7- periodontal classification
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What did the 1999 Armitage classification lead to?
Difficulties in establishing a clear diagnosis
Put preventative and therapeutic measures into practice
What are the 3 entities for classification of gingivitis and what is it based on?
Periodontal and gingival health
Gingivitis- dental biofilm induced
Biofilm alone
Systemic or local risk factors
Drug influenced gingival enlargement
Gingival diseases- non dental biofilm induced
based on history of periodontal disease, clinical attachment level
What characteristics does biofilm induced gingivitis have? (Biofilm alone)
Confined to gingiva
Plaque main etiological factor
Inflammation changes colour, shape, texture, bleeding on stimulation, elevated sulcular temp
No bone loss, stable clinical attachment
Reversible
What are 6 systemic or local risk factors of gingivitis?
Smoking
Hyperglycemia- diabetes
Nutritional factors
Pharmacological agents
Sex steroid hormones
Haematological conditions
How does smoking cause gingivitis?
Microvascular vasoconstriction and fibrosis masks clinical signs like bleeding despite underlying pathology
How can nutritional factors cause gingivitis and how will the gingiva look?
Ascorbic acid (vitamin c) deficiency can exacerbate gingiva response to plaque
Gingiva looks bulbous, spongy, hemorrhagic, swollen, erythematous gingival lesions
How can pharmacological agents cause gingivitis?
Oral contraceptives cause higher incidence of gingival enlargement, inflammation- but reversible
Other drugs affect salivary flow, endocrine function

How do sex steroid hormones cause gingivitis?
Puberty- increases gingivitis
Menstrual cycle- minor gingivitis during ovulation, exudate increase- reversible
Pregnancy- in 2nd or 3rd trimester, gingivitis, pyogenic granuloma

How do hematological conditions cause gingivitis?
Leukemia associated gingivitis- oral manifestations are acute
Cervical adenopathy
Petechia
Gingival enlargement
Mucous ulcers

