Chapter 2: Social Determinants of Health (Week 2)
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
Chapter 2: Social Determinants of Health
Factors within a community or location that affect individual health.
Strongly influence health risks, daily functioning, and quality of life.
Six Categories
Social & Community Context – relationships, social support, community engagement.
Neighborhood & Built Environment – housing, safety, transportation, green spaces.
Health & Healthcare – access to care, insurance, provider availability.
Economic Stability – income, employment, poverty level.
Food & Nutrition – access to healthy food, food security.
Education – literacy, language, educational attainment.
Management of Care
Case Management: Explore resources that support client independence.
Safety and Infection Control
Accident/Error/Injury Prevention: Protect clients from harm.
Home Safety: Assess environment for fire and other hazards.
Health Promotion and Maintenance
Developmental Stages & Transitions: Recognize cultural/religious influences on family functioning.
Health Screening: Perform health history + risk assessments.
Lifestyle Choices: Evaluate alternative/homeopathic practices.
Health Promotion/Disease Prevention: Plan and participate in health education.
Psychosocial Integrity
Cultural Awareness/Influences: Assess client’s culture/ethnicity when planning/evaluating care.
Stress Management: Implement measures to reduce environmental stressors.
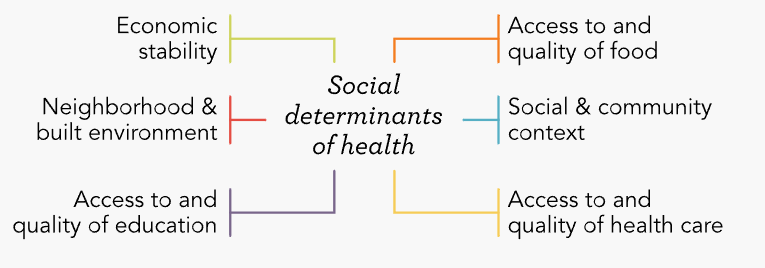
Social Determinants of health (Image)
Social & Community Context – relationships, social support, community engagement.
Neighborhood & Built Environment – housing, safety, transportation, green spaces.
Health & Healthcare – access to care, insurance, provider availability.
Economic Stability – income, employment, poverty level.
Food & Nutrition – access to healthy food, food security.
Education – literacy, language, educational attainment.
Health disparities
Preventable differences in disease, injury, violence, or access to health.
Racial inequalities
Impact access to education, housing, income, and employment → higher illness & death rates in minority groups.
Vulnerable populations
Higher risk for poor health, limited access to care, food insecurity, shorter life expectancy.
Social justice
Ensures equitable distribution of resources so vulnerable populations receive fair health opportunities.
CLAS Standards (Culturally and Linguistically Appropriate Services)
Promote workforce diversity and responsiveness to cultural needs.
Provide language assistance and information in clients’ preferred language.
Support ongoing improvement and accountability for culturally appropriate care.
Recognize culture-health congruence: health beliefs strongly influence care practices.
Assessing Cultural Beliefs
Understand variations within each culture.
Respect uniqueness of each client.
Learn about cultures present in the local community.
Cultural Competence
Nurse’s ability to respect dignity and preferences while acknowledging cultural differences, guiding diverse workforces and providing equitable care.
Cultural humility → Understanding & partnering with clients.
Cultural preservation → Supporting traditional practices beneficial to health.
Cultural accommodation → Facilitating safe/useful cultural practices.
Cultural repatterning → Helping clients modify practices harmful to health.
Cultural brokering → Mediating between client’s culture and healthcare system.
Cultural Assessment
Identifies how culture affects communication, space, time, social organization, environmental control.
Helps nurses provide culturally appropriate care.
Self-Assessment for Nurses (before assessing clients)
Am I aware of my own culture and biases?
Can I perform a culturally sensitive assessment?
Do I have knowledge to create culturally appropriate interventions?
What is my goal in learning about diverse populations?
Key Cultural Factors
Environmental Control
Beliefs about how the environment affects health.
If people believe they can control environment → engage in health promotion, prevention, treatment.
If people believe outcomes are predetermined → less likely to engage in health behaviors.
