biliary tree and gallbladder
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
largest gland in body
liver
liver is divided into large right lobe and smaller left lobe at
falciform ligament
two minor lobes are on medial side of right lobe
caudate-posterior
quadrate-inferior
hilum called __ is situated transversely between two minor lobes
porta hepatis
convey blood to liver
portal vein and hepatic artery
both portal vein and hepatic artery enter __ and branch out through __
porta hepatis
liver substance
liver receives blood from
portal system
the hepatic veins convey blood from
liver sinusoids to IVC
numerous functions of liver and biliary system including formation of
bile
amount of bile secreted each day
1-3 pints or ½ to 1 liter
bile is an
excretion and secretion
aid in emulsification and assimilation of fats
secretion
channel of elimination for waste products of red blood cell destruction
excretion
bile collected from __
the two main hepatic ducts emerge at the __ and join to form the __ which unites with the cystic duct to form the __
porta hepatis
common hepatic duct
common bile duct
The common bile duct joins the pancreatic duct to enter together into an enlarged chamber called the
hepatopancreatic ampulla
another name for hepatopancreatic ampulla
ampulla of vater
ampulla opens into descending portion of the
duodenum
the distal end is controlled by the __ as it enters the duodenum
choledochal sphincter
The hepatopancreatic ampulla is controlled by a circular muscle called the
sphincter of the hepatopancreatic ampulla
sphincter of Oddi.
During periods between digestion, the sphincter remains closed/contracted, so most of the bile is routed into the
gallbladder for concentration and storage
During digestion, the sphincter relaxes to
permit the bile to flow into the duodenum.
The ampulla of Vater opens on an elevation on the duodenal mucosa called the
major duodenal papilla
a thin walled, pear shaped ,musculomembranous sac
gallbladder
capacity of gallbladder
2 ounces
gallbladder concentrates bile by
absorption of water content
gallbladder stores bile
during interdigestive periods
gallbladder evacuates bile
during digestion
The muscular contraction of the gallbladder is activated by a hormone called
cholecystokinin
cholecystokinin is secreted by __
duodenal mucosa
cholecystokinin releases into blood when
fatty or acid chyme passes into the intestine
gallbladder has a __ continuous with cystic duct
narrow neck
body (main)
fundus (broad lower portion)
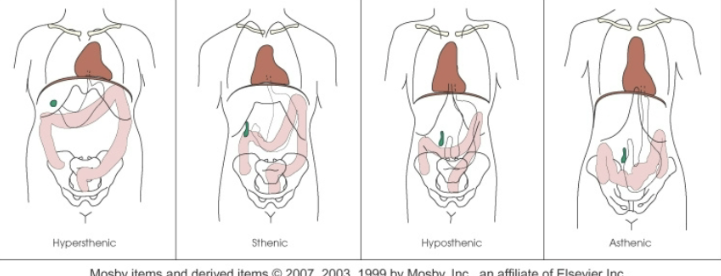
position of gallbladder varies with
body habitus
an elongated gland on the posterior abdominal wall
pancreas
head of pancreas extends inferiorly and is enclosed within the curve of
duodenum at level of L2-L3
the body and tail of pancreas pass transversely behind __ and in front of __, with tail ending at __
stomach
left kidney
spleen
pancreas is an ___ gland
exocrine and endocrine
exocrine cells of pancreas are arranged in
lobules with a duct system
pancreas exocrine produces
pancreatic juice to act on proteins, fats, and carbohydrates
endocrine portion of pancreas consists of
islets of langerhans
islets of langerhans produce the hormones
insulin and glucagon
The digestive juice secreted by the exocrine glands is conveyed into the
pancreatic duct and then into duodenum
The pancreatic duct often unites with the common bile duct to form a single passage via the __ which opens directly into the
hepatopancreatic ampulla
descending duodenum
Belongs to the lymphatic system
Glandlike, but ductless organ
spleen
spleen functions
produce lymphocytes
store/remove dead or dying rbc’s
spleen can be visualized
with/without contrast
general term for radiographic study of the gallbladder
cholegraphy
radiographic study of gallbladder
cholecystography
radiographic study of the biliary ducts
cholangiography
radiography of gallbladder and biliary ducts
cholecystangiography
cholecystocholangiography
contrast agent used for direct injection of biliary may be
any water-soluble iodinated compounds used for IVU
Performed on patients with jaundice when the ductal system has been demonstrated as dilated by CT or sonography, but the cause is unclear
percutaneous transhepatic cholangiography
PTC may also be used to
place a drainage catheter to treat obstructive jaundice
pt is placed __ for PTC with __ surgically prepared and draped
supine
right side (local anesthesia administered)
skinny needle used for PTC
chiba
after ductal system is filled
spot AP projections are made
If dilated ducts are identified
drainage catheter may be placed in the biliary duct
a __ is placed through the needle, the needle removed —>
guide wire
catheter threaded over wire
catheter can be left in place for
prolonged drainage or for stone extraction
__ may be used for stone extraction
wire basket
Performed using a T-shaped or pigtail-shaped catheter left in the common hepatic and common bile ducts for post-op drainage
postoperative cholangiography
postoperative cholangiography also called
delayed cholangiography
t-tube performed to demonstrate
Caliber and patency of ducts
Status of sphincter of the heptopancreatic ampulla
The presence of residual or previously undetected stones
t-tube chol Drainage tube clamped day before exam to
prevent air bubbles that would simulate cholesterol stones
cleansing enema is done __ before t-tube
1 hour
Contrast is water-soluble iodinated, no more than
25-30% so small stones are not obscured
After preliminary abdomen image, patient is adjusted into
RPO position with RUQ of abdomen centered to the grid
Stern stressed the importance of a lateral projection to show
branching of the hepatic ducts.
Used to diagnose biliary and pancreatic pathologic conditions
endoscopic retrograde cholangiopancreatography
ERCP is useful method when
ducts are not dilated and ampulla is not obstructed
ERCP performed by
passing a fiberoptic endoscope through the mouth into the duodenum under fluoroscopy
patient’s throat is __ to make passage of endoscope easier
local anesthetic
endoscopist locates __ and passes __
injects contrast into __
ampulla of vater
small cannula
common bile duct
why should radiographs be taken immediately after contrast?
the injected contrast should drain from normal ducts within approx. 5 minutes
dense contrast agents opacify small ducts well but may
obscure small stones
If small stones are suspected, use of a
more dilute contrast is suggested
abnormal passages, usually between two internal organs
fistulae
abnormal channels leading to abscesses
sinuses
to show origin and extent of fistula and sinuses
-fill tract with contrast
-obtain right angle projections