Stage 2
1/2471
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
2472 Terms
what is Heart Failure (HF)?
where the heart is unable to pump sufficiently to maintain blood flow to meet the body's needs.
what is End-diastolic volume (EDV)?
Volume of blood in ventricles at the end of diastole. Normally = 110-130 mL.
what is End-systolic volume (ESV)?
Volume of blood left in ventricles at the end of systole. Normally = 40-60 mL.
what is Stroke volume (SV)?
Amount of blood ejected from ventricles during systole/beat. Normally = 70-80 mL/beat.
what is Ejection fraction (EF)?
Fraction of end-diastolic volume ejected during a heart beat. SV/EDV = EF. Normally around 50-70%.
what is Cardiac Output (CO)?
Volume of blood ejected by each ventricle in each minute. Normally = around 5 litres in an adult at rest. SV X HR = CO.
What is preload?
The amount of blood presented to the ventricles.
what is Afterload?
The resistance against which the ventricles contract. (BP)
what is HFrEF?
Heart Failure with Reduced Ejection Fraction, characterized by a reduced EF
- dilated cardiomyopathy - wall of V becomes thin as heart enlarges - decreases pump efficiency, reducing SV
what is HFpEF?
Heart Failure with Preserved Ejection Fraction, characterized by a preserved EF - thickening and stretching of arteries
- hypertrophic cardiomyopathy, where V walls thicken and stiffen - V filling capacity drops resulting in drop in SV
what is aim in treatment of HFrEF?
no longer aims to decrease mortality - now it is to prevent hospitalisation
what are the risk factors of developing HF?
- LV hypertrophy - thickening prevents enough space for blood to actually fill it - so not enough leaves it
- chronic HTN - causes heart stretch, decreasing contractility
- any MI - ischaemic tissue cannot contract
- thyroid disease - related to arrhythmias and DM
- prolonged arrythmias
what is the pathophysiology of HF?
- reduced CO, leading to blood pressure drop
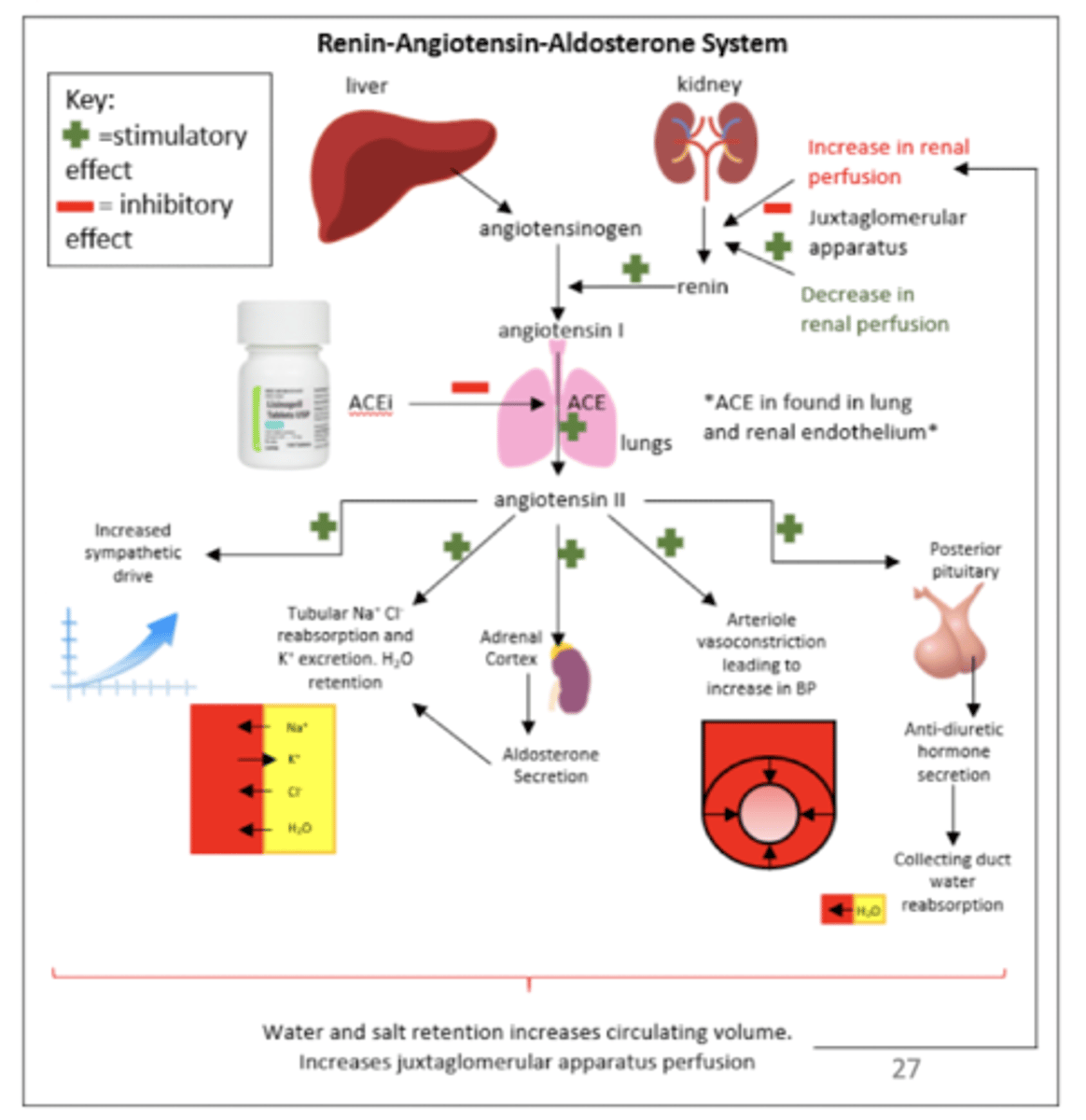
- RAAS and SNS stimulated: increasing contractility, tachycardia and vasocontriction (all bad corrective mechanisms)
- exhausts failing heart
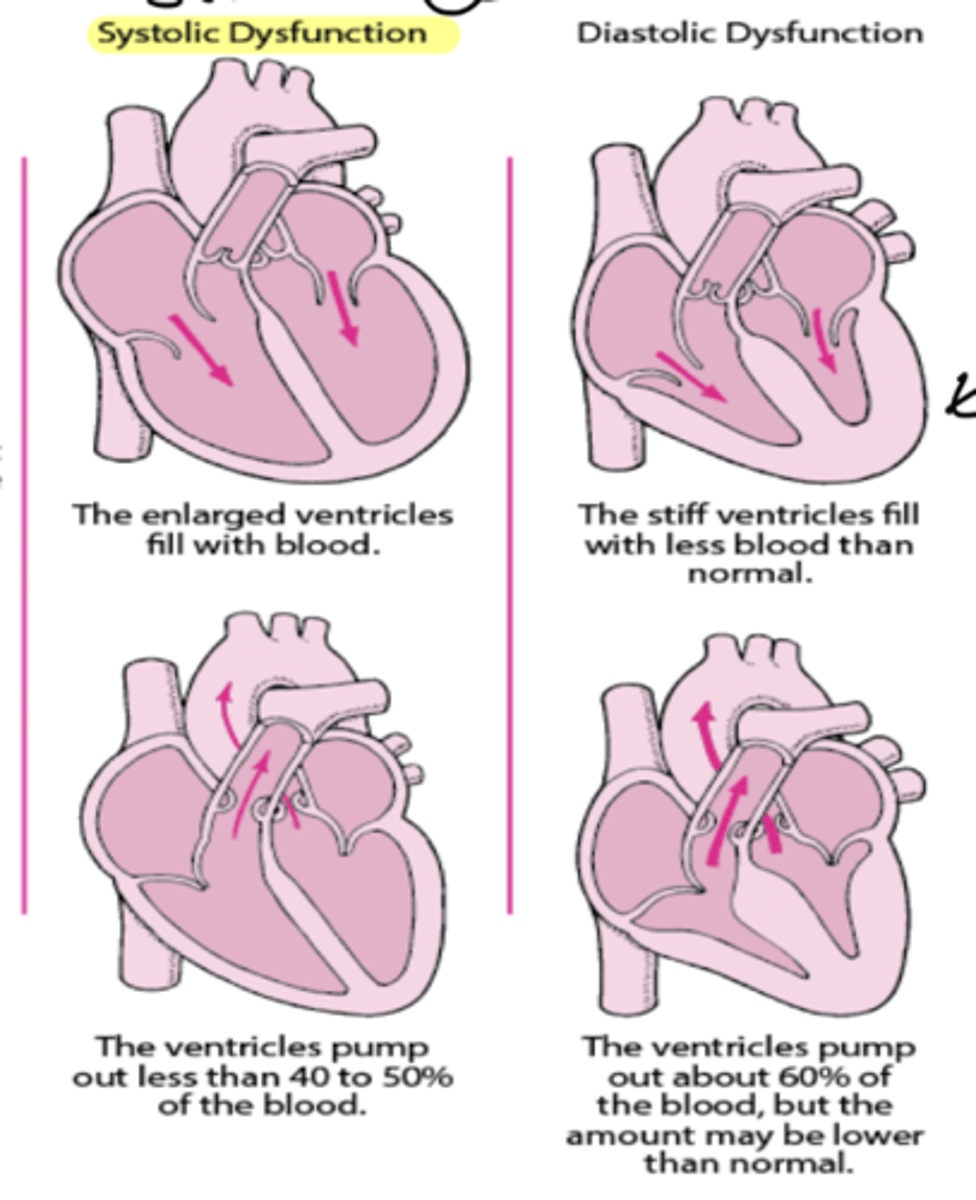
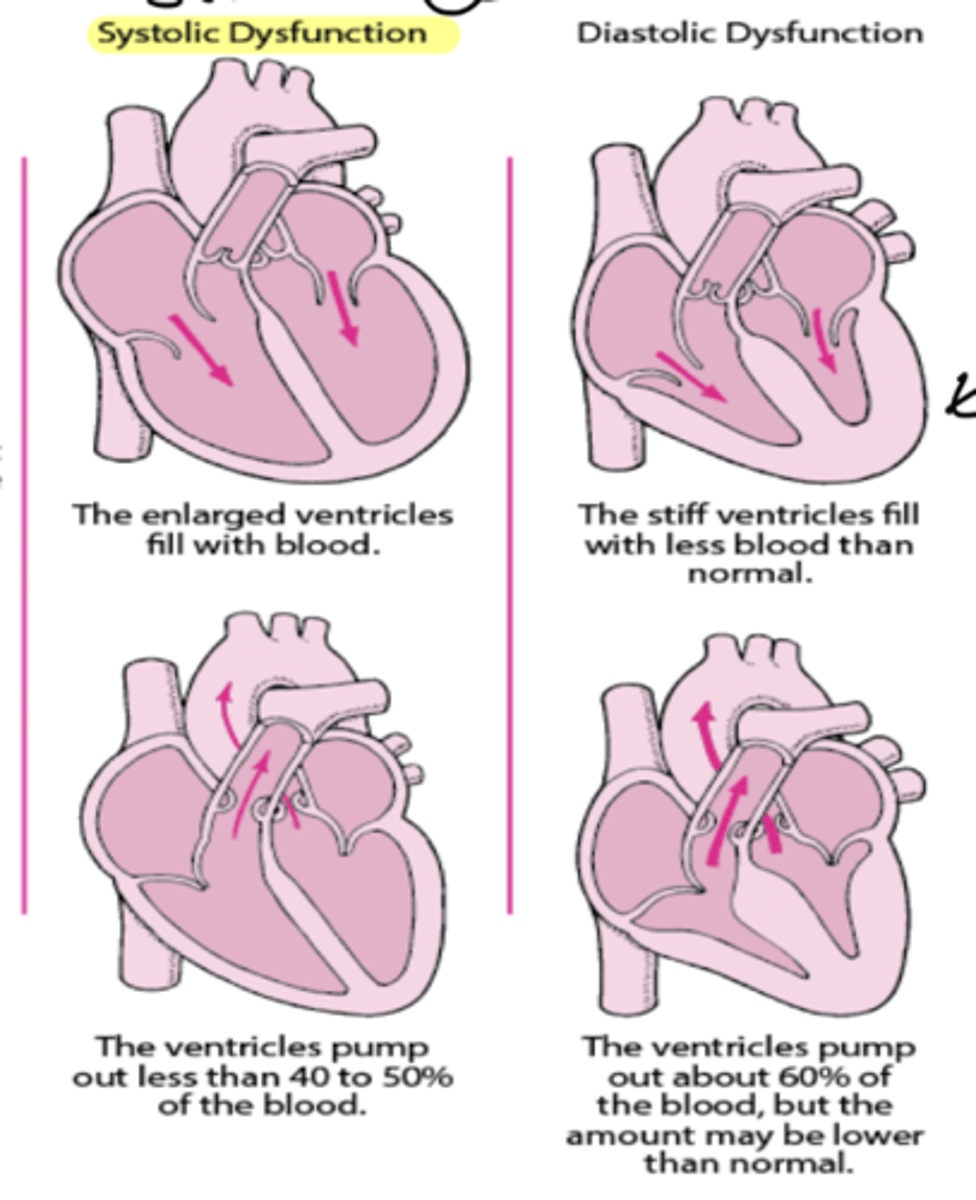
what are the consequences of systolic and diastolic dysfunction?
