Folic Acid in Pregnancy – Should We Fortify? (POPLHLTH 206 / Lecture 13)
1/65
Earn XP
Description and Tags
38 vocabulary flashcards covering definitions, study findings, policies, benefits, and risks related to folic acid use for preventing Neural Tube Defects, as presented in POPLHLTH 206 Lecture 13.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
Neural Tube Defects (NTDs)
A major birth defect of the neural tube failing to close 22-28 days post conception
Neural tube closure window
Critical period between days 22–28 post-conception when the neural tube must seal to avoid NTDs.
Spina bifida
NTD involving incomplete closure of spinal structures; may cause paralysis, incontinence, and learning difficulties.
Anencephaly
Fatal NTD in which cranial structures, including much of the brain, fail to develop.
Folic acid (synthetic folate)
A B-vitamin added to supplements or foods that can prevent most NTDs when taken periconceptionally.
Red blood cell (RBC) folate
Biomarker of long-term folate status; levels ≥905 nmol/L are considered optimal for NTD prevention.
Medical Research Council (MRC) Vitamin Study
1991 multicentre RCT showing a 72 % relative reduction in recurrent NTDs with 4000 µg folic-acid supplementation.
MRC study key dose
4000 µg (4 mg) daily folic acid started before conception for women at high NTD risk.
China–US Collaborative Project
1999 cohort study showing 79 % NTD reduction in high-incidence northern China with 400 µg folic acid daily.
High- vs. low-incidence regions (China study)
NTD prevention effect was strong in the North (high baseline rate) but non-significant in the South (lower baseline rate).
Daly et al. (Ireland) finding
Demonstrated inverse, dose-response relation between RBC folate and NTD risk; 905 nmol/L threshold adopted by WHO.
400 µg folic-acid supplement
Standard periconceptional dose recommended for primary NTD prevention in the general population.
Bioavailability advantage
Folic acid in supplements/fortified foods is more readily absorbed than naturally occurring food folate.
Mandatory fortification
Government requirement to add folic acid to a staple (e.g., flour); aims to reach entire population regardless of behaviour.
Voluntary fortification
Industry may choose to add folic acid to products; coverage depends on manufacturer participation.
Targeted supplementation strategy
Providing high-dose folic acid to women planning pregnancy or at high NTD risk; needs awareness and adherence.
Masking vitamin B12 deficiency
High folic acid can correct megaloblastic anaemia while allowing irreversible B12-related neuropathy to progress undetected.
Antifolate drugs
Cancer therapies (e.g., methotrexate) that inhibit folate metabolism; reason for caution about excess folic acid and cancer risk.
Folic acid & cancer evidence
Meta-analysis (Vollset 2013) showed no significant increase in total cancer (RR 1.06, 99 % CI 0.99-1.13) after supplementation.
Stroke benefit (Huo et al. 2015)
800 µg folic acid daily lowered stroke risk by 21 % in hypertensive Chinese adults.
Global NTD burden
≈260,100 affected births annually worldwide (Blencowe 2018).
NTD prevalence in New Zealand
≈10.2 per 10,000 births (MPI 2018), including live births, stillbirths, and terminations.
NZ hospital impact
Average 21 major operations, 178 hospital days, and NZ$944,000 cost per year for NTD cases.
