NMSK - Tissues
1/83
Earn XP
Description and Tags
Week 1 -
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
84 Terms
Where does connective tissue originate from?
The mesodermal layer of the embryo, embryonic mesenchymal tissue
Give a general overview of tissues
Tissues consist of distinct types of materials, formed from specialised cells and their products.
They’re a cellular organisation level between cells and a complete organ.
Similar cells and their extracellular matrix from the same embryological origin, working together to perform a specific function.
What are the 4 different kinds of tissue
Epithelial tissue
Nervous tissue
Connective tissue (blood tissue (may be categorised as its own connective tissue)
Muscle (contractile) tissue
Outline nervous tissue structure
Called nerve cells/neurones.
Neuroglial cells are found in the central nervous system and include astrocytes, oligodendrocytes, microglial cells, ependymal cells. In the peripheral nervous system we have satellite cells and Schwann cells.
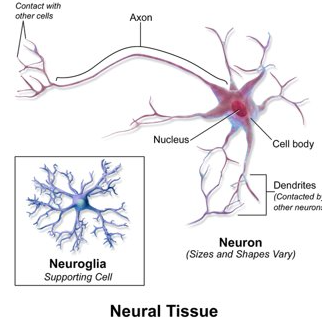
What are the functions of neurones and neuroglial cells
Neurones receive and facilitate nerve impulses and are classified based on function and structure
Neuroglial cells are supporting cells, facilitating conduction of nerve impulses, immune function and maintenance of neurones (for example)
What are some of the functions of connective tissue
Mechanical and structural support
Support and connecting various part of the body by a 3D framework known as the stroma
Separating tissues and organs
Support, movement, protection and fat (energy) storage.
Name the 5 main categories with subgroups of connective tissues
Loose connective tissue
Dense connective tissue (regular and irregular)
Cartilage (hyaline, elastic and fibro~)
Bone (lamellar and trabecular)
Blood
What do all connective tissue structures have in common?
All are composed of a variable cell structure and fibres surrounded by an extracellular matrix that may be solid, fluid or gel (depends on the function of the particular connective tissue)
Describe/draw the structure of loose connective tissue, examples, function and how it compares to DCT
Structure: cells are found within a network of mostly collagen fibres, type 3 collagen
Also called areolar connective tissue.
Examples: mucosal and submucosal connective tissues of blood vessels, muscles, nerves and organs such as the kidney and liver. Example - interstitium (supporting nerves and vessels), stroma (structural tissue of organ, framework supporting parenchyma)
Function: Loose packing, support, nourishment to associated structures and tissue sliding, fluid reservoir, defense and regeneration.
Compared to DCT:
Fewer fibres (although still collagen and elastin), more cells around ground substance, less rigid and more easily distorted but due to collagen presence, it can still provide resistance when stretched creating a tough barrier.
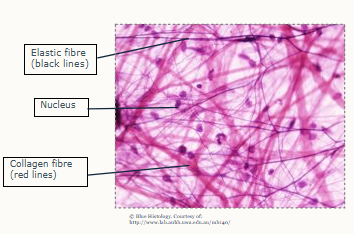
Outline the structure, function, location and compare to LCT of Dense connective tissues (DCT)
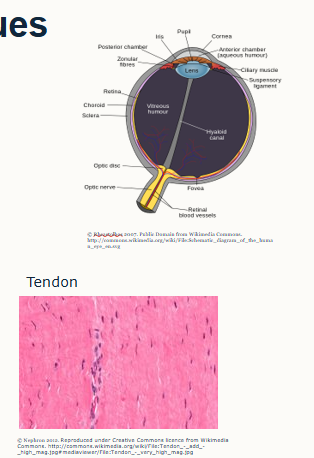
Structure: Matrix composed of collagen and elastin fibres, type 1 collagen, fibre rich (disordered bundles of parallel fibres (sclera, skin, dura matter), parallel ordered bundles (tendon and ligaments). Sparce cellularity
Function: Tensile strength and stretch resistance.
Location: tendon, ligament, cornea of eye and arteries
Compared to LCT: A higher proportion of fibres, fewer cells and less ground substance in extracellular matrix.
