ETC8363-2020 BCCCP-Infectious Disease I
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
121 Terms
Individual risk factors for VAP
Chronic lung disease or acute lung injury
trauma (chest trauma or TBI)/ Burns
Re-intubation
aspiration
coma
How long after intubation does VAP happen?
>48hrs after endotracheal intubation.
VAP is caused by monomicrobial or polymicrobial pathogens?
Both, rarely viral or fungal.
Risk factors for MDROs Causing VAP?!?!
Prior IV ABX in preceding 90 days
Acute Renal Replac Therapy (RRT) before VAP onset
5 or more days of hospitalization prior to onset of VAP
Increased sputum production.
Septic Shock at time of VAP
ARDS preceding VAP.
How to prevent VAP
1.Avoid or limit duration of ET Intubation
2. Minimize duration & deep level of sedation ( to promote assessment of readiness to extubate)
3. Maintain/improve physical conditioning while on MV
4. Minimize pooling of secretions above ET tube cuff.
5. Elevate head of bed at least 30 degrees.
6. Maintain integrity of MV circuit.
Clinical Signs and Symptoms of pneumonia include?
new or changing infiltrate on chest X-ray AND 2 or more of the following....
Elevated WBC
Fever (>100.4*F/38*C)
Macroscopic purulent sputum production
Impaired or worsening oxygenation
Non-invasive techniques for obtaining resp. tract cultures for VAP are...
Obtained from what part of lung?
What kind of results does is yield?
Tracheal aspirate from ET or Tracheostomy tube
obtained sample from upper airway secretions
Yields semi-quantitative results.
Invasive Techniques for obtaining resp. tract cultures in VAP are?
obtained from where?
What king of results does it yield
Blind Catheter-directed/Bronchoscopic BAL
distal sample of lung lobe/segment (uses saline lavage) yields significant QUANTITATIVE results. (if <10,000 CFU/mL = d/c ABX)
Bronchoscopic protected specimen Brush (PSB): Distal sampling of specific bronchial segment significant QUANTITATIVE growth. <1,000 CFU/mL= d/c ABX
Diagnostic Strategy for VAP includes what?
Clinical Suspicion + NON-INVASIVE sampling = SEMI-quantitative results
and not invasive sampling which yields quantitative results.
ALL patients with suspected VAP should receive a ABX against what organisms.
MSSA and P.Aeruginosa
At least give one agent for each in all pts.
Vanc + Cefepime
In patients with VAP, when do you need to have double pseudomonal coverage (with different MOA)?
MDRO risk factors
ICU antibiogram with >10% gram(-) isolates resistant to agent used as monotherapy
ICU ABX susceptibility is unavailable.
When should you include MRSA coverage for VAP?
MDRO risk factors
ICU MRSA prevalence is >10-20% S. Aureus
Prevalence of MRSA is not know.
When treating VAP patients
WITHOUT MDRO risk factors
SINGLE-Antipseudomonal agent with 90% or more activity
MRSA prevalence is < 10-20%.
What is the most likely pathogen and
What is the treatment?
P. Aeruginosa
S. Pneumoniae
Haemophilus Influenzae
A/B-hemolytic Strep
MSSA
Gram Neg Bacilli (GNB, like E.coli, Klebs, Enterobacter, Proteus, serratia)
Give:
Cefepime, Imi/meropenem, Levofloxacin, Zosyn
Ceftriaxone is a reasonable agent for empiric manage-
ment of early onset VAP with activity against common
pathogens
When treating VAP patients
Patients WITHOUT MDRO risk factors
Single antipseudomonal agent has <90% activity
and/or MRSA prevalence is > 10-20%
What are the likely pathogens and how do we treat them?
P. Aeruginosa
S. Pneumoniae (all same but + /MRSA)
Haemophilus Influenzae
A/B-hemolytic Strep
MSSA
Gram Neg Bacilli (GNB, like E.coli, Klebs, Enterobacter, Proteus, serratia)
Give:
Antispeudomonal B-Lactam
Aztreonam, Cefep/ceftazidime, imi/meropenem, Zosyn
++PLUS++
Antispeudom FQ ///or/// Aminoglyco
( Levaquin/Cipro) //////// ( ami/gent/tobramycin)
+/- MRSA ( Vancomycin or Linezolid)
Patients with MDRO what are the likely pathogens for VAP and how do we treat them?
P.Aeruginosa
MRSA
Acinetobacter
RESISTANT-GNB ( ESBL)
Stenotrophomonas Maltophilia
Give:
Antispeudomonal B-Lactam
Aztreonam, Cefep/ceftazidime, imi/meropenem, Zosyn
+++PLUS+++
Antispeudom FQ ///or/// Aminoglycoside
( Levaquin/Cipro)______________________( ami/gent/tobramycin)
+++PLUS+++
MRSA ( Vancomycin or Linezolid)
Which ABX cannot be used for MRSA VAP and why?
Daptomycin due to direct inhibition of daptomycin by lung surfactant.
True of False:
In VAP, monotherapy with a beta-lactam to treat P. Aeruginosa can be used in all patients when beta-lactam shows great susceptibility to organism?
FALSE:
Even if beta-lactam has great suceptibility you would not do monotherapy with beta-lactam if pt is Immunocompromised, has septic shock, or at high risk of dying. In these patients you would do
Beta-Lactam + Antipseudomonal FQ or/aminoglycoside.
After septic shock has been resolved in IMMUNOCOMPETENT pt then you can scale down to monotherapy.
What ABX do you give for VAP with Acinetobacter spp?
Imi/meropenem (Amp/sulbactam as an alternative)
What ABX do you give for Stenotrophomas Maltophilia?
Sulfa/Trimethoprim (Bactrim)
How long should you treat VAP for with ABX?
7 days ( definitive for ALL patients)
Risk Factors for CLABSI?
1. Excessive manipulation before/after insertion
2. Internal jugular or Femoral insertion site
3. Microbial Colonization at insertion site/ catheter hub
4. Neutropenia
5. Prolong duration of catheterization
6. Prolong hospitalization prior to catherization
7. TPN
Where do CVC catheters end?
Placed in ...
Inferior/Superior/Distal Vena Cava
Right Atrium
Pulmonary artery
(usually short term catheters)
what is the most commonly used CVC lumen?
Singe and Triple lumen.
What type of catheter is a PICC line?
Peripherally Inserted Central Catheter (PICC)
Short-Medium term central catheter
How does the CDC define a CLABSI with respect to time from insertion?
Infection occurring from 2 days after insertion up to one day AFTER catheter removal.
CDC : A CLABSI is defined/classified how?
Due to ...
Recognized pathogen: culture from one or more blood cx ( and org is not related to another infection at different site. like change in chest x-ray)
Common Commensal organism: Diptheriod, Bacillus, Coag(-) staph, Viridans Strep. ( this is from two or more blood cultures drawn on SEPERATE occasions AND organism is not related to another infection at different site)
+ At least ONE of the following...
