Anesthesia - New material for FINAL exam
1/66
Earn XP
Description and Tags
TY Abby
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
What is the function of the cardiovascular system?
to circulate blood and ensure delivery of oxygen to the body
___________ = cardiac output x oxygen content
Oxygen delivery equation
CO x SVR (systemic vascular resistance) =
MAP/mean arterial pressure equation
What are the 4 mechanisms that can cause hypotension?
*separate answers with a comma
vasodilation, bradycardia, decrease in cardiac preload, decrease in myocardial contractility
decreased systemic vascular resistance
vasodilation
What are causes of vasodilation?
*separate answers with a comma
anesthetic agents like inhalant anesthetics or acepromazine, cardiac drugs, sepsis, anaphylaxis
What are the causes of bradycardia?
excessive anesthetic depth, arrythmias, opioids, alpha-2 adrenergic agonists
causes include:
- hemorrhage
- dehydration
- 3rd spacing
- vascular compression/obstruction
- positive pressure ventilation...which is due to cardiac compression
- vasodilation
decreased preload causes
occurs when too much fluid moves from the intravascular space (blood vessels) into the interstitial or "third" space which can then cause edema, reduced cardiac output, and hypotension
- i.e. effusions, ascites, GI fluid
3rd spacing
causes include:
-neonate/juveniles/pediatrics - receptors are immature and don't respond to catecholamines
- dilated cardiomyopathy
- isoflurane
- propofol
- hypocalcemia
- acidosis
decreased/poor contractility causes
What are the treatment(s) for Vasodilation (mechanism of hypotension)?
*separate answers with a comma
fluid volume, vasoconstrictors or pressors
What are the treatment(s) for bradycardia (mechanism of hypotension)?
*separate answers with a comma
anticholinergics, antiarrhythmics
What are the treatment(s) for decreased preload (mechanism of hypotension)?
*separate answers with a comma
volume bolus, decrease ventilation, relieve obstruction/compression
What are the treatment(s) for Decreased contractility (mechanism of hypotension)?
*separate answers with a comma
positive inotropes, reduce inspired inhalant levels
Stage of cardiovascular disease where the patient is at risk but has no clinical signs
Stage A
Stage of cardiovascular disease where there is a murmur but no past or present clinical signs of heart enlargement or failure
Stage B1
Stage of cardiovascular disease where there is a murmur and cardiomegaly but they're asymptomatic
Stage B2
Stage of cardiovascular disease where patients have past or present clinical signs of heart failure with structural cardiac disease
Stage C
Stage of cardiovascular disease where patients have end-stage heart failure that are refractory to standard therapies
Stage D
What is the anesthetic management for Cardiovascular disease Stage A and B1?
generally do not require intensive management
What is the anesthetic management for Cardiovascular disease Stage B2?
keep patient heart rates normal, keep patient normothermic, avoid Alpha 2s
What is the anesthetic management for Cardiovascular disease Stage C and D?
rely on balanced anesthesia, avoid Alpha 2s, use opioids/benzodiazepines to reduce amounts of induction & inhalant agents needed
the thickening of the cardiac muscle leading to stiffening and failure of relaxation & adequate filling (think of body builders)
HCM/hypertrophic cardiomyopathy
this is the primary loss of myocardial contractility that can lead to dilation of the ventricles
DCM/Dilated cardiomyopathy
the volume of gas inhaled or exhaled in the lungs per minute ventilation
minute ventilation
Maintain ventilation by maintaining CO2 levels of ________________ and pH value of ________________ since these parameters are directly related
*separate answers with a semicolon
35-45 mmHg; 7.35-7.45
What does adequate oxygenation depend on?
*separate answers with a comma
hemoglobin/Hb, arterial oxygen saturation/SaO2, alveolar partial pressure of oxygen/PaO2
Main 3 causes of Hypoxemia...
*separate answers with a comma
low inspired oxygen fraction- FiO2, Hypoventilation, diffusion impairments
Obstructive respiratory diseases include...
*separate answers with a comma
asthma, laryngeal paralysis, tracheal collapse, brachiocephalic
What is the anesthetic management for Obstructive respiratory diseases?
*separate answers with a comma
minimize excitement & stress, mild sedation may be warranted
What are 6 examples of conditions/diseases that cause decreased lung capacity?
