Week 9a Connective Tissue Structure and Function
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
connective tissue
group of tissues that demonstrates the “form follow function” idea, group of tissues with large extra-cellular components (meaning low cell density and more extracellular components like fibers, etc)
connective tissue proper
dense or loose connective tissue
can be regular or irregular
cartilage
hyaline
fibrocartilage
types of connective tissue
connective tissue proper
cartilage
bone
blood
adipose (though atypical because not much extracellular components, rather HUGE intracellular elements- lipid droplets)
cells of connective tissue
fibroblasts
osteoblasts/cytes
chondrocytes
mesenchymal cells (pleurapotential stem cells, hang around to differentiate or proliferate to replace CT)
components of the extracellular matrix
ground substance (GAGs, hyaluronic acid, fibronectin)
fibers (collagen and elastin)
function of connective tissue
primary: handle mechanical loads
secondary: energy/mineral reserves (bone- largest reservoir of calcium), injury response (scar)
fibroblast
principle cell of most CT
synthesize different fibers and carbohydrates of ground substance
secrete MMPs and TIMPS
MMPs/matrix metalloprotienases
approx 20 known human ones, examples are collagenases, gelatinases, stromelysins
breaks down protiens
activated by metals (Ca and Mg)
overproduction involved in chronic inflammation- damages CT and may damage free nerve endings causes pain
TIMPS
endogenous inhibitors: tissue inhibitors of matrix metalloproteinases
collagen
fiber: glycoprotein
assembled from procollagen subunits
vitamin C is important component in its development
as many as 10 types, tho type I most common and type II found in hyaline cartilage
reticular fibers
type III collagen
narrow fibers, loosely arrange as a mesh
provide support to different cellular components
type III collagen
aka reticulin
weaker and immature, eventually develops into type I
develop in response to injury as repair tissue
elastic fibers
allow tissue to respond to distension and stretch (return back to original length- reformation)
elastin component
randomly coiled molecule
crosslinked
form fiber with fibriliin
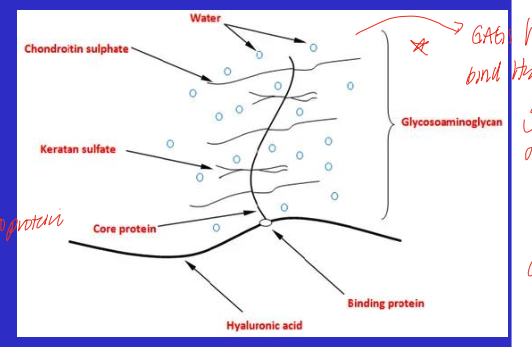
proteoglycans
core proteins bound to GAGs
GAGs have high density of negative charges due to sulfate and carboxyl group- this attracts water since positive pole and forms a hydrated gel (amount of gel depends on the cell/tissue)
hyaluronic acid