Fever > 100.4F (38C), Chills, or Hypotension.
How does the IDSA define CLABSI?
bacteremia/fungemia in pts with intravascular device:
*>1 (+) Peripheral Blood cx (same organisms growing from percutaneous blood cx + CVC tip/catheter hub
(or catheter cup/tip + peripheral vein)
*clinical manifestation ( fever, chills, hypotension)
*no additional source of infection other than catheter.
like change in chest x-ray suspecting pneumonia.
CLABSI are monomicrobial or polymicrobial?
What type of organisms?
MONOmicrobial
Coag-neg staph ( Staph epi)
Staph Aureus
Candida (less common)
Enteric Gram Neg Bacili: E.coli, Klebs, Enterobacter
(less common)
Candida-CLABSI is more common in what type of pts?
TPN
Prolonged exposure to broad spectrum ABX
Hematologic malignancy
Stem cell/Solid organ transplant
Catherization at femoral site.
Colonization at several sites with candida.
What three organisms increase the suspicion of CLABSI if found in two blood samples?
(+) for Staph Aureus, Coag (-) staph epi, candida
(if NOT ATTRIBUTABLE to another source of infection)
CLABSI. How do we treat?
Fever = most sensitive
Inflammation/purulence @ insertion site= most specific
ALL pts should be considered for cath removal, if cath still needed then insert to DIFFERENT site. but GET CULTURES PRIOR TO REMOVAL.
Treat for possible resistant coag(-) MRSE (staph epi)
Treat for possible resistant coag (+) MRSA (staph Aur)
Give : Vancomycin or Daptomycin (alone)
If possible MDRO (pseudomonas): Cover ALL
--Vanc (MRSA/MRSE)+ cefepime+ tobramycin (double anti-pseudomonal coverage)
14 days after initial negative blood culture.
!!! NEVER LINEZOLID for empiric CLABSI therapy it has WORSE pt outcomes !!!
If pt has CLABSI along with high risk of MDROs how does that change our treatment?
you would add coverage agains gram-neg bacilli
How do we treat Candida-CLABSI?
Echinocandins
(anidulafungin, caspofungin, micafungin)
Fluconazole is okay if pt does not have recent exposure and low prevalence of non-susceptible species.
In CLABSI the duration of ABX therapy is relative to what?
1st day of negative blood culture (treat for 7-14 days uncomplicated gram-neg CLABSI)
What makes a CLABSI "complicated" how does that change our treatment?
Endocarditis (treat for 4-6 wks)
Immunosupression / Diabetes(S. Aureus only)
Chronic Intravascular hardware. (treat for 4-6 wks)
Osteomyelitis(treat for 4-6 wks)
(+) blood cx for > 72hrs from initiation of ABX
Septic thrombus / Thrombophlebitis (treat for 4-6 wks)
you would remove catheter and treat specific pathogen for 4-6wks ( 6-8 wks if osteo)
How do we treat UN-Complicated CLABSI due to coagulase (-) staph EPI?
Consider cath removal
or
If cath remains in place give ABX systemically for 5-7 days +/- ABX lock therapy. for STAPH EPI!
How do we treat UN-Complicated CLABSI due to coag(+) Staph Aureus?
1.Remove cath
2. Give ABX against MSSA or MRSA for 14 days after first negative blood culture.
MSSA: Nafcillin or 1st gen cephalosporin-cefazolin
MRSA: Vanc/Dapto/Linezolid/ Bactrim
T/ F:
If pt has a (+) bacterial growth from catheter tip/hub but (-) blood culture from peripheral vein they should not get ABX?
FALSE:
you would still give ABX towards bacterial for 5-7 days and monitored for s/sx of infection and consider repeat blood cultures.
What are the risk factors for developing SEVERE influenza (requiring hospitalization)
Chronic respiratory/ metabolic illness.
Immunosupression (Disease or pharmacotherapy)
Pregnancy
Age > 65 yrs old
What are the most common complications of SEVERE Influenza are?
Hypoxemic respiratory failure
Bacterial Pneumonia
ARDS
SEVERE Influenza usually caused by strain A & B
How does Influenza spread from person to person?
Droplet transmission
Signs & Symptoms of Influenza?
Fever(3-5 days)
Myalgias (3-5 days)/ Malaise (>2wks)
Headaches
Dry cough
Pharyngitis
Rhinorrhea
How is Influenza diagnosed?
upper resp tract sampling via nasal washing
nasopharyngeal swab (rapid and reliable)
lower resp tract culture (sputum or BAL)
(Dx tests > 5 days beyond onset = false negative results)
Antiviral therapy for flu should be initiated when?
within 48hrs from onset of symptoms
(if in hospital then giving antivirals past 48hrs may also benefit to a lesser extent)
What are the mainstay medications for Influenza and how do they work?
Neuraminidase Inhibitors: Inhibit viral neuraminidase = decrease release of post-replication viral partivles "virions" = limit spread to other tissues.
What are some type of Neuraminidase Inhibitors and what is their niche in treating Influenza
Oseltamivir: oral capsule or powder suspension ( can be given via Oro/Nasogastric tubes but needs liver to convert to active form.
Zanamivir: Inhaled drug via Diskhaler. (not via MV)
IV formulation also available via clinical trial participation in pts who cannot tolerate/absorb oseltamivir due to gastric stasis, malabsorbtion, GI bleed.
Peramivir: only in pts >18yrs old with acute & uncomplicated flu. ONE TIME 15min infusion.
