GDM - EPIDEMIOLOGY, DEF , TYPES OF DIABETES AND Pathophysiology
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
28 Terms
Pathophysiology - GDM
decrease in insulin (beta cell’s insufficient response) sensitivity & insufficient insulin selection by beta cells is key for mechanism of GDM (results in increase blood glucose)
Because of insulin resistance, the Beta cells compensate by releasing insulin
Increase blood glucose causes inflammation
GDM disappears AFTER birth of placenta as NO more placenta hormones = insulin sensitivity & BG Levels restored to normal
IF ABLE to compensate - will NOT have GDM
Pathophysiology of GDM 2
Fetoplacental hormones ( glt, cortisol, prolactin, HPL) leads to —>
INCREASED insulin resistance
Compensatory increase in insulin selection if not —>
(Compensatory) If not ? GDM
(insulin Secretion) Normal in pregnancy
HPL - Human placental lactogen - increases as measuring ( pregnancy ) progresses
creates resistance of insulin for growth baby → maximise fetal growth
LGA
SGA
Role insulin
Facilitates glucose uptake —> uptake from blood into cells (liver, skeletal & muscle)
Stimulates formation & storage of lipids & glycogen
Decrease in BG levels =
increase glucose transport by target cell
Accelerating glucose utilisation (target cells) & enhanced ATP production
Stimulating glycogen synthesis
Decrease in glycogenesis
Role of glucagon
Mobilises energy reserves & promotes glucose
Synthesis & glycogen breakdown
Elevates BG concentrations = stimulating breakdown of glycogen in Skeletal, muscle & liver cells
Stimulating breakdown of inglyceridxen in adipose tissues → production of glucose in liver
HbA1c
(50g) Polycose → oral glucose test → no risk factors ( > 7.8mmol)
oral glucose tolerance (75g) → 24 - 28 weeks
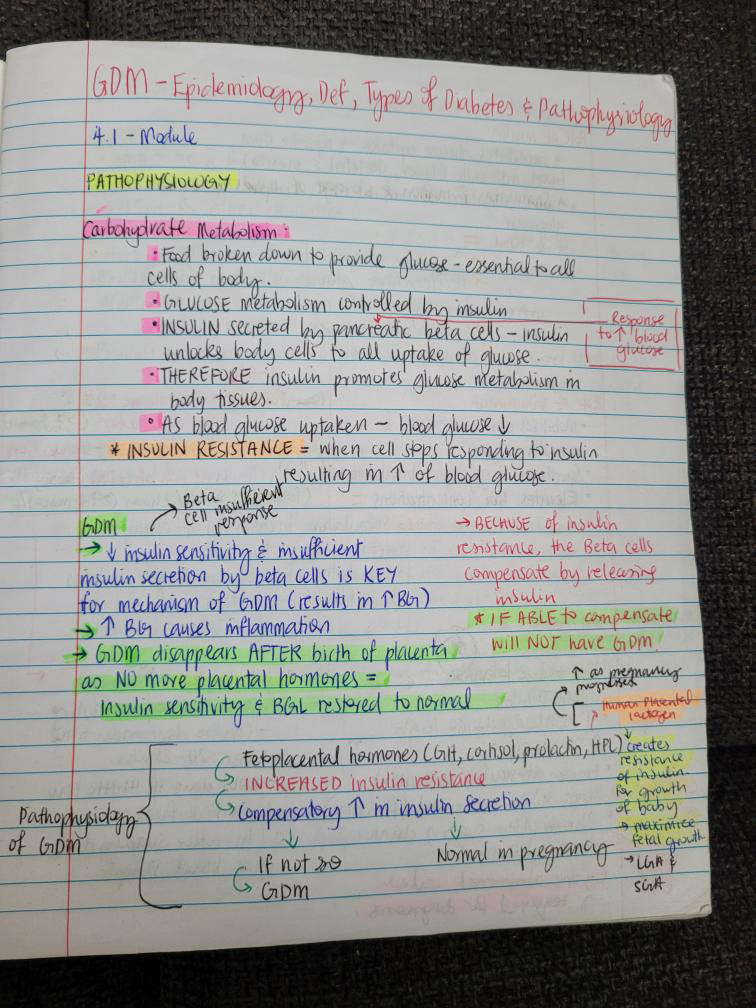
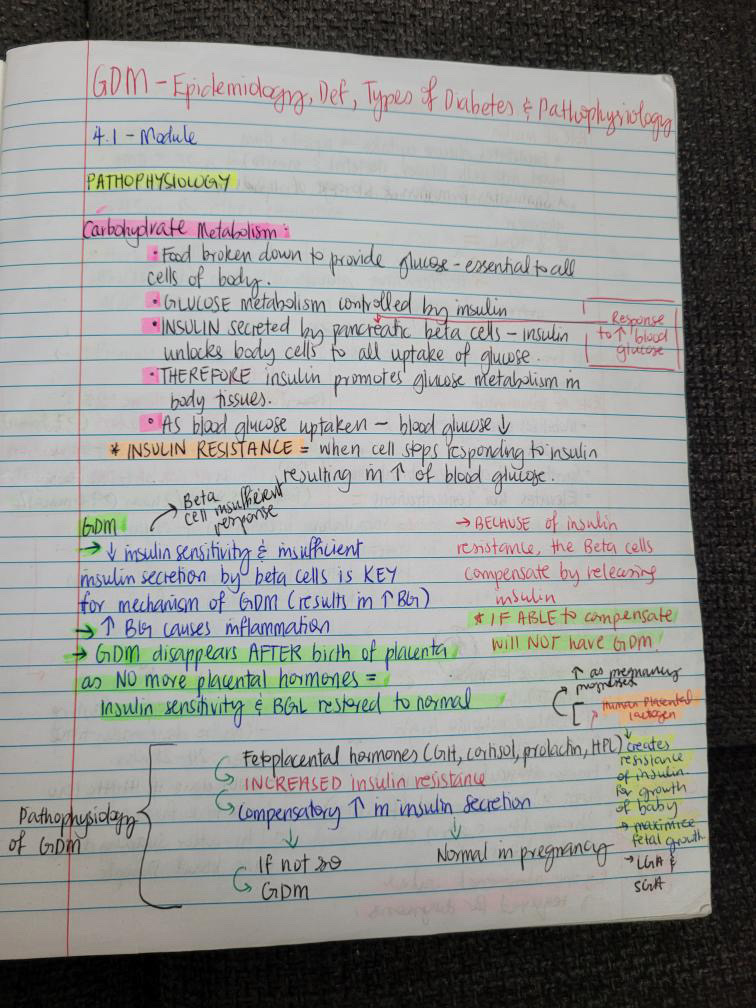
PATHOPHYSIOLOGY - Carbohydrate Metabolism:
Food broken down to provide glucose - essential to all cells of body
• GLUCOSE metabolism controlled by insulin
Insulin secreted by pancreatic (response to increase in glucose) beta cells - insulin unlocks body cells to all uptake of glucose
THEREFORE Insulin promoTes glucose metabolism in body tissues.
As blood glucose uptaken - blood glucose decreases
* INSULIN RESISTANCE = When cell stops responding to insulin resulting in increase of blood glucose
GDM1
(Beta cell insufficient response) Decrease insulin sensitivity & insufficient insulin secretion by beta cells is key for mechanism of GDM (results in increase blood glucose)
Increase in BG causes inflammation
GDM disappears after birth of placenta as no more placental hormones = insulin sensitivity & BGL restored to normal
