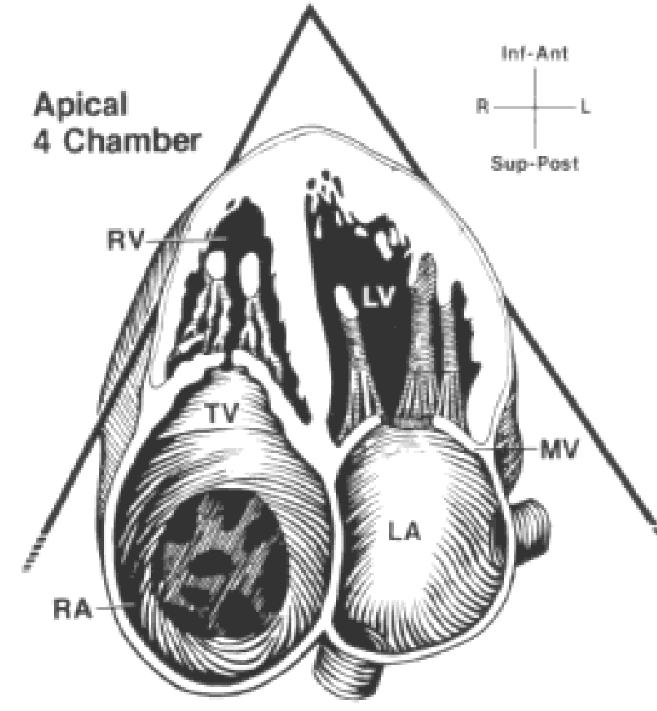
Using CW to find the peak velocity of TR can be done in what views?
LAX RVIT
SAX Base
A4
Subcostal
What is the normal range for PHTN by RVSP/PAP?
18-30 mmHg.
What is the range of pressure of RVSP/PAP when there is mild PHTN?
30-40 mmHg.
What is the range of pressure of RVSP/PAP when there is moderate PHTN?
40-70 mmHg.
What is the range of pressure of RVSP/PAP when there is severe PHTN?
> 70 mmHg.
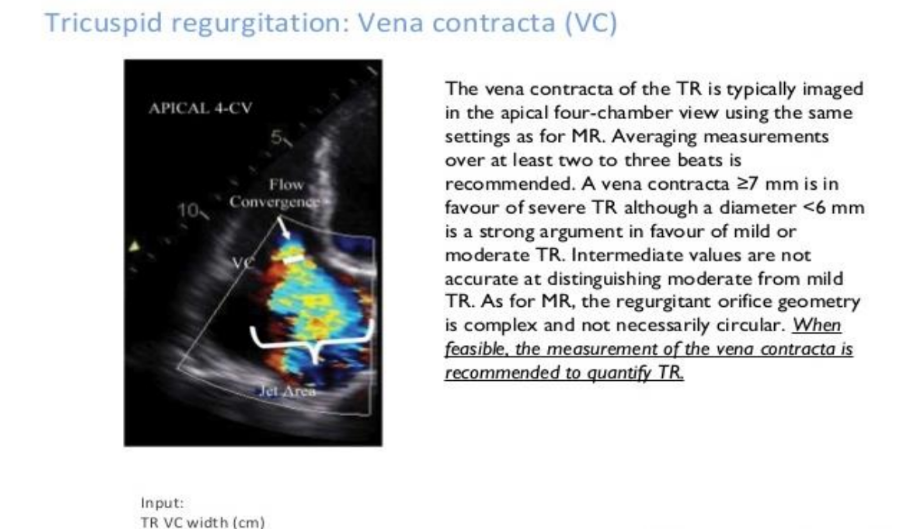
Colour Doppler is useful with TR by doing what?
Isolating where the TR jet is directed and is helpful with small eccentric TR jets.
The colour flow Doppler of a normal RV inflow tract has what colour in diastole?
Normal red diastolic flow.
The colour flow Doppler of a TR has what colour in diastole?
A blue jet demonstrated in the RA in systole.
Is measuring the vena contracta useful to use for patients with TR?
No.