Harmony belief → prefer naturalistic solutions (mind-body-spirit balance).
Time Orientation
Focus on past, present, or future.
If focused on past/present → may be less motivated in preventive health behaviors (future benefit).
Social Organization
Importance of family or group in decision-making.
Decisions may be made by family/group, not just the client.
Nurse should:
Include family in teaching & planning if requested.
Respect client’s preference if they defer decisions to family/community.
Health Beliefs and Practices
Biomedical: Illness has a biological/physical cause (body = machine).
Common in U.S. medical model.
Naturalistic: Illness = imbalance with nature.
Eastern/Chinese medicine, Mexican hot-cold theory.
Magico-Religious: Illness = supernatural forces, good vs. evil.
Seen in faith healing, voodoo, witchcraft.
Biological Variations in Health
Linked to genetics and heredity.
Includes differences in:
Growth and development.
Lab test findings.
Skin color.
Susceptibility to disease.
Cultural Assessment Parameters
Ethnic background
Religious preferences
Family structure
Language & literacy needs
Communication needs
Education level
Cultural values
Food patterns
Health promotion/maintenance practices
Types of health practitioners used
Medicines, remedies, treatments, therapies
Steps of Data Collection
Collect self-identified data (ethnicity, religion, family, food patterns, health practices).
Ask about client’s perceptions of health needs.
Identify how cultural factors affect nursing interventions.
Nursing Interventions
Build community partnerships:
Neighborhood associations.
Social media information exchange.
After-school/extracurricular activities.
Identify programs/resources for stress/crisis:
Emergency housing.
Financial assistance.
Services for vulnerable populations.
A nurse is preparing an educational program on cultural perspectives in nursing. The nurse should include that which of the following actions by community members are influenced by social and cultural determinants of health?
Select all that apply.
a
Changing methods of preparing food
b
Moving in with a parent to become their caregiver
c
Seeking care from a medical provider when ill
d
Family history of hypertension
e
Asking a faith healer to cure a mental illness
a Changing methods of preparing food
b Moving in with a parent to become their caregiver
c Seeking care from a medical provider when ill
e Asking a faith healer to cure a mental illness
Conveying Cultural Sensitivity
Address clients by last name unless invited otherwise.
Introduce yourself with name and role.
Be honest and authentic about what you know/don’t know regarding their culture.
Use culturally sensitive language.
Ask what clients already know about health problems/treatments.
Incorporate client preferences/practices into care when possible.
Avoid assumptions about clients.
Encourage questions to reduce misunderstanding.
Show respect for values, beliefs, and support systems.
Provide health teaching in primary language and at appropriate readability.
Using an Interpreter
Use when nurse/client cannot understand each other’s language.
Interpreter should know medical terminology.
Avoid family members as interpreters → privacy concerns & lack of objectivity.
Consider client’s preference for age/gender of interpreter.
Interpreter should not be from the same community as the client (to protect confidentiality).
Be aware of translation barriers: socioeconomic, religious, education, dialect differences.
Federal mandate: agencies must ensure interpreter services for clients with limited English proficiency.
Subcultures may affect how effectively translation occurs.
A nurse is working on a plan for primary prevention within a community that has cultural practices which are unfamiliar to the nurse. Place the steps the nurse will take for the cultural assessment in the correct order.
Determine the perception the clients have about their current health practices.
Organize data, including differences between the community’s culture and Western medicine.
Identify cultural factors that may influence the effectiveness of nursing actions.
Obtain an overview of cultural characteristics of the community.
Determine the perception the clients have about their current health practices.
1
Obtain an overview of cultural characteristics of the community.
2
Determine the perception the clients have about their current health practices.
3
Identify cultural factors that may influence the effectiveness of nursing actions.
4
Organize data, including differences between the community’s culture and Western medicine.
Neighborhood and Built Environment
Refers to quality of surroundings: air, land, water, housing, and community spaces.
Positive factors: sidewalks, bike lanes, green spaces.
Negative factors: crime, violence, industrial complexes (pollution).
Includes access to transportation and healthy food stores.
Nursing Role
Identify environmental health risks and use advocacy to improve environmental quality.