It can be divided into regular and irregular connective tissue (depends on alignment of fibres)
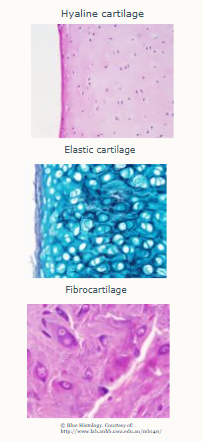
Outline the types, structure and function of cartilaginous tissues
3 types: hyaline, fibrocartilage and elastic cartilage.
Calls in cartilage are called chondrocytes that produce a matrix made up of type 2 collagen, glycoproteins and water. It does not contain Calcium Phosphate (Ca3PO4,2) therefore it’s more flexible than bone. It is continually broken down and renewed.
Structure: varies depending on cartilage type
Function: provides flexibility with rigidity, fibrocartilage can withstand considerable pressure
NOTE: poorly supplied with blood
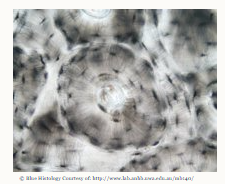
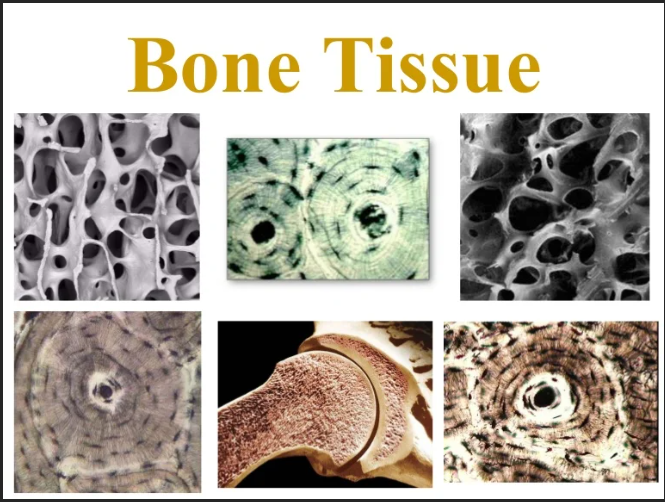
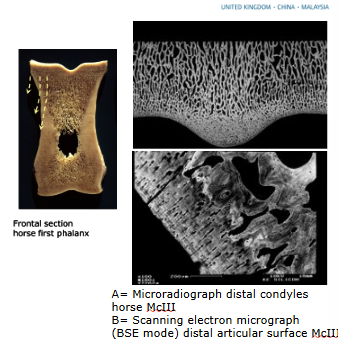
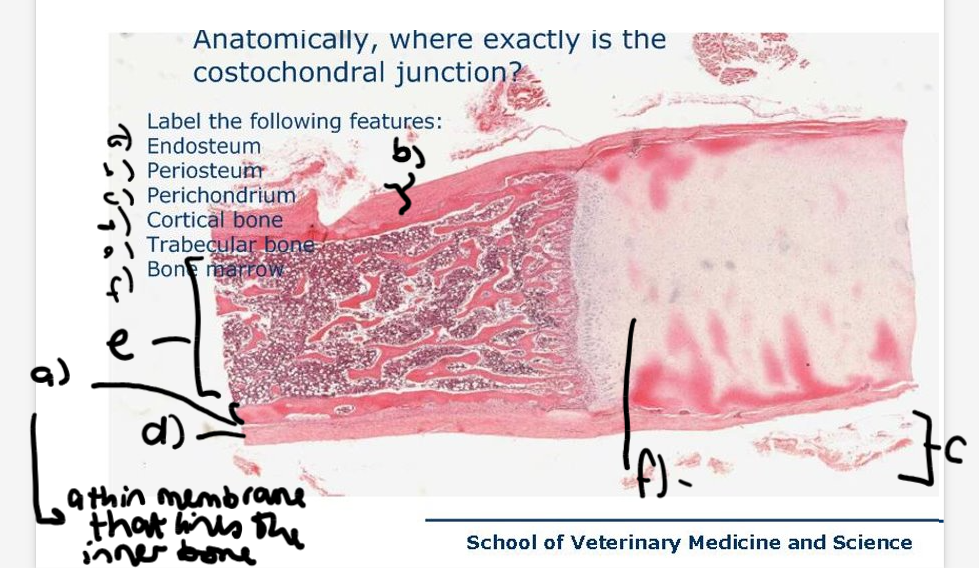
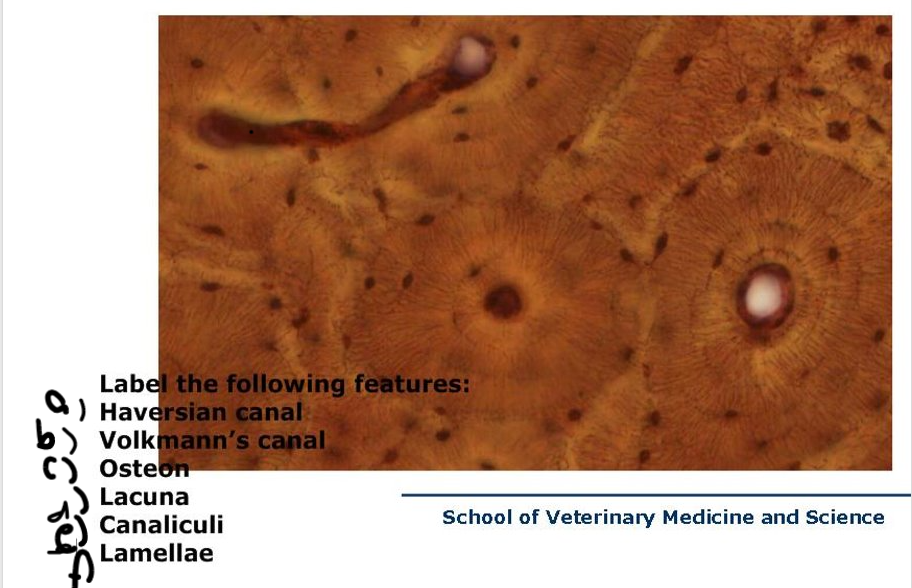
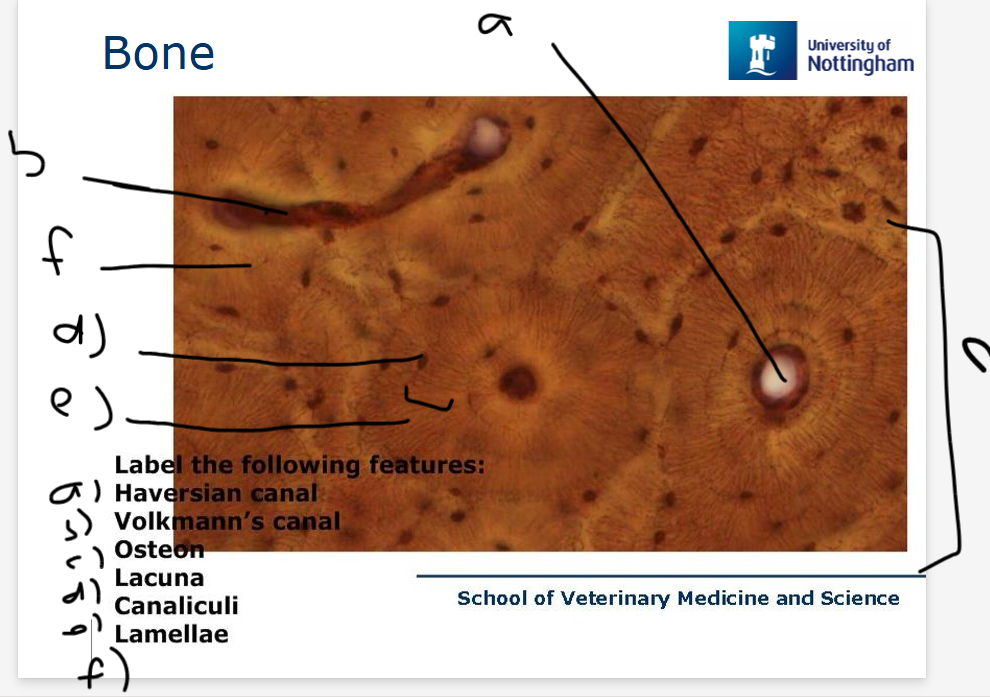
Outline the structure, types and function of bone tissue
2 types: Lamellar (compact) and Trabecular (spongy) bone
constantly remodelled through life
Hard because of calcium phosphate (as hydroxyapatite) in the extracellular mix
Structure: collagen network - tensile strength
crystalline - compressive strength
bone cells - maintenance of bone
Function - provide strength and support
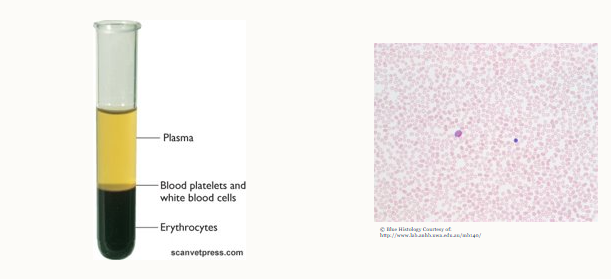
What about blood tissue
Blood tissue is a special kind of liquid connective tissue
contains plasma, blood platelets, white blood cells and erythrocytes
What are the 3 main components of connective tissue structure
Cells, Collagen fibres, ground substance (special proteins)