*separate answers with a comma
aspiration pneumonia, muscle rigidity, obesity, intra-abdominal changes like tumors and GDV, spinal injuries, intervertebral disc disease
What is the anesthetic management for Decreased Lung Capacity?
*separate answers with a comma
protect airway & suction mouth as needed, pre-oxygenate, mechanical ventilation, monitor oxygenation
blood flow to the brain
- blood pressure affects it's pressure (i.e. if BP is low, blood flow to the brain may be limited
cerebral perfusion
Neurological disease can include...
*separate answers with a comma
brain injury, trauma, tumors, hydrocephaly
if this is too high, blood flow to the brain may be limited
intracranial pressure
What is the anesthetic management for neurological disease, specifically brain injury, trauma, tumors, and/or hydrocephaly?
*separate answers with a comma
maintain MAP, oxygen & ventilatory support, mannitol, hypertonic saline
The liver provides multiple essential functions. List 4...
*separate answers with a comma
bile formation & excretion, metabolic functions, stabilizes osmotic pressure, helps maintain pH
list 3 complications associated with hepatic disease...
*separate answers with a comma
hepatic encephalopathy, hypokalemia, hypoglycemia
What does the GI tract provide to the body?
*separate answers with a comma
supply of water, electrolytes, and nutrients
What are 5 things that GI disease could cause?
anorexia, dehydration, protein loss, abdominal pain, hypovolemia
correct any imbalances before anesthesia. FOR instance, correct dehydration how long before anesthesia?
24 hours prior
___________ functions in:
- excretion of metabolic waste and toxins
- regulation of blood volume and extracellular fluid
-aids in acid-base regulation
kidney functions
- hormone imbalance imbalance - decreased
- decreased metabolism
- weak muscles
- bradycardia
-hypothermia
hypothyroid
- hormone imbalance - increased
- hypertension
- hyperthermia
- cardiac changes
hyperthyroid
What is done for Newborns with airway problems?
*separate answers with a comma
suction mouth, stimulate breathing, don't sling/swing puppies
What is done for Newborns with cardiovascular problems?
*separate answers with a comma
chest compression about 120 bpm, epinephrine drop under tongue
Humane killing is subdivided into what 3 things?
*separate answers with a comma
euthanasia-individuals, humane slaughter-large numbers, depopulation-large numbers
methods producing humane death as the sole means of euthanasia
acceptable
acceptable methods of euthanasia when certain conditions are met
acceptable with conditions
methods of euthanasia not to be used under any conditions
unacceptable
- pain perception requires functioning cerebral cortex
- anesthetized or properly euthanized animals do not feel pain
- loss of consciousness should precede loss of muscle movement
painless and distress free euthanasia
What are the three basic mechanisms?
*separate answers with a semicolon
direct depression of neurons necessary for life functions; hypoxia meaning CO or CO2 overdose; physical disruption of brain activity
- expensive; personnel exposure
- CO2
inhaled anesthetics
How do we administer an anesthetic overdose?
*separate answers with a comma
inhaled anesthetics, injectable anesthetics
- Pentobarbital
- 1 minute onset, minimal movement if properly restrained
- carcass contamination (risk of carcass being dug up, consumed, causing further issues to animal consuming it)
injectable anesthetics
regardless of euthanasia method, death ________________
must be confirmed
regarding Euthanasia and animal workers,
___________ methods have potential to cause physical injury and death
ALL
- transferal of personal feelings/fear onto the animal (animals catch on to how we're feeling)
- depression, grief, anger, guilt, sleeplessness
- job dissatisfaction may result in absenteeism, belligerence, careless/callous animal handling
"killing-caring paradox"

Ethical dilemma involving life-and-death decisions.