Promote eco-friendly practices and educate the public on environmental health.
Apply toxicology knowledge → understand effects of chemical exposure on at-risk populations.
(e.g., refer to National Library of Medicine resources).
Data Collection
Availability of accessible, safe, clean parks and public spaces.
Homes/workplaces built to code.
Low crime rates.
Access to potable water & sewage systems.
Safe traffic patterns.
Environmental Risks (TAWC)
Toxins: lead, pesticides, mercury, solvents, asbestos, radon.
Air pollution: CO, particulate matter, ozone, lead, aerosols, nitrogen dioxide, sulfur dioxide, tobacco smoke.
Water pollution: wastes, soil erosion, runoff chemicals.
Contamination: food products contaminated with bacteria, pesticides, radiation, medications (growth hormones, antibiotics).
Roles for Nurses
Facilitate public participation in environmental improvements.
Perform risk assessments (individual + population).
Implement risk communication (clear hazard education).
Conduct epidemiological investigations.
Participate in policy development.
Environmental Health Assessment: “I PREPARE”
I – Investigate: potential exposures.
P – Present Work: current job, PPE use, exposure trends, safety practices.
R – Residence: housing age, remodeling, chemical storage, water supply.
E – Environmental Concerns: air, water, soil, local industries, waste sites.
P – Past Work: history of jobs (farming, military, seasonal work).
A – Activities: hobbies (gardening, fishing, soldering, hunting, pesticide use, etc.).
R – Referrals & Resources: EPA, OSHA, SDS, local health dept., poison control.
E – Educate: risk reduction, prevention, follow-up.
Primary vs Secondary vs Tertiary Environmental Health Prevention
(Prevent exposure before it happens)
Individual
Educate individuals on reducing environmental hazards.
Community
Educate groups on environmental risks.
Advocate for safe air & water.
Support programs for waste reduction & recycling.
Advocate for waste management policies.
(Detect early & limit severity)
Individual
Survey for environmental/occupational-related conditions.
Obtain environmental health histories.
Monitor workers for chemical exposure.
Screen children (6 months–5 years) for blood lead levels.
Community
Survey for health conditions linked to environmental exposures.
Assess schools, neighborhoods, work sites for hazards.
(Reduce impact & promote rehab after exposure)
Individual
Refer homeowners to lead abatement programs.
Educate asthma clients about environmental triggers.
Community
Advocate for legislation & policies addressing environmental issues.
Support toxic waste cleanup and hazard removal efforts.
Global Health
Health care delivery and problems worldwide affect population health across countries.
Global initiatives improve worldwide health status & equity.
Health for All in the 21st Century (HFA21) → promotes productivity through access to healthcare globally.
Measuring years of life lost to disability or early death = indicator of global disease burden.
Influences
Wars & political unrest
Natural & man-made disasters
Limited resources in developing nations
International travel (disease spread)
Sanitation practices
Climate change
Maternal health
Nutrition
Global Health Goals
(From UN Millennium Development Goals → Sustainable Development Goals, 2015)
End hunger & extreme poverty.
Ensure worldwide access to primary education.
Empower women, promote gender equality.
Sustainable ecosystem use (forests, oceans).
Global partnerships & equality.
Promote well-being & healthy lives.
Ensure sustainable water, energy, sanitation.
Encourage economic growth & innovation.
Safe human settlements/cities.
Combat climate change.
Promote peaceful & just societies.
Nursing Interventions
Support creation of healthcare roles in underserved countries.
Promote nursing as a key profession in health promotion & disease prevention.
Advocate with governments for nursing rights and supportive policies.
Develop environmental sustainability programs (“go green” initiatives).
Mentor & consult with communities internationally.
Access & Quality of Health Care
Primary care should be close to those in need & adaptable to income variation.
Community health nurses must:
Advocate for improved access.
Shift health care from acute/curative to primary prevention.
Promote equity & cost reduction through prevention.
Data Collection in Community Health Nursing
Evaluate adequacy and accessibility of health services in the community.
Identify barriers faced, especially by vulnerable populations.
Key Assessment Areas
Access to healthcare facilities/services.