Cells are separated from each other by abundant extracellular matrix which is non-living and is the basis for classification of connective tissue subgroups
Outline connective tissue cells (names, how are they named, overview)
Overview - various cell types are embedded within all connective tissues
Named by the tissue they produce/maintain:
Cartilage - chondrocytes
Bone - osteoblasts/osteocytes/osteoclasts (derived from monocytes)
Muscle - myocytes
Tendons - tenocytes (elongated fibrocytes)
What is the structure of the extracellular matrix structure?
Collagen and elastin fibres:
a) collagen is strong, flexible but inelastic (several types, type 1 is most common)
b) Reticular fibres - fine collagen type 2 (networks of these fill space between tissue and organs)
c) elastin - elastic properties (percent varies according to tissue function)
Ground substance (non-fibrous protein and other molecules): amorphous gel-like substance (surrounds cells), components including hyaluronic acid and proteoglycan
d)water
Blood doesn’t contain collagen fibres.
Doesn’t consist of tightly packed cells and most of the tissue volume is made up of extracellular space - filled with the extracellular matrix.
What is the function of extracellular matrix (ECM)
Structure gives connective tissue its morphology and functional characteristics
not inert, it’s dynamic.
Supports cells, guides their division, growth and development
What cells produce the ECM
Specialist cells in the tissues - name of cells ends with suffix that identifies function:
blasts = create matrix
cytes = maintain matrix