GDM2
Bc of insulin resistance, the beta cells compensate by releasing insulin - IF ABLE TO COMPENSATE, WILL NOT HAVE GDM
Pathophysiology GDM
Fetoplacental hormones (GH,CORTISOL PROLACTIN,HPL- HUMAN PLACENTALLACTOGen - increases as pregnancy progresses - creates resistance of insulin for growth of baby -maximize Fetal growth- lga & saga)
Then - results in increased muslin
Then - Compensatory 9in not GDM ) increase in insulin (normal in pregnancy )secretion
Role of insulin
facilitates glucose uptake - uptake from blood into cells (liver , skeletal and muscle)
Stimulates formation & storage of lipids & glycogen
Decrease BGL = increase glucose transport by target cells, accelerating glucose utilisation (target cells & enhanced ATP production, stimulating glycogen synthesis, decrease in glycogenesis
Role of glucagon
mobilises energy reserves& promotes glucose
Synthesis & glycogen breakdown
Elevates BG concentrations = stimulating breakdown of glycogen in skeletal muscle & liver cells.stimulating breakdown of inglycerides in adipose tissues → production of glucose in liver
HbA1c
(50mg) poly one - oral glucose test - no risk factors (7.8mmol)
(75g) Oral Glucose tolerance → 24-28 weeks - at risk of GDM (5.5mmol)
Fasting > 5.5mmol/2hr > 9.0mmol)
Oral glucose tolerance test (OGTT)
done if hba1c & polycose result high
Diagnostic
Empty stomach in the AM
Bloods taken on arrival (fasting 5.5mmol)
2hr after sugary drink - blood taken (9.0mml) -one abnormal results required fo diagnostic
Polycose test (50g)
Does not require fasting
Can be done anytime 24-28wks
Only done if hba1c low & no risk factors
1hr after sugary drink,bloods done
Risk factors GdM
ama >= to 35y/o for Māori, indo Asian & pasifika - 45y/o for other ethnic groups
Prev LGA baby ( > 4000g)
Family history - first degree relative
Increased bmi > 27kg/m2 in indo asain, >= 30kg/m2 in other ethnic groups
Prev GDM
Prev impaired fasting glucose or impaired glucose tolerance
PCOS
Cvd or (vd),presistant hypertension (135/80mmhg >=),elevated triglycerides/cholesterol
Acanthosis nigrican (brown darkening of skin folds)
Long term use of steroids antipsychotic meds
Physical inactivity/sedentary (lazy/careless) lifestyle
Screening - Hba1c
As rBC are made they combine with glucose in blood to form hba1c link - this can cause inflammation and ends __ damage - pet
hba1c (glycated haemoglobin) - tested on whole body
Indicates average BGL over prev 6-8wks
Reliable method of detecting probable diagnosed diabetes in first 20wks gets
DO NOT OFEER HBA1C AS DIAGNOSTIC TEST FOR GDM AS NOT SENSITIVE ENOUGH.