Adequate providers (general + specialty).
Affordability of services.
Availability of benefits (employer, government, or free programs).
Community barriers limiting access.
Common Barriers
Inadequate insurance.
Inability to pay for services.
Health literacy issues.
Language & cultural barriers.
Lack of healthcare providers.
Geographic or social isolation.
Lack of communication tools (e.g., phones).
Lack of transportation to facilities.
Inconvenient service hours.
Negative attitudes of health personnel toward low-SES or diverse backgrounds.
Strict eligibility requirements for assistance programs.
A nurse is conducting health screenings at a community health fair and identifies several clients who require referral to a provider. Which of the following statements by a client indicates a barrier to accessing health care?
a
“I don’t drive, and my son is only available to take me places in the mornings.”
b
“I can’t take off work during the day, and the local after-hours clinic is no longer in operation.”
c
“Only two doctors in my town are designated providers by my health insurance.”
d
“I would prefer to schedule an appointment with a doctor who is bilingual.”
b “I can’t take off work during the day, and the local after-hours clinic is no longer in operation.”
Microeconomic theory
Looks at individual choices (preferences, finances) and how they influence:
Cost of care
Resource distribution
Macroeconomic theory
Looks at large-scale trends (aggregate behaviors):
Economic growth
Employment
National spending on health
Organizations and Financing
Health care is both a human service and a business, shaped by economic influences.
Good health → stronger economy (increases productivity, wage-earning potential).
Challenges
High costs = barriers to care.
Providers may ration services or limit access to specific coverage types.
Government Role (U.S.)
Provides direct health services.
Offers public information & protection.
Sets policies to guide providers.
Assists both providers & public with finances.
International Health Organizations
World Health Organization (WHO)
Provides daily info on internationally important diseases.
Sets global standards for antibiotics & vaccines.
Focus areas:
Health care workforce & education
Environment & sanitation
Infectious diseases
Maternal & child health
Primary care
Federal Health Agencies
Veterans Health Administration
Finances health services for active & retired military personnel and dependents.
U.S. Department of Health & Human Services (HHS)
Directed by the Secretary of Health.
Funded through federal taxes.
Includes multiple agencies:
Administration for Children and Families (ACF)
Administration for Community Living (ACL) – supports needs of aging & disabled populations.
Centers for Medicare & Medicaid Services (CMS) – manages Medicare, Medicaid, HIPAA, SSI, AFDC, disability insurance.
Agency for Healthcare Research & Quality (AHRQ) – conducts research to improve quality, affordability, & safety.
Centers for Disease Control & Prevention (CDC) – disease prevention & control, U.S. and international.
Agency for Toxic Substances & Disease Registry (ATSDR) – decreases harmful exposure to toxic substances.
Food & Drug Administration (FDA) – ensures food and drug safety, evaluates medications.
Health Resources & Services Administration (HRSA) – oversees nursing, medicine, dentistry education & distribution.
Indian Health Service (IHS) – promotes health for American Indians & Alaska Natives.
National Institutes of Health (NIH) – supports biomedical research & training.
Substance Abuse & Mental Health Services Administration (SAMHSA) – focuses on behavioral health, reducing negative effects of substance use & mental illness.
State Departments of Health
Funded by: State legislature + federal public health agencies
Responsibilities:
Manage WIC (Women, Infants, and Children) program → promotes nutrition for women, infants, and children up to age 5 of low SES.
Oversee CHIP (Children’s Health Insurance Program) → expanded coverage for uninsured children not qualifying for Medicaid.
Establish state-level public health policies.
Provide support to local health departments.
Administer Medicaid program.
Report notifiable communicable diseases within the state to the CDC.
State Boards of Nursing
Develop & oversee Nurse Practice Act.
License RNs and LPNs.
Oversee schools of nursing within the state.
Local Health Departments
Funded by: local taxes with state + federal support.
Focus: Health of local citizens through community-level programs.
Services & Roles:
Identify & intervene in community health needs.
Collaborate with local officials, businesses, and stakeholders.
Report communicable diseases to state departments of health.