clasts = break down matrix for remodelling
State the function for each type of these cells:
osteoblast
osteocyte
osteoclast
fibroblast
chondrocyte
Osteoblasts create the cell matrix for bones
Osteocytes maintain the cell matrix for bones
Osteoclasts are cells that breakdown bone for its remodelling
Fibroblasts are cells that create ECM
Chondrocytes produce and maintain cartilaginous matrix
What are the 2 types of fat cells
Adipocyte and lipocyte
Compare a fibrous ECM to a liquid ECM and what happens to the structure of the connective tissue?
Fibrous ECM is a network of protein fibers like collagen and elastin that provides structural support and tensile strength, liquid ECM is the "ground substance" or hydrated gel composed of proteoglycans and glycosaminoglycans that fills spaces, facilitates transport, and acts as a medium for cellular signaling
What do different bone tissues look like
Outline the different kinds of fatty tissue and their structure/function
•Brown adipose tissue - heat
•White adipose tissue - energy store
•Structure: little ECM surrounding cells, cells full of lipid
•Function: packaging, protection, insulation
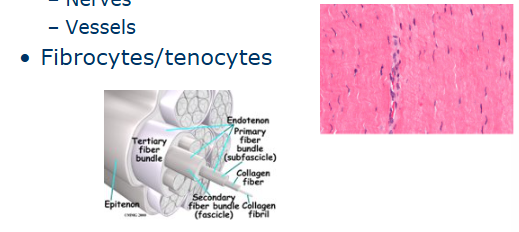
What does tendon tissue look like?
Made of parallel collagen fibres (strong, flexible and resistant to damage). Surrounded by the peritenon (nerves and vessels)
Arranged in small fibres in bundles.
Primary fibre bundles (subfascicles ) - smallest bundle
Secondary fibre bundle (fascicles) - groups of subfascicles
Tertiary (3rd) fibre bundles - contains groups of fascicles that form the tendon itself.