long, rigid GAG, not bound to proteoglycan
also a key element of ground substance
loose connective tissue proper
irregular
sparse, thin fibers (collagen, reticular, elastin)
abundant ground substance
mostly found beneath surface epithelia which is often a site of immune and or inflammatory reactions
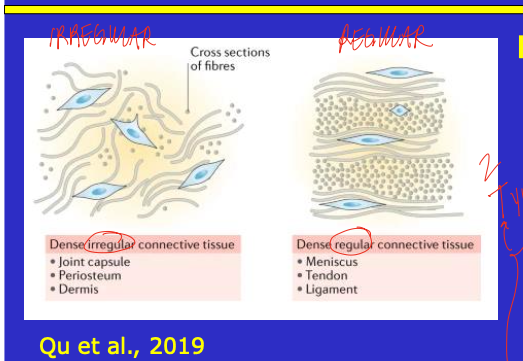
connective tissue proper
dense CT with mostly fibers, few cells and little ground substance
can be irregular or regular
irregular: no primary orientation of fibers
regular: tendon, ligament, ordered arrangement of fiber
elastic CT: more elastin by proportion (lungs, aorta) but don’t even need much elastin
skin layers
epidermis
dermis
subcutaneous (hypodermis)
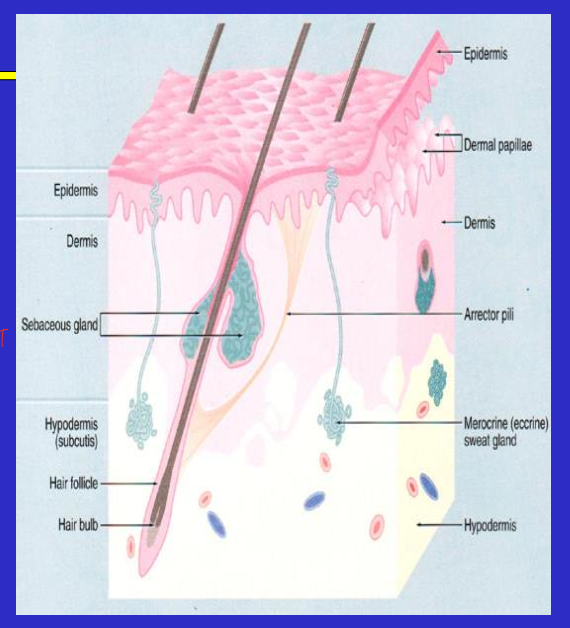
epidermis
most superficial later of skin, 0.06 to 0.6 mm
dermis
below the epidermis, 2-4 mm
consists of 2 layers and is highly vascular with lymphatic vessels
papillary dermis
reticular dermis
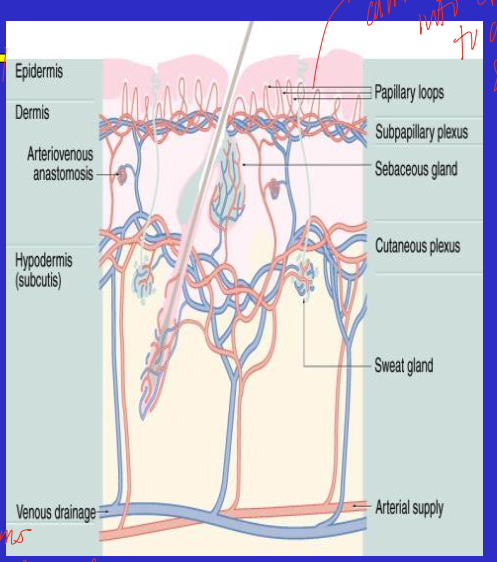
subcutaneous
deepest layer of skin (hypodermis), very variable in thickness both within and across individuals, depends on adiposity
papillary dermis
layer of dermis that is anchored to the epidermis via basement membrane
loose irregular connective tissue
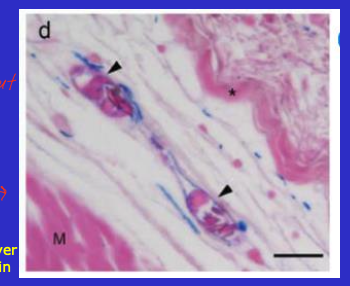
reticular dermis
layer of the dermis
dense, irregular connective tissue
contains fibroblasts, macrophages, and mast cells (have inflammatory function since slow to skin surface and may need to fight off foreign material)
function of irregularity of fibers in skin
irregularity allows for flexibility in the skin that is due to the differences in forces and directions of forces that the skin comes in contact with, allows for some freedom of movement
tendons
bone to muscle
some degree of vascularization and nerve supply
immune cells and cytokines respond to injury and signal type III collagen formation- which is weaker and may increase the risk of reinjury
ligament
bone to bone
some have a direct blood supply and innervation (example is the PCL)
tendon and ligaments
fibers and fibroblasts in parallel
exhibit crimp
produces toe region
ligament mechanics
stress strain curve, as force increased the deformation also increases until a yield point where enters the plastic region, and then ultimate failure point
cartilage
matrix heavy
3 main type- hyaline, fibro-, elastic
tend to be avascular (particulary hyaline)and aneural
hyaline cartilage examples
intercostals- ribs
trachea and bronchi
articular cartilage at bone
epiphysial plate
