Nausea and Vomiting
1/28
Earn XP
Description and Tags
PEBC
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
nausea
unpleasant sensation experienced prior to vomiting with underlying causes (this is a symptom, not diagnosis)
acute < 1 week
chronic >1 month
vomiting (emesis)
oral discharge of gastric contents
retching
muscle contraction without expulsion of gastric contents (gagging or dry heaving)
conditions associated with nausea and vomiting
GI:
PUD
Pyelonephritis
Gastroenteritis
functional dyspepsia
pancreatitis
gastric outlet/ bowel obstruction
gastroparesis
gastric malignancies
Drug withdrawal
opiates
BDZ
Neurological
HA/Migraines
vestibular disorders
ICH, head trauma
Metabolic:
Diabetic ketoacidosis
Addison disease
renal disease
other:
Pregnancy
acute infection
Hyponatremia
uremia
Anxiety/ depression disorders
anticipatory nausea
anorexia
otitis media
post-op
noxious odours
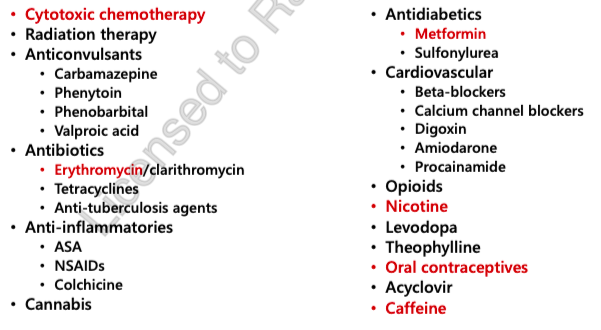
drug causes
Cytotoxic chemotherapy
radiation
Anticonvulsants
Antibiotics
Erythromycin
Anti-inflammatories
Cannabis
Anti-diabetics
Metformin
Cardiovascular
Opioids
Nicotine
Levodopa
Theophylline
Oral Contraceptive
Acyclovir
Caffeine
clinical presentation
Dehydration (assess mucous membranes, skin turgor)
Abdominal pain
Distress/Anxiety
Discomfort
Electrolyte abnormalities
Taste alterations
Weight loss
red flags
Significant dehydration = dizziness, sunken eyes, repeated vomiting, unable to keep liquids down for > 8hrs
Blood in vomit (hematemesis)
Coffee ground emesis
Altered Mental status, neurological deficits, recent head trauma
“Thunderclap” headache = severe HA with nausea and vomiting (HA youve never experienced before)
Fever and Stiff neck
dehydration in children
dry mouth, tongue, skin
lack of tears
decreased urine output (<4 wet diapers/ 24 hr)
irritability and lethargy
reduced skin turgor
sunken eyes
change in skin colour
sunken fontanel (infants)
dehydration in adults
dry mouth and tongue
feeling more thirsty than usual
weakness and lethargy
reduced need to urinate
sunken eyes
goals of therapy
Treat underlying cause and/or condition
Minimize the severity and frequency of nausea and/or vomiting
Prevent complications and reoccurrence of N/V
Minimize side effects of antiemetic medications
Decrease or eliminate the day-to-day disruptions caused by Nausea and/or vomiting
non pharm
ensure adequate hydration (at least 2.5 L of fluid daily); treat with oral rehydration solutions for moderate to severe cases of N/V
eat small, bland and frequent meals and avoid stimuli (noxious odours)
consult dietitian when necessary (nausea associated with food intolerances)
Avoid triggers (spicy foods, high fat foods, strong odours)
pharmacological therapy options
viral gastroenteritis (food poisoning) = lack of superiority of 1 agent over another
vestibular = antihistamines, anticholinergics
problems with GI motility = Metoclopramide or Domperidone
CTZ stimulation = Dopamine antagonists, serotonin antagonists
if monotherapy is refractory, combine antiemetics with different MOAs
types of nausea and vomiting
motion sickness
post-operative (PONV)
N/V of pregnancy (NVP)
chemotherapy induced (CINV)
motion sickness
normal physiologic response to unusual perception of motion
occurs due to abrupt changes in motion
car sickness
air sickness
sea sickness
involves inner ear and vestibular system
Acetylcholine and histamine = NTs responsible for signalling to medulla oblongata —> antihistamines or anticholinergics for treatment
Prevention > Treatment = adequate hydration, avoidance of smells/ foods that induce nausea, frequent small meals, relaxation therapy, pain treatment
motion sickness treatment
target Histamine and Acetylcholine!
take medication 30-60 mins BEFORE motion exposure
Dimenhydrinate (Gravol) if ≥2yr or Diphenhydramine (Benadryl) if ≥ 6y
more effective for short durations
onset = 15-30 mins
duration = 4-6 hrs
S/E (both) = sedation, anticholinergic effects (dry mouth, constipation, urinary retention)
S/E (dimenhydrainate/Gravol) = Paradoxical excitation (children)
Promethazine = longer duration of action than dimenhydrinate (not recommended)
ginger and acupressure wristbands (SeaBands) = not consistently demonstrated benefit but are widely promoted for antinausea effects
postoperative nausea and vomiting (PONV)
within 24 hr after surgery
includes all known pathways!
