MICR5831 L11: Molecular Koch’s Postulates 9/24/25
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
71 Terms
What is this?
-Set of criteria
-Connection between a particular microbe and a particular disease
Koch's Postulates
What is the first Koch postulate?
-Microbe is found in all disease cases
-Not found in healthy individuals
What Koch postulate comes after this?
1) Microbe is found in all disease cases
-Not found in healthy individuals
Pure culture of microbe is grown using isolate of microbe from diseased host
What Koch postulate comes after this?
2) Pure culture of microbe is grown using isolate of microbe from diseased host
Introducing microbe into healthy/susceptible host causes same disease
What Koch postulate comes after this?
3) Introducing microbe into healthy/susceptible host causes same disease
Same strain of microbe can be obtained from new diseased host
What are some challenges to this assumption?
1. Disease symptoms depend entirely on bacterium, not host
-Host factors also play a huge role in symptoms
-Asymptomatic carriage occurs in some patients (V. cholerae, S. Typhi)
What are some challenges to this assumption?
2. Any pathogen can be isolated from the infected animal and cultured in pure form
M. leprae, Treponema pallidum, Chlamydophila pneumoniae cannot be cultured
What are some challenges to this assumption?
3. A good animal model (or human volunteer) exists for re-inoculation
-No good model for re-inoculation, still useful though
-Ferret model for H. pylori
-Chinchilla model for otitis media
4. Diseases are caused by a single pathogen
-Some diseases are polymicrobial
-Microbial shift diseases that cause dysbiosis
What is this?
-Microbial shift diseases cause microbiome changes
-Triggers inflammation/tissue damage that is hard to reproduce in animals
Dysbiosis
What is this?
-IBS, periodontal disease, bacterial vaginosis
Dysbiosis
What is this?
-Dysbiosis examples
1) IBS (Inflammatory bowel disease)
2) Periodontal disease
3) Bacterial vaginosis
True or False: Chlamydia pneumoniae can be found in both healthy blood vessels and atherosclerotic plaques
True
True or False: C. pneumoniae can only be cultivated in tissue culture
True
What is this?
-Ability of a microorganism to cause disease
Pathogenicity
What is this?
-Successful colonization of the body by a microorganism capable of causing damage to the host i.e. a pathogen
Infection
What is this?
-Degree of pathogenicity of a microorganism, or its relative ability to overcome host defences
Virulence
What is this?
-Bacterial product or strategy that contributes to the ability of the bacterium to survive in the host and/or cause infection
Virulence factor
What are some important bacterial virulence factors?
1) Iron acquisition
2) Attachment to host tissues
3) Motility and chemotaxis
4) Invasion of host cells
5) Toxin production
6) Quorum sensing
7) Biofilm formation
8) Secretion/delivery of virulence factors
9) Antimicrobials
What are some advantages of using tissue culture models over animal studies?
-Easily controlled system, less complex/variable
-Defined medium, reproducible conditions
-Visualized by microscopy/flow cytometry
-Cheaper and easier to maintain
What are some limitations of tissue culture models?
-Some genes only expressed in vivo
-Loss of normally distributed surface antigens
-Pathogens enter cells they don't normally infect
-Tissue culture monolayers not differentiated
What does it mean if tissue culture cells are polarized in vivo?
Membranes on different sides of cells contain different proteins
What approach to identifying virulence factors is this?
-Can be purified from filtered bacterial culture supernatants
-Filtrate is processed by chromatography
-Fractions can be tested for toxicity
Biochemical Approach
How can you determine the amino acid of a purified toxin using Biochemical Approach?
Mass spectrometry
What were the first virulence factors to be Identified and characterized at the molecular level via Biochemical Approach?
Bacterial protein toxins
How do these methods for identifying virulence factors via the Biochemical Approach work?
1) Ion exchange columns
2) Gel filtration columns
1) Separation based on charge
2) Separation based on molecular size
What approach to identifying virulence factors is this?
-Identify virulence genes by cloning and expressing them in avirulent bacterial strains
Molecular Genetic Approach
What approach to identifying virulence factors is this?
-Listeria haemolysin (LLO) gene is cloned into avirulent lab strain of Bacillus
-Very successful
Molecular Genetic Approach
What is this?