How does the embryo form
Expands by binary fission after which the divisions are less obvious as cell no. increases. Eventually a ball forms, part of which becomes the embryo and 2 cell layers are formed, then a 3rd by the invagination of the surface layer.
Outline 3 embryonic components
Ectoderms - epithelium of extreme ends of the tract (outer epithelium and nervous tissue)
Mesoderm - becomes the musculoskeletal system including smooth muscle (note - produces the embryonic mesenchyme as it differentiates - the term for the loose tissue ‘stuff’ in an embryo that gives rise to various tissues)
endoderm - becomes the intestinal epithelium
Where does connective tissue come from? Give examples
The MESODERM (middle later)
Myocytes, chondrocytes, cardiomyocytes, adipocytes, odontoblasts, cementoblasts, osteoblasts (derived from monocytes), erythrocytes, leukocytes, osteoblasts and osteocytes, collagen-producing cells (fibroblasts, fibrocytes, tenocytes and ligamentocytes) and leiomyocytes (smooth muscle cells, blood vessels, bronchioles, gut, uterus, prostate and uterus)
name and outline features of 3 additional connective tissues
Embryonic connective tissue
loose connective tissue formed during early embryonic development
found primarily in the umbilical chord
features: hydrophilic ECM, jelly-like, known as mucoid connective tissue/Wharton’s jelly.
Reticular connective tissue
contains reticular and elastic fibres (predominate in irregular connective tissue)
reticular fibres (type 3 collagen) form the stroma of the lymphoid system (lymph nodes, spleen)
elastic fibres - intervertebral disks and wall of aorta
Adipose tissue (see other card)
Outline the 12 stages of embryology
1. Fertilised egg
2.Cell Zygote
3.Cell Adhesion
4. Cell morula
5. Blastocyst
6. Zona hatching
7. invades uterine wall
8. Cell mass differentiates
9. bilmainar disc forms
10. mesoderm forms
11. mesoderm spreads
12. amniotic sac grows
What are the 4 tissues in embryology
1.Epithelial (skin, lung and GIT lining).
2.Neural (nervous system, derived from embryonic ectoderm, hence termed neuroectoderm).
3.Contractile (all muscles, derived from embryonic mesoderm).
4.Connective (everything not in 1, 2 & 3! Derived from embryonic mesoderm).
What are some key characteristics of epithelial cells
form basement membranes
very little extracellular space b/w cells
no blood vessles (inparticular near the surface, often underneath and nutrients are transported via diffusion)
Can have apical modifications (because they have the top/bottom/inside/outside orientation, they can have adaptions on one of these sides)
How can we classify tissues such as epithelia
morphology - shape and arrangement (layers)
function - glandular vs non-glandular (on its own or in unison?)
what 4 kinds of simple epithelium are there - morphology classification
simple squamous - e.g. endothelium
simple cuboidal - e.g. renal tubules
simple columnar - e.g. gall bladder (markedly polarized, often with apical modifications)
simple pseudostratified columnar (means, almost stratified (layered), columnar cells) - the nuclei are not all orientated on one level, giving the impression of a multi layer. All cells rest on a basement membrane.
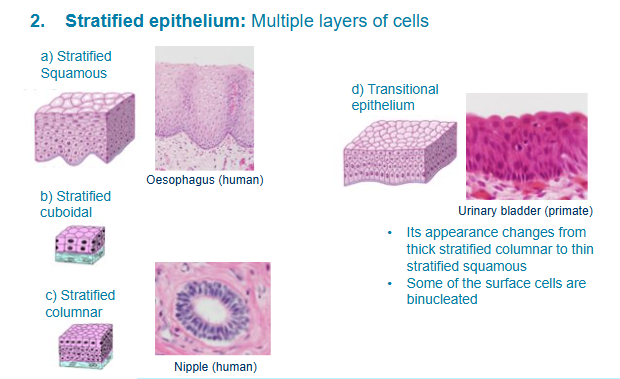
What 4 kinds of stratified epithelium are there
stratified squamous - cuboidal at the bottom, become more squamous towards the top (flattened)
stratified cuboidal - look cuboidal in all layers
stratified columnar - the outer level becomes cuboidal
transitional epithelium - starts columnar and ends cuboidal (often found in the urinary tract) - may make you think it looks like there are 2 nuclei in the cell
What is the function of simple squamous
best suited for passive transport of substances across the cytoplasm.
provide little protection so they’re not found on surfaces subject to high stress
examples - alveoli, vessels 9endothelium), body cavities (mesothelium).