Why HBA1c
hba1c screening (threshold >= 34.4mmol) was superior to risk factor screening risk factor screening alone would miss 18% of all subjects and a third of Europeans who had an hba1c >8% (64mmol)
Plan with hba1c results
wome with GDM have 3mnths pp and then annually
Levels decline during pregnancy
If diabetes under control , plan birth at 40wks if not well managed , plan birth at 38-39wks
hba1c 4=40mmol/mol (NORMAL)
Receive; dietary advice, lifestyle advice and have a glucose challenge (polycose) or oral GTT at 24-28wks (if polycose > 7.mmo> 11.1ml refer to dip)
Hba1c 41 - 49mmol receive; dietary advice, and lifestyle advice and OGTT at 24-28wks (pre diabetic)
hba1c >= 50mmol receive: care from dip an specialist (diabetic NOT GDM)
Further advice - Plan with hba1c results
eat healthy and balanced diets with 30mins of exercise (moderate) per day
Women with risks factors should avoid excessive weight gain - healthy diet and lifestyle should continue pp
To avoid GDM: prior and during pregnancy take into consideration their lifestyles
BMI Chart - average levels
BMI - underweight < 18.5 - REC weight gain 13-18kgs
Healthy weight 18.5 - 24.9 → 11-16kg
Overweight 25-29.9 → 7-11kgs
Obese >30 → 5-9kgs
Twins/multiples: different BMI chart (weight gain)
Diabetogenic state: peak @ 24-28gst
occurs in pregnancy to ensure optimal glucose uptake by fetus
Due to placental hormones (also increase i adiposity) Causing insulin resistance and compensatory hyperinsulianemia - begins in 2nd tr and right through pregnancy, resembling t2dm levels
In 2nd and 3rd tri, placental steroids and hormones exacerbate tissue insulin resistance
If maternal pancreatic insulin response inadequate = 1st maternal then Fetal hyperglycemia
Diabetes overall 1
absolute or relative deficiency of insulin production by pancrease
Lacoste cannot be inverted to glycogen or released as energy so = increase in BGL
Glucose osmotically active = draws water after it resulting in polyurice and thirst
Due to lack of glucose uptake,body tries to seek glucose through fats and proteins -. Production of ketones by liver -. Ketosis
Diabetes overall 2
T1DM - Beta cels destruction → decrease in insulin products and release
T2DM - Beta cells work but not as efficiently as cells receptors are resistant to insulin - resistance can cause insufficient beta cell function of insulin release
GDM - Pancreatic B cells insufficient insulin secretion , insulin secretion due to placental hormones
Diabetes/GDM Poor management consequences Women
retinopathy may worsen in pregnancy and should consult ophthalmologist prior to conception and further consultations during pregnancy
Nephropathy - in combinations with PE and chronic hypertension = pre term birth , pet, miscarriage, increased risk of t2dm, c/s and IOL, polyhydramnos ,UTI
Diabetes/GDM Poor management consequences Fetal
CDV and neural tube defects (13x-20x more common in diabetic pregnancies)
LGA
Stillbirth
Preterm (SROM OR Planned to avoid SB)
Congenital malformation
Birth trauma due to LGA
Hypoglycaemia PN
Diabetes/GDM Poor management consequences - MW Role
Advise and information sharing preconception and during pregnancy
Refer to dip
AN care components: history taking = current and past contraception menstrual history
Screening fro existing diabetic complications
Doc and management of situation
Med review
High doc 5mg folic acid pre conception and 1st tri
Smoking/alchol help
BMI and referral to dietian