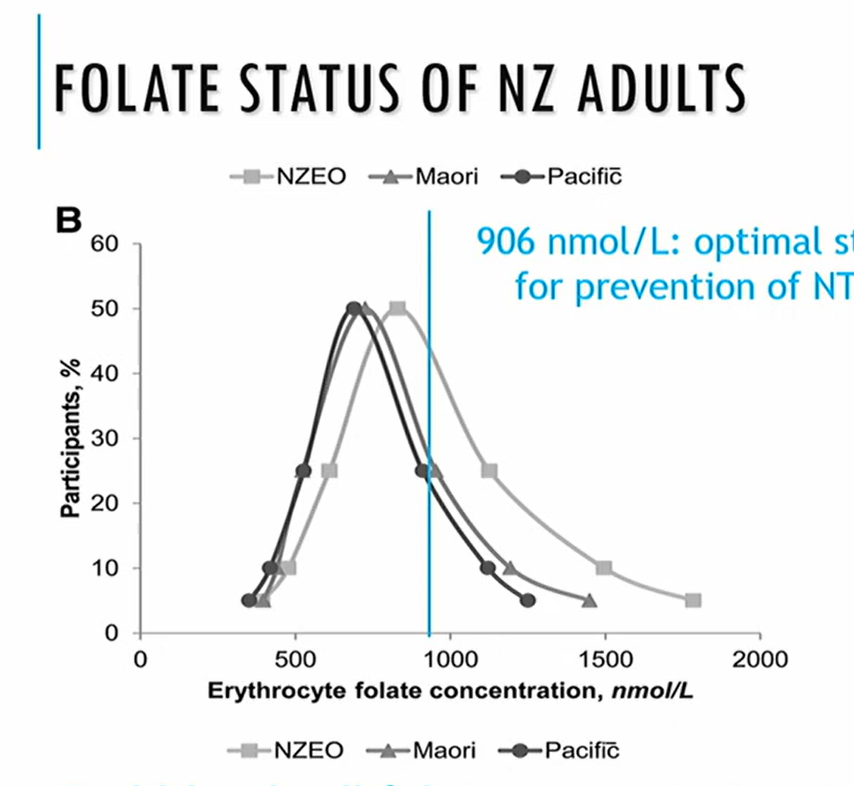
NZ RBC folate status (2008/09)
Mean 544 nmol/L in women 15-49 y; 16.2 % below minimal-risk cutoff (748 nmol/L).
NZ supplement recommendation
800 µg folic acid daily from at least four weeks pre-conception to 12 weeks gestation.
Supplement use rates (NZ)
Growing Up in NZ (2010): 58 % of planned pregnancies used supplements before conception; only 9 % of unplanned did.
NZ fortification timeline
Voluntary (1996);
planned mandatory (2009) - delayed;
mandatory fortification announced 2021;
Came into effect 2023
Bread-making flour standard (NZ); what’s added per kg?
Non-organic wheat flour for bread must contain 2-3 mg folic acid per kg under Food Standards Code 2.1.1-5(a).
low amount considering high-risk women planning to get pregnant are recommended 5mg a DAY
Canadian fortification outcome; why was the RR reduction of NTD’s different across regions?
Mandatory folic acid in flour (1998) cut NTD rates by up to 38 per 10,000 births in provinces like Newfoundland.
Regions with high risk stood to benefit the most from mandatory fortification
low-risk areas already had lower MTD prevalences to begin with; they were ‘closer’ to the ‘true effect’ = smaller RR reduction %
Targetting Population vs. Targetting High-Risk Peoples
Small risk reduction for each individual but large population effect (fortification)
versus
large individual benefit but limited reach (targeted supplements).
What is WHO’s Optimal RBC folate level/cut-off?
≥905 nmol/L,
associated with minimal NTD risk
Why is it unlikely for women in NZ/ people in general to get 260 µg natural folate?
Obtaining 400 µg folate/day from food alone is difficult; natural folate has low bioavailability.
folic acid supplements MORE BIOAVAILIBLE
why folic acid made MANDATORY in 2023
NZ health survey in 2014/15 had a RBC folate 748 nmol/L cutoff; what was the % of NZ women below this MINIMUM cut-off?
The level below which NTD risk begins to rise 16 % of NZ women fall below this threshold.
What are the two major conditions
spina bifida: affects the spinal cord (leads to paralysis, incontinence, cognitive issues)
Anencephaly: affects the brain, does not develop properly or fully (fatal)
risk factors for Spina bifida and Ancephaly
Risk factors:
low folate/b9
genetic mutations, maternal obesity, diabetes, anticonvulsants
What is the size of the problem? ( NTD)
Global: ~260,000 babies affected/year (live births)
NZ: 10.2 per 10,000 pregnancies (stillbirths, livebirths and terminations)
Māori: 4.5
pasifika: 4.1
Pakeha: 2.8
logistical spina bifida costs/burdens
(aside from healthcomplications /wellbeing)
21 operations
expensive; close to $1 million
178 days in hospital minimum/aver
Does Folic Acid Prevent NTDs
Yes!
MEDICAL RESEARCH COUNCIL:
Folic acid supplementation reduces NTD; no demonstrable harm from folic acid supplementation
START BEFORE PREGNANCY; if you’re pregnant, it’s likely too late.
