DSE OSCE - 2022
1/189
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
190 Terms
41-yo woman, pregnant; prev rheumatic fever with heart murmur (no valvular abnormality); allergy to penicillin. Positive history of infective endocarditis. Does she need to pre med?
- yes
- no
yes
- on my exam, this patient had a previous history of infective endocarditis. Pre-med IS indicated
Pre-med options for pregnant woman w/hx of infective endocarditis and penicillin allergy
- amoxicillin
- cephalexin
- clarithromycin
- ciproflaxacin
*clarithromycin*
I may not be correct, the correct option may be cephalexin. however I chose clarithromycin due to penicillin allergy, cross reaction with cephalosporins, and since clindamycin/erythromycin/azthromycin were not options. Ciproflaxacin is contraindicated in pregnancy. article for reference
What procedure can a dentist perform without consulting MD if a patient is currently taking bisphosphonates?
- endo therapy
- prophy and scaling
- extraction
- occlusal restoration
*occlusal restoration*
although the main HELL NO is extraction, completing endo therapy increases risk if the apex is compromised/damaged during therapy. I teetered on prophy and scaling, but since it did not specify supragingival, decided that the risk of scaling can negatively affect the periosteum of a bisphosphanate patient. ADA recommendations:
Pregnant person afraid of needles - stress management by putting patient in what position when in your chair (BEFORE they even get to the point of passing out)?
- supply oxygen
- place in Trendelenburg
- make patient sit up straight
- tell them to suck it up buttercup
place her in Trendelburg position
6 months pregnant had bleeding gums and mobile teeth, how should they be treated?
- immediate extractions
- do not treat until baby is born
- conservative debridement
- immediate endo
conservative debridement
.- pregnancy gingivitis: important to do ScRP (and stress good oral hygiene) to prevent plaque growth. The plaque can enter blood stream and stimulate patient's immune system to produce prostaglandins, which can trigger uterine contraction leading to early labor, premature birth, and a small baby.
Pregnant lady with a diastema in between #8 and #9 with deep probing depth and class 1 mobility on 8 and 9. What is the reason for diastema?
- chronic periodontitis
- distal drift
- normal during pregnancy
chronic perio
- increased incidence of periodontal disease during pregnancy => must emphasize good oral hygiene, and remove all their plaque so it doesn't lead to premature birth / low birth weight
Permanent staining as a result of tetracyline; did this happen?
- During development (as fetus)
- 0-5yrs
- 5-10 yrs
- 10-15 yrs
age 0-5 years
- remember that PERMANENT dentition does not begin calcification until birth
Pentobarbital (Nembutal) and Secobarbital (Seconal) are what type of drugs?
- benzodiazepines
- NSAIDS
- barbituates
- atypical antipsychotic
barbituates
- used primarily evening BEFORE appointment
A patient has an allergic reaction to a barbiturate, how do you treat?
- epinephrine
- diphenhydramine
- send to ER
benadryl (diphenhydramine)
A patient is on a steroidal medication. What information do you need to obtain before treating them?
- dose and pharmacy that filled the RX
- duration of prescription
- both dose and duration
*dose and duration*
- "The rule of twos": Ask whether the patient is currently on steroids or has been on corticosteroids for 2 weeks or longer within the past 2 years. You must go back 2 years in the history because it can take 2 weeks to 2 years for the adrenal glands to bounce back to normal function.
What is the most important factor when calculation medication dosage for a child
- age
- weight
- gender
- height
weight
A patient is confirmed to have trisomy 21. What are you initially concerned about?
- congenital heart defect
- Cushings
- cerebrovascular accident
congenital heart defects
Consider cardiac status and posibility of pre-medication:
- atrioventricular septal defect, patent ductus arteriosus, Tetralogy of Fallot
A patient has recently had a stroke. What is your first concern?
- when was their last cleaning
- are they on anticoagulants
- current blood pressure
Are they on anticoagulants
- Stroke patients could be on blood thinners, such as aspirin, dipyradamole (Persan- tine), clopidogrol (Plavix), or Coumadin, postrecovery. Prior to major surgery, always consult with the patient's physician to determine whether and when the blood thinners can be stopped and subsequently restarted.
What is the main symptom that differentiates anaphylaxis from syncope?
- bronchoconstriction
- clammy skin and pallor
- nausea, vomiting
Bronchoconstriction
- Anaphyalxis: intense itching, hives, flushing over the face and chest. Rhinitis, conjunctivitis, nausea, vomiting, abdominal cramps, and perspiration. Palpitation, tachycardia, sub- sternal tightness, coughing, wheezing, and dyspnea. BP drops rapidly and loss of consciousness or cardiac arrest can occur in severe cases.
-Syncope: fight or flight response. Anxiety, tachycardia, perspiration, light-headedness, and blurred vision are commonly experienced.
