Malignant hyperthermia
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
Characteristics of MH
An uncontrolled rise in myoplasmic calcium results which causes a hyper-metabolic response
Leads to increased CO2 production, oxygen consumption, fever, tachycardia, tachypnea, acidosis, hyperkalemia, myoglobinuria, increased CPK, cyanosis and death
pathophys of MH
An abnormal structure and function of a calcium channel within their skeletal muscle.
When exposed to the agent, an abnormal Ca released, causing sustained muscle contraction, abnormal increase in energy utilization and heat production.
Muscle cell eventually runs out of energy and dies releasing large amounts of K and myoglobin into the bloodstream, leading to arrhythmias and kidney failure.
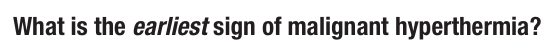
clinical S&S of MH
Unexplained tachyarrhythmia- compensatory mech (96% of cases) & HTN [ EARLY SIGN ]
Increased end-tidal CO2 [ EARLY SIGN ]
Hypoxemia [ EARLY SIGN ]
Acidosis (80%) [ EARLY SIGN?- on the powerpoint as early but Zhang said it was a later sign b/c compensatory mech fail- for exam purposes just choose the BEST answer..]
Masseter rigidity (common in early phase)
Unexplained tachypnea (85% of cases)
General muscle rigidity – late sign
Cyanotic or mottled skin – generally starts with a generalized flush (70%) [late sign]
Rapid, sustained increase in body temperature – late sign only 30% of cases. Temperature can be as high as 110°
Cola-colored urine due to rhabdomyolysis (late sign)
lab findings with MH
ABGs: Respiratory & Metabolic Acidosis: Arterial hypoxemia
Decreased pH ; Decreased PO2; Increased PCO2
Serum K greater than 6mEq/L
Creatine Kinase greater than 20,000units/L
Serum myoglobin greater than 170mcg/L
Urine myoglobin greater than 60mcg/L
Predisposing factors of MH
Most common between ages 2 – 42
2/3 cases are men
1st degree relative of someone who has had MH or MH susceptible is at greater risk
Higher risk in someone with a muscle disorder
Central Core disease
Multi-minicore disease
King Denborough syndrome
2/3 of susceptible patients manifest this syndrome during their first anesthetic
Gene for MH: chromosome 19, the genetic coding site for Ryanodine receptors (calcium release channel) of skeletal muscle sarcoplasmic reticulum.
2 genetic mutations have been identified as predisposing a patient to MH:
RYR1: encodes the Ryanodine receptor,
& CACNA1S [ hopefully not testing on this one]
DX of MH
caffeine halothane contracture test (CHCT).
Done with thigh muscle biopsy
Drugs considered trigger of MH
Known triggers:
Volatile anesthetics - sevoflurane, isoflurane, and desflurane
Inhaled anesthetics (except nitrous oxide)
Muscle relaxant – succinylcholine
Definitive treatment for MH and MOA
dantrolene
Reduces contraction of skeletal muscle by a direct action on excitation-contraction coupling
Contains Mannitol (converts hypotonic solution to isotonic)
Can potentiate [ inc] NDNMBs – does not affect reversal
differential dx for MH
o Is depth of anesthesia adequate? hypovolemic ?
o Is pain addressed?
o Esmolol?
o Check for rigidity- check TOF to assess NMB
could it be NMS?
thyroid storm?
pheochromocytoma?
is there a CO2 leak from insufflation?
steps when MH is suspected
- Stop triggering agent – give propofol
- Call for help [ MDA or chief CRNA ]
- Alert surgeon- close up if possible
- Ask someone to get MH cart
- Change CO2 absorber/ breathing circuit
- Turn baer hugger to ambient and Ask for chilled IVF [ also ask for ice packs —> gastric lavage also good for rapid temp control- stop when temp is <38]
o If pt does NOT have foley, place one now to monitor UOP and color
- Inc FiO2 to 100% and hyperventilate [#1 according to Zhang] the patient
o This will help blow off CO2 and improve acidosis if present
o If pt has an a-line, get an ABG- administer Bicarb if acidotic
§ 1-2mEq/Kg
- Calculate and administer dantrolene
Does patient have peaked T waves?
o Could indicate high K
o CaCl to stabilize the heart
o Give 10 units insulin + 1-2 amps of D50
o Hyperventilate [ already doing that ]
o Na biacarb [ might already be given ]
o Albuterol – 8-12 puffs
If pt still have arrythmias after K tx:
o Amiodarone 150mg IV
o Lidocaine 1.5 mg/kg
Check labs
o CK
o Electrolytes
o Coagulation studies?
- Admit to ICU
DO NOT USE Calcium Channel Blockers in presence of Dantrolene- WHY ?? and which med specifically
Verapamil can interact with Dantrolene to produce hyperkalemia and myocardial depression
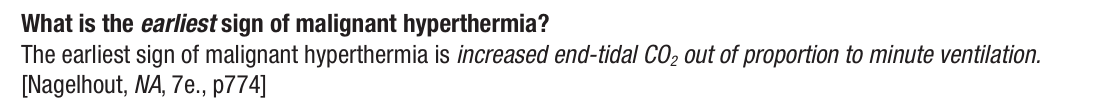
Dantrolene management (initial, infusion and postop)
2.5 mg/kg IV [ max 10mg/kg]
Continue IV Dantrolene for 24 - 48 hrs = 1 mg/kg every 6 hrs or 0.25mg/kg/hr to prevent recrudescence (relapse) of symptoms
Dantrolene ___mg in one vial. How to constitute
20
Mix with Sterile Distilled Water = 60ml H2O /20mg Dantrolene per ampule
Clear yellow to yellow/orange color
DO NOT use bacteriostatic water
Requires at least 2 providers -- labor intensive [ does not dissolve easy ]
Do not use iced fluid to dissolve Dantrolene
Ryanodex
: more expensive -$6,900/ vial
Approved by FDA for use in Malignant Hyperthermia patients on July 23, 2014
250 mg mixed in 5ml of Sterile Water
in this list of drugs, which are considered SAFE and not a trigger for MH?
local anesthetics
barbiturates
Benzodiazepines
Succ
etomidate
Ketamine
Sevoflurane
nitrous oxide
Nondepolarizing muscle relaxants
Isoflurane
propofol
Desflurane
local anesthetics
barbiturates
Benzodiazepines
Succ
etomidate
Ketamine
Sevoflurane
nitrous oxide
Nondepolarizing muscle relaxants
Isoflurane
propofol
Desflurane
preparation for a patient with known susceptibility to MH
1st case of the day
Avoid triggering agents
Remove vaporizers, or tape in “OFF” position
Change CO2 absorber, replace breathing system & reservoir bag
Flush the anesthesia machine with O2 set at >10L/Min
Review & know your machine’s recommendation
Older machines require only 20 minutes
Newer machines may require up to 104 minutes of O2 flushing
Keep fresh gas flow at 10L/min during case to prevent rebound phenomenon
Place activated charcoal filters on inspiratory & expiratory limbs
Know where MH cart is
Know where crushed ice for OR is to cool pt
3L refrigerated/cold IV solution
Monitoring for signs of MH
Ensure all OR personnel are informed of treatment protocol