4000 µg folic acid/day reduced recurrence of NTDs from 3.5% to 1.0% (RR = 0.28)
CHINA STUDY: 79% reduction in high-risk region for NTD
dose-response relo; Folate increases, NTD decreases
Minimal effect in low-risk region, showing background folate status matters
low risk region has higher vege intake; wealthier, longer growing seasons
What Influences Folic Acid’s Impact on NTDs
Timing: taking folic acid supplements before contraception
58% of women with planned pregnancies took folic acid before contraception; 9% of women with unplanned pregnancies
Access & health literacy: influenced by SES, planning and Awareness
Why people in wealther areas have lower prevalencies of NTD’s?
Higher consumption of folic acid (B9); higher consuption of fresh vegetables (which can be expensive year-round)
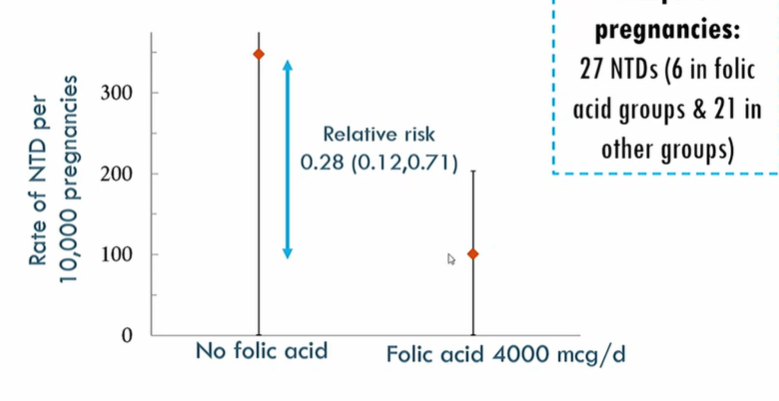
Medical research council & folic acid RCT
RCT WITH 33 CENTRES, 7 COUNTRIES
Risk of 1817 women (Genetic of previous NTD risk) having a pregnancy with NTD
4000 µg folic acid/day reduced recurrence of NTDs from 3.5% to 1.0% (RR = 0.28)
Case control study for folate cut-off…. (WHO’s baseline)
as folate increases, NTD risk decreases (graded reduction)
if women have above 906nmol of folate = lowest risk of NTD
is the WHO cut off
Two ways to increase RBC folate
target high-risk individuals: (Large change in individual risks, small change in population prevalence)
target populations: (small change in individual risks, large change in population prevalence)
IF you fortify folate on a population-wide level, what are the GOOD effects?
folic acid supplementaion (800mcg) reduced risk of stroke in 21% of adults with hypertension in China
IF you fortify folate on a population-wide level, what are the bad effects?
high doses of folic acid MASK B12 DEFICIENCIES
b12 deficiency causes irreversible neuro damage, anaemia is a symptom (megaloblastic anaemia)
folic acid will cure anaemia, but not b12 deficiency
CANCERS