-Allows bacterial escape from host endosomal vacuole into cytosol and survival in host cell
-Found in Listeria
-Cloned using Molecular Genetic Approach into Bacillus
Hemolysin
What approach to identifying virulence factors is this?
-Works best if only one or a few contiguous genes give desired phenotype
-Requires gene of interest to be expressed in E. coli or other avirulent bacterium being used
Molecular Genetic Approach
True or False: Standard cloning isolates only fragments of genome
True
What approach to identifying virulence factors is this?
-Mutagens are used to increase the frequency of mutation
-Makes it easier to find desired mutants
-Traditional and Transposon Mutagenesis
Molecular Genetic Approach
What is the first step of Mutagenesis Screening using the Molecular Genetic Approach to virulence factors?
-Observe a phenotype in an organism
-Toxin production, invasion etc
What happens during Mutagenesis Screening using the Molecular Genetic Approach after this step?
1) Observe a phenotype in an organism
Mutagenize the organism
What happens during Mutagenesis Screening using the Molecular Genetic Approach after this step?
-Mutagenize the organism
Isolate mutants that no longer have that phenotype
What happens during Mutagenesis Screening using the Molecular Genetic Approach after this step?
-Isolate mutants that no longer have that phenotype
Work out what change(s) have occurred in the mutants' DNA
What type of mutagen is this?
-Chemicals like ethyl methane sulphonate (EMS) or ethidium bromide, or UV irradiation
-Produce random mutations in any gene
-May cause too many DNA changes for easy analysis
Traditional Mutagens
What type of mutagen is this?
-Insertion mutants (Tn) are generated by almost random single-insertion into a pathogen's genome
-Many of these insertions disrupt a gene
-Screened for loss of virulence
Transposon Mutagen
What is this?
-Antibiotic resistance gene or a reporter gene
-Example: Inactive LacZ gene with no promoter
-Found by cloning gene/sequencing mutant chromosome
Selectable marker for presence of Tns
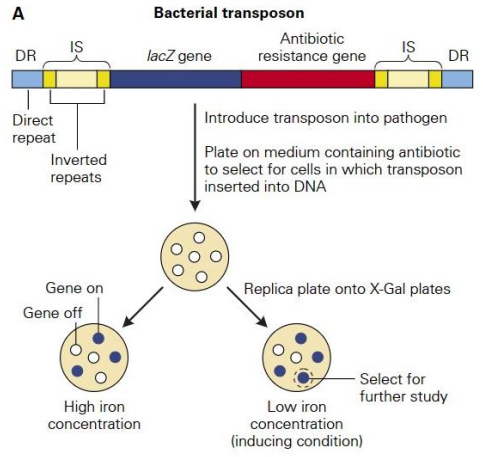
How can Transposon Mutagenesis be used to locate virulence genes based on their regulation?
1) Tns without a lacZ promoter or antibiotic resistance
2) Generate collection of random Tn inserts
3) Colonies plated on X-gal, screened for lacZ
4) Some mutants have Tn inserted downstream of virulence gene promoter with reactivated virulence factor
True or False: Virulence genes may be upregulated in high iron conditions/medium
False
True or False: Virulence genes may be upregulated in low iron conditions, similar to in a host
True
What will happen if lacZ is expressed?
-LacZ is expressed and transcribed using the promoter of the gene next to the Tn insert
-X gal is cleaved by LacZ and turns blue
True or False: When screening for virulence genes, LacZ is transcribed using its own promoter
False, LacZ's promoter has been removed so it is using a gene next to the Tn insert
What does this mean?
-Blue colony on low iron (LacZ expressed)
-White colony on high iron (LacZ inactive)
When LacZ is transcribed/expressed, the promoter it used most likely came from a virulence gene that is regulated via iron
What happens if a Tn with a transcriptional terminator lands in the first gene of an operon?
-Eliminates expression of all operon genes
-Failure to identify gene responsible for virulence
True or False: Tn insertion mutants can only be obtained for genes that are not essential for growth in vitro
True
Would you be able to form a colony using an insertion mutant that inactivated a gene that is essential for growth in-vitro?
No, because if it is essential then inactivating it will make growth impossible
What does it mean if you knock out one copy of a gene and the phenotype ends up as WT instead of mutant?
The two genes in the chromosome are homologs with the same redundant function
What approach to identifying virulence factors is this?