Nurses’ roles at the local level → caregiver, advocate, case manager, referral source, counselor, educator, outreach worker, disaster responder, surveillance expert, community mobilizer.
Health Care Organizations
U.S. health care system shaped by federal agencies, private organizations (insurers, employers), and global health organizations.
International Health Organizations
World Health Organization (WHO)
Provides daily info on internationally important diseases.
Sets global standards for antibiotics & vaccines.
Focus areas:
Health care workforce & education
Environment & sanitation
Infectious diseases
Maternal & child health
Primary care
Federal Health Agencies
Veterans Health Administration
Finances health services for active & retired military personnel and dependents.
U.S. Department of Health & Human Services (HHS)
Directed by the Secretary of Health.
Funded through federal taxes.
Includes multiple agencies:
Administration for Children and Families (ACF)
Administration for Community Living (ACL) – supports needs of aging & disabled populations.
Centers for Medicare & Medicaid Services (CMS) – manages Medicare, Medicaid, HIPAA, SSI, AFDC, disability insurance.
Agency for Healthcare Research & Quality (AHRQ) – conducts research to improve quality, affordability, & safety.
Centers for Disease Control & Prevention (CDC) – disease prevention & control, U.S. and international.
Agency for Toxic Substances & Disease Registry (ATSDR) – decreases harmful exposure to toxic substances.
Food & Drug Administration (FDA) – ensures food and drug safety, evaluates medications.
Health Resources & Services Administration (HRSA) – oversees nursing, medicine, dentistry education & distribution.
Indian Health Service (IHS) – promotes health for American Indians & Alaska Natives.
National Institutes of Health (NIH) – supports biomedical research & training.
Substance Abuse & Mental Health Services Administration (SAMHSA) – focuses on behavioral health, reducing negative effects of substance use & mental illness.
States Health Agencies
Manage WIC (Women, Infants, and Children) program → promotes nutrition for women, infants, and children up to age 5 of low SES.
Oversee CHIP (Children’s Health Insurance Program) → expanded coverage for uninsured children not qualifying for Medicaid.
Establish state-level public health policies.
Provide support to local health departments.
Administer Medicaid program.
Report notifiable communicable diseases within the state to the CDC.
Boards of Nursing
Local Health Department
Identify & intervene in community health needs.
Collaborate with local officials, businesses, and stakeholders.
Report communicable diseases to state departments of health.
Nurses’ roles at the local level → caregiver, advocate, case manager, referral source, counselor, educator, outreach worker, disaster responder, surveillance expert, community mobilizer.
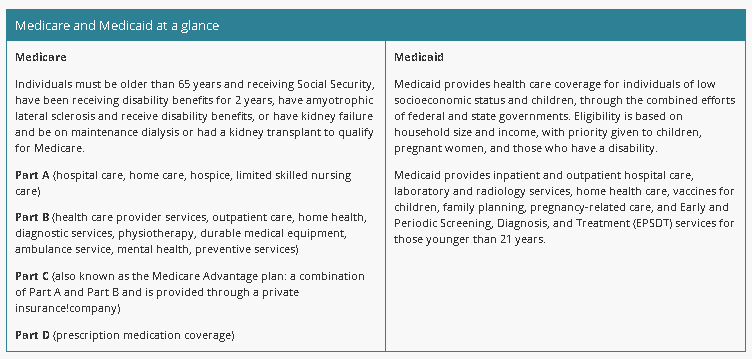
Medicare vs Medicaid (Table)
Age/disability-based, structured into 4 parts (A–D).
A: Inpatient
B: Outpatient
C: Advantage w/ A + B through private insurers
D: Drugs
Income-based, broader coverage for vulnerable populations, especially children & pregnant women.
Financing
Sources
Individual payment (self-pay, out of pocket).
Organized insurance (health maintenance organizations, private insurance, employer benefits).
Health maintenance organizations (HMOs) → comprehensive care by designated providers.
Preferred provider organizations (PPOs) → set service rates with incentives for in-network providers.
Medical savings accounts (MSAs) → pre-tax money saved for medical expenses.
Public funding (Medicare, Medicaid, government programs).