systolic - stretched cells - causing a weaker contraction so ventricles pump out less than 40-50% of blood
diastolic - no place to occupy blood due to hypertrophy - ventricles pump out 60% of blood still but amount may be lower
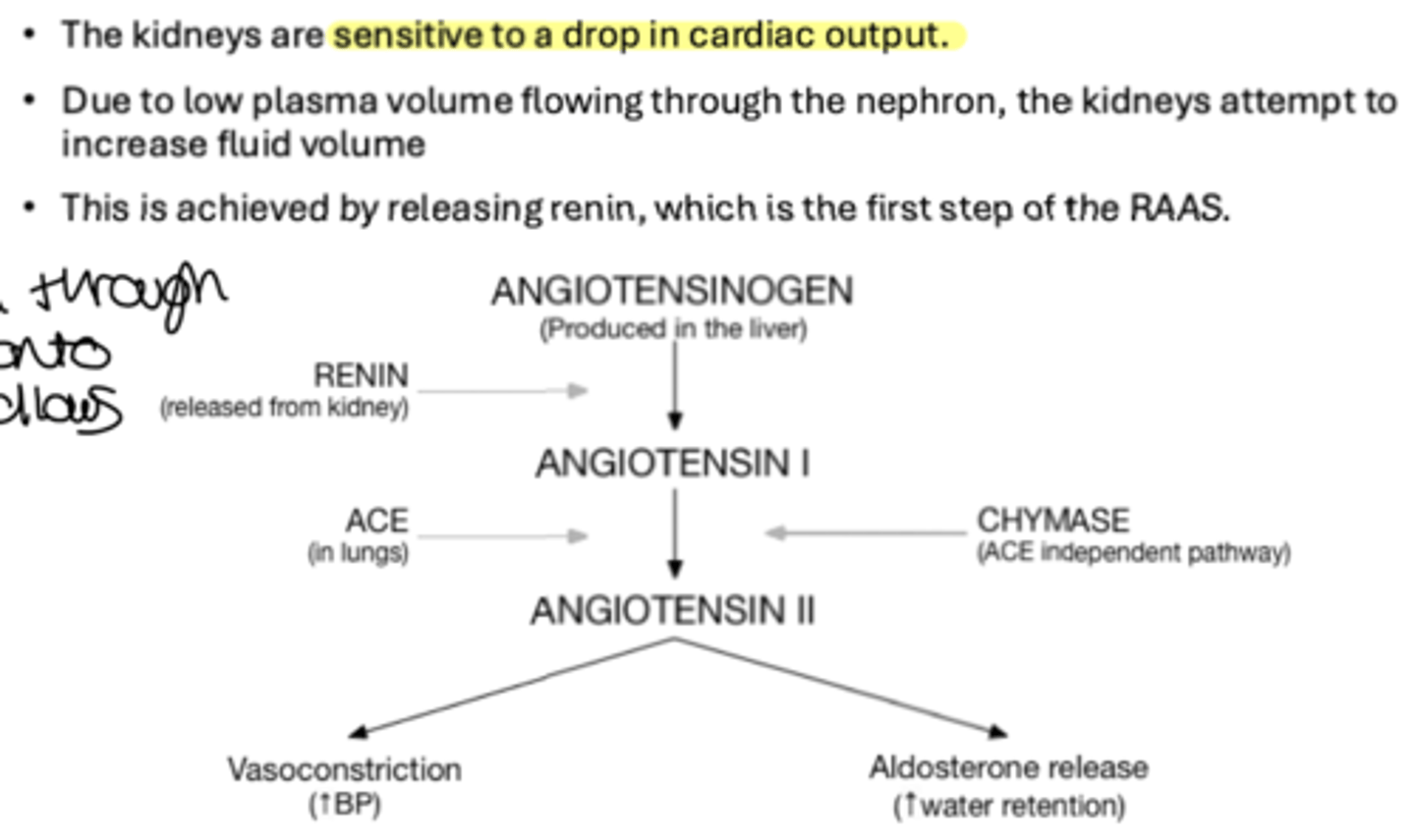
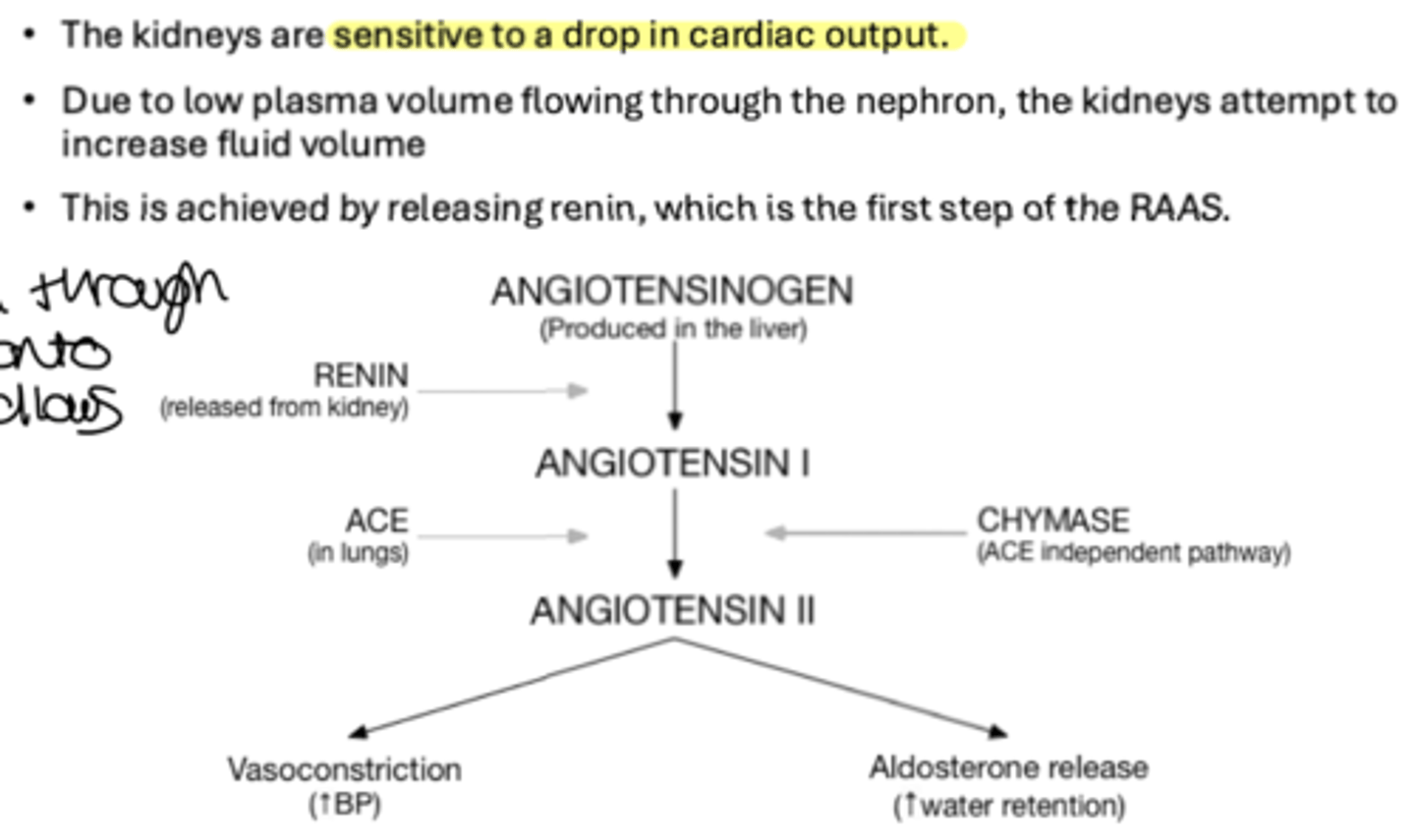
what is the consequence of HF on the kidneys?
- sensitive to a drop in CO
- a drop in CO increases fluid volume
- increasing reabsorption through the nephron and hold onto salt and water follows and stimulates RAAS
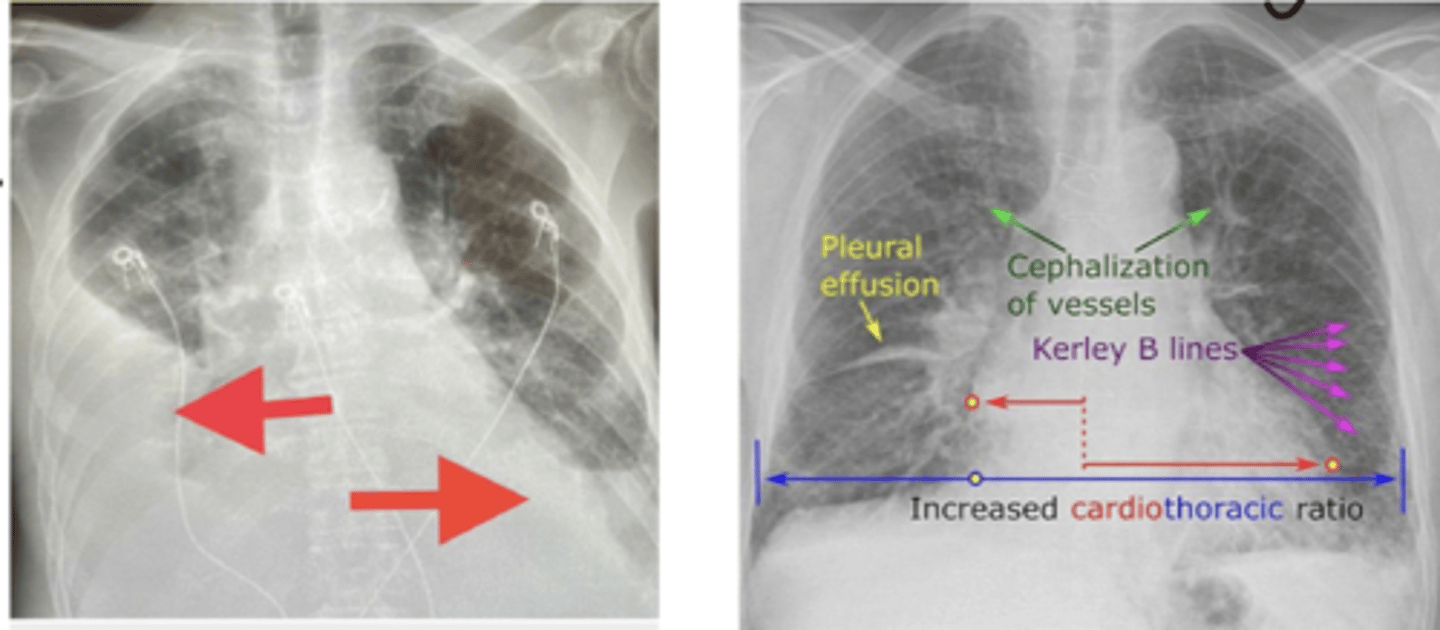
what is the consequence of HF on the lungs?