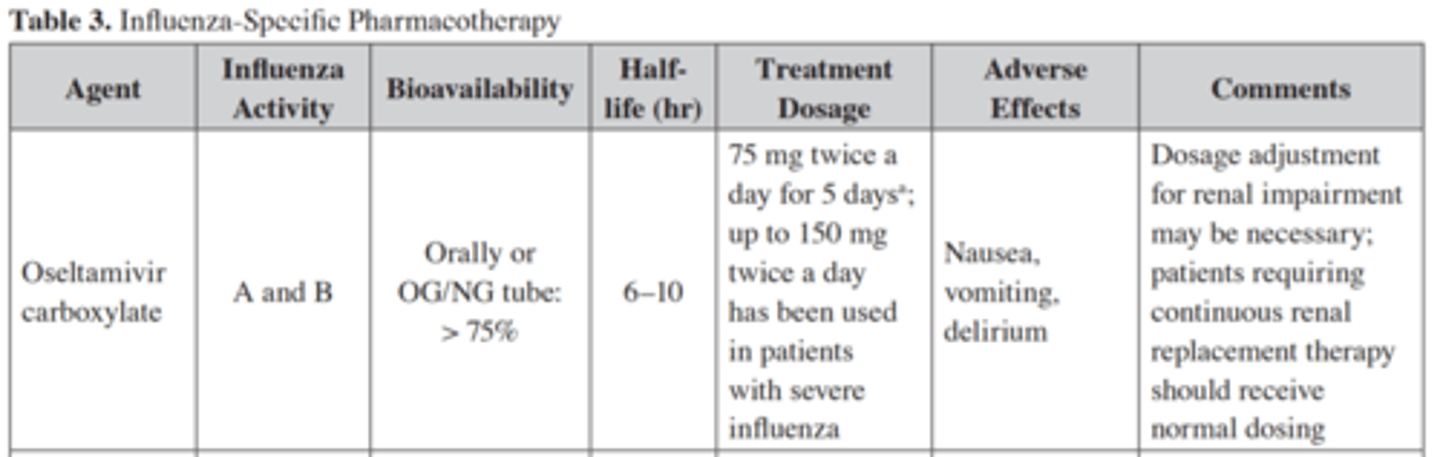
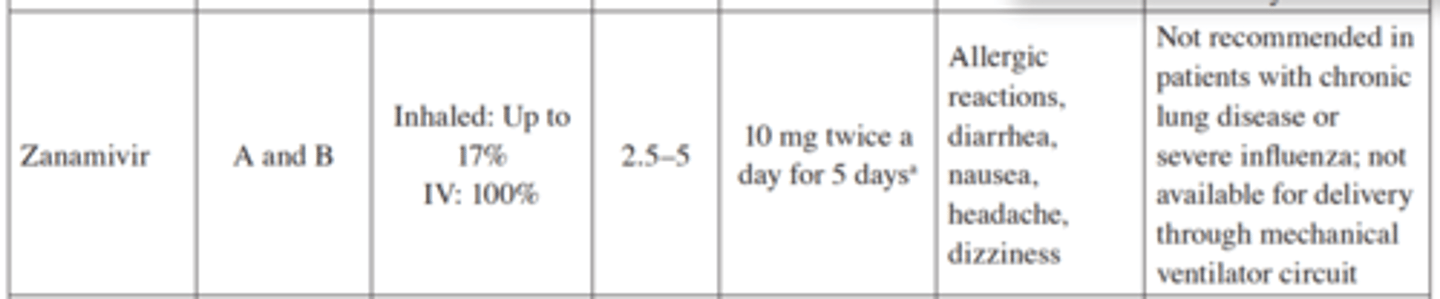
Oseltamivir :
Activity against which strain?
Treatment dose?
ADE?
Influenza A & B
75mg BID x 5 days (150mg BID for severe Flu)
N/V , delirium
Peramivir
Activity against which strain?
Treatment dose?
ADE?
Influenza A&B ( limited data for B)
One time 600mg IV infusion over 15 min.
Diarrhea, Hypersensitivity rxn, Delirium
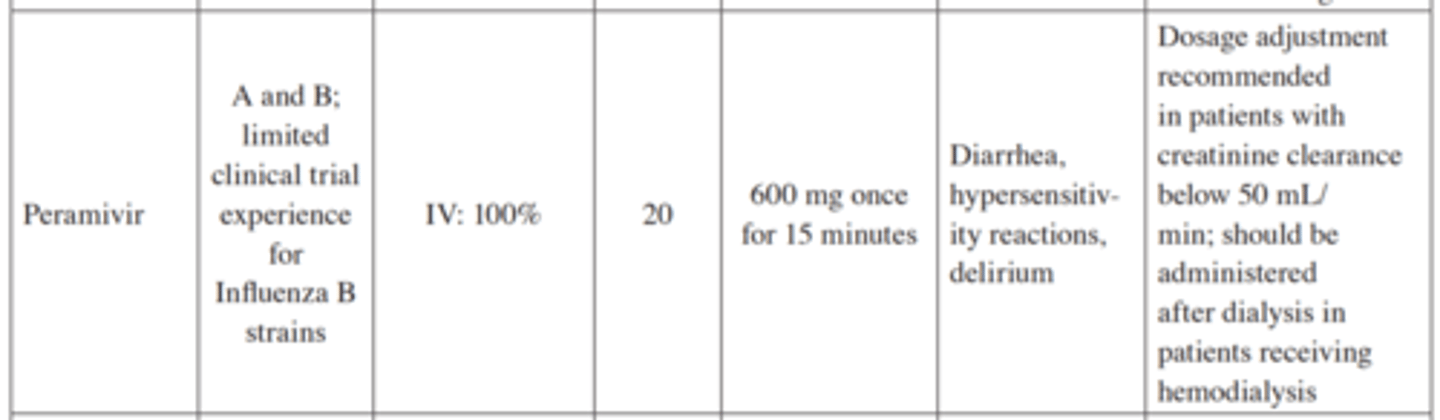
Zanamivir
Activity against which strain?
Treatment dose?
ADE?
Flu A & B
10mg BID x 5 days (Diskhaler inhalation or IV)
Allergic rxn, diarrhea, N/V, HA, Dizziness
Amantadine
Activity against which strain?
Treatment dose?
ADE?
Flu A only ( even then there is high resistance to it)
100mg BID
N/V, Insomnia, Lower Seizure threshold, Anti-cholinergic effects
CDC defines a UTI as.......
Having AT LEAST one of the following:
1. Fever >100.4*F
2. Suprapubic tenderness
3. Costovertebral angle pain or tenderness
+
__(+) urine cx of >105 CFU/mL ( no more than 2 organisms)
or
__(+) dipstick for Leukocyte esterase / Nitrite
__Pyuria (urine specimen > 10 WBCs in unspun urine)
__Organisms seen on Urine Gram Stain and (+) Urine cx for 103-105 CFU/mL for no more than 2 organisms.
CDC defines a CAUTI as
UTI in a patient who has a catheter for > 2 days
( or UTI in a pt whos catheter was removed 1 day prior to infection)
IDSA defines CAUTI as.....
UTI signs/sx with no other source of infection AND >103 CFU/mL of ONE bacterial species from catheter urine sample ( or midstream-voided sample from pt who has had catheter removal within 48hrs)
Short term Catheters are usually poly or mono microbial?
Short term cath= monomicrobial
Long term caths= form biofilms = polymicrobial.
What is the most prevalent pathogen in CAUTIs?
33%: E. Coli
33%:
Enteric GNB ( Klebs, proteus, Enterobacter)
Non-lactose fermenting GNB ( P. Aeruginosa)
Gram(+) Cocci: Enterococcus, MSSA, MRSA, MRSE
33%: Candida
How do we prevent catheter-associated ASYMptomatic bacteruria
and CAUTIs?
reduce use of urinary catheters ( restrict use to patients with clear indications and removing them as soon as possible)
How long do we treat CAUTI for?
7 days if the pt has signs of improvement < 72hrs after appropriate ABX.
14 days if pt has signs of improvement > 72hrs after appropriate ABX.
How often should you replace a catheter?
