Lecture 2 - Foundations of Image Analysis
1/43
Earn XP
Description and Tags
ONCOL 306 - Imaging. University of Alberta
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Image registration
the process of aligning two images to each other
what treatment techniques mainly use image registration
IGRT, multi-modality treatment planning, and adaptive treatment planning
image fusion
the combined display of two images after they have been registered to each other
what are three types of image registration
rigid registration
affine registration
deformable registration
rigid registration
a best-fit registration where image are not modified in order to match each other
shapes are rigidly maintained, so translation and rotation of image occur as a whole
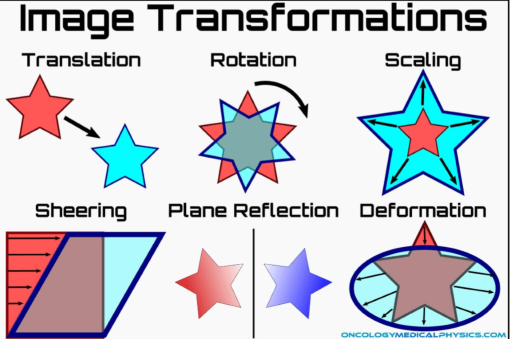
affine registration
modifications change the distance between points in an image, but do not change the relationship between the lines
translation and rotation occur but there will be some scaling, sheering and plane reflection
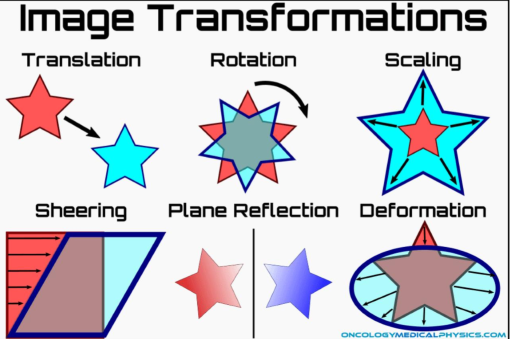
deformable registration
a complex registration process where one or more objects are reshaped in order to accurately align with each other
this can correct for organ motion as we deform one image to match another
what is the purpose of IGRT
to use in-room imaging before the radiation treatment in order to improve the precision of radiation delivery
these images are not used to plan treatments, just to check set-up
4 pros of IGRT
improve accuracy of treatment
allows for identification and correction of set-up discrepencies
allows for assessment of anatomical or tumor changes to aid replanning
decreases margin size resulting in less patient side effects
what is image matching?
the process of aligning the treatment image to the DRR in order to localize the treatment location
what happens once the images are aligned after matching?
shift information is used to move the treatment couch, putting the patient in the correct location relative to the machine isocenter
what does the RT need to be able to see to perform a match well, what can be used to help this?
the RT must be able to see key structures clearly (thus we often use kV images for better contrast)
image filters can be used to emphasize certain objects or structures that may be poorly visable on the standard view setting
we can only apply one image filter at a time
what types of structures can help the RT make an optimal match
bones, organs, fiducials, or foreign objects
what is a primary match structure and give an example
structures that best represent the treatment target or close proximity to the target
in prostate set-ups, we can either use the prostate itself or the pubic symphysis
what is the best primary match structure?
the best match structure is the tumor or target itself, if this is not visable, we look for surrounding anatomical landmarks that can provide a reliable reference for alignment.
what is a secondary match structure and give an example
structures that help with the image match but alone don’t accurately represent the target, helps confirm match
when matching prostate, a secondary match structure may be the pelvic brim
what is a manual-match
the imager software enables the RT to perform a matching of the treatment image to the DRR
what is an auto-match
the imager software performs a match and attempts to best match all anatomy in the image
what is an ROI (region of interest)?
the area to be searched during a 2D auto match
referred to as a VOI (volume of interest) in a CBCT automatch
is it better to have a large ROI or smaller?
the smaller the ROI focuses the automatch algorithm and speeds up the automatch
we don’t want to the computer to prioritize non-relevent information (ex: exclude head of femurs from prostate match)
what are the three P’s that an RT needs to understand to have the best possible image match
patient
diagnosis and staging will change the match: late stage prostate will need to account for nodes
plan
understand the technique, parameters, field and targets
protocols
department information on sequences of imaging, frequency of imaging, etc
give a general workflow of best-practice image guidance
review all patient and treatment related documentation
review prior images (if applicable)
determine imaging parameters
acquire quality images
assess anatomy
assess treatment positioning
perform image match (reference image) or image assessment (BEV)
initiate corrective action (adjust set-up, perform shifts, other)
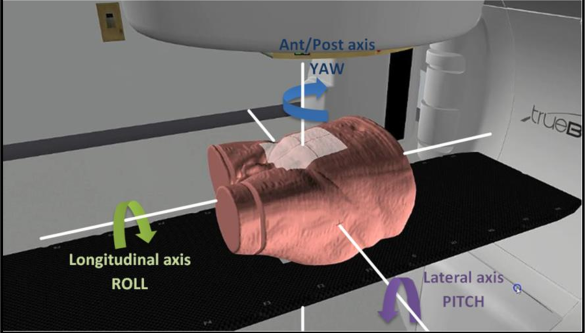
what are the three types of patient rotation (non-translational adjustments)?