The Enzyme Linked Immune Absorbent Assay (ELISA) Test - a negative response for a person who had needle stick means what?
- the patient definitely has an HIV infection
- the patient has antibodies to HIV-1 present
- the patient definitely does not have an HIV infection
- the patient has no antibodies to HIV-1 present.
*the patient does not have HIV antibodies*
- consider that false negatives are a thing, life happens. We cannot definitively say they do not have HIV,but we can say that no Ab were detected.
14 year old presents with inflamed gingiva. Bloodwork indicates abnormal RBC, WBC, and platelets. Diagnosis?
- normal 14 year old
- hypothyroidism
- leukemia
- anemia
leukemia
-high WBC, lymphadenopathy, painful gingiva. Don't forget that WBC can be elevated OR decreased in leukemia! Gingival hypertrophy is a common sign/symptom
Stem indicates patient has recently taken medications, which one likely caused the rash present on their arm?
- Acetamiophen
- Barbituates
- Penicillin
- diphenhydramine
Penicillin allergy
- hives is a common response to penicillin allergies
Name the drugs that induce gingival hyperplasia
"CDC"
Calcium channel blockers (amlodipine, nifedipine)
Dilantin (anticonvulsants)
Cyclosporines
Drugs that may have increased chance of periodontal destruction
- "-statin"
- "-olol"
- "-ipril"
- "-ipine"
Amlodipine (Ca Channel Blocker)
Pt presents with white lesion, lateral anterior tongue. History of trauma (continuously biting it, ect). Resembled a papillary lesion.
- papilloma
- fibroma
- squamous cell carcinoma
History of trauma: Fibroma diagnosis
vs
Medical history: Papilloma
*If described as "cauliflower" assume papilloma
Pt has a history of multiple odontomas. What syndrome is suspected?
- Addison's disease
- Ectodermal dysplasia
- Gardner's syndrome
- Cushing's syndrome
Gardner's Syndrome
- colorectal polyposis
What is the treatment for a mucocele?
- corticosteroids
- excision with local glands
- biopsy
- antifungal medication
Excision
*image*
Pt presents with shallow ulcerated lesion on the lower lip that has been present for several months. Has been a farmer for several years. Likely diagnosis?
- squamous cell carcinoma
- traumatic burn
- apthous ulcer
- mucocele
Squamous cell carcinoma
- ALWAYS pay attention to medical history. Knowing that he is a farmer, you know that he spends the majority of his time in the sun; also knowing that the lesion has been present for an extended time. SCC is more common on the lower lip vs upper lip.
A patient was diagnosed with Hepatitis A, presentation of jaundice. How soon can you treat?
- 1 day
- 1 week
- 1 month
- 1 year
1 week
Patient presents with jaundice. Name three possible causes?
Liver Cirrhosis
Hep A
Hep C
Pt presents with missing teeth and no hair. What is the likely medical condition?
- Gardner's disease
- Ectodermal dysplasia
- Trisomy 21
- Paget's syndrome
Ectodermal dysplasia

Pernicious anemia is associated with:
- autoimmune destruction of parietal cells in stomach
- acute, chronic blood loss
- both
autoimmune destruction of parietal cells in stomach
- pernicious anemia = associated with intrinsic factor from parietal cells, which is required to absorb B12 from food
What does intrinsic factor do?
- allows iron to bind to hemoglobin
- prevents destruction on RBCs
- required for absorption of vit B12 from food
Required for the absorption of vitamin B12 from food
Another version Pernicious anemia is caused by:
- Decrease in intrinsic factor (required for absorption of B12)
- Chronic use of aspirin, NSAIDs, corticosteroids
- A variant of hemoglobin A (called hemoglobin S)
- Destruction of RBCs
decrease in intrinsic factor
- Schilling's test to evaluate B12 absorption; most commonly used to eval pts w/pernicious anemia
What is hemolytic anemia?
- autoimmune destruction of parietal cells in stomach
- genetic defect, includes variant of hemoglobin A (called hemoglobin S)
- RBCs destroyed, removed from bloodstream before normal lifespan is over
- Folic acid is deficient, patient presents w/neurologic symptoms
destruction of RBCs (think about it. hemo (RBC) lytic (destroy))
Hereditary Hemorrhagic Telangiectasia is associated with:
- B12 deficiency
- Pernicious anemia
- Iron deficiency
- hypertension
Iron deficiency
"Iron deficiency anemia"
Pt presents, upset with look of with canine and premolar area; spotted (pick up stains), pits and grooves on outer surface of teeth. Likely diagnosis
- hypoplasia
- hyperplasia
- abfraction
- erosion
hypoplasia
-consider that fact it is localized, likely not related to systemic disease

Several spots with yellowish concave areas in cervical 1/3rd of anterior teeth. Likely cause?