Catheters in place for > 2 wks should be replaced and urine sample should be obtained from newly inserted catheter port ( if we pull from old catheter bag = high risk for colonization)
confirmatory urinalysis from old catheter is not needed if catheter has been in place for < 2 weeks so start ABX if pt presents with infection.
What is the most common type of complicated intra-abdominal infection?
Appendicitis.
How does the IDSA define a COMPLICATED intra-abdominal infection?
Infection that extends BEYOND the hollow viscus origin into the peritoneal space creating abscesses or peritonitis. (Spillage of viscus fluid/ flora into peritoneal cavity)
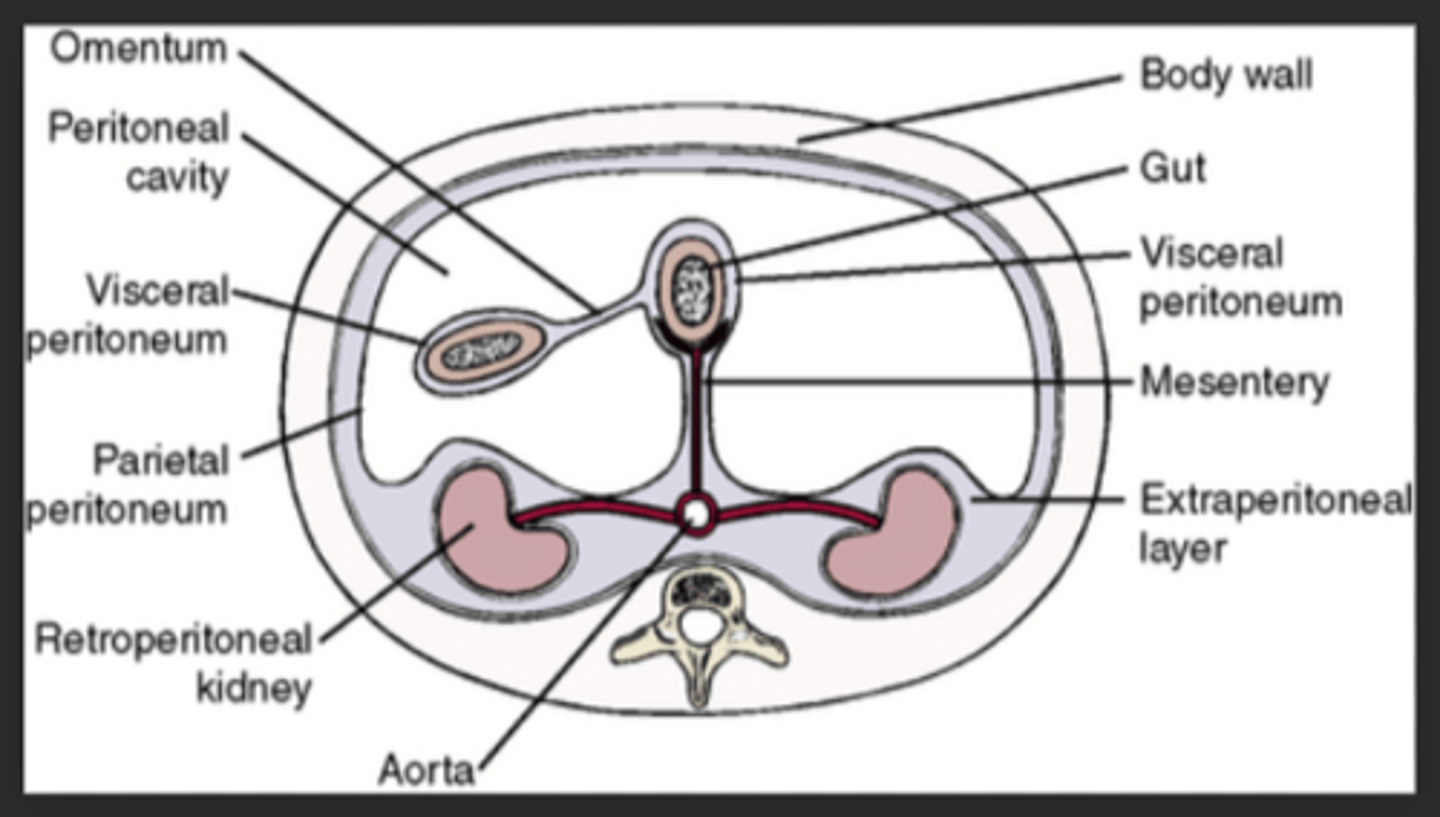
What is PRIMARY peritonitis?
Primary: (SPONTANEOUS Bacterial Peritonitis, Diffuse in nature) related to bacteria translocation from small bowel overgrowth and not peritoneal disruption or organ perforation.
What is SECONDARY peritonitis?
leakage of intraluminal fluid and microorganism 2ndary to macro/micro-perforation of GI tract.
Can be diffuse or localized to an organ.
Causes: direct trauma, ischemia, thrombosis, ulceration, malignancy, and anastomic leak.
What is harder to treat between HA-Intraabdominal infection versus community acquired abdominal infection and why?
HA is harder to treat because those arise from resistant and nosicomial pathogens.
Primary Peritonitis is poly or monomicrobial?
What is/are the pathogen(s)?
Primary peritonitis (translocation across diaphram/small bowel) usually MONOmicrobial
-S. Pneumoniae
-E. Coli
-Klebs.
Secondary Peritonitis is poly or monomicrobial?
2ndary involves leakage from a source. therefore it is usually POLYmicrobial and realted to origin of leakage.