What is the function of simple cuboidal and columnar epithelium
usually making and secreting and/or absorbing a substance.
Simple cuboidal examples are thyroid, kidney, lung, ovary, ducts and secretory portions of many glands
simple columnar - intestine, female reproductive tract and in many exocrine glands.
what is the function of pseudostratified epithleium
secretion and movement of particles along the tubular organs
called ‘respiratory epithelium’
e.g. trachea bronchi, epididymis, vas deferens.
when may we use other stains such as trichrome stain instead of H&E?
if wwe want to see certain features such as cilia that we can’t see with H&E
what is the function of stratified squamous epithelium
protection of underlying tissues and prevent their desiccation
most common multi-layered epithelia.
In small animals - in the skin, the outer layers undergo keratinisation, however it doesn’t occur where tissues remain moist (oral cavity, oesophagus, anal canal, eyes or vagina)
In animals where really tough food is being digested, they will have more keratinised cells in response to their diet (oral cavity, oesophagus and non -glandular part of stomach)
large animal - ^, also found on skin.
What is the function of stratified cuboidal and columnar
not abundant
found voering areas of transition b/w simple and stratified epithelia - resp tracts, ducts of exocrine glands.
what is the function of transitional epithelium
urogenital system only
also called urothelium
subject to marked variation fo internal pressure, found in these areas because they’re able to alter cell shape based on degree of distension.
What do we need to consider when looking at microscope slides
orientation of the sample we’re viewing on a slide - it will change how the cells appear to be orientated.
How do we classify epithelial glands
method of secretion
type of secretion
shape
cell numbers
Outline endocrine (ductless) glands
lack a duct system, no connections to external or internal surfaces
produces hormones
near blood vessels
high diversity in morphology
outline exocrine glands
secrete to a lumen (e.g. pancreas) or free surface (intestines)
calssify regarding their number of cells (unicellular or multicellular)
shape a)of the secretory component (tubular or acinar) b)simple (one unbranched tube) or compound (branched tubules)
type of secretory product - serous (clear, watery fluid), mucous (more viscous fluid), mixed (mixture of serous and mucous fluid)
Type of secretion - merocrine (exocytosis, cell membrane intact), holocrine (cell membrane rupture), apocrine (‘decapitation’ secretion).
what specialisation of epithelia are there
basal membrane
apical modifications
cell junctions
what are 3 apical modifications we see?
Cilia - motile, long cell processes (resp tract, oviduct and uterus)
Microvilli - non-motile, minute projections found in epithelia specialised for ABSORPTION, they markedly increase SA (kidney and intestine)
Stereocilia - long microvilli (epididymis and vas deferens)

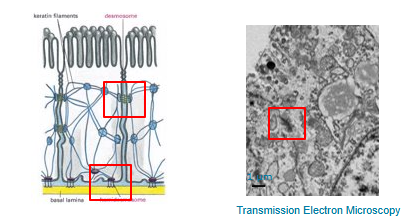
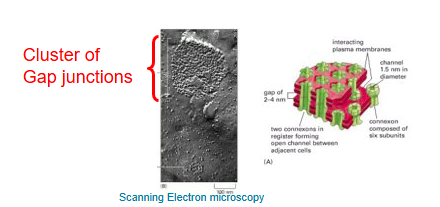
What 3 types of cell junctions are there
Adherent junctions - anchor. Cells must bind to each and to the connective tissue to assure tissue cohesion
Tight junctions - occluding. Cells are involved in the control of what enters the body
Gap junctions - communicating. Cells must communicate with each other.
Go into more detail about adherent junctions
The stiffness of a tissue is provided by these links mechanically.
cells together = desmosomes
cells to the extracellular matrix = hemidesmosomes
Go into more detail about tight/occluding junctions
specific compounds from the intestinal lumen (apical surface) must diffuse toward the blood vessels however their entrance must be controlled.
two pathways exist for it - paracellular and transcellular
tight junctions limit the paracellular movement of water and other molecules.