- erosion
- abfraction
- hypoplasia
- hyperplasia
Facial erosion due to acidic beverages

Once thought to be associated with BLUE SCLERA and multiple bone fractures
- hemolytic anemia
- grave's disease
- pernicious anemia
- dentinogenesis imperfecta
dentinogenesis imperfecta
- question stem refers to a picture of blue sclera

All of the following are symptoms of hyperthyroidism except:
- fatigue
- exopthalamus
- tachycardia
- tremor of extremities
fatigue is NOT a symptom
symptoms include:
nervousness, anxiety and irritability.
hyperactivity - you may find it hard to stay still and have a lot of nervous energy.
mood swings.
difficulty sleeping.
feeling tired all the time.
sensitivity to heat.
muscle weakness.
diarrhea.
Large space (diastema) between #11 and #12. What do you do?
- place implant
- removable partial denture
- fixed partial denture (bridge)
- do nothing
Do nothing
-let it be... seriously, if it ain't broke, don't fix it.
The greatest disadvantage of resin bonded bridges?
- staining
- debonding
- fracture
- less tooth reduction
debonding
What is gutta percha made of?
- barium salts
- zinc oxide
- silicate dioxide
- graliam prema
zinc oxide
Drug that increase the concentration of lidocaine in the blood?
- Prozac
- Asprin
- Propanalol
Propanalol
What is an advantage of a Maryland bridge?
- staining
- debonding
- fracture
- less tooth reduction
less tooth reduction
Minimum height for posterior crown preps
- 1-2mm
- 2-3mm
- 3-4mm
- 4-5mm
3-4mm
- a short clinical crown is defined as a tooth with <2mm of sound opposing parallel walls remaining after occlusal and axial reduction
Best initial treatment for maxillary oroantral fistula?
- antibiotics
- irrigation
- gauze pack
- two of the above
two of the above: antibiotics and irrigation
Medication taken for arthritis?
- propranolol
- benadryl
- naproxen
- aleve
naproxen
In an effort to improve gingival health, temporary crowns should be:
- undercontoured
- overcontoured
- left short of the margin
- extended past the margin
UNDERcontoured; bulbous crowns are not good for the gingiva.
Radiographs with many well-demarcated PARLs. What's next?
- initiate RCT
- endodontic testing
- incision and drainage
- extract
endo testing
- don't perform RCT or ext without confirming diagnosis. Radiographic hard tissue lesions may be benign
Minimum recommended occlusal reduction for a PFM crown
- 0.5mm
- 1mm
- 1.5mm
- 2mm
2mm
In order to preserve biological width the crown margin must be ___mm above the alveolar crest
(fill in the blank)
2mm
When preparing a tooth your goal is:
- minimal taper
- maximal taper
minimal taper
- conserve tooth structure, adequate retention, proper draw
What is the maximum amount of unsupported porcelain allowed/minimum thickness?
- 1.0mm
- 1.5mm
- 2.0mm
- 2.5mm
2mm
The most important treatment for ANUG is?
- antibiotics: chlorohexidine rinse
- debridement
- patient understanding the importance of oral hygiene
- explaining to the patient the link between oral health and systemic health
debridement - take away the disease causing factor. educating the patient is important too
Which presentation is gingivectomy indicated for?
- gingival hypertrophy
- gingival hyperplasia
- gingival recession
- hemostasis
gingival hyperplasia
Treatment plan for patient with a liver clot?
- antibiotic prescription
- irrigate
- apply pressure, re-assess
- two of the above
two of the above: irrigate, apply pressure, reassess
- liver clot: unstable, large, friable clot commonly forming in mucous membranes; lead to excessive bleeding and abnormal wound healing
- it looks like a mini liver... but in your mouth. #thatswhatshesaid ?
Image of mx and md full arch crowns with erythematous gingiva. What might be the issue?
- impingement on gums
- hyperocclusion
- increased VDO
impingement on gums
Patient presents with pain on swallowing when wearing their mandibular partial denture. All signs point to....
- TMJ disorder
- overextension of the lingual flange
- increased ridge resorption
overextension of the lingual flange
- difficulty swallowing can also be attributed to excessive VDO
Patient presents with space between mandibular 3rd molar to premolar, class II mobility on 3rd molar. Best treatment option?
- FPD
- RPD
- implant prosthesis
- full denture
Implant
Furcal involvement through and through w/class III mobility. Plaque control is an issue. Prognosis?
- questionable
- good
- poor
- hopeless
Hopeless
If you didn't say hopeless, please tell me how you would save that tooth #herodentistry
#1 present w/class III mobility, furcal involvement; #2 and #3 are missing. best way to restore?
- fixed bridge #1-4
- place two implant-supported crowns for #2 and #3; frequent recall to re-eval #1
- ext#1; implants for #2, #3, or both
ext#1, implants for 2, 3, or both
- #1 has hopeless prognosis
When shade matching, you struggle with finding the right color. You should choose ____ shade saturation, and ____ gray
- higher, more
- lower, less
- higher, less
- lower, more
choose lower shade saturation and less gray
Ceramic restorations should have similar ___ to adjacent natural teeth to have a good esthetic outcome.