- release of aldosterone through RAAS stimulations leads to fluid retention - progressing to fluid overload
- in left sided backlog of blood seeps out entering lungs due to fluid retention (pulmonary oedema)
- in right sided fluid leaks which increases blood volume and accumulates in peripheral circulation - causing raised JVP and peripheral oedema
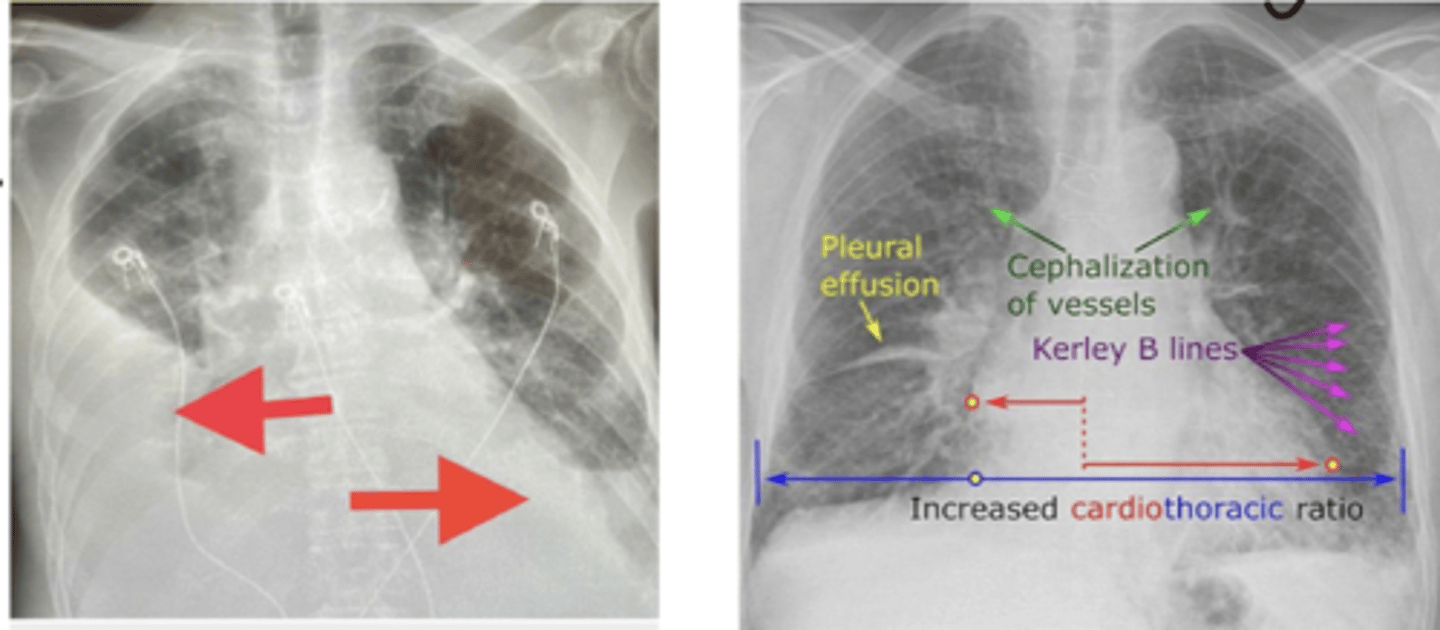
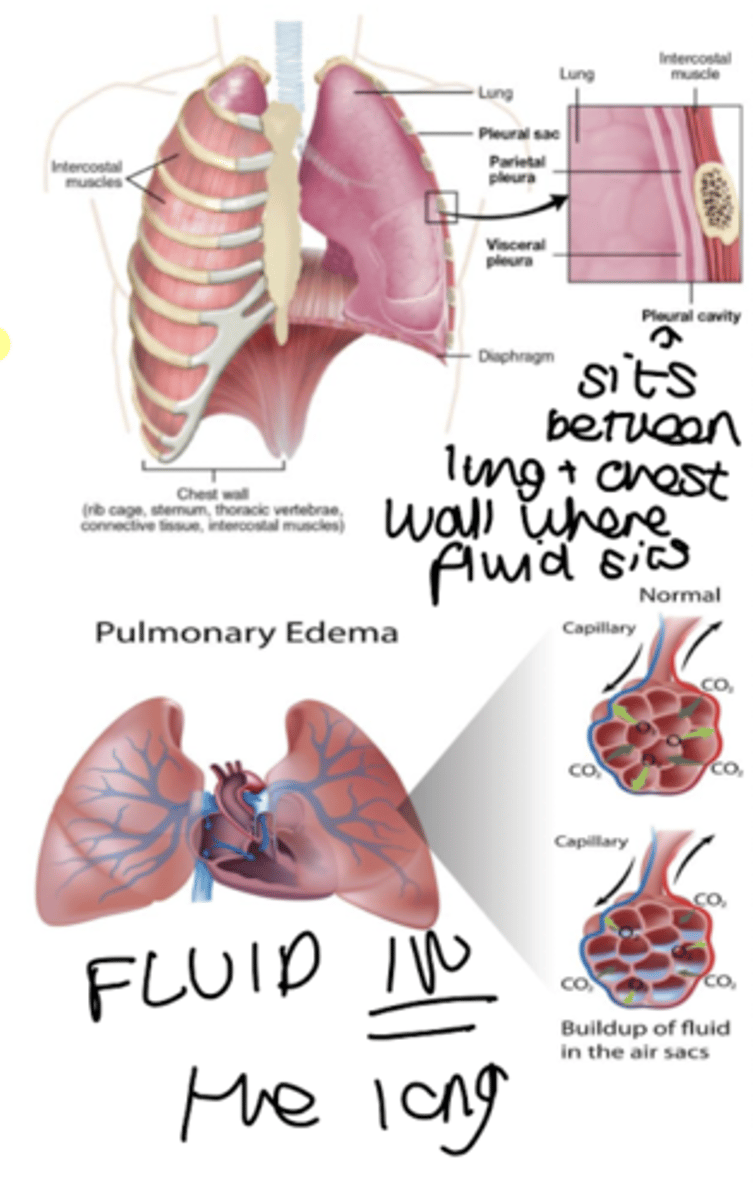
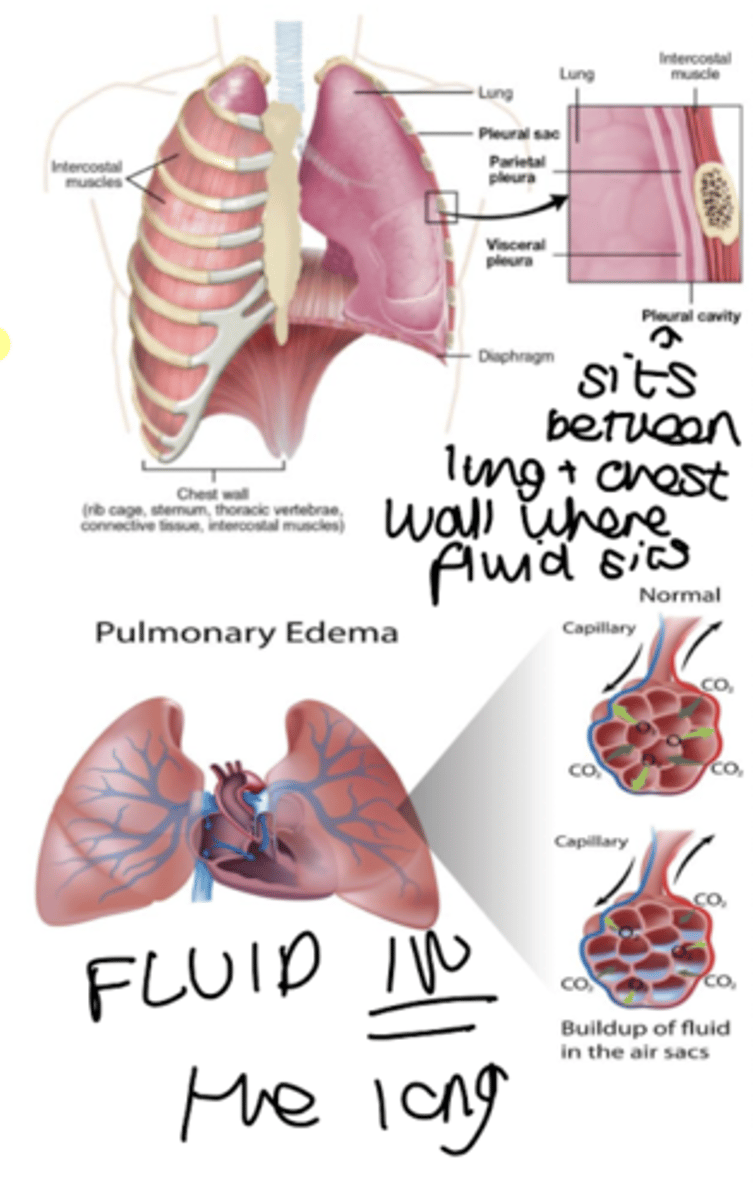
what is the difference between pleural effusion and pulmonary edema?
pleural effusion - fluid on the lung
pulmonary oedema - fluid in the lung
how do we know if a patient has peripheral oedema?
when pressed on with finger, pit will stay and this indicates fluid
how is HFrEF, HFmrEF and HFpEF catagorised numerically by ejection fraction?
HFrEF - less than 40%
HFrEF - 41-49%
HFpEF - over 50% (cardiac problem cannot be seen)
what does failure of myocardium to contract normally and dilation in left ventricle result in?
HFrEF
what does stiff, hypertrophy myocardium failing to relax result in?
HFpEF
occupational space for blood has become smaller
what is the typical specific presentation of HF?
- fatigue
- SOB - worse on exertion
- peripheral oedema
- reduced exercise tolerance
- orthopnoea - SOB when lying down but relieved when sitting up as fluid is pulled back down to gravity
- paroxysmal nocturnal dyspnoea - sudden shortness of breath
what is the NYHA classification?
classification for HF
Class 1 - no limitations - asymptomatic LV dysfunction
Class 2 - slight limitation of physical activity
Class 3 - marked limitation of physical activity
Class 4 - unable to carry on any physical activity - present at rest
what are the pathway of investigations for suspected HF?
- take history
- perform ECG, bloods, CXR, urinalysis, spirometry to rule out ACS/infections
- measure NT-proBNP
- if less than 400ng/l, no confirmed HF
- if 400-2000ng/l refer for echocardiography within 6 weeks
- if over 2000ng refer for echocardiography within 2 weeks
what is NT-proBNP?
B type natriuretic peptide which is released from ventricles in periods of stress
it CAN appear in pregnancy and cancers - so it is HF sensitive but not specific
who contraindicates echocardiography?
tachycardic patients
what are the 5 pillars to HFrEF treatment?
- ACEi/ARB
- B blocker
- MRA
- NI
- SGLT2i
what is the first pillar of HFrEF treatment?
ACEi - use ARB if intolerant
decreases mortality
improves symptoms, exercise tolerance and QoL
what is the MoA of ACEi in treatment of HF?
- inhibit ACE
- reduces conversion of AT1 to AT2
- reducing vasoconstriction and stimulation of aldosterone secretion
- decreasing aldosterone concentration
- increasing Na+ and H2O excretion
- therefore decreases preload - beneficial to HF
what are the baseline tests, indication and dosage titration and patient info for ACEis?