Go into more detail about gap junctions
cells from the body must also communicate efficiently between them. This is controlled by these gap junctions
They’re aqueous channels (‘pore’ like structures) allowing small molecules (<_ 1000Da molecular weight) to pass b/w adjacent cells.
Outline mesenchyme tissue
loosely associated via cell processes
surrounded by extensive extracellular matrix - proteoglycans, glycoproteins, fibres and other molecules
Outline connective tissue
fibroblast/cyte
extracellular matrix:
fibres: collagenous, elastic and reticular
ground substance: GAG (hyaluronic acid), proteoglycans, glycoproteins (laminin and fibronectin)
Outline fibres
collagen fibres (crimp, arrangement, tension, tendon, fascia, capsules, cartilage, bone)
elastic fibres (capsules, lungs, arteries, stretch up to 150%)
reticular fibres: stroma (supportive), liver, kidney, spleen, lymph nodes, bone marrow
Outline collagen structure
main structural protein in connective tissue
polypeptide triple helix = tropocollagen
main amino acids are glycine, proline, hydroxyproline, hydroxylysine
lysyl oxidase - cross links which form covalent bonds
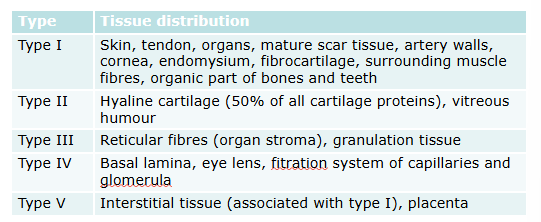
Where do we primarily find the first 5 types of collagen
Outline the contents of ground substance
interstitial fluid - transport of small molecules b/w cells and blood supply
ground substance has GAG (glycoaminoglycans: hyaluronic acid, chondroitin sulphate and keratin sulphate), proteoglycans and glycoproteins
What are glycosaminoglycans
unbranched polysaccharide chains composed of repeadting disaccharide monomers (one is usually an amino sugar)
huge molecules that occupy large amount of extracellular space
highly negatively charged (sulphated or carboxylated)
qualities:
attract cations
highly osmotically active (draw and hold water into matrix)
good at withstanding compressive forces
what are clinical uses of GAGs
reduces inflammation
enhances function
mechanism isn’t completely understood
Name 3 properties of hyaluronic acid
resists compression - major component of hyaline cartilage and synovial fluid
major component of skin (involved in many aspects of skin repair)
facilitates cell migration and proliferation
Outline proteoglycans
large aggregates (core protein, covalently bound GAGs)
lend plasticity and elasticity to tissues
trap water to influence tissue consistency
Outline glycoproteins
proteins that contains oligosaccharide chains covalently attached to polypeptide side chains
often important integral membrane proteins
play a role in cell-cell interactions
bind together fibres, cells and ground substance in connective tissues
Outline laminin
major proteins in basal lamina
influence: cell differentiation, migration, adhesion, phenotype and survival
outline fibronectin
secreted in many cells, mainly fibroblasts
involved in cell adhesion, growth, migration and differentiation, wound healing and embryonic development
Outline supportive connective tissue
bone and cartilage
sparce cellularity
collagen fibres give tensile strength
composition of ground substance give characteristic mechanical properties
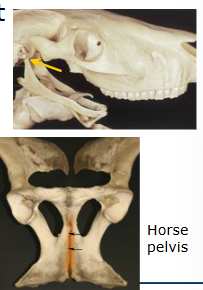
What 3 types of joints are there
fibrous joints - sutures (skull), syndesmoses (splint bones), gomphosis (teeth - alveoli).
Cartilagenous - synchondroses (b/w skull and hyoid bone), symphysis - 2 halves of pelvis.
synovial joints e.g. metacarpophalangeal (fetlock) joint.