primarily type II collagen
fibrocartilage examples
intervertebral discs
pubic symphysis
attach tendons to bones
more type I collagen
elastic cartilage examples
external ear
external auditory and custachian tubes
cartilage in larynx
tip of nose
face, nose, ears, larynx
chondrocytes
cells of cartilage
actively produce matrix components
tends to decline with age- ground substance is greater than collagen, so the capacity to accommodate load and injury declines with age
tend to localize in nests or lacunae
cartilage matrix
thin, sparse type II collagen fibrils
GAGs (hyaluronic acid, chondroitin sulfate, keratan sulfate)
H2O accounts for about 70%, most is tightly bound to GAGs. gives resilience and resistance to compression
intermittent compression of cartilage
“milking”
critical to nutrition, waste removal
synovial joint (diathrosis)
joint with capsule
inner lining has synovial membrane which secretes synovial fluid
behaves like epithelium bc adapted to secrete
lacks the structural hallmarks of epithelium tho
secretes proteoglycans and hyaluronic acid
synovial fluid
filtrate of plasma, hyaluronic acids, and GAG complexes
combined with hyaline cartilage, produces a very low friction environment, allows for smooth movement and less shear
important for joints that bear a lot of weight
bone
mineralized CT
reservoir for Ca and PO3- (calcium and phosphate)
functions in structure, movement, protection, mineral homeostasis, hematopoiesis (blood cell synthesis)
compact and cancellous bone
good blood supply and innervated
aka cortical and trabeculae bone
combination provides strength flexibilty, and limited weight
osteocyte
mature bone cell
isolates in its own lacunae with canaliculi to get blood supply
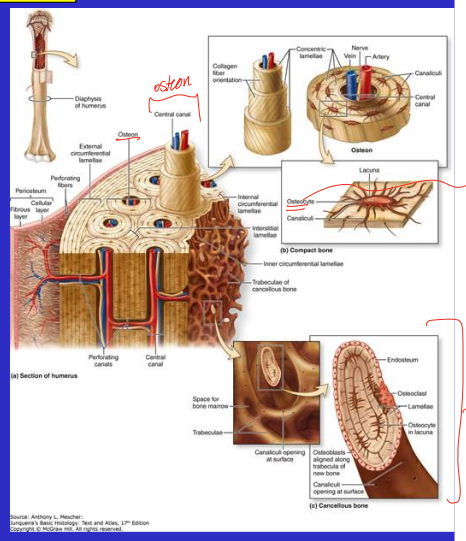
periosteum
tough fibrous connective tissue around surface of bone
highly vascular
highly innervated
anchored by Sharpey’s fibers
hurts if damages (this is where we feel pain when we break a bone)
cells of bones
osteoprogenitors- periosteal and endosteal, divide, differentiate, and proliferate
osteocytes- mature osteoblast, maintains matrix
osteoblasts- immature osteocyte, active, secretes matrix and involved in mineralization
osteoclasts- large, multinucleate, phagocytic cells, bone resorption
matrix of bone
osteoid- type I collagen and glycoproteins
hydroxyapatite- calcium and phophate salts, 60% of the mature matrix
osteogenesis imperfecta
issues with osteoid in the matrix (less and fewer than normal), increases risk of fractures
ex: Mr Glass from that movie