- hue
- chroma
- value
value --> brightness
Worst location for an implant?
- mandibular anterior
- mandibular posterior
- maxillary anterior
- maxillary posterior
maxillary posterior (due to bone type)
Best location for an implant; best long term prognosis?
- mandibular anterior
- mandibular posterior
- maxillary anterior
- maxillary posterior
mandibular anterior (best bone)
Worst cement for a deep restoration?
- Glass ionomer
- zinc phosphate
- composite resin
- RMGI
Zinc phosphate
Best type of cement for short clinical crowns?
- resin bonded
- polycarboyxlate
- zinc phosphate
resin bonded
Zinc phosphate is the worst cement for what type of restoration?
- Class V
- Deep caries
- Shallow caries
deep caries (zinc phosphate is know for pulpal irritation)
Radiograph of amalgam restoration, patient complained of pain when provoked by hot or cold. What is the issue?
- apical periodontitis
- deep amalgam restoration
- galvanic shock
deep amalgam restoration
A periodontal pack stays in how long?
- 24 hrs
- 3 days
- 1 week
- 3 months
1 week
- periodontal dressing used to promote wound healing following flap surgery
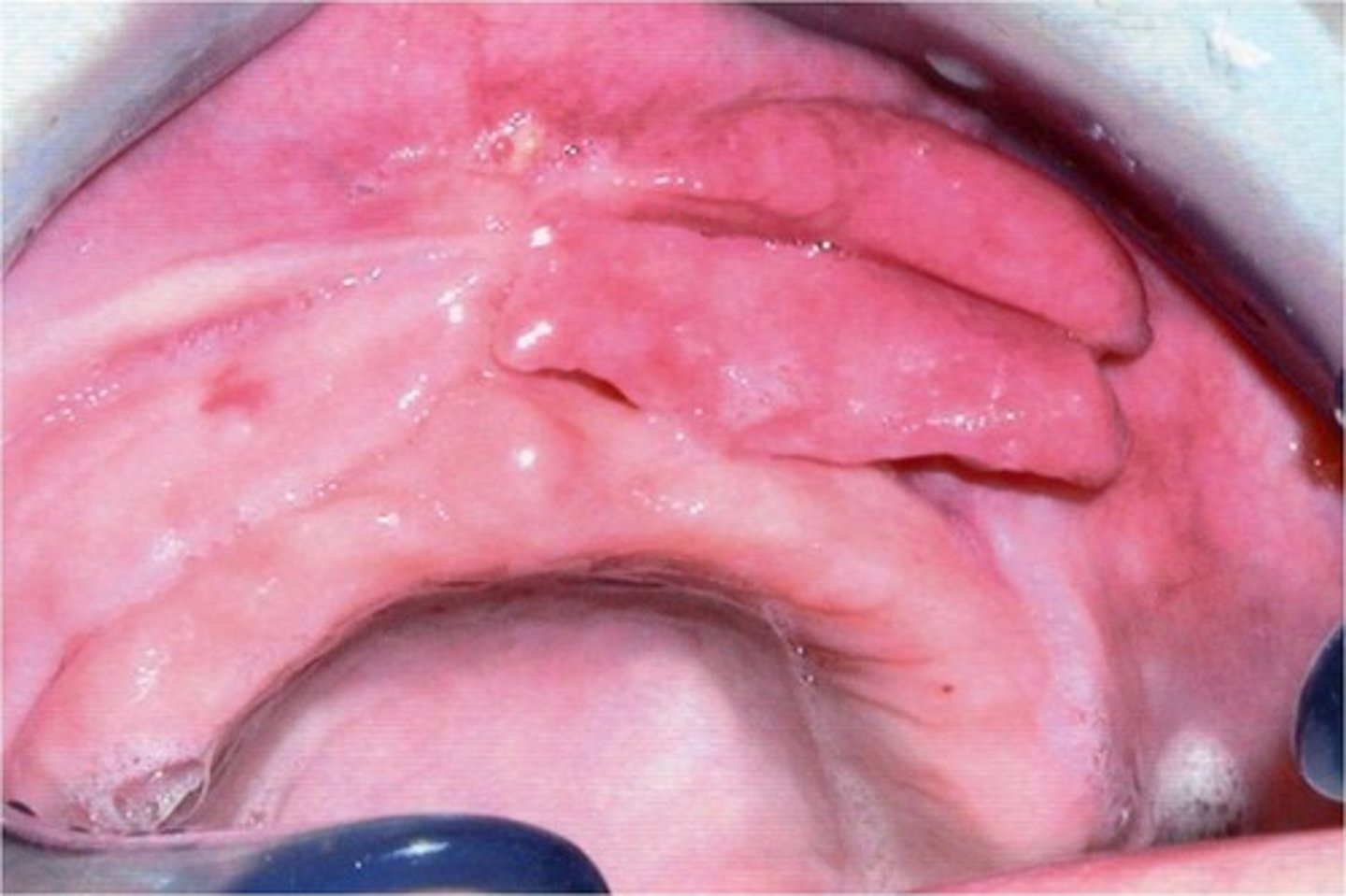
Question stem describes an epulis in a denture patient., photo included How would you treat?