- bloods and obs - checking kidneys due to nephrotoxic effects of ACEis that can cause AKI also check K levels
- start low go slow, monitor within 1-2 weeks as it takes some weeks for effect, but often double dose at 2-4 weekly intervals until getting to MAX TOLERATED DOSE
counsel pt on:
- hypotension
- monitor for hyperkalemia
- avoid any OTC NSAIDs
- angioedema - go to hospital
- sick day rule
what is the 'sick day rule'?
during vomiting and diarrhoea - stop taking med and then start taking again when better
what is THAD-BEANS?
drugs that cause hyperkalemia:
- Trimethoprim - Abx for UITs
- Heparins - LMW heps
- ACEis and ARBs
- Digoxin
- Beta blockers
- Epelerone - MCRA for HF
- Amiloride - K sparing diuretic
- NSAIDs
- Spirinolactone
what is pillar 2 (2nd line) of treatment for HFrEF?
Beta blockers
- reduction in morbidity, huge reduction in hospitilisation
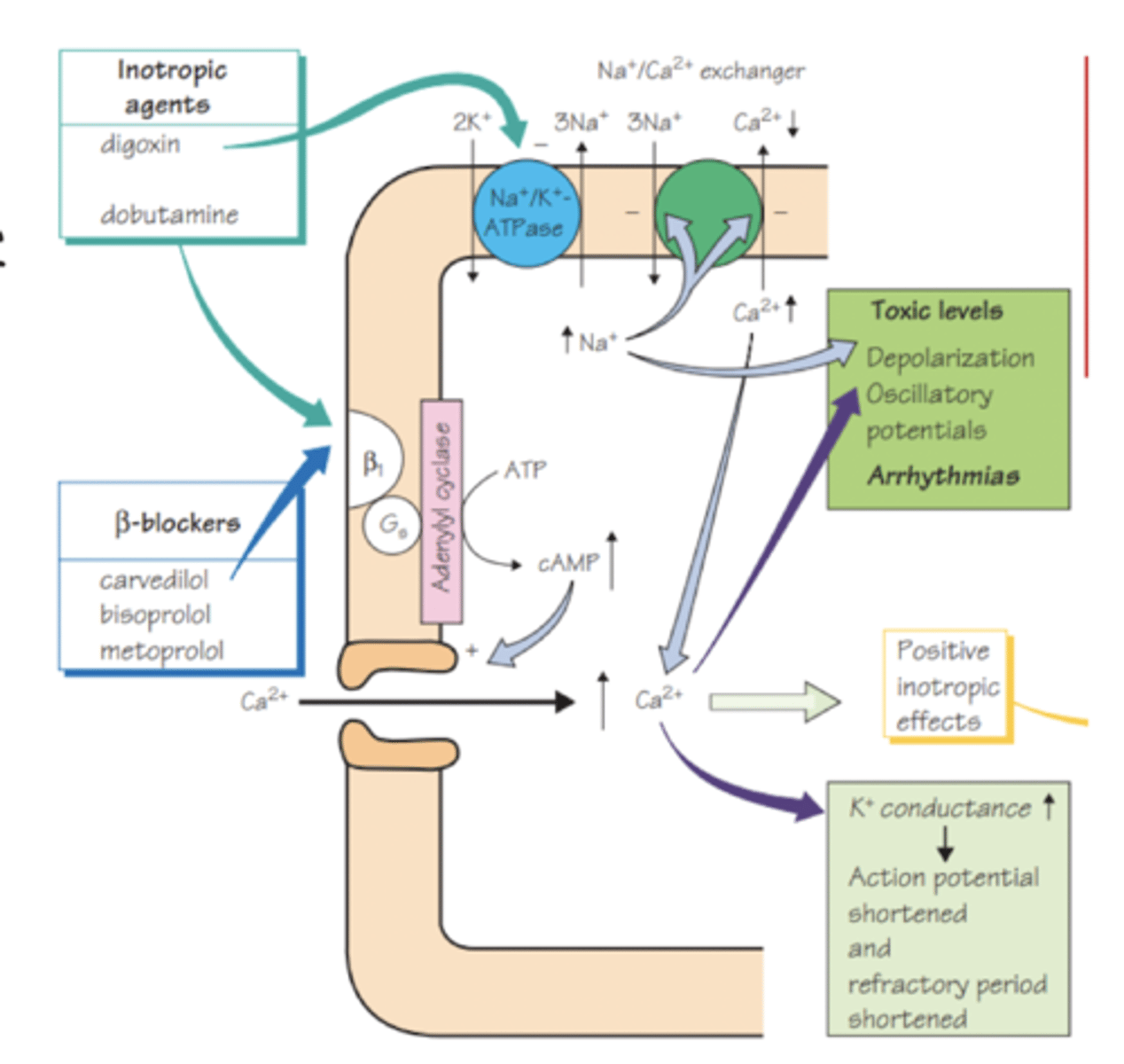
what is the mechanism of beta blockers in HFrEF?
- block B1 - adrenergic receptor (1 heart = B1, 2 lungs = B2)
- reduce force of cardiac contraction and speed of conduction
- block the damaging effects of overactive sympathetic activity
- negative chronotrope (decrease HR) - negative inotrope
what are the clinical considerations of using BB in treatment of HFrEF?
- BB should be offered to all ULVALEMIC Pts with LVSD (LVEF less than 40%)
- do not start BBs if signs of fluid overload as can cause fluid retention on initiation
- use cardiac selective
- may take a while to notice benefit
- expect temporary SOB and fatigue
- do not stop suddenly due to rebound tachycardia
what does uvalemic mean?
normal body fluid volume
what are the monitoring and dose considerations for using BBs in treatment of HFrEF?
- HR, BP, fluids and ECG (for bradycardia)
- start at lowest dose and titrate to tolerated
- increase every 2-4 weeks to achieve max
which beta blockers cause less bradycardia and less coldness of extremities? and why?
ISA - intrinsic sympathoimetic activity
ice PACO:
Pindolol
Acebutol
Celoprolol
Oxprenolol
which beta blockers cause less nightmares and sleep disturbances? and why?
water soluble, less likely to cross BBB
reduce dose in renally impared as renal cleared
water CANS:
Celiprolol
Atenolol
Nadolol
Sotalol
which beta blockers are cardioselective? why are these necessary?
cardio selective = less bronchospasm
Be A Man
Bisoprolol
Atenolol
Metoprolol
Acebutol
Nebevolol
which beta blockers are OD?
BACoN
Bisoprolol
Atenolol
Celiprolol
Nadolol
intrinsically longer duration of action
what is pillar 3 of treatment of HFrEF?
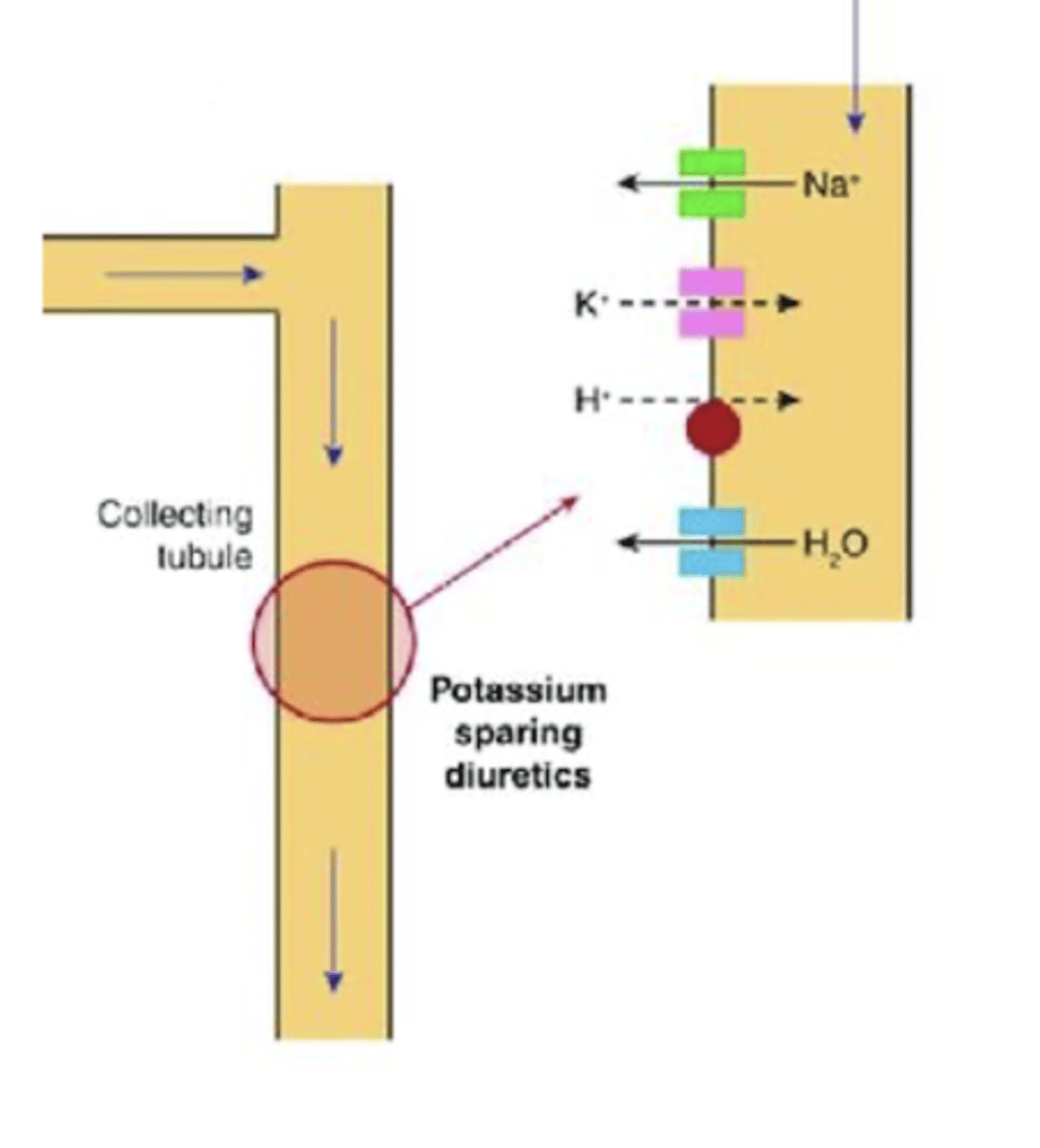
Mineralocorticoid receptor antagonists (MRAs) - type of K sparing diuretic
also known as aldosterone antagonists
should be considered in all LVSD patients if still symptomatic (NYHA 2-4) despite max tolerated ACEi, BB and diuretics
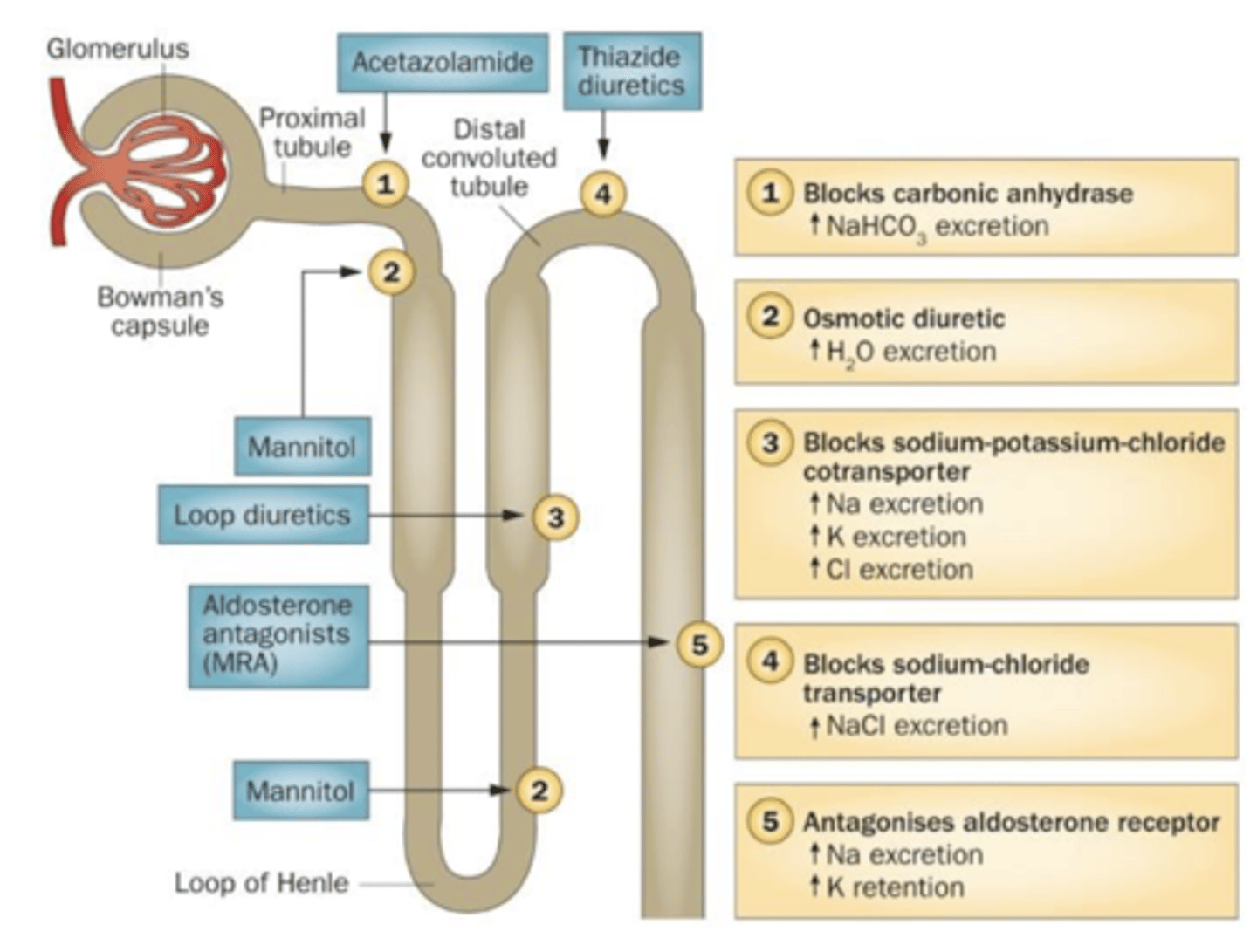
what is the mechanism of mineralocorticoid receptor antagonists?