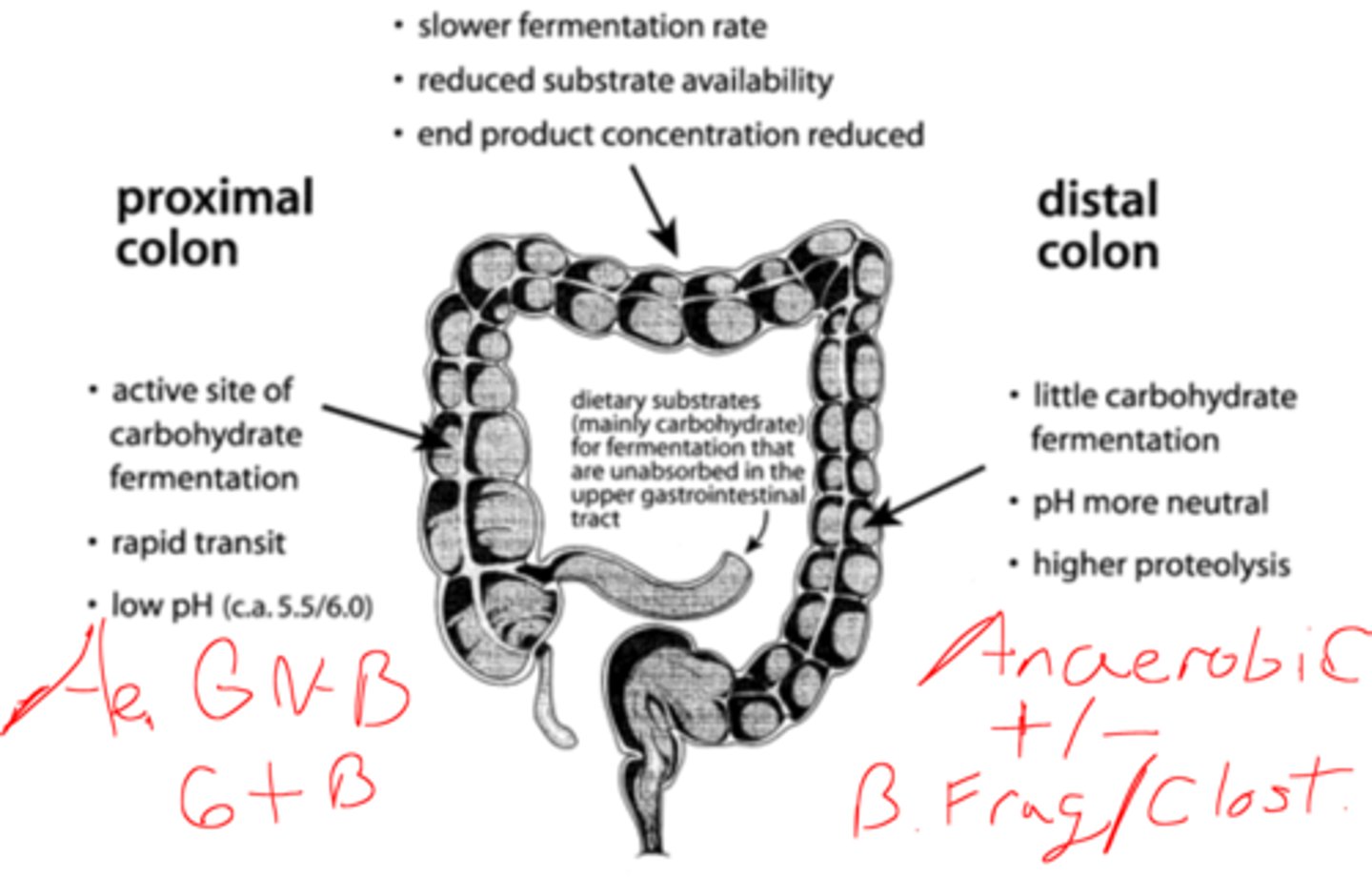
2ndary peritonitis with leakage from Gastric/duodenal secretions have which type of bacteria?
usually sterile or with limited gram(+) or candida
2ndary peritonitis with leakage from Proximal small bowel have which types of bacteria?
1 Aerobic gram-negative bacilli
( E.coli, Klebs, Proteus, Enterobacter)
2 Aerobic gram- positive bacteria
( S. Aureus, strep, enterococci)
2ndary peritonitis with leakage from distal small bowel / large bowel have which type of bacteria?
(Proximal small bowel bacteria + pos/neg Anaerobes)
All the 2ndary proximal small bowel bacteria
--Aerobic GNB: E.Coli, Klebs, Proteus, Enterobacter
--Aerobic gram(+) bacteria: S. Aureus, strep, enterococc
..........................................PLUS......................................................
Anaerobic gram (+) & (-) bacteria :
--Bacteroides. fragilis
--clostridium species (not C.diff)
What is tertiary peritonitis?
-Peritonitis from either primary or secondary further complicated by management strategies such as:
--malnutrition
--anatomic disruption
--antimicrobial therapy.
-Either Primary or Secondary Peritonitis that persists for > 48hrs after management of either peritonitis.
How do you diagnose an Intra-abdominal infection?
along with S/Sx of rapid onset abd pain + tenderness pt can also experience anorexia, N/V, +/- fever, emesis, tackycardia, tachypnea.
May also need radiographic eval/ ultrasound/ CT/ or in some cases contrast studies for post-op drains to assess for anastomic integrity.
How does the surgical management of peritonitis differ from diffuse to local peritonitis?
Diffuse peritonitis= diversion or resection recommended
Focal peritonitis= percutaneous abscess / fluid drainage.
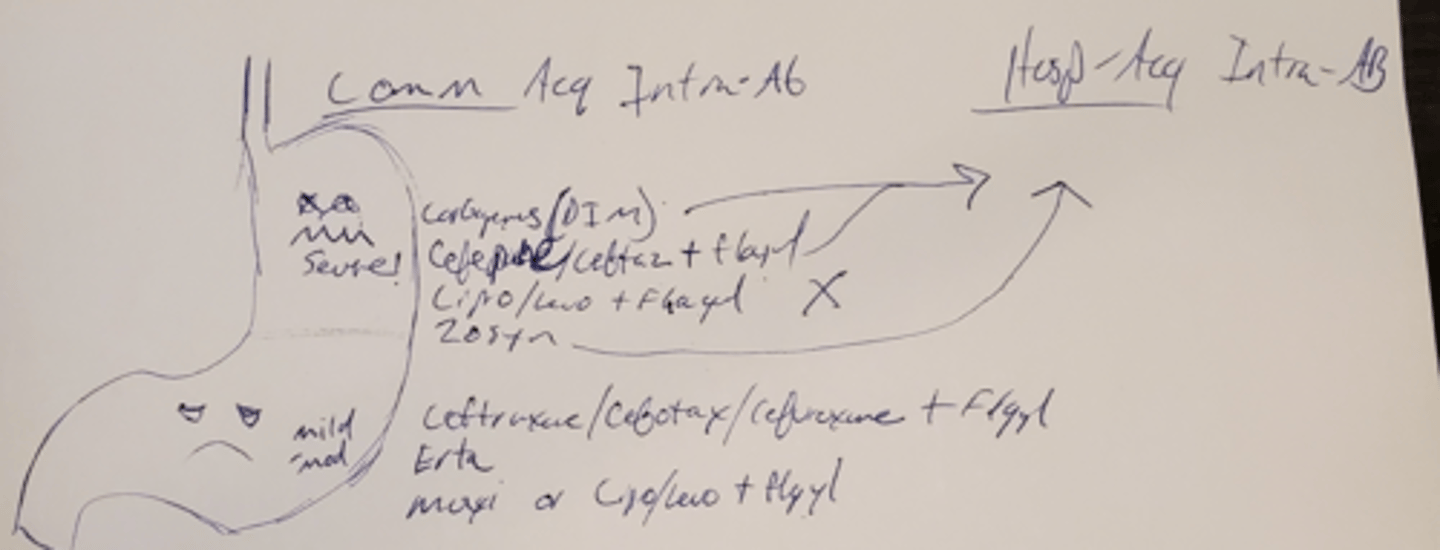
What organisms are seen and what ABX do you use in Community Acquired (mild - moderate) Intra-abdominal infections?