pitch
roll
yaw
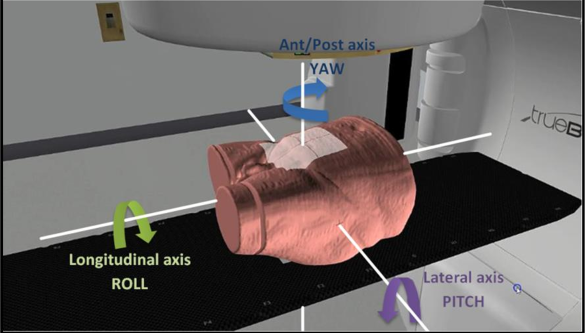
describe pitch
the rotational movement about the lateral axis, causing the patient to tip anteriorly or posteriorly
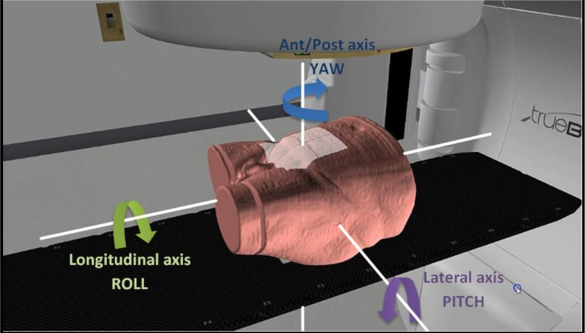
describe roll
patient rotation about the longitudinal axis which causes the patient to tilt side to side.
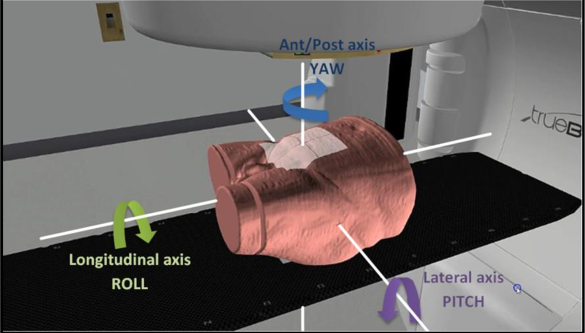
describe yaw
patient rotation about the ant/post axis causing the patient to turn left or right.
unless the treatment couch is 6DOF, how must patient rotations be adjusted
by adjusting the patient's position using additional supports or manual repositioning.
what are translational adjustments
Adjustments made to the patient's position along the x, y, or z axes to achieve the desired treatment alignment.
we can move the couch, not the patient to achieve precise positioning
what determines if the patient/couch needs to be shifted to ensure the treatment area is correctly placed within the path of the beam
the image match
what is Online Set-up Correction?
set-up correction done in real time with the patient on the treatment couch
will reduce both systematic and random errors through real-time matching and applying bed shift corrections within a treatment fractions
what two action levels are relevant to online set-up corrections
shift action level and image repeat action level
what is the shift action level (SAL)
a couch shift threshold for an image match at which the bed shifts should be applied
what is the value of an SAL
commonly half of the PTV margin
if PTV is 1 cm, SAL is 5 mm
what is the image repeat action level
a couch shift threshold for an image match at which bed shifts should be applied and subsequently verified with a repeat image
what is the value for an image repeat action level
typically equal to the PTV margin
if PTV is 1 cm, image repeat action level is 1 cm
what is Offline Set-up Correction
a method of set-up error correction done with the patient off the treatment couch (in-between treatment fractions)
we evaluate a series of shifts we have done for the patient to see if we can make an adjustment somewhere: if we are always moving the patient 1 cm superior, we should just have the patient move 1 cm sup in the field before we image (move from tattoo)
what errors does offline set-up correction account for? what does it not account for
offline set-up correction reduces systematic errors by evaluating set-up errors and applying a correction to a subsequent fraction. however, random set-up error is not accounted for
What is a No-action level protocol (NAL)
NAL is an offline set-up correction strategy
patient set-up errors are averaged over a predetermined number of fractions and corrected for
the mean shift is calculate and applied to the patient by remarking the isocenter
what is systematic set-up error?
set-up deviations that occur in the same direction and magnitude throughout the treatment course of RT
will remain unchanged over the course of treatment for a given patient
systematic set-up error is defined as the ___ of set-up errors and results in a ___ of dose from the treatment plan
mean value of set-up errors, results in a shift of dose from the treatment plan
give an example of systematic set-up error
After CT Sim images with BBs, they must be removed and a tattoo is placed instead. this placement may not be completely perfect
another example: perfect bladder fullness and empty rectum in CT Sim will never be accomplished 100% during image matching
what is random set-up error?
set-up deviaitons that can vary in direction and magnitude
less serious than systematic set-up error but PTV will still get underdosed
random set-up error is defined as the_____ of set-up errors, and results in a _____ of dose in relation to the treatment plan
standard deviation of set-up errors, resulting in a blurring of dose (in a non-constant direction)
what is residual set-up error
the remaining error after performing a correction