- aldosterone is a mineralcorticoid, produced in adrenal cortex
- acts on mineralcorticoid receptors in distal tubules of kidney
- increase activity of luminal epithelial sodiun channels
- increases reabsorption of sodium and water
- elevates BP, with a corresponding increase in K excretion
- MRA inhibit the effect of aldosterone by competitive inhibition at mineralcorticoid receptors
- increases sodium and water excretion and K retention
- stops aldosterone in the RAAS system
what are the baseline tests required for use of MRAs?
U&Es, eGFR, LFT
nepherotoxic
which MRAs should be used in treatment of HFrEF?
Spironolactone in females
Eplerenone in males - due to spironolactone causing gynaecomastia - development of breast tissues
what are the clinical considerations for use of MRAs in HFrEF?
- start low and not max tolerated dose
- if symptoms remain after 4 weeks increase depending on bloods
- avoid high K foods
- eplerenone is a strong CYP3A4 inhibitor
- take spironolactone with food
- hypovchemia is common side effects - dizziness
what is Pillar 4 for the treatment of HFrEF?
SGLT2 inhibitors
Dapagliflozin or Empagliflozin lisenced as add on to: ACEi/ARNI/BB/MRA
- only initiate on advice of consultant cardiologist
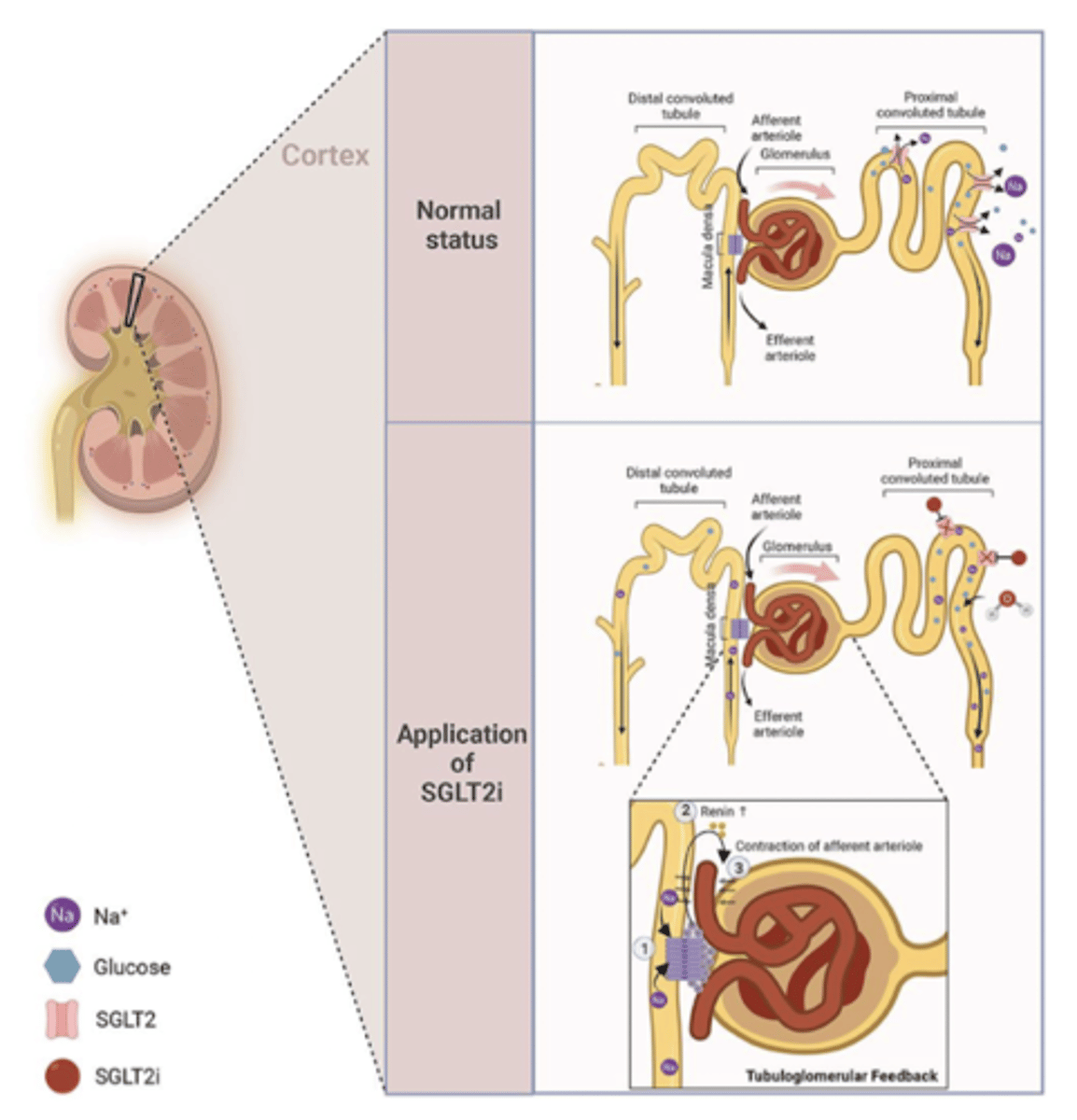
what is the MoA for SGLT2i in treatment of HFrEF?
- selectively and reversibly inhibit the SGLT2 in PCT of nephron
- SGLT2 mediates active transport of glucose and Na from filtrate into blood
- SGLT2 inhibition impairs glucose reabsorption in the nephron, increasing renal excretion of glucose (glycosuria)
- increased renal Na/H2O excretion reduces extracellular water vol, blood pressure and cardiac preload
- overall triggers tubuloglomerular feedback mechanisms that reduce intra-glomerular pressure
what are the baseline tests and dose associated with use of SGLT2s for HFrEF?
BP and U&Es - nephrotoxic
at initiation one standard dose - no titration phase - no dose reduction, consider ending treatment if eGFR is less than 30 - risk benefit treatment for Pt with HF and DM if kidney function less than 30
what are the counselling pts associated with use of SGLT2s for HFrEF?
- sick day rules
- increased risk of UTI, polyuria, fungal genital infections, lower limb amputation
- volume depletion effects
- euglycemic DKA - diabetic ketoacidosis, masked effect - it looks normal
- fournier's gangrene - cell death causing lower limb amputation
- patients will test positive for glucose in urine
what is DKA?
diabetic ketoacidosis - body has no sugar that can process in its cells - breaks down fats and release ketones and you go acidic
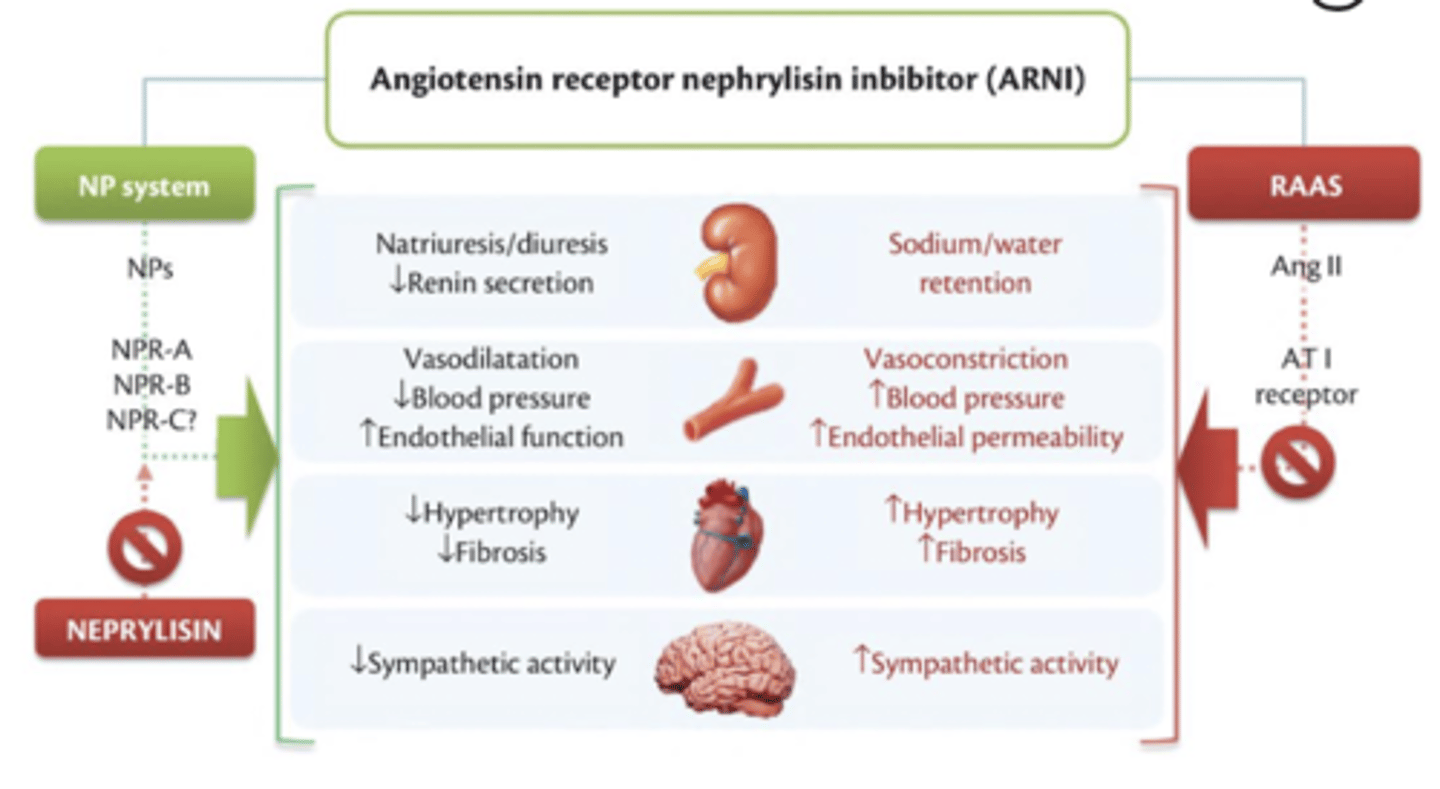
what is the 5th pillar of treatment of HFrEF?