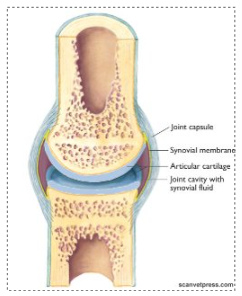
what is the synovial joint structure
articular cartilage
subchondral bone
epiphyseal bone
synovial membrane
synovial fluid
capsule and ligaments
What is subchondral bone
forms joint surfaces
supports cartilage
distributes loads to epiphyseal, metaphyseal and cortical bone
variable thickness
undulating junction with cartilage (no fibres cross)
rich supply of blood vessels, lymphatics and nerves
Relatively compliant:
maintains joint congruency and absorbs impact load
what is epiphyseal bone
undergoing modelling - growing bone, functional adaption
remodelling - functional adaption and repair
what is synovial fluid
appearance:
clear, slightly yellow-ish, slippery yet viscous (should feel like egg white 2-5cm stretch)
role:
fills joint space
ultrafiltrate of plasma (contains similar ions and small molecules, high conc of hyaluronan)
lubrication (soft tissues)
nutrition
Outline some parameters of synovial fluid
volume usually low
slightly negative pressure (-1.25mmHg - helps stabilise the joint)
pathology leads to an increased volume (distended joint, >51mmg) - reduced joint stability and increased distance for nutrients to diffuse down
How do we analyse synovial fluid and what are some benefits
Benefits = allowing the clinician to determine if there’s evidence of disease (joint infection, OA, immune-mediated arthritis)
How? Intra-articular injection (joint block) and therapeutic (intra-articular med) purposes - synovialsentesis
Technique:
suitable restraint
aseptic prep (minimum 3 minutes contact with a suitable disinfectant after clipping, gloves, sterile alcohol wipe post disinfectant, sterile equipment).
good knowledge of anatomy is needed
collect suitable samples
Compare normal vs abnormal looking synovial fluid
Normal:
clear/yellow
no cloudiness/tubidity
viscous - forms a string b/w fingers/from end of syringe
cytology - usually low cell count (,5×10^9 cells/litre), some neutrophils, lymphocytes and mononuclear cells
pH <6.9
total protein 10-20g/l
Abnormal:
yellow/red
cloudy/tubid
watery - doesn’t form a string
increased neutrophil levels for bacterial/fungal infections
increased eosinophils for autoimmune disease
Note - some disease conditions may have normal looking fluid
How can we use biomarkers in analysing synovial fluid
markers of increased metabolism (bone and cartilage)
markers of increased matrix destruction
markers of inflammation
What is the synovial membrane
lines all inner surfaces of joint (except cartilage)
highly vascularised
ruffled villi/smooth surface
2 main synoviocytes:
A = macrophage-like (eat debris)
B = fibroblast-like (synthesise macromolecules, collagen and hyaluronan)
what is the function of the synovial membrane
produces synovial fluid (plasma filter, synthesise essential molecules e.g. collagen and hyaluronan)
nutrition - brings blood vessels close to cartilage surface
clear debris from joint
what is the joint capsule
supports synovium
stabilises joint
contains nerves which are important in proprioception - monitor joint position and movement
what are collateral ligaments
providing stability between bones forming a joint
tendon-like but higher ration of elastin to collagen, allows some more stretch
Name 2 other synovial structures
tendon sheaths - ease passage of tendons around angles
bursae - cushion and protect soft tissues passing over hard ‘points'
What factors affect joint homeostasis
load bearing - non-weight bearing leads to a decrease in subchondral bone, joint space and cartilage proteoglycan content which can lead to OA
‘normal’ forces - ensures even load-bearing across the joint surface, distributes weight evenly through peri-articular tissues
cartilage turnover - continual SLOW process of remodelling and repair of collagen and proteoglycans
low concentrations of cytokines (peptide regulatory factors)

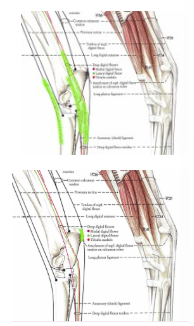
Label this diagram correctly
Label this diagram
What minerals are stored in bone tissue?
calcium
phosphate
sodium
citrate ions
magnesium
traces of zinc, selium
potassium
What are the roles of calcitonin, calcitriol and parathyroid hormone in calcium regulation?
calcitonin - helps lower blood Ca levels and blocks the activity of osteoclasts to reduce the amount of Ca entering the blood
Calcitriol - increases absorption of dietary Ca and phosphate from the GI tract and stimulating the release of Ca stores from the skeletal system
Parathyroid hormone - stimulates osteoclasts which increase the rate at which they release calcium.