Aerobic & Facultative EGN bacilli (E. Coli, Klebs) are the most common in somewhat stable pt.
Enteric Strep
Obligate anaerobic (sml bowel/ Appendiceal/colonic source)
Ceftriaxone/Cefotaxime/Cefuroxime + Flagyl
Ertapenem
Moxifloxacin ( alone) or Levo/Cipro + Flagyl
Tigecycline (some studies show increased mortality)
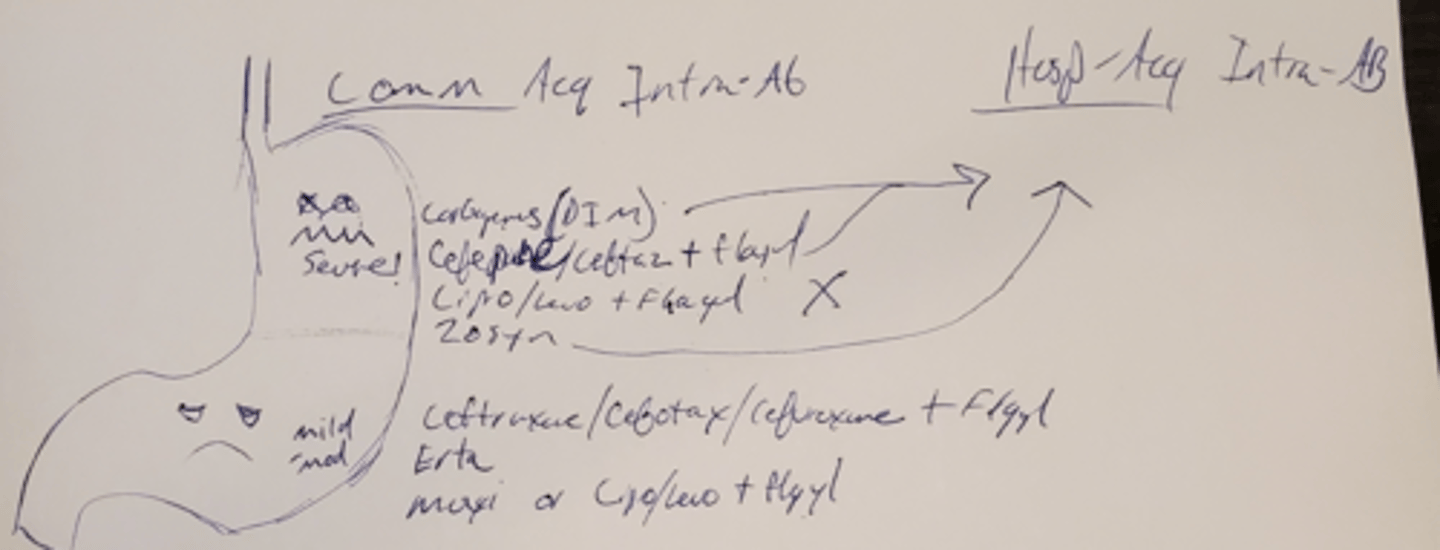
When is a Community Acquired intra-abdominal infection considered "High in Severity" and how does that change therapy?
High in Severity:
physiologic disturbance ( Septic Shock +\- pressors)
Older in Age
Immunocompromised state
Delay/High probability of failure in primary control
Broaden coverage: MDRO (pseudomonas), enterococci, oblgte anerob
Carbapenems ( dori, imi, mero) NOT ERTApenem.
Cefepime/ Ceftaz + Flagyl
Cipro/Levofloxacin + Flagyl
Zosyn
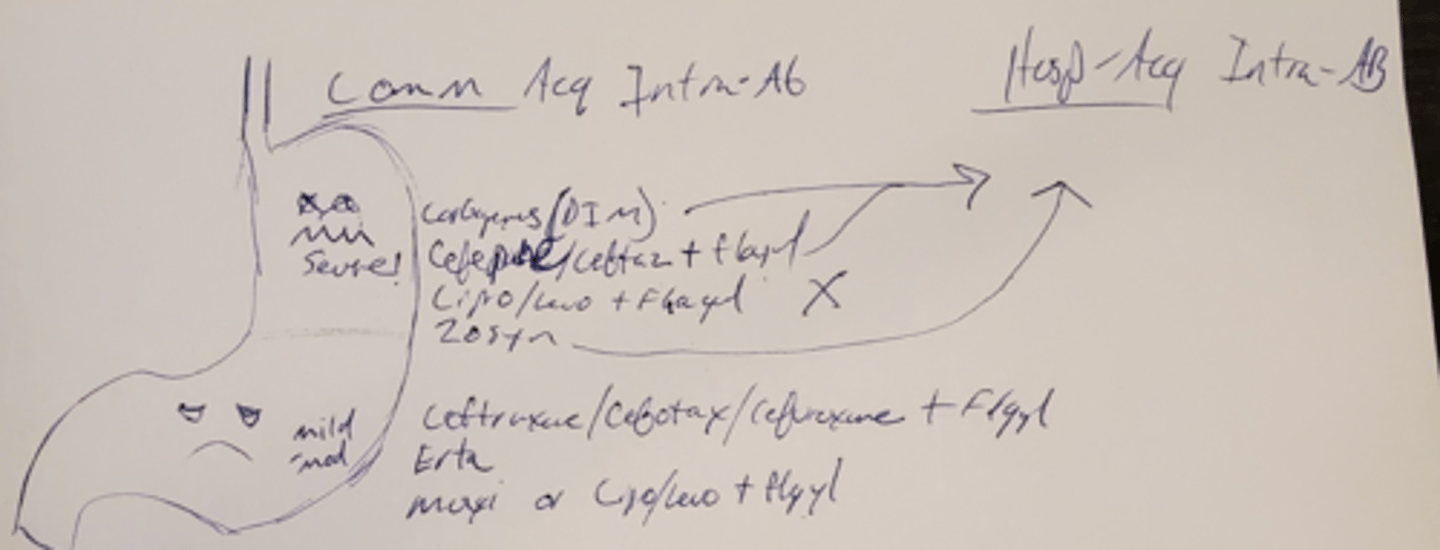
How do you treat HEALTHCARE associated Intra-Abdominal Infections?
Start with Broad Spectrum ABX. (kinda like Community AQR SEVERE Intra-abd Infec but without cipro/levof)
Main focus here: P. aeruginosa and obligate anaerobes
Broaden coverage to include MDROs
Carbapenems ( dori, imi, mero)
Cefepime/ Ceftaz + Flagyl
Zosyn
When should antifungal therapy be initiated in pts with intra-abdominal infections?
pts with yeast on gram stain.
evidence of heavy colonization.
surgically treated pancreatitis
prolonged broad spectrum abx
Critically ill pts with upper GI source
Fluconazole is DOC for susceptible strains but echinocandins should be 1st line in critically ill until results are available.