Antifolate drugs are used to treat some cancers
POSSIBLE RISKS associated with folic SUPPLEMENTS
B vit trialist collaboration:
NZ Supplementation Recommendations: Folic acid
MoH: 800 µg folic acid/day from at least 4 weeks before conception to 12 weeks after
FORTIFICATION:
Access: prescription or OTC from pharmacy
ways to increase folate intake
Naturally rich Folate diet:
NZ low intake of dark green leafy vege
mandatory fortification: bread, flour
supplements: prescription or OTC from pharmacy
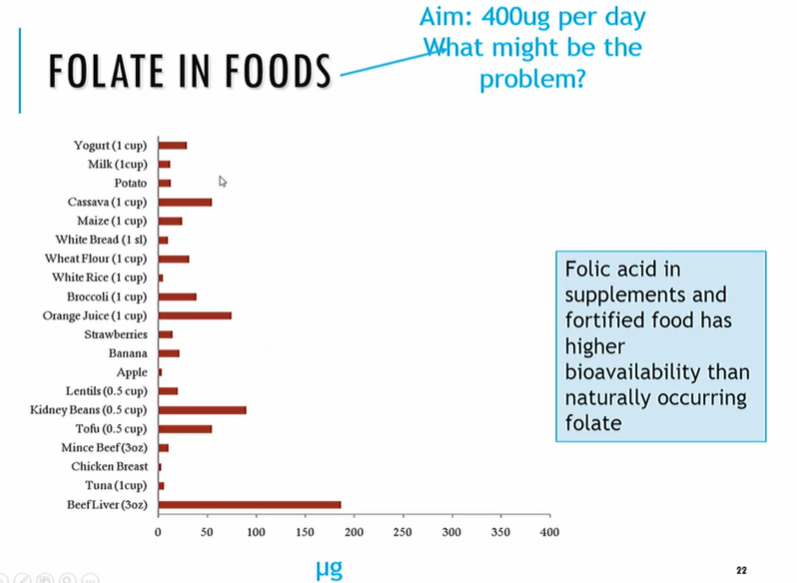
hard to get good levels of folate because…
low bioavailibility; folic acid supplements and fotified foods have higher bioavailibility than naturally occuring folate in dark leafy greens, or dairy and animal products
pros of supplementation (b9 800mcg/day)
correct dosage at correct time (pre-contraception or pre-pregnancy)
no risk posed to non-target population
cons of supplementation (b9 800mcg/day)
conscious choice that must be made; health literacy and awareness required
cost barrier, questions for SES and inequitable access/results:
NTD presence in Māori vs Pasifika vs pakeha women = 4.58, 4.09 and 2.81 per 10,000 births
fortification pros (b9)
reaches the most women; equitable choice for reduces across all populaiton groups despite awareness, health literacy and access.
fortification cons (b9)
only uses a low low level of b9 in fortification to prevent any risk to wider non-target population for b9.
very very few people would have 400mcg
NZ SUPPLEMENTATION RECCOMENDATIONS (FOLATE)
low risk women: 800mcg/day (prior conception, & 12 weeks after)
women at risk of NTD: 5000mcg (5mg)/day
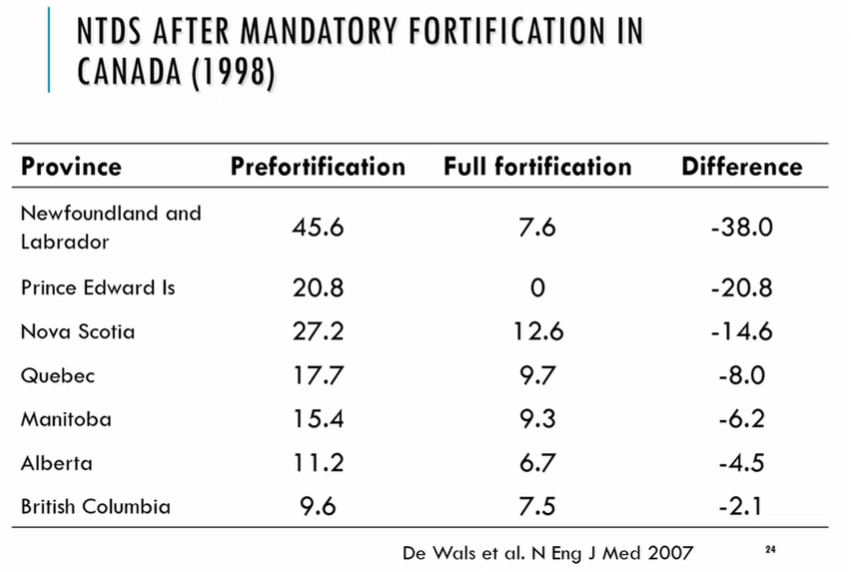
results of canada’s fortification (b9) in 1998
all types of flour, cornflour, pasta
e.g newfoundland vs British Columbia; Newfoundland
places that already had low risk had minimal/little change after fortification, whereas high-risk areas saw the greatest changes because they had the greatest deficiencies.