Affordable Care Act (ACA)
Goal: Increase affordability and access to insurance, reduce federal healthcare spending.
Key elements:
Dependents can stay on parents’ insurance until age 26.
No denial for pre-existing conditions (children under 19).
No lifetime limits on coverage.
Covers preventive services.
Self-Pay
Patients responsible for costs not covered by insurance.
Some clinics use sliding-fee scales based on income.
Nursing Interventions
Use community assessments to identify barriers to care.
Stay aware of standards & organizations influencing care.
Advocate for distributive justice in healthcare.
Collaborate with local, state, and federal agencies.
Help individuals/groups obtain access to care.
Maintain knowledge of economic principles to address healthcare funding & policy.
Economic Stability
Ability to access resources for life necessities: money, housing, food, employment.
A stable job provides a consistent living wage.
Data Collection
Availability of diverse and multiple job opportunities.
Jobs with advancement potential.
Salaries that cover cost of living.
Thriving businesses that attract economic growth.
Poverty & Homelessness
Federal poverty level determines eligibility for assistance (Medicaid, welfare).
Poverty limits ability to pay for food, shelter, transportation, clothing, healthcare.
Neighborhood poverty = poor housing, low employment, higher disease/death rates.
Extreme poverty → inadequate housing & homelessness.
Homeless individuals:
No regular nighttime residence.
May live in shelters, institutions, temporary housing, or on the street.
Challenges:
Incidence/prevalence counts often inaccurate (transient populations, hidden homelessness).
Hard to locate homeless individuals (may stay with friends, reside in inaccessible areas).
Healthcare access:
Often delayed until crisis or acute exacerbation.
Poverty
Characteristics of Individuals
Insufficient insurance coverage
High-risk work and unsafe living environments
Poor nutrition due to food insecurity
Increased stress levels
Less likely to engage in preventive activities or seek health treatment
Higher rates of chronic illness and related physical limitations
Increased morbidity and mortality rates
Nursing Actions for Prevention
Coordinate free or low-cost health services and providers
Collaborate with businesses/employers to improve wages, benefits, and working conditions
Teach health promotion and disease prevention strategies
Establish community partnerships for culturally sensitive and competent services
Collaborate with housing insecurity resources
Homelessness
Characteristics of Individuals
Adults who are unemployed, earn low wages, or are migrant workers
Female heads of households
Families with children (fastest-growing segment)
People with mental illness (large segment)
Veterans
People with substance use disorders
Unaccompanied youth
Adolescent runaways (high incidence among LGBTQ+ adolescents)
Survivors of violence or neglect
People who have HIV/AIDS
Older adults with no support system
Health Issues
Upper respiratory disorders
Tuberculosis
Skin disorders (athlete’s foot) & infestations (scabies, lice)
Substance use disorders
HIV/AIDS
Trauma
Mental health disorders
Dental caries
Hypothermia & heat-related illnesses (environmental exposure)
Malnutrition
Nursing Actions for Prevention
1. Prevent individuals/families from becoming
Address underlying risk factors contributing to homelessness.
Refer clients with mental health disorders to therapy/counseling.
Enhance parenting skills to prevent youth from running away.
2. Alleviate existence
Refer clients to financial assistance, food supplements, health services.
Assist in locating temporary shelter and long-term housing options.
If no shelters exist, advocate with government officials to develop shelter programs.
3. Prevent recurrences
Advocate for political action to expand needed mental health & housing services.
Refer for employment, education, and assistance programs to address root causes.
Rural Residency
<20,000 residents; frontier areas: <6 persons per square mile.
Low population density → decreased access to care, poorer health status, reduced health-seeking behaviors.
Health Status
Nurses in rural settings often face limited resources and professional isolation.