What are example of drugs involved in drug induced gingival enlargement, characteristics and treatment?
Anticonvulsant- e.g Dilantin- 50% incidence
Immunosuppressant- cyclosporin- 25-30%
Ca2+ channels blocking agents- hypertensive drugs- nifedipine, verapmil, diltiazem- 15-20%
Higher prevalence in children, onset within 1st 3 months, stippling of gingiva, starts in anterior interproximal then expands
Control etiological factors, do full mouth gingivectomy- may need annually
What are 7 types of gingival diseases- non dental biofilm induced?
Genetic/developmental disorders- hereditary gingival fibromatosis
Specific infections
Inflammatory and immune conditions
Reactive processes
Neoplasms
Endocrine, nutritional and metabolic diseases
Traumatic lesions
Gingival pigmentation
What are the different type of origins for specific infections which cause gingival lesions?
Bacterial- neiserra gonorrhoeae, treponema pallidum, mycobacterium tuberculosis, streptococcal gingivitis
Viral- coxsackie, herpes, varicella zoster, molluscum contagiosum, HPV
Fungal- Candidiasis, histoplasmosis- granulomatous
What is herpes simplex virus type 1 responsible for?
Primary Herpetic gingivostomatitis- primary infection- painful ulcers, edema, stomatitis, high fever, malaise, vesicles rupture causing crusty lips
Need palliative treatment
Recurrent oral herpes- virus reactivates in 20-40%
What are the different types of inflammatory and immune conditions?
Hypersensitivity- conatct allergy of dental materials, toothpaste, mouthwash, foods presentation of type 4 sensitivity
Plasma cell gingivitis- velvet erythematous gingiva, dense infiltrate of plasma cells in lamina propia
Erythema multiforme- produces froth which rupture and leave ulcers, swollen crusty lips
What are the types of neoplasms associated with gingival diseases?
Premalignant- leukoplakia, erythroplakia
Malignant- oscc, leukemia, lymphoma (Hodgkin, non Hodgkin)
What are examples of endocrine/nutritional/metabolism diseases?
Vitamin deficiencies-
Fat soluble vitamins- a, d, e
Water soluble- complex band vitamin c
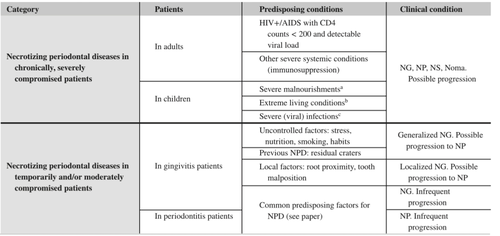
What are the 3 entities for classifying periodontitis?
Necrotising periodontal diseases
Periodontitis
Periodontitis as a manifestation of systemic disease
What is the difference between necrotising gingivitis and necrotising periodontitis?
NG- pain, ulcers, inflamed, erythema, halitosis, decapitated interdental papilla
Sometimes with fever, cervical lymphadenopathy- indicates severity
Gray white pseudomembranous lesions- fibrin, bacteria, wbc, epithelial cell remains
NP- diff stage of same disease, loss of attachment, necrosis of gingival tissues, pdl, alveolar bone
Common in immunosuppressed and malnourished
What is necrotising stomatitis?
Evolution of NG and NP
Affects beyond mucogingival junction- tongue, Buccal mucosa or palate
Erosions, ulcers, necrosis of bone
How can systemic diseases that affect the periodontum be grouped?
Genetic disorders affecting immune response or ct
Metabolic and endocrine disorders
Inflammatory conditions
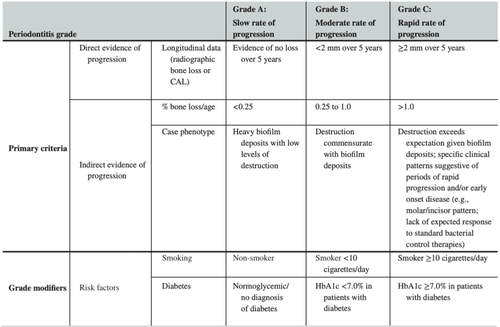
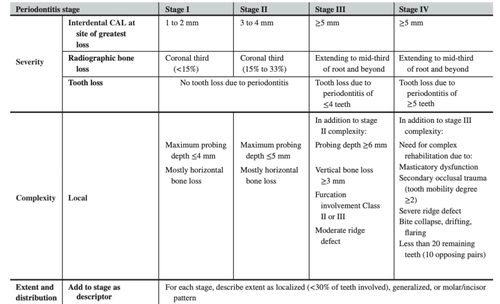
How is periodontitis divided into stages and grades?
Stage 1- initial
2- moderate
3- severe with potential for tooth loss
4- severe with potential for loss of dentition
Extent and distribution- localised, generalised, molar incisor distribution
Grade A- slow progression- lots of plaque proportionally to bone loss
B- moderate- plaque amount proportional to bone loss
C- rapid- little plaque proportionally to bone loss
What is a periodontal abscess and how can it arise?
Localised accumulation of pus within gingival wall of periodontal pocket
Easily detectable clinical symptoms
Pulp necrosis, periodontal infections, trauma, surgery, foreign body, pericoronitis
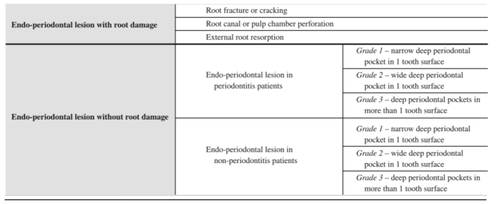
What is an endoperiodontal lesion?
Clinical conditions involving both pulp and periodontal tissues
Chronic or acute
Associated with recent traumatic or iatrogenic event
Signs- deep pocket close to apex, negative pulp vitality response
What is an occlusal trauma and the 2 types?
Occlusal forces cause injury- tissue changes in attachment apparatus
Primary- to a tooth with normal periodontal support, no attachment or bone loss, excessive occlusal forces
Secondary- to a tooth with reduced periodontal support