Neprilysin inhibitors
NI + ARB = Entresto
for NYHA classes 2-4
what is Entresto?
Neprilysin inhibitor (sacubitril) and ARB (valsartan)
what is the MoA of Entresto?
- inhibit neprilysin
- increase levels peptides degraded by neprilysin - natriuetic peptides
- NPs exert their effects by activating membrane-bound receptors - resulting in increased concs of 2nd messengers
- results in vasodilation, natriuresis and diuresis - increased GFR and renal blood flow
- simultaneous inhibition of the effects of AT2 by valsartan
- inhibits renin and aldosterone release, reduction of sympathetic activity and anti-hypertrophic and anti-fibrotic effects
what are the counselling points for using Entresto in HFrEF?
- must stop ACEi or current ARB
- hypotension and dizziness common SE
- monitor for increased K
what are the baseline tests and dosage titration for Entresto in HFrEF?
- bloods U&Es, K, Na, eGFR and BP
- start at lowest dose and titrate up
- current ACEi/ARB discontinued at least 36h before initiation
- prescribed using generic na,e to avoid co administration with ACEi or ARB
- BD dose
- double dose every 2-4 weeks to reach max
how are diuretics used in symptom control of HF?
- used for both HFrEF and HFpEF
- loop diuretics preferred over thiazides - more intense and shorter in duration of diuresis compared with thiazide
- can be used in worsening renal function - effective even if GFR is less than 30ml/min
- IV route
- start low and titrate to response
- treatment resistant peripheral oedema needs thiazide like diuretics used in combination with a loop diuretic - for significant diuresis effect - a ONCE ONLY dose
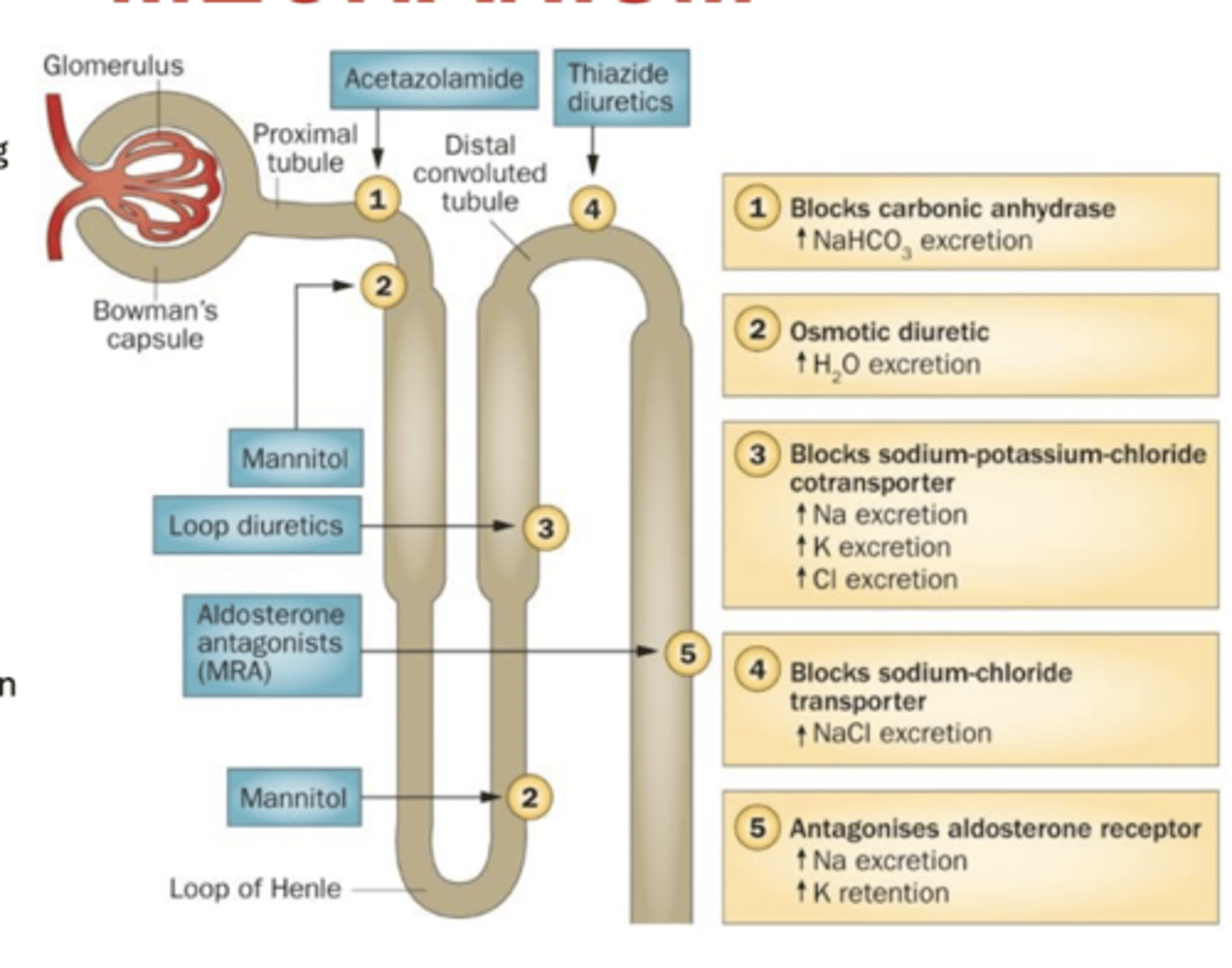
what is the MoA of loop diuretics?
- Na+/K+/2Cl- co transporter - in the thick ascending limb normally reabsorbs approx 25% of the Na+
- responsible for transporting Na+, K+ and Cl- ions from tubular lumen into epithelial cell
- water follows by osmosis
- inhibition of transporter increases DT Na+ conc
- therefore, less H2O reabsorption from CD
- reduces preload and improves contractile function of 'overstretched' heart muscle
- loop diuretics also induce renal synthesis of prostaglandins - which increase renal blood flow
what are the clinical considerations for use of loop diuretics?
- symptomatic hypotension with dizziness, fainting or loss of consciousness
- monitoring - GOUT due to UA build up due to excretion of increased fluid
- increased electrolyte excretion
- weight loss caused by increased urine excretion should not exceed 1kg/day
- important to ensure infusion rates do not exceed 4mg of furosemide per min as tinnitus and deafness may occur
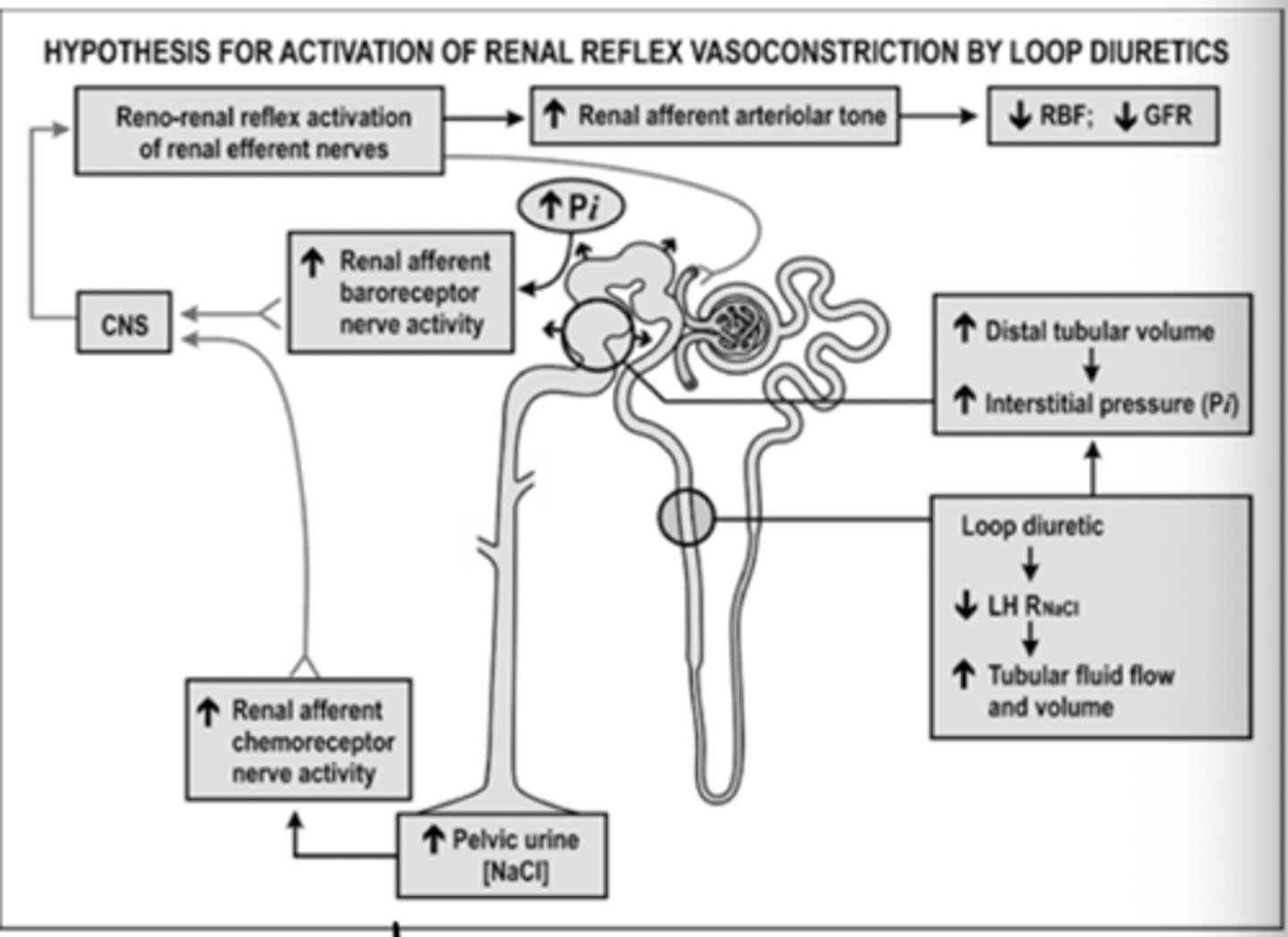
what is diuretics resistance?
- loop diuretics reduce Na+/Cl- reabsorption in the LoH
- this activates renal afferent chemoreceptor nerves
- at the same time renal afferent baroreceptor nerves are activated due to pressure and flow changes
- signals lead to increase in afferent nerve discharge, which stimulates CNS
- CNS responds by increasing renal efferent nerve activity
- loop is less intense on the kidneys therefore first line
what is the MoA for thiazide (like) diuretics?
Indapamide, Metolazone, (Bendroflumethiazide)
- inhibits Na+/Cl- co transporter in DCT
- stops Na+ reabsorption and therefore H2O
- resulting diuresis causes initial fall in the ECF volume
- because this mechanism normally only reabsorbs about 5% of filtered Na, thiazide diuretics are less effective than loop
what are the clinical considerations in using Thiazide diuretics?
- Na+ reabsorption from nephron can cause hyponatremia
- hypokalemia
- increase plasma conc of glucose
- may cause impotence in men
what are the additional therapies for treatment of HFrEF?
only reduce symptoms not mortality
Ivabradine, Digoxin, Hydralazine-Isosorbide Dinitrate, thiazide/thiazide like diuretics
what non-pharmacological management is offered for HFrEF?