- apply tissue conditioner
- leave alone
- prescribe antibiotics
- excision
excision
What is the main reason for periodontal flaps?
- visualize bone quality
- access for instrumentation
- greater surface field
- increase primary wound healing
access for instrumentation
Large maxillary torus in denture patient causing ill-fitting dentures. How would you treat?
- remove
- leave alone
- remove that section from denture base
remove torus
Characteristic of a major connector in a denture?
- provide relief
- does not act as a support element
- rigidity
- stability
rigidity
- transmit force equally to all areas
As required by OSHA, the autoclave is checked...
- daily
- weekly
- bi-weekly
- annually
weekly spore testing
Ortho case: what was the most important thing they did in the maxillary arch?
- close U and L diastemas
- align the teeth for future restorations
- adjust the occlusion for patient comfort
- promote movement of mandibular teeth
Alignment for future restorations (and hygiene)
What pain reliever do you give to a patient with kidney disease?
- aspirin
- acetaminophen
- morphine
- naproxen
acetaminophen
Picture of a diagnostic cast on a surveyor with the survey marker at the distal of #28, #31 is present but #30 and #29 are not. What is the survey marker pointing to?
- mesial guide plane
- rest seat
- site of termination for major connector
mesial guide plane
- the picture makes it obvious that you are surveying the distal of tooth #28; knowing that it is adjacent to an edentulous space you can see that this would be the location for a guide plane (marker extends to the gingiva)
What is a major complication of phlebitis?
- atrial fibrillation
- pulmonary embolism
- peripheral neuropathy
- myocardial infarction
pulmonary embolism
Patient complaining of space between teeth after an SRP?
- removal of tooth structure during SRP
- tooth movement is normal following SRP
- reduction in edematous tissue
- cause is unknown
Reduction of edematous tissue causing appearance of black triangle
1-2mm reduction of probe depth after SRP. What caused this?
- deposition of alveolar bone
- reattachment
- formation of long junctional epithelium
formation of long junctional epithelium
Patient has a shunt on the left arm, where do you obtain blood pressure?
- wrist
- right arm
- neck
- finger
right arm
- patient is on dialysis, take BP on side shunt is NOT present
(Very grainy) picture of #10 and #11, lingual surfaces. What is wrong with the gingiva?
- edema
- artifact
- squamous cell carcinoma
edema - enlargement of marginal and interproximal gingiva; smooth shiny surface, loss of stippling, diffuse redness
Space between mandibular premolar and molar in an older patient, #31 and #32 are not present, barely in occlusion w/#3. Why is this happening?
- supraeruption
- mesially drifting premolars
- malignant growth
mesially drifiting premolars
- this one is hard to visualize... but knowing this is an older patient makes you think mesial drift. Also, the occlusion w/#3 is preventing #30 from moving mesially (it is tipped)
Surgical stent fits the gums but the immediate denture doesn't fit, what do you do?
- re-construct the surgical stent
- re-construct the immediate denture
- relieve it until it seats
Relieve until it seats
Picture of the bottom of the tongue with multiple white lesions. Stated that the patient had complaint of sore gums and tongue, he had a fever of 101 degrees.Most likely diagnosis?