4 patient risk factors:
Female
Non-smoker
Hx of motion sickness/ PONV
Opioid use
other risks:
type of anesthetic (NO, volatile anesthetics)
dehydration
reducing risk factors = MORE EFFECTIVE management strategy
preventative therapy with anti-emetics in moderate-high risk patients
Non-pharm:
stimulate P6 acupuncture point
Avoid significant food intake 48 hr post-surgery
remain hydrated
avoid noxious odours
PONV treatment
combination therapy is more effective due to numerous NTs involved
ondansetron
haloperidol
dexamethasone
metoclopramide
dimenhydrinate
nausea and vomiting of pregnancy (NVP)
morning sickness —> can occur any time and may be constant throughout
normally occurs first trimester of pregnancy —> usually subsides by 16 weeks
severe, persistent NVP = Hyperemesis gravidarum (HG)
can continue throughout entire pregnancy
leads to weight loss, electrolyte imbalances, dehydration, nutritional deficiency
non pharm:
Avoid triggers = spicy food, food with high fat content, fried food, strong food odours
eat small and bland meals
prevent dehydration and electrolyte imbalance
fluid intake
rehydration solutions (if severe and/or accompanied by diarrhea)
treatment of NVP
1st line for MILD:
Diclectin (pyridoxine/ doxylamine) or Pyridoxine (Vit B6) alone, Ginger
1st line for Moderate-Severe:
Dimenhydrinate (gravol), Promethazine (diphenhydramine when necessary)
If NVP persists:
chlorpromazine, metoclopramide (for up to 5 days), Ondansetron (refractory cases only), Prochlorperazine
Resistant cases AFTER 1st trimester
Methylprednisolone IV
IV fluids if dehydration
dimenhydrinate (gravol)
1st line for motion sickness (short term)
used in persistent or mod-severe NVP (in addition to Ginger or Pyridoxine)
onset = 30 mins
effective in ALL types of N/V (except chemo-induced)
s/e = Sedation, anticholinergic effects (dry mouth, constipation, urinary retention, blurred vision), confusion, increased IOP
The elderly may be particularly susceptible
Paradoxical excitation in children
Additive sedation with alcohol or other sedating medications
diphenhydramine (benadryl)
1st line for motion sickness (use short term)
can be used in persistent or moderate-severe NVP (in addition to ginger or pyridoxine)
Dimenhydrainte is a better option!
onset = 30 mins
effective in ALL types of N/V (except chemo-induced)
s/e = sedation, anticholinergic effects (dry mouth, constipation, urinary retention, blurred vision), confusion, increased IOP —>elderly particularly susceptible
Additive sedation with alcohol or other sedating medications
Inhibits CYP2D6 and can increase serum levels of many drugs —> antidepressants and cardiovascular drugs
ginger (gravol natural source)
1st line in mild NVP (<1000 mg/d)
used for motion sickness, PONV
s/e = GI discomfort, diarrhea, dyspepsia, pepper-like irritant effect in mouth/throat
may inhibit in vitro CYP2c19 = clinical significance unknown
pyridoxine (vitamin B6)
1st line in MILD NVP
may be used alone or combined with doxylamine (diclectin)
used to treat NVP
onset = 1-2 hr
s/e = GI pain, HA, loss of appetite, photosensitivity, somnolence
diclectin (doxylamine succinate/pyridoxine)
Antihistamine in combo with Vit B6
1st line for NVP
Take at regular intervals (delayed release tablet)
2 tablets QHS PO, plus 1 tablet QAM PO, plus 1 tablet mid-afternoon PO
s/e (antihistamine) = VERY SEDATING, Diarrhea, disorientation, HA, Epigastric pain, Palpitations, Urinary retention
interactions:
MAOIs
Antimuscarinics
CNS depressants
Metoclopramide
dopamine antagonist
treatment for drug-induced nausea, migraine-induced nausea, gastroparesis, NVP (persistent), CINV
cross BBB
larger concern for EPS and Tardive dyskinesia
s/e = Diarrhea, abdominal cramps and distention, headache, hyperprolactinemia, drowsiness, fatigue, EPS
Additive sedation with alcohol or other sedating medications
interactions with dopaminergic medications/ disease states (Parkinsons disease)
Domperidone
dopamine antagonists
DO NOT USE IN PREGNANCY!
treatment for functional dyspepsia, gastroparesis
does NOT cross BBB
s/e = QT prolongation! Serious ventricular arrhythmias, hyperprolactinemia, Diarrhea, abdominal cramps and distention, headache, hyperprolactinemia, QTc prolongation
Additive sedation with alcohol or other CNS depressants.
Metabolized by CYP3A4; may be affected by CYP3A4 inhibitors or inducers.
haloperidol
dopamine antagonist
Low doses
treatment of PONV and refractory CINV (less effective than metoclopramide for refractory CINV)
s/e = QT prolongation, sedation, EPS
caution:
when used with other drugs that cause QT prolongation
in drugs/ disease states that have dopaminergic involvement (Parkinsons, antipsychotics or prokinetics)
highest likelihood of causing EPS
mild anticholinergic effects
dopamine receptor antagonists (Phenothiazines)
Chlorpromazine = persistent NVP
Perphenazine = PONV
Prochlorperazine = PONV, CINV, drug-induced nausea, persistent NVP
Promethazine = Motion sickness, PONV, gastroenteritis, moderate-severe NVP and persistent NVP
s/e = anticholinergic effects, sedation, hypotension (when administered IM or IV)
EPS/QT prolongation rare but possible at higher doses
5HT3 receptor antagonists (5HT3RA)
Granisetron
Ondansetron
decreases analgesic effects of tramadol
CYP3A4 inducers decrease ondansetron (CBZ, Phenytoin, rifmapin, St johns wort)
Palonsetron
treatment of PONV and acute CINV
alternative for persistent, moderate-severe NVP
s/e = constipation, HA, Diarrhea, QT prolongation, bradycardia, dizziness
risk for serotonin syndrome when combined with other serotonergic meds