Cardiac Resyncronization therapy (CRT) - device that sends electrical impulses to L and RVs of heart to help them beat together in synchronized pattern. Unsure if benefits in AF
Inplantable Cardioverter Defibrillator (ICD) - after 30 months if still very low EF, reduces motality in survivors of cardiac arrest and in patients with sustained symptomatic V arrythmias
Ablation - arrhythmia driven HF could benefit from heat to create fibrotic tissue preventing faulty signals and restores sinus rhythm
Fluid restriction and weight monitoring - avoid Xs salt, hyponatraemia pts should be careful about fluid intake - to less than 2l per day
what are the functions of cholesterol?
- precursor of steroid hormones: sex, tissue growth, adrenocortical
- bile acids - cholic acid - added to emulsify water insoluble foods
- biological membranes
where do LDLs carry cholesterol?
to cells
where do HDLs carry cholesterol?
from cells to liver
what lipid levels is mortality associated with?
high levels of LDLs or low levels of HDLs
what is the 3 main phases to the pathway of biosynthesis of cholesterol?
- formation of mevalonic acid
- conversion of mevalonate into farnesyl pyrophosphate
- condensation of 2 farnesyl pyrophosphate units to yield squalene
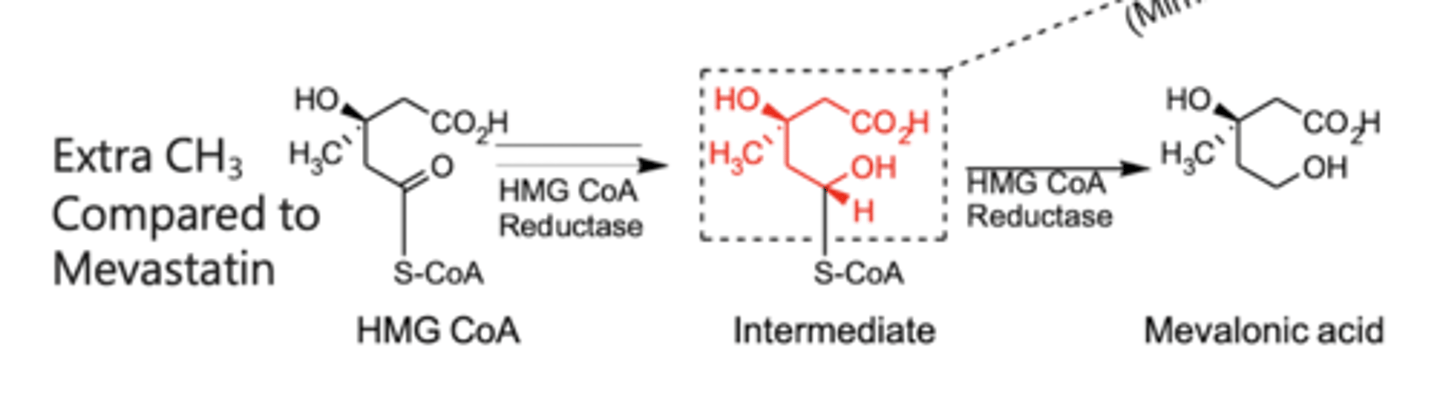
what is the phase 1 process of cholesterol biosynthesis?
- 2 thioesters
- nucleophilic substitution with thiolase occurs
- HMG CoA synthesis added to make an alcohol
- HMG Coa reductase leads to MEVALONIC ACID
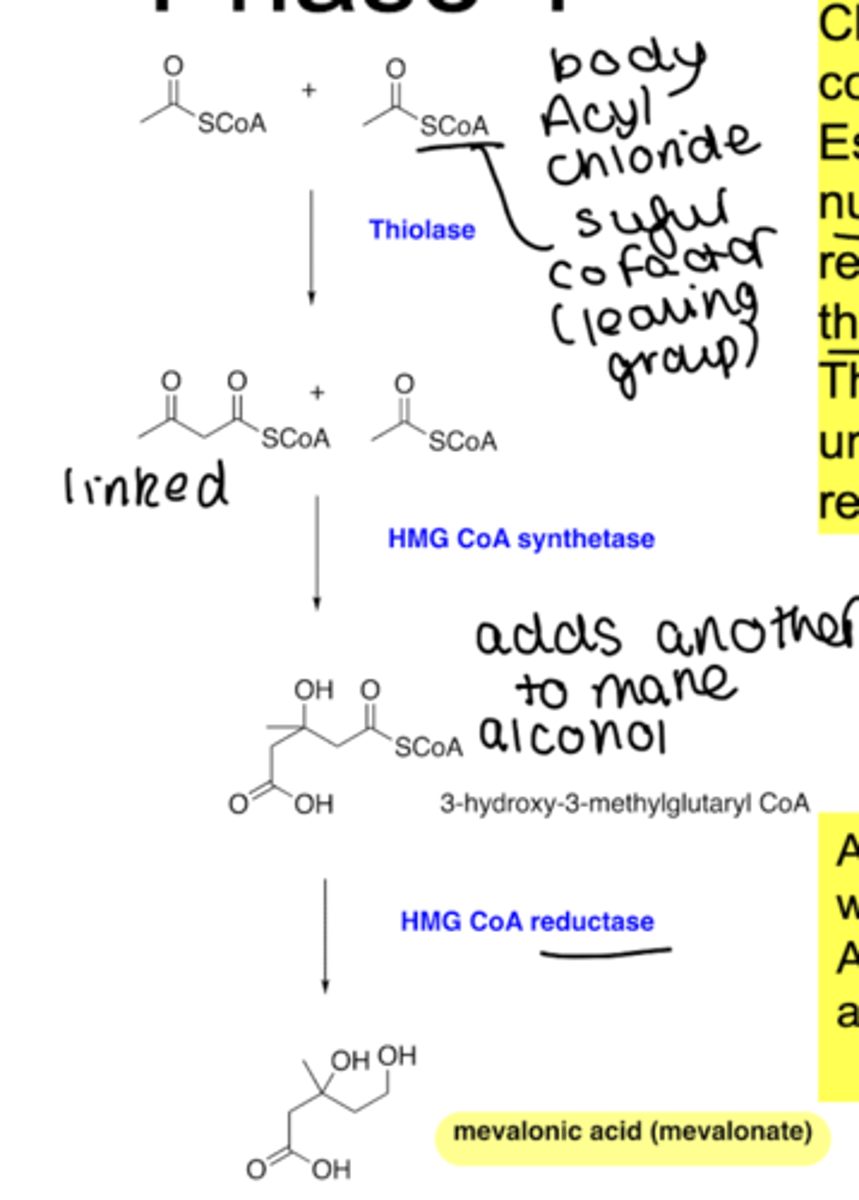
what parameters regulate cholesterol production via HMD-CoA?
- kinase - turns off and on on the basis of intracellular cholesterol level
- transcription and translation which cholesterol feeds back on
- enzyme degradation controlled by concentration of cholesterol
how do statins work (1)?
work by blocking HMG-CoA reductase
final step in phase 1 of sequence in reduction of 3-hydroxy-3-methylglutaryl-coenzyme A to mevalonic acid
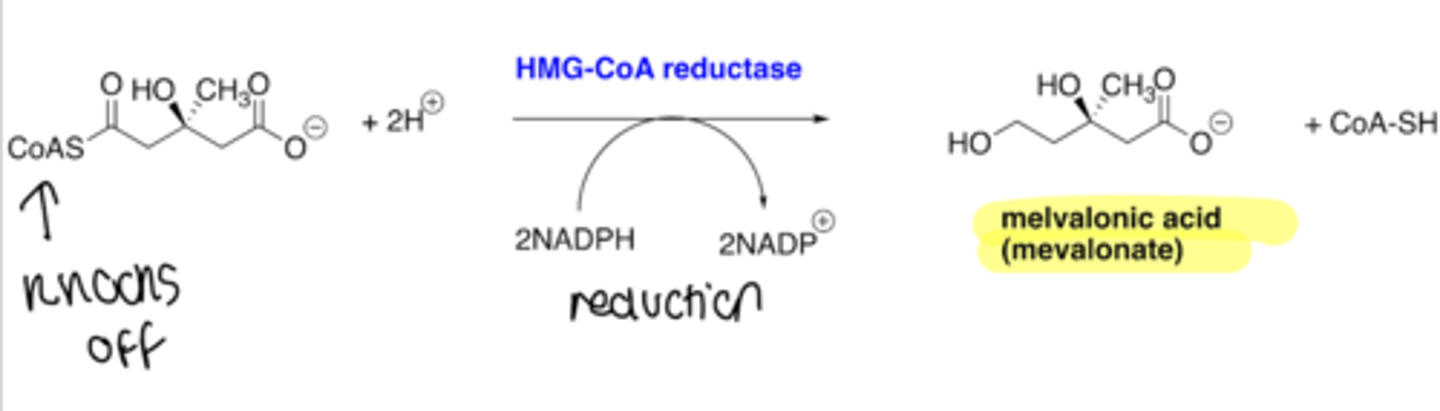
what is the mechanism of action of statins?
statin is a competitive inhibitor (with x10,000 higher affinity for enzyme than substrate) in the reduction pathway from HMG CoA to mevalonic acid
what structural modifications happened to new generation of statins?
modifications that have a longer interaction with the enzyme in the active site
they have a larger hydrophobic moiety with no asymmetric centres
what is the structure on type 1 and 2 statins that remained the same?
the 'polar head'
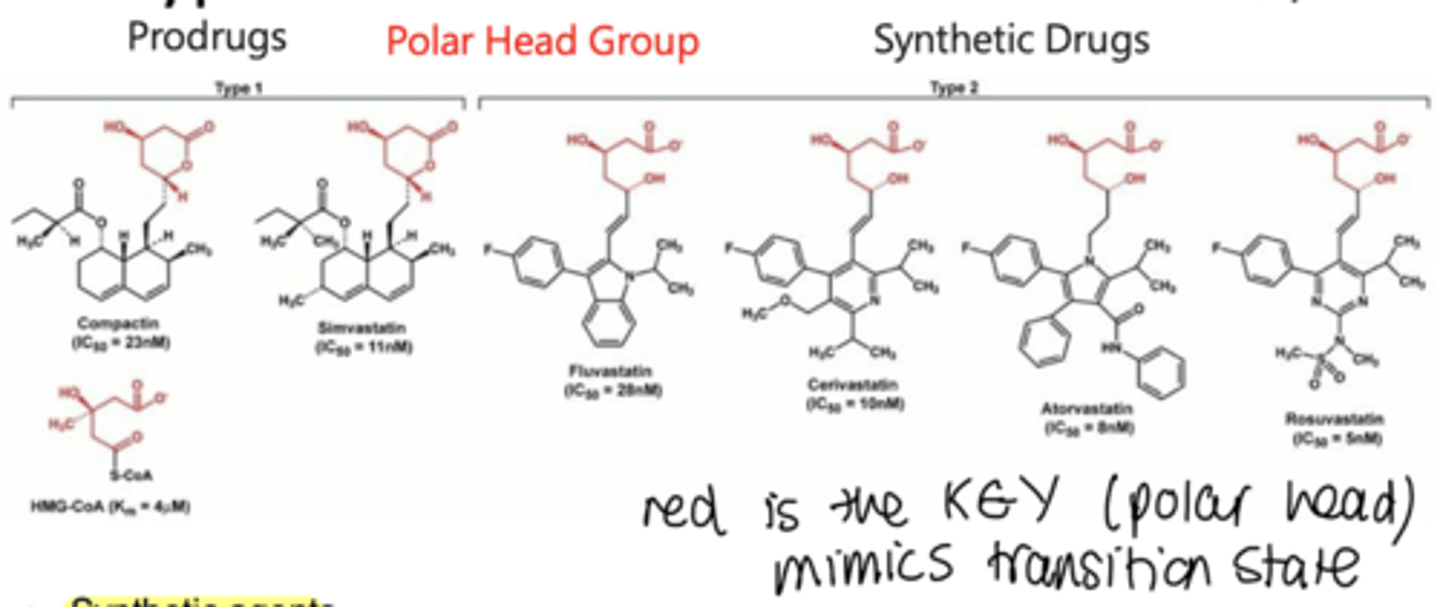
what was got rid of in type 1 statins to be type 2?