- Primary Herpetic Stomatitis
- Secondary Herpetic Stomatitis
- Herpangia
- Recurrent Apthous Stomatitis
primary herpetic stomatitis
-treat with palliative care
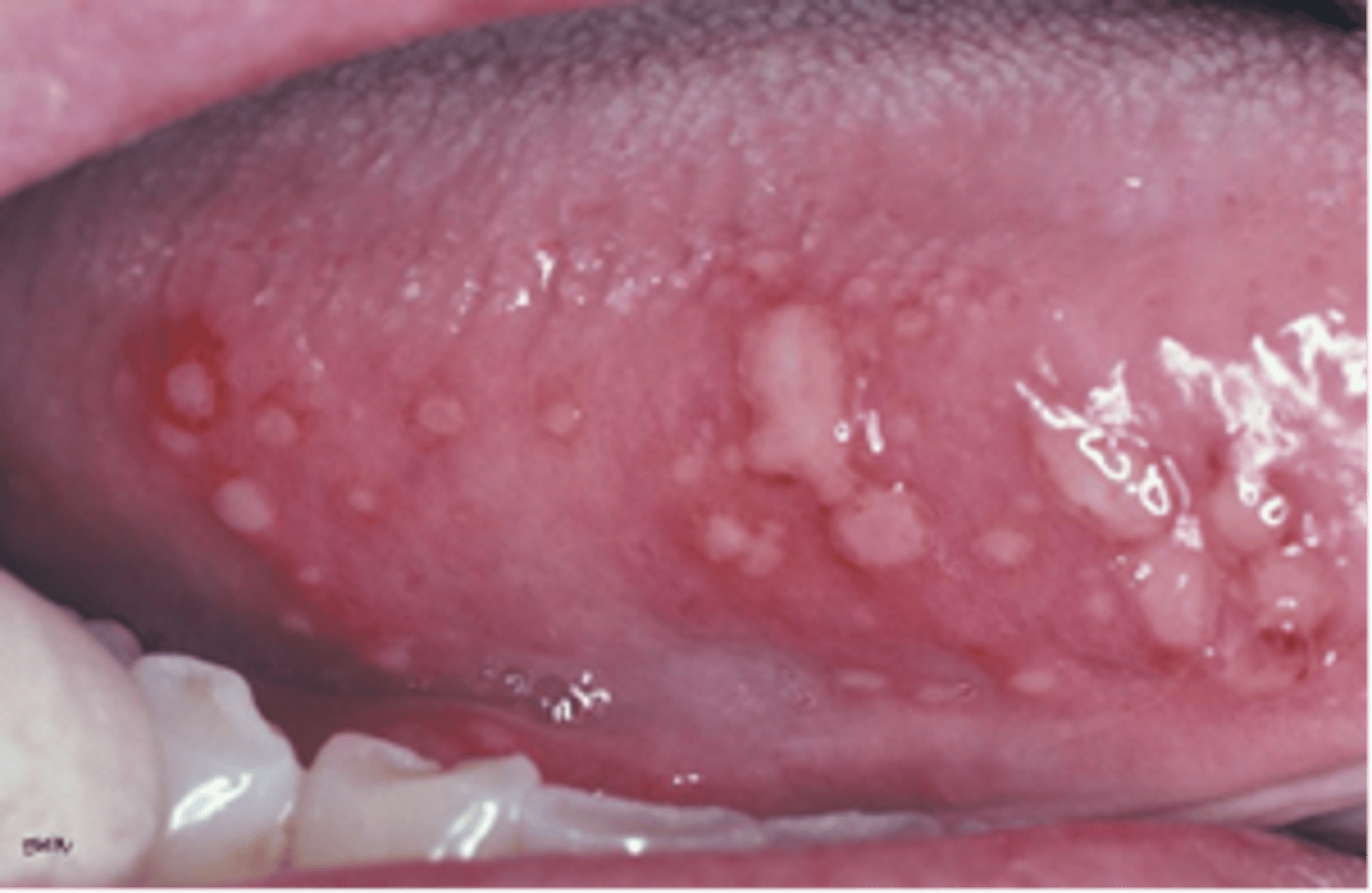
What is the treatment for primary herpetic stomatitis?
- antibiotics
- palliative
- do nothing
- antifungals
palliative care
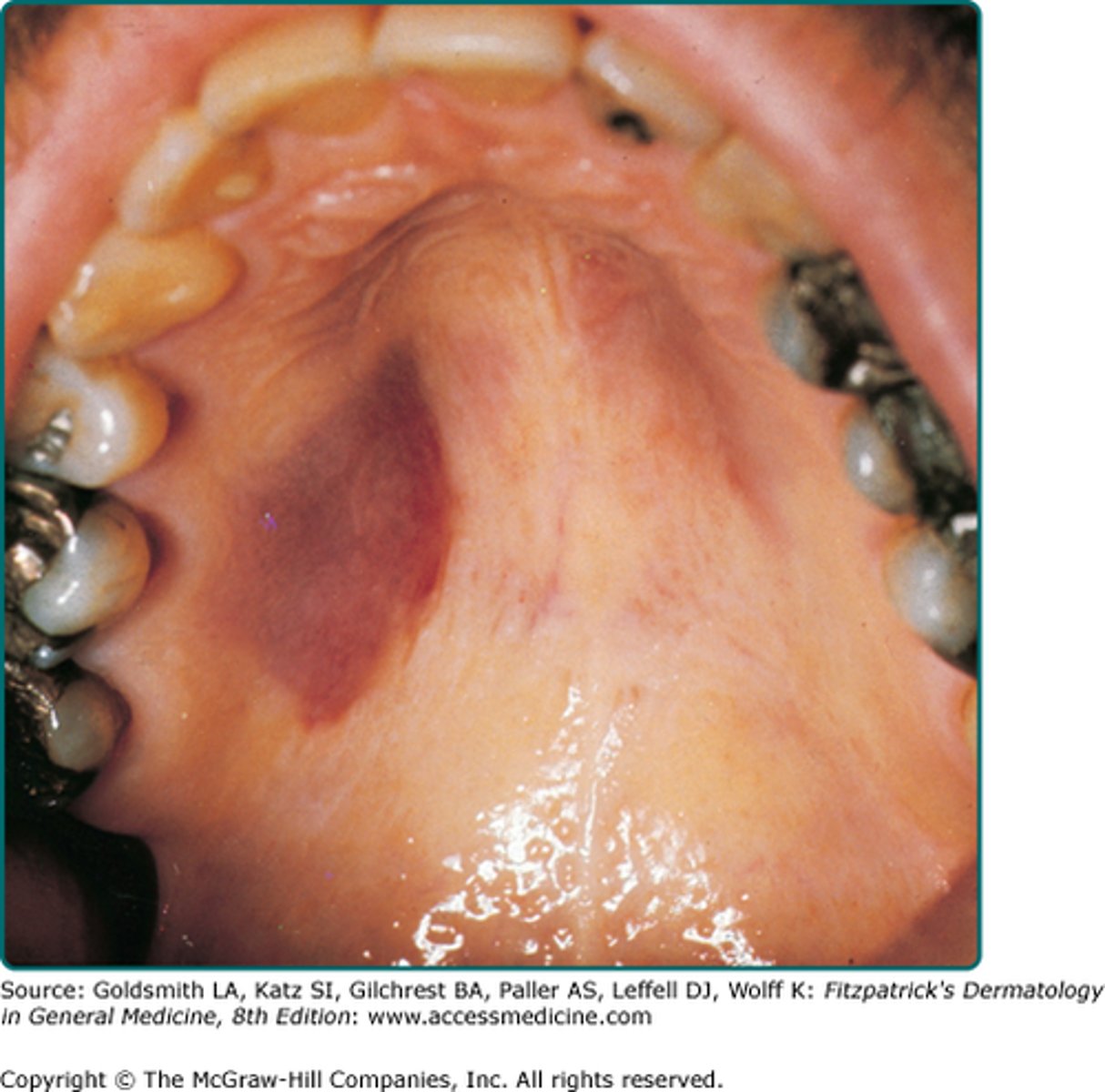
Adult patient with purple lesions on palate and said they had similar lesions on their body too. What is the most probable cause?
- Surge Weber
- Erthyema Multiforme
- HIV
- Malignant Melanoma
HIV
- lesions are Kaposi sarcoma
Lesion in the mouth that heals with a scar?
- Primary Herpes Labialis
- Minor Apthous Ulcer
- Major Apthous Ulcer
- Recurrent Herpes Stomatitis
major apthous ulcer
- minor ulcers heal without scarring
Arrows pointing to soft tissue mass on Floor of Mout, base of tongue. This is the opening of what?
- Stenson's duct
- sublingual salivary gland
- Wharton's duct
Wharton's duct; submandibular duct

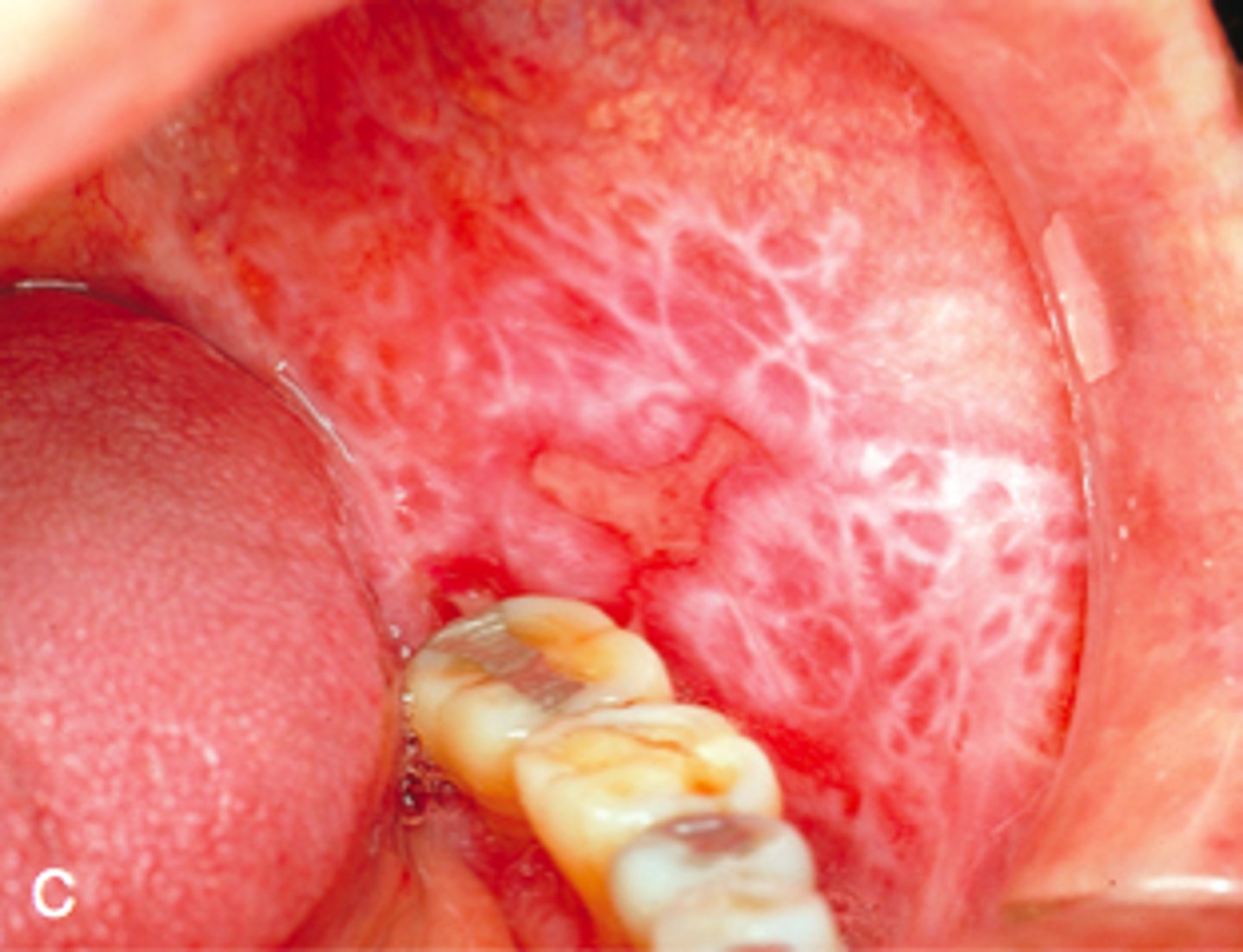
Tongue lesion is diagnosed as lichen planus. Lesion is asymptomatic, how do you treat?
- antifungal
- corticosteroids
- antibacterial
- chlorhexidine rinse
corticosteroids (there was no option for do nothing)
White lesion present on buccal mucosa. Likely diagnosis?
- leukoedema
- cheek biting
- lichen planus
- squamous cell carcinoma