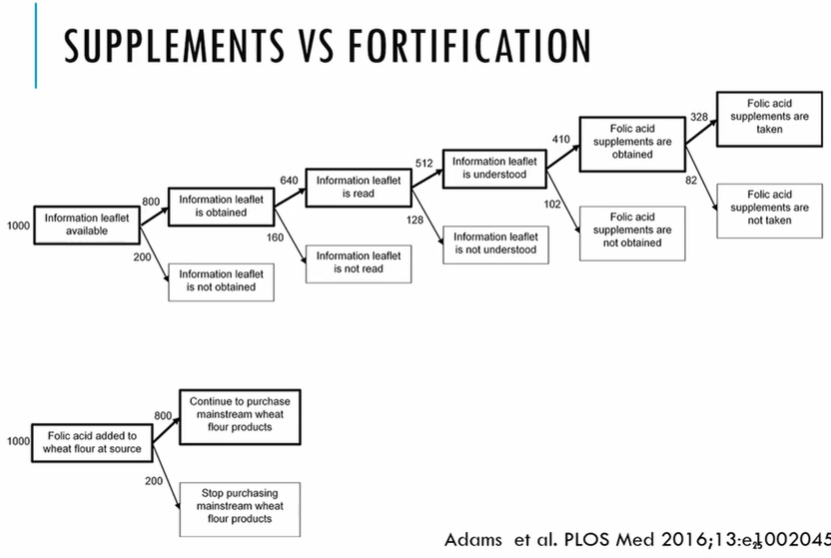
supplementaion vs fortification
Fortification is a ‘one-stop’ solution; you just put it in the flour/bread people buy.
Supplementation means people must have
The health information available
actually obtain the health information
read/engage with health information
understand the health information (awareness)
decide and get supplements
actually take and adhere to supplements
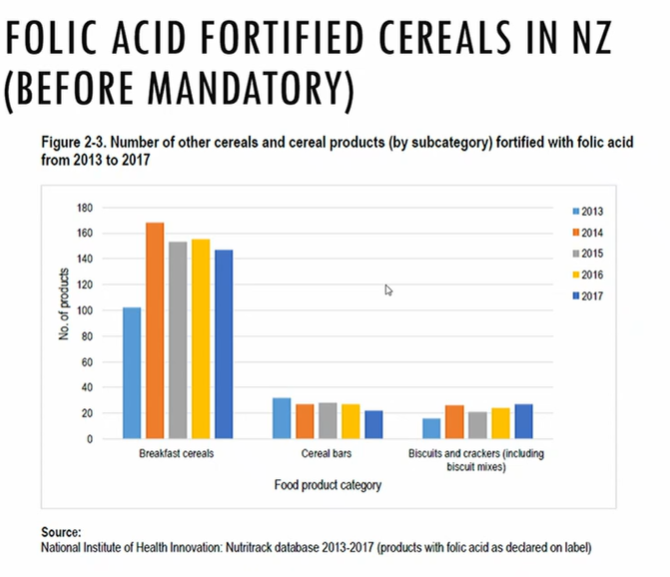
timeline of NZ folic acid (b9) Fortification
Timeline:
1996: Voluntary fortification allowed (e.g., cereals)
2009–2012: Mandated plan paused (Australia went ahead)
2023: Mandatory fortification of non-organic wheat flour for bread (2–3 mg/kg) now required
Mandatory fortification
reduces prevalence of NTD
efficacy/evaluation affected by background rate of NTD’s, factors of wealth, ses, access to healtcare (etc) on folate status
NTDS in NZ
10.6 per 10,000 total births;
4.6 for Māori
4.1 for Pasifika
2.8 for Pakeha
folate status of nz adults
2008/09 Nutrition survey:
906nmol/L was ideal;
NZHS 2014/15:
mean RBC folate (before fortification in NZ) 544nmol/L
below the ideal cut-off of 748nmol/L
16.2% below the minimal cutoff
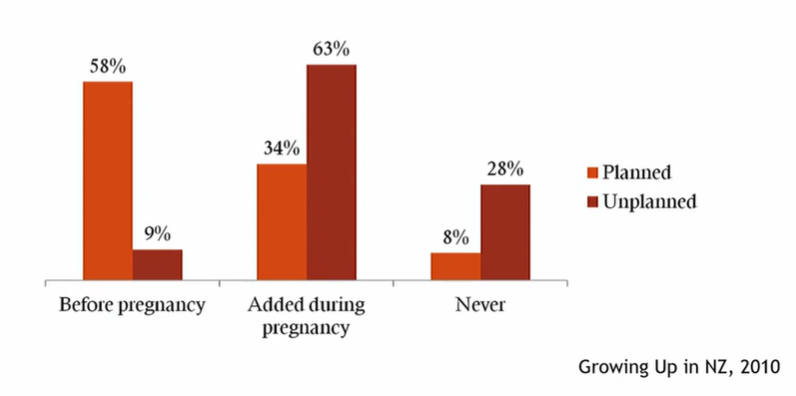
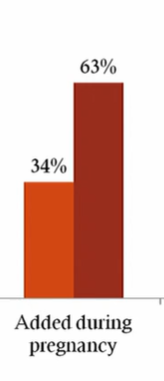
prevalence of folate supplementation before pregnancy
Growing Up in NZ study (2010) found that 58% of women with planned pregnancies used folic acid supplements before pregnancy VS 9% of those with unplanned pregnancies.
issues of getting women to use folic acid supplements
Folic acid supplements must be taken prior to conception through 12 weeks post-conception.