the decalin ring
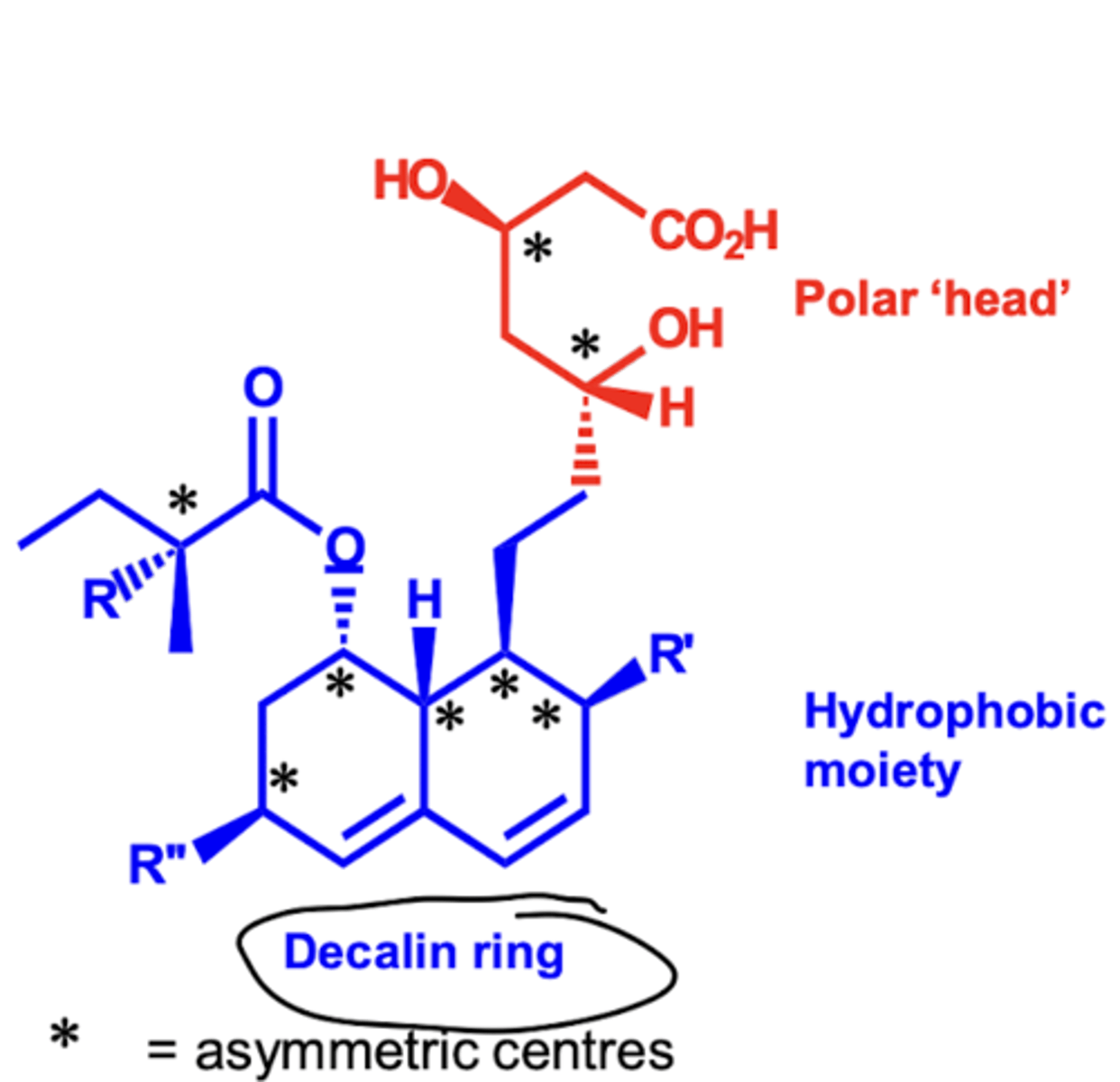
why do type 2 statins have lower side effects?
- lower hydrophobic character
- therefore do not cross cell membranes easily
- therefore better side effect profiles
why is a common side effect of statins myalgia?
(muscle pain)
due to inhibition of HMGR in other cells such as muscle cells
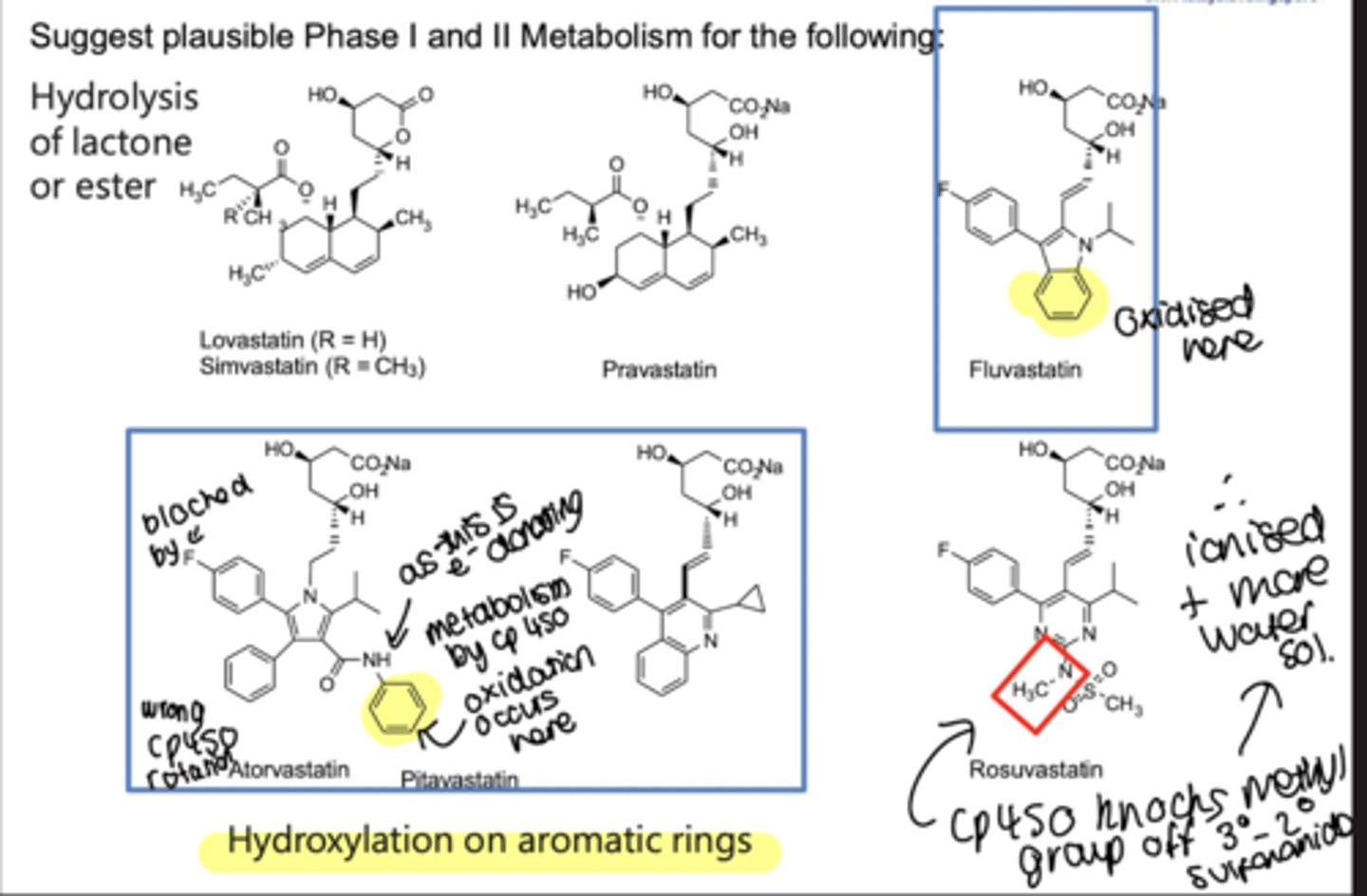
how are statins metabolised?
hydroxylation occurs on aromatic rings by cp450
what is Heart Failure (HF)?
where the heart is unable to pump sufficiently to maintain blood flow to meet the body's needs.
what is End-diastolic volume (EDV)?
Volume of blood in ventricles at the end of diastole. Normally = 110-130 mL.
what is End-systolic volume (ESV)?
Volume of blood left in ventricles at the end of systole. Normally = 40-60 mL.
what is Stroke volume (SV)?
Amount of blood ejected from ventricles during systole/beat. Normally = 70-80 mL/beat.
what is Ejection fraction (EF)?
Fraction of end-diastolic volume ejected during a heart beat. SV/EDV = EF. Normally around 50-70%.
what is Cardiac Output (CO)?
Volume of blood ejected by each ventricle in each minute. Normally = around 5 litres in an adult at rest. SV X HR = CO.
What is preload?
The amount of blood presented to the ventricles.
what is Afterload?
The resistance against which the ventricles contract. (BP)
what is HFrEF?
Heart Failure with Reduced Ejection Fraction, characterized by a reduced EF
- dilated cardiomyopathy - wall of V becomes thin as heart enlarges - decreases pump efficiency, reducing SV
what is HFpEF?
Heart Failure with Preserved Ejection Fraction, characterized by a preserved EF - thickening and stretching of arteries
- hypertrophic cardiomyopathy, where V walls thicken and stiffen - V filling capacity drops resulting in drop in SV
what is aim in treatment of HFrEF?
no longer aims to decrease mortality - now it is to prevent hospitalisation
what are the risk factors of developing HF?
- LV hypertrophy - thickening prevents enough space for blood to actually fill it - so not enough leaves it
- chronic HTN - causes heart stretch, decreasing contractility
- any MI - ischaemic tissue cannot contract
- thyroid disease - related to arrhythmias and DM
- prolonged arrythmias
what is the pathophysiology of HF?
- reduced CO, leading to blood pressure drop
- RAAS and SNS stimulated: increasing contractility, tachycardia and vasocontriction (all bad corrective mechanisms)
- exhausts failing heart
what are the consequences of systolic and diastolic dysfunction?
systolic - stretched cells - causing a weaker contraction so ventricles pump out less than 40-50% of blood
diastolic - no place to occupy blood due to hypertrophy - ventricles pump out 60% of blood still but amount may be lower
what is the consequence of HF on the kidneys?
- sensitive to a drop in CO
- a drop in CO increases fluid volume
- increasing reabsorption through the nephron and hold onto salt and water follows and stimulates RAAS
what is the consequence of HF on the lungs?
- release of aldosterone through RAAS stimulations leads to fluid retention - progressing to fluid overload
- in left sided backlog of blood seeps out entering lungs due to fluid retention (pulmonary oedema)
- in right sided fluid leaks which increases blood volume and accumulates in peripheral circulation - causing raised JVP and peripheral oedema
what is the difference between pleural effusion and pulmonary edema?
pleural effusion - fluid on the lung
pulmonary oedema - fluid in the lung
how do we know if a patient has peripheral oedema?
when pressed on with finger, pit will stay and this indicates fluid
how is HFrEF, HFmrEF and HFpEF catagorised numerically by ejection fraction?
HFrEF - less than 40%
HFrEF - 41-49%
HFpEF - over 50% (cardiac problem cannot be seen)
what does failure of myocardium to contract normally and dilation in left ventricle result in?
HFrEF
what does stiff, hypertrophy myocardium failing to relax result in?
HFpEF
occupational space for blood has become smaller