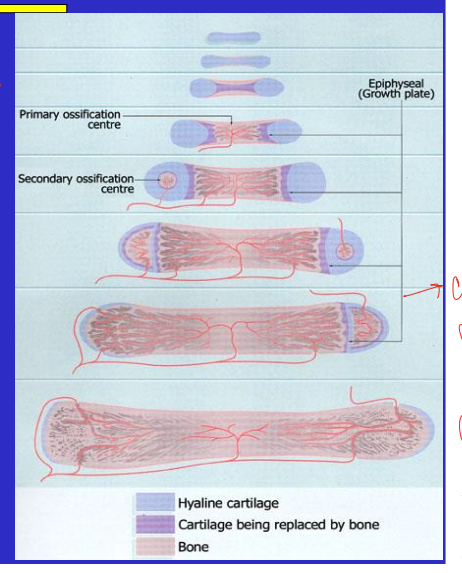
endochondral ossification
bone formation
bones built on a cartilage model
axial growth continues until closure of epiphyseal plate
flat bones tho are via intramembranous ossification that may continue throughout life
bone remodeling
occurs throughout life
regular breakdown/replacement of osteocytes and bone mineral
bone deposition occurs at sites of injury or stress
phone bone (bone formation on back of skull bc of looking down at phone all the time), osteophytes (kinda like bone spurs)
bone pathology
pathology in matrix, bone mass and density, or mineralization of bone, examples include:
osteoporosis/penia
osteopetrosis
ostomalacia
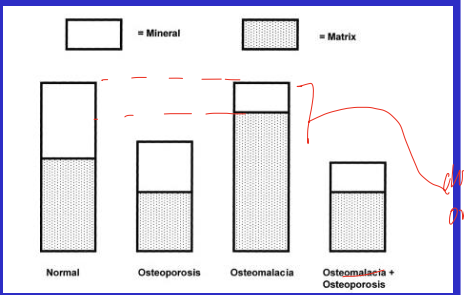
osteopetrosis
bone pathology characterized bu excess mineralization- bones get heavy and dense, the mineral crystal aren’t formed right and end up making the bones brittle
osteomalacia
(bone softening)- exhibits matrix demineralization, but not reduction of bone mass
osteoporosis/penia
net reaabsoption will reduce bone mass, loss of matrix, low bone mass
numerous risk factors but exact cause unknown
fracture healing of bone
bone does not actually heal
other cell/tissue types are activate to make new bone to unite ends of the break
periosteum and marrow
re-engage endochonral ossification (normally rapid in healthy tissue)
problems include malunion, nonunion, or critical defect
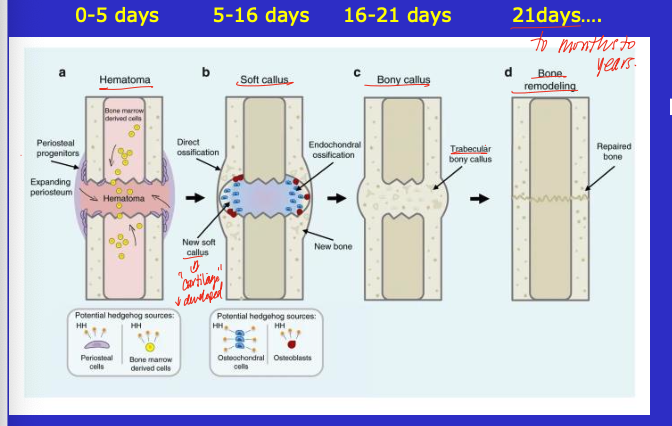
role of periosteum in fracture healing
cells divide and about half move to clot and become osteoblasts
role of marrow in fracture healing
cells dedifferentiate, form procallus (blastema) and later become cartilage
critical defect of bone
2.5-6 cm, bone can’t recover from this gap in bone on its own
adipose tissue
more cellular, less matrix than other CT
white and brown
hypertrophy and hyperplasia- post mitotic
precursors differentiate into new adipocytes (adipogenesis)
highly vascular
white adipose tissue
energy depot
structural support by dispersing load over bony prominences
beige-ing: takes on aspects of brown adipose and may be a consequence of aerobic exercise
brown adipose tissue
minimal in adults (if at all)
increased mitochondria
increase rate of fat oxidation
thermogenic
uncoupling- uncouple oxidation from phoshorylation- still do the ETC but don’t phsophorylate ATP, instead use energy to make heat
white adipose tissue variability
gene expression differences between depots (subcutaneous vs visceral)
diet and exercise effects on morphology