Higher:
Infant & maternal morbidity rates
Diabetes mellitus & obesity
Suicide rates
Lower likelihood of:
Seeking preventive care
Meeting physical activity recommendations
Increased risks:
Trauma/injuries (farm machinery, drowning, ATV/snowmobile/motorcycle crashes)
Occupational hazards (agriculture, fishing, mining, construction)
Skin cancer (sun exposure)
Respiratory complications (exposure to pesticides, chemicals)
Stress-related mental health issues
Barriers to Health Care
Distance from services
Lack of personal/public transportation
Unpredictable weather or travel conditions
Inability to pay (underinsured/uninsured)
Shortage of rural hospitals/health providers
Priority Needs
Cancer prevention & care
Mental health care
Substance use prevention & treatment
Immunizations
Family planning
Addressing food insecurity
Nursing Actions
Assist clients in applying for assistance programs.
Use cultural competence in planning interventions.
Build trusting partnerships with community leaders.
Leverage local ties for outreach programs.
Teach prevention & protection measures (elements, chemicals, sun, occupational hazards).
Food Insecurity
Defined as limited access to affordable, nutritious foods.
In 2020, 10.5% of U.S. households (13.8 million) experienced food insecurity.
Higher rates of in households:
Incomes near/below poverty line
Single-parent households
Black or Hispanic household heads
Large metropolitan areas
Social Factors
Low literacy levels
Language barriers
Limited knowledge of nutrition & food safety
Lack of social support
Inadequate cooking supplies
Low income
Limited access to transportation for food
Advanced age (>80 years)
Lack of physical activity options
Tobacco or drug use
Limited use/knowledge of community resources
Impact
For children: impairs physical development & school performance.
For adults: worsens management of chronic diseases (hypertension, heart disease, obesity).
Can lead to hospitalizations and delayed healing.
Food Deserts
Urban areas: Members live ≥ ½ mile from a supermarket or grocery store.
Often surrounded by stores/restaurants offering high-calorie, low-cost, low-nutrition foods.
Rural areas: Members live > 10 miles from a supermarket or grocery store.
Healthy People 2030 Objectives
Reduce household food insecurity and hunger.
Eliminate very low food security in children.
Nursing Actions
Identify food deserts and assess community barriers.
Partner with & refer to organizations addressing food insecurity:
Food banks
Meals on Wheels
SNAP (Supplemental Nutrition Assistance Program)
WIC (Women, Infants, and Children)
National School Lunch Program
School Breakfast Program (provides ~¼ of daily recommended nutrients)
Encourage:
Milk & fruit servings
Two servings of bread/cereal or meat/meat alternatives (or combination of bread + meat)
Access to and Quality of Education
Education provides opportunities for:
Making a living wage
Obtaining health care benefits
Making better health decisions
Living in safer neighborhoods with better access to goods/services
Low education levels → poorer health outcomes, more stress, lower self-confidence, and reduced ability to secure steady income.
Vulnerable populations are disproportionately affected.
Data Collection
Standards & benchmarks:
Strong retention and graduation rates
Adequate supplies and competent teachers
Access & affordability:
Must be available in-person or virtually
Low SES & rural areas may lack internet or government funding for schools
Education influences the types of jobs available.
Must meet the needs of employers with varied skill demands.
Provides opportunities for preventive screenings (vision, hearing, obesity, mental health).
Access to libraries supports lifelong learning.
Nursing Interventions
Advocate for job training programs.
Promote literacy programs.
Support community-based efforts to encourage diversity in hiring.
Coordinate computer skills workshops.
Partner with schools to enhance cultural competency among educators.

Access to and Quality of Education
Schools with strong retention and matriculation rates
Institutions of learning that have adequate supplies and culturally competent educators
Access to libraries

Food and Nutrition
Availability of food and nutrients
Access to healthy food options
Reliable sources of food

Economic Stability
Diverse and multiple job opportunities
Salaries that can cover the cost of living for that area
Thriving businesses with potential to attract more business

Access to and Quality of Health Care
Affordable health care facilities and services
Adequate health care providers in general and specialty fields of expertise
Access to medical benefits (provided through employers or on the free market)

Neighborhood and Built Environment
Safe, clean, and accessible parks and public spaces
Access to fresh food supplies within a two-mile radius
Safe traffic patterns

Social and Community Context
Access to programs that aid during times of crisis
Support groups
Neighborhood associations
Rural Population
< 20,000 residents; frontier < 6 persons per square mile
Urban Population
20,000–49,999; central cities ≥ 1 million