How long should treatment for COMPLICATED intra-abd infection last for?
No more than 4 days with adequate source control
5-7 days in pts without definitive source control and depending on clinical response.
When should you use only short term (<24hrs) prophylactic ABXs in regards to abdominal infections?
Acute Gastric/ Jejunal Perforation (only if there is no malignancy or acid-reducing meds and source control within 24hrs)
Traumatic / iatrogenic bowel injuries repaired within 12 hrs of injury
Acute appendicitis without perforation or abscess.
What categorizes patients as having SEVERE Acute Pancreatitis?
APACHE II score of > 8 or Ranson's Criteria >3 along with clinical presentation.
True or False:
We treat all patients with necrotizing pancreatitis?
No
2/3 acute necrotizing pancreatitis is sterile
(mortality 2-9%) just hydrate and and remove necrosis with surgery.
1/3 Infected necrotizing Pancreatitis. (mort 44-62%)
needs evidence of fluid collection or abscess to treat
Why do people develop Pancreatitis?
Glandular Autodigestion due to excessive ductal/tissue exposure to amylase/ lipase/ protease.
Excessive enzymes due to:
Trypsin-related hyperstimulation
Macro/micral-ductal blockage
What are the 3 phases of Pancreatitis?
1. Excess activation/ decrease inactivation of trypsin
2. Local inflammatory / immune response to pancreatic injury
3. Systemic Inflammatory / immune response (SIRS, hypovolemia, ARDS)
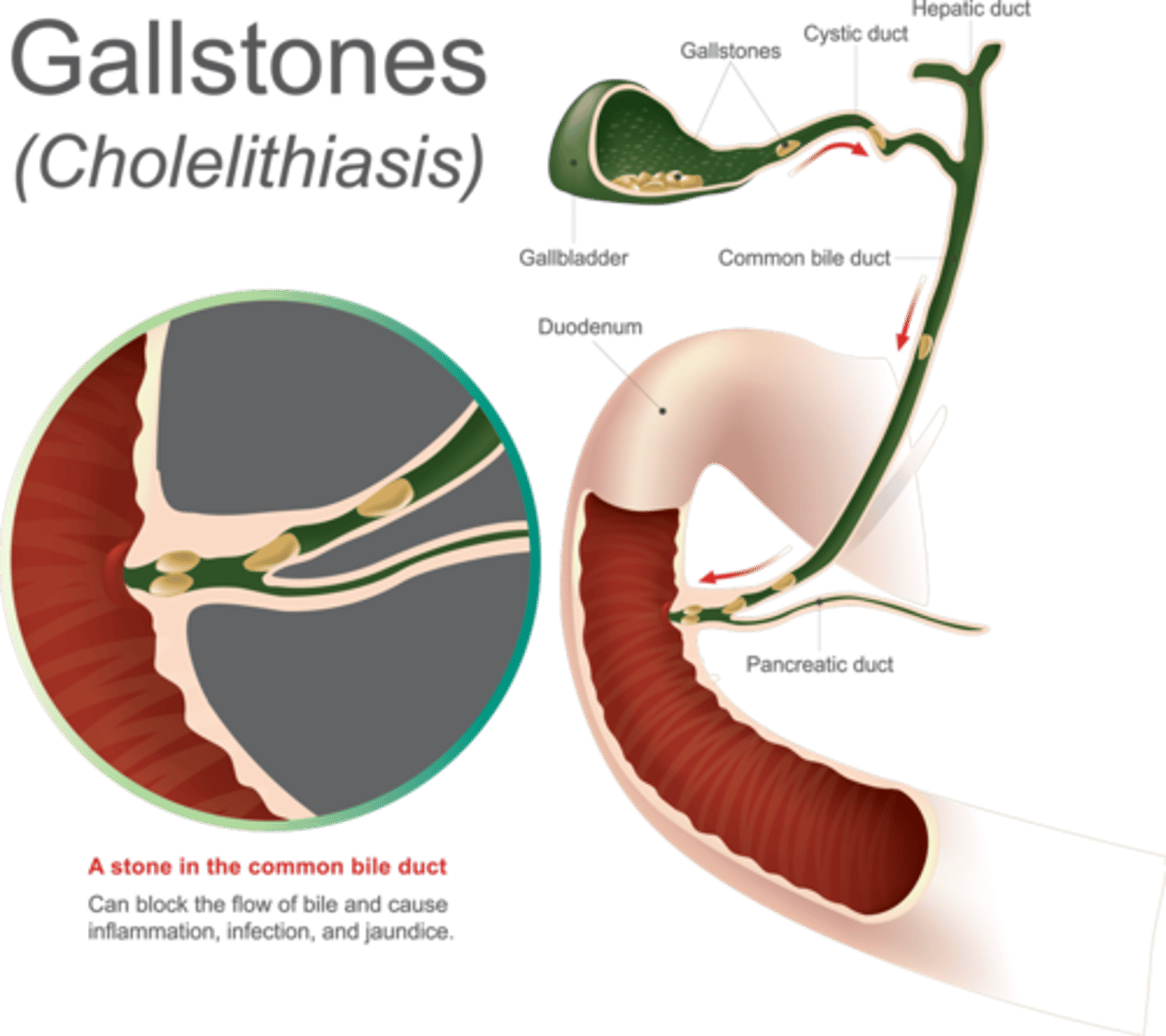
What are some common causes of Acute Pancreatitis?
Biliary obstruction ( gallstones)
Direct Toxicity ( alcohol)
Trauma/surgery/biliary procedures
drugs
What is SEVERE Pancreatitis?
Pancreatitis + hypovolemia, organ failure, local complications ( necrosis, abscess, or psudoyst) if present then treat. = TREAT WITH ABX
hypovolemia increases risk of necrosis to pancreas and intestine due to hypoperfusion.