-Preferred approaches to identifying bacterial virulence
-Transposon Sequencing (Tn-Seq)
-RNA-Seq technology
-Comparative Genomic Sequence Analysis
Genome-Wide Sequencing
What type of Genome-Wide Sequencing is this?
-Combines Tn mutagenesis with in-vivo selection
-Uses animal model to screen for mutants that do not grow in the host
Transposon Sequencing
What is the first step of Transposon Sequencing?
Tn library is made and plated onto antibiotic plates
What happens during Transposon Sequencing after this step?
-Tn library is made and plated onto antibiotic plates
Colonies containing Tns are pooled and stored
What happens during Transposon Sequencing after this step?
-Colonies containing Tns are pooled and stored
-Tn mutants are divided into two parts
-Each part is grown under a different condition
What Transposon Sequencing pool is this?
-Tn mutant in nonselective culture medium
-In vitro growth
Input pool
What Transposon Sequencing pool is this?
-Tn mutant in an animal host
-In vivo growth
-After infection, organ/blood is harvested and the bacteria are recovered
Output pool
What happens during Transposon Sequencing after this step?
-Tn mutants are divided into two parts
-Each part is grown under a different condition
-DNA is extracted from both pools of bacteria and sequenced starting from each Tn
-Initiate all sequencing reads from the edge of the inserted Tns to the adjacent bacterial chromosome
What happens during Transposon Sequencing after this step?
-DNA is extracted from both pools of bacteria and sequenced starting from each Tn
-Sequences are mapped to the genome
-Sequence read counts from the Input and output pools are compared
What does it mean if there are no mutants containing Tn inserts in gene "C" in the input or output pool?
Gene is essential for growth under both conditions
What does it mean if there are plenty of mutants containing Tn inserts in gene "B" in both pools, and the mutants survive in vitro/in vivo?
-Gene is not required for growth in input/output pools
-Growth occurs even when gene is modified/inactivated by Tn inserts, so it’s not necessary
What does it mean if there are no surviving mutants containing Tn inserts in gene A after the pool has been grown in the animal model?
Gene is required for survival in vivo
Which type of gene would you treat as a putative/believable virulence gene and analyze further to see if it encodes anything for bacterial colonization/survival?
Gene is required for survival in vivo
What are some advantages of the Tn Seq (Transposon Sequencing) method?
-Rapid
-Wide range of bacteria it works on
-Doesn't require many animals
What type of Genome-Wide Sequencing is this?
-Used to identify in-vivo-expressed genes
-Next-generation Illumina sequencing of whole bacterial and/or host transcriptome (RNA)
-Preferred method for genome-wide identification of bacterial genes expressed during infection
RNA Sequencing Technology
What type of Genome-Wide Sequencing is this?
-Fluorescently-labelled bacteria infect host cells
-Host cells sorted by FACS to enrich for infected cells
-Total RNA extracted, host RNA removed
-cDNA produced and sequenced
RNA Sequencing Technology
What type of Genome-Wide Sequencing is this?
-Comparing genomes of pathogenic and non-pathogenic strains of the same bacterial species
-Can identify genes found exclusively in the former
-Strong candidates as virulence factors
Comparative Genomic Sequencing
How do modern technologies overcome exceptions to Koch's postulates?
1) Detection via PCR or immunohistochemistry or ELISA
2) Antibiotic therapy eliminate H. pylori and cure ulcers
3) HPV vaccine used against genital warts and cancer
What is the fundamental philosophy of the molecular Koch's postulate?
1) Gene should be found only in infectious strains
2) Gene should be isolated by cloning/sequencing
3) Disrupting the gene should show a loss of function/virulence
4) Introducing the cloned gene should make a strain virulent
What are the strengths and weaknesses of three models often utilized to measure virulence?
-Human: Seriously unethical
-Animal: Needs to mirror human host
-Tissue: Cheap, easy to control, reproducible but loses normal expression
What are some animal models that don't exactly mirror human infection but are still useful?
H. pylori: Ferrets
Otitis media: Chinchillas
Describe the experimental design using an avirulent strain to identify a virulence factor.
What is the drawback of this method?
-Works best if only one or a few contiguous genes give desired phenotype
-Requires gene of interest to be expressed in E. coli or other avirulent bacterium being used