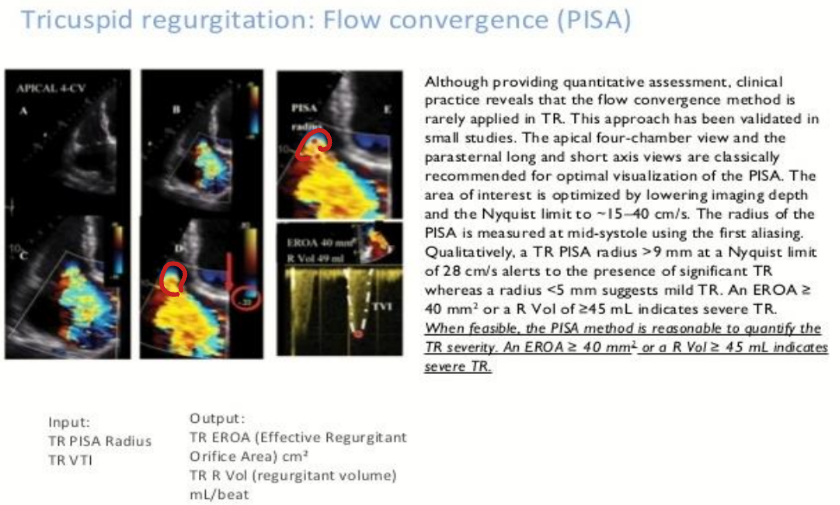
Do sonographers use PISA on TR?
No. But it can be done.
Should you grade TR?
YES! Always!
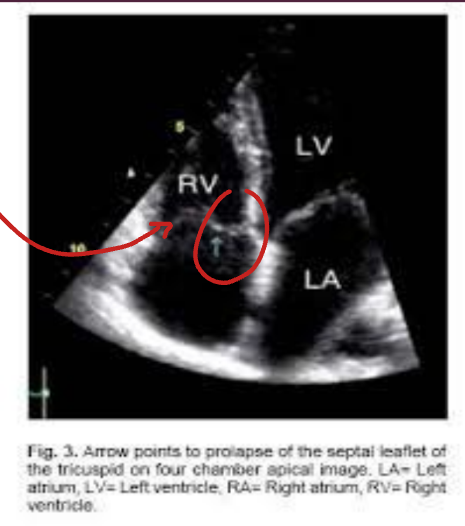
What is tricupsid valve prolapse? (TVP)
The prolapse of any part of the TV leaflets beyond the TV annulus.
Is isolated TVP common?
No, it is rare. TVP is usually associated with MVP.
What is the most common TV leaflets to prolapse?
The anterior leaflet.
Using 2-D, what view demonstrates the anterior and septal leaflets of the TV?
A4.
Using 2-D, what view demonstrated the anterior and the posterior TV leaflets?
LAX RVIT.
TVP is indicative if leaflets proplase past TV annulus superiorly by how much?
> 2 mm.
With TVP, leaflets may appear looking…?
Myxomatous and redundant.
What does the Doppler findings of TR look like?

What is tricuspid stenosis?
The obstruction of flow from the RA to the RV in diastole (when the TV is opened).
Is TS rare as an isolated lesion?
Yes. It is usually paired with something else.
What is TS most commonly due to?
Rheumatic disease with mitral and aortic valve involvement.
What are some symptoms of TS? (3)
Edema
Abdominal swelling
Ascites (fluid in the belly)
If you get rheumatic heart disease, which valves are effected and in what order?
Mitral Valve
Aortic Valve
Tricuspid Valve
Pulmonary Valve (RARE)
What are some causes of TS? (3)
Rheumatic fever
Congential
Carcinoid
What is TS secondary to? (4)
RA clot
Infective endocarditis
Prosthetic valve dysfunction
Pacemaker wire that obstructs flow
What is the auscultation like when there is TS?
An opening snap and diastolic rumble which may occur later than the MV opening.
In what transducer position is the auscultation of TS best heard?
The left lateral sternal border (LLSB)
Can the murmur of TS get louder with inspiration?
Yes.
Normally, the TV should open before or after the MV?
Before.
In TS, the TV opens before or after the MV?
After.
What are the 2-D findings associated with TS? (5)
Thickened, echogenic leaflets with restricted movement
Diastolic doming
Decreased orifice size
Enlarged RA
Dilated IVC due to back up of blood
Can planimetry of the TV orifice be done to determine the TVA?
Yes, but rarely. This is because we cannot see all three leaflets.
What are the M-Mode findings associated with TS? (4)
Thickened TV leaflets
Decreased D-E excursion (due to decreased leaflet separation)
Decreased E-F slope (similar to MS) - function of RV filling
Anterior motion of the posterior TV leaflet
Normal TV on M-Mode looks like an “M”. What does a TS TV look like on M-Mode?
A box.
What is the method of choice used to aid inn the diagnosis of TS?
Doppler.
How can you obtain the area of the TV?
Using planimetry or pressure half time (PHT is the way too go).
What is the normal TV area?
7-9 cm²
The minimum TV area which is considered stenotic is what?
< 2 cm²
What is the normal TV blood flow velocity?
0.3-0.7 m/sec.
If there is TS, there is usually what?
TR.
What is the carcinoid syndrome?
TS that is associated with carcinoid tumors.
What is the most common sites (2) for carcinoid tumors?
Appendix (benign)
Ileum (maligant) - metastases to liver