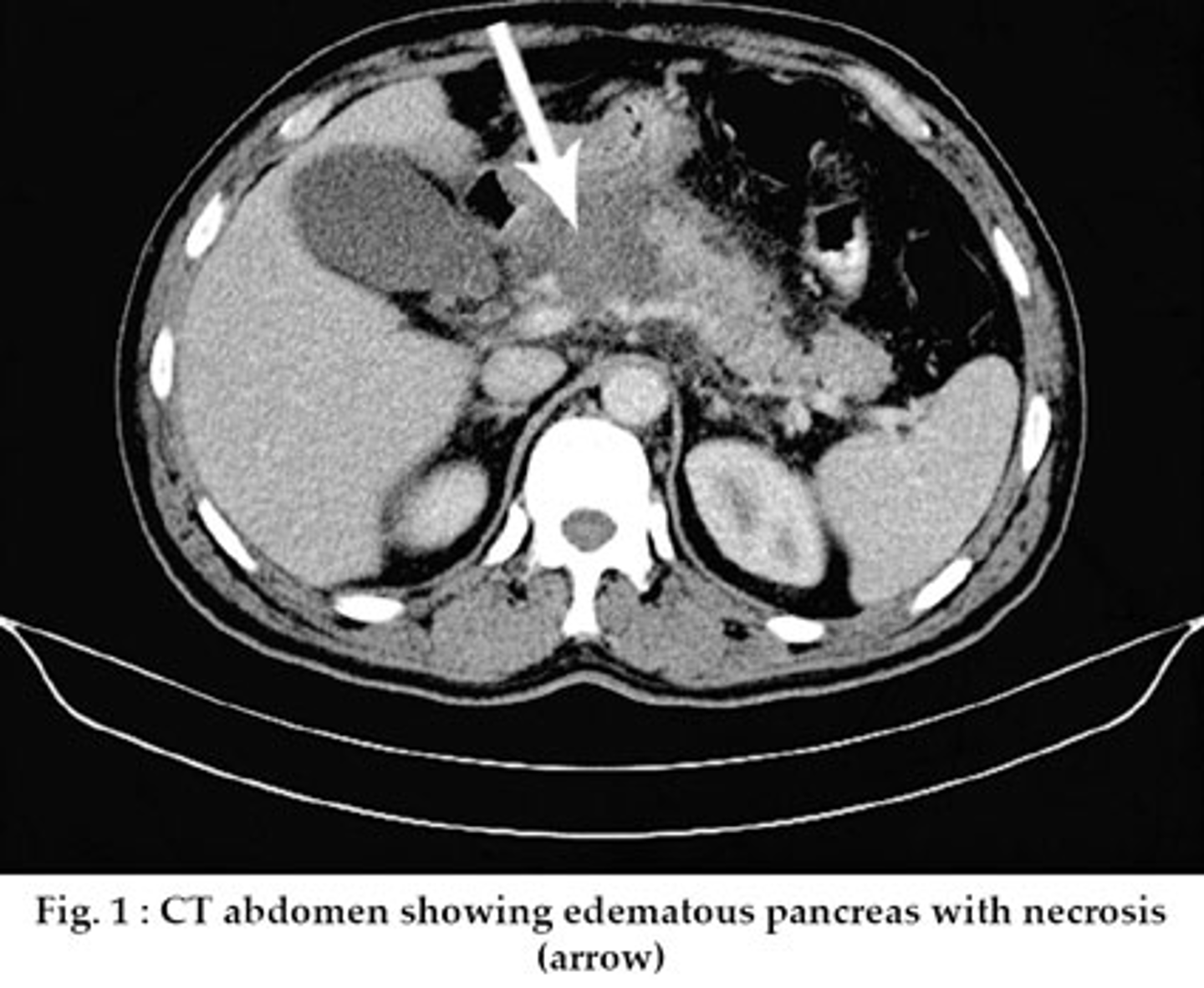
What exam is used to see pancreatic necrosis?
A CT scan will show diffuse/focal nonviable pancreatic tissue +/- peripancreatic fat necrosis. >30% of the pancreas should be affected.
Infected necrosis just means that the necrotic tissue is positive for microorganisms.
What is a pancreatic pseudocyst?
non-epithelialized wall containing pancreatic excretions due to acute/chronic/traumatic pancreatic trauma.
psuedocysts are usually sterile= no treatment
What is a pancreatic abscess?
Either a
pseudocyst that has become infected or....
liquefaction of pancreatic necrosis that is infected
How is acute pancreatitis diagnosed?
Need TWO of the following three to be present:
1. Acute + Constant pain ( epigastric or right upper quadrant) +/- nausea and vomiting.
2. Serum amylase/lipase > 3 x the upper limit of normal
3. (+) CT scan for acute pancreatitis.
How do we treat Infected Necrosis and Pancreatic Abscesses?
1. Both need CT or ultrasonography guided drainage.
2. Culture drainage.
3. Treat with ABX for up to 14 days.
If a pancreatic abscess or infected necrosis is drained, what are the most likely pathogens that are going to be found?
What abx do we use as empiric therapy?
GN- Bacilli ( Enterobacteriaceae) or Strep (((KEEP-S)))
Klebsiella, E. Coli, Enterobacter, Proteus - Strep
Carbapenems ( imi/mero).....or
Flagyl + FQ.....or
Flagyl + 3rd/4th Gen cephalosporin
Can we give prophylactic ABX for sterile necrotizing pancreatitis ?
Current recommendations DO NOT support routine use of ABX prophylactically for sterile necrotizing pancreatitis. if sterile just hydrate and and remove necrosis with surgery.
needs significant fluid collection or abscess formation to indicate infection= to treat.
What do we suspect when amylase and lipase do not decrease after intervening in the treatment of pancreatic/periphancreatic inflammation?
persistent pancreatic/peripancreatic inflammation
pancreatic duct blockage.
development of pseudocyst.
Definition of regular C. Diff Infection (CDI)?
Diarrhea +++PLUS+++
Stool (+) for C. Diff/ toxigenic C. Diff.....or
Pseudomembranous colitis via colonoscopic examination.
Definition of SEVERE C.diff infection?
Regular CDI + ONE of the following:
-WBC > 15
-SrCr >1.5 times greater than premorbid level.
Definition of SEVERE COMPLICATED CDI?
Severe C. Diff Infection + ONE of the following:
-Hypotension/ shock
-Colonic Ileus
-Toxic Megacolon
What are the risk factors for CDI?
1. ABX (ALL OF THEM- highest risk with...
FQs, Cephalosporins, PNCs, Clindamycin)
2. PPIs & H2-Blockers
3. Age >65
4. Duration of hospitalization
5. Chemotherapy
6. GI Surgery
7. Previous CDI
True/False:
In order to reduce the spread of C.Diff you need to wash your hands with alcohol based substance?
False, non-alcohol based handwash such as water+soap
or chlorhexidine+ water.
How many bouts of diarrhea are needed to suggest CDI?
3 or more UNFORMED stools within 24hrs.
Cecal or Right-sided CDI colitis = may have formed stools.
In C. Diff what ABX do we give for an INITIAL episode that is NON-Severe?
Vanco 125mg PO/NG/FT four times a day x 10 days
or
Fidaxomycin 200mg PO BID x 10 days
Alternative: Flagyl 500mg PO/NG/FT three times a day x 10-14 days (has a delayed response)
In C.DIff what ABX do we give for an INITIAL episode that is SEVERE?
Vanco 125mg PO/NG/FT four times a day x 10 days
or
Fidaxomycin 200mg PO BID x 10 days
In C. Diff what ABX do we give for an INITIAL episode that is
Severe Complicated or Fulminant?
Vancomycin 500mg PO/NG/ FT four times/day +PLUS+ Metronidazole 500mg IV q8hrs.
If Illeus present: ADD Rectal Vanc 500mg/100ml NS and instill rectally for 1hr--QID.