lichen planus
- white lesion can be describe as Wickham striae
Panoramic radiograph with radiopacity below mandibular incisors. What is the likely condition?
- odontoma
- impacted incisor/canine
- supernumerary tooth
- osteoma
impacted tooth
- verify all teeth are present, if primary tooth is present without succedaneous, impacted tooth is likely.
- I had a lot of odontoma questions; look for 'mini teeth' in the radiopaque mass to diagnose compound odontomas

Gingival edema is caused by?
- aerobic bacteria
- anaerobic bacteria
- forces
anaerobic bacteria
Sensitivity post crown cementation is due to...
- inadequate cement
- microleakage
- too much cement
- reaction to crown material
microleakage
- marginal defects and gaps caused by polymerization shrinkage during placement
Before relining a complete denture, you must first establish:
- anterior guidance
- maximum intercuspation position
- posterior occlusion
- centric relation
posterior occlusion
Precision attachments should not be used in patient's with:
- poor ridge adaptation
- flabby tissue
- low dexterity
- high esthetic demand
Low dexterity
- case discusses older patient with arthritis
Purpose of a wedge during a restoration is?
- Good marginal seal
- Interproximal contact contour
- Adaptation of the matrix band
- Help with filling of the material
adaptation of the matrix band
Which medication is contraindicated in a patient with hyperthyroidism?
- acetaminophen
- epinephrine
- meperidine
- carbocaine
epinephrine
- avoid the use of vasoconstrictors in anesthetic
Patient was on penicillin for two weeks and now complains of a sore tongue. What do you do?
- cytology smear
- fungal test
- prescribe antibiotics
- send to emergency room
fungal test
- possible Candida infection
Image of a red, painful tongue in an uncontrolled diabetic. What is the likely diagnosis?
- malnutrition
- median rhomboid glossitis
- benign migratory glossitis
malnutrition
If there is a red and white lesion, which do you biopsy?
- only the red portion
- only the white portion
- red and white portions of the mixed lesion
- none of the above
both red and white portions
Most likely reason for sealants to fail?
- inadequate retention
- poor light curing device
- contamination
- patient bruxing habit
contamination
There is an unconscious patient in your living room, what do you do first?
- check to confirm if they are unconscious
- check pulse
- check breathing
- call for help
Check Breathing
(ABCs: Airway, Breathing, Circulation)
-oxygen not indicated if patient is breathing adequately
-- only give oxygen if true breathing difficulty
-- rule out obstruction due to improper position before administering oxygen
-- if necessary, stabilize and get to hospital