NZ a high rate of unplanned pregnancies
Women (63% unplanned and 34% planned) added folate during pregnancy, when it’s actually too late.
what year did NZ make folate fortication mandatory?
2023 (delayed 2009, voted not to in 2012)
non-organic wheat flour for BREAD MAKING
decided/introduced 2021, 2023 was just the ‘must be fortified by’ cut-off.
VOLUNTARILY: Certain Breads and breakfast cereals were voluntarily fortified
2023 increased this significantly
Why was bread-making non-organic flour fortified? why not breads as well?
because maeks ti even across a population, starts at the actual source so fortification levels are same across bakeries, stores, in the actual bread made
logistical reasons
harms of high-dose folic acid supplements?
Possible harms: High-dose folic acid can mask B12 deficiency and has uncertain links to cancer risk, though overall risk appears low at standard doses.
pros of fortificaiton AND supplementaiton
Fortification: equitable, passive uptake, benefits unplanned pregnancies; may underdose individuals needing higher amounts.
Supplementation: targeted and dose-specific; requires planning, awareness, and access.
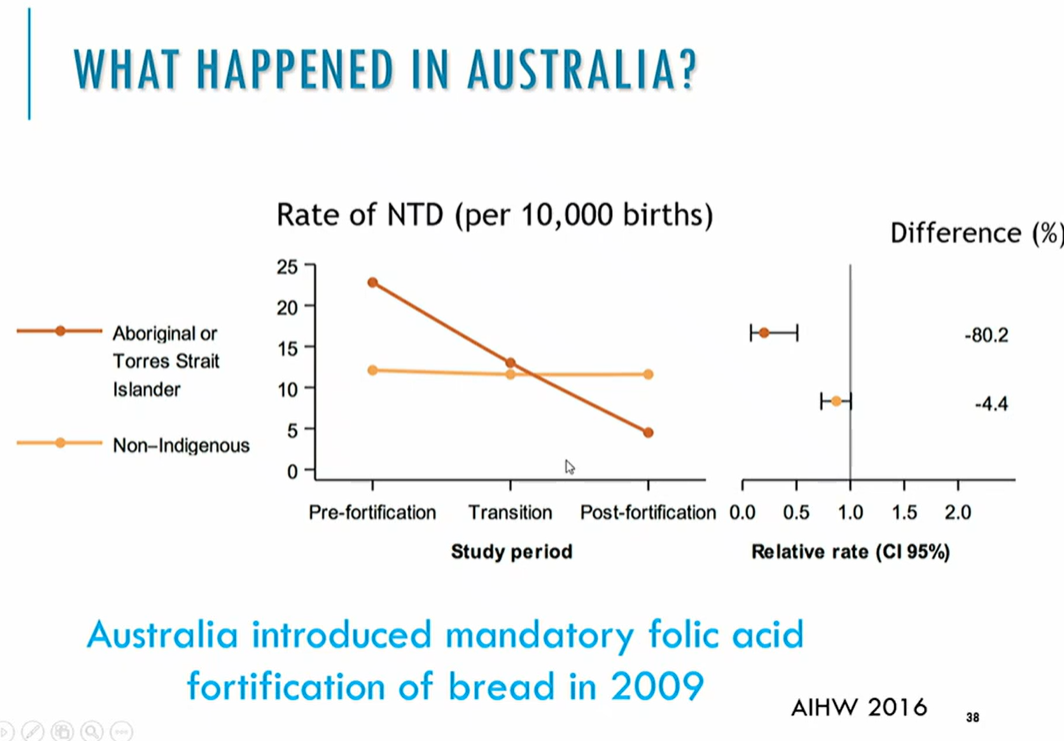
fortificaiton results in australia
a bit like canada; significant risk reduction in high-risk, small/non in low-risk