The Trolly Problem
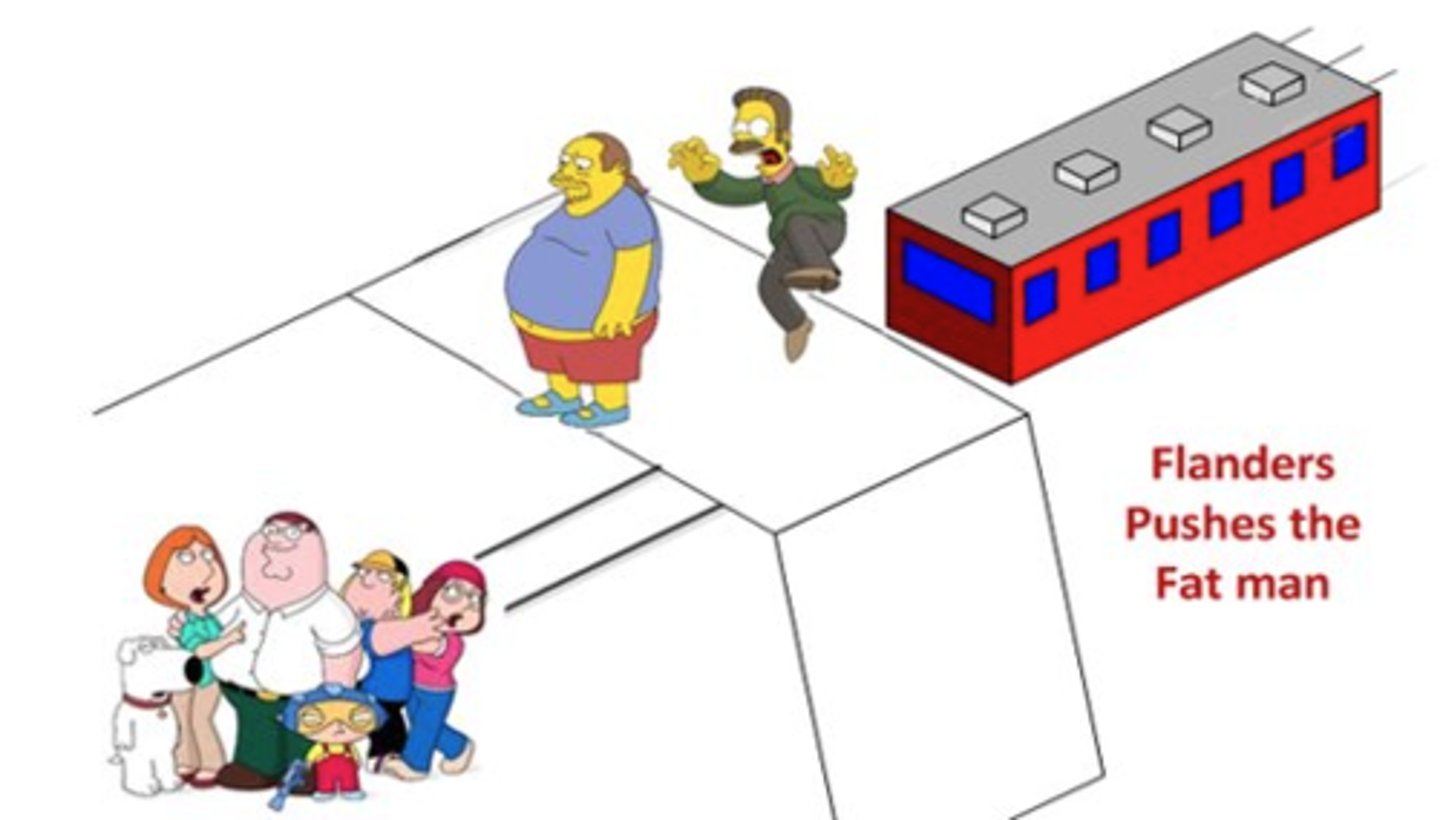
Similar to the Trolley Problem, but instead of pulling a lever, you are asked whether it is morally permissible to push a large person off a bridge to stop a runaway trolley from hitting five people on the track below. The dilemma is whether to take direct action to save five lives at the cost of one.
The Fat Man Problem
– IV injection of DEA II, III pentobarbital cpds
– IC or intra-organ injection only on unconscious or anesthetized animals
Pet euthanasia issues
CO2 is minimally affected by _______________disease.
respiratory
What is Medium or High-expansion Water-based Foam euthanasia used for?
*separate answers with a comma
Zoonosis; spreading infectious disease-Immersion causes airway occlusion and death by suffocation
-Pentobarbital; large volumes (approx 100 mls) needed-gunshot or penetrating captive bolt
Horse euthanasia methods
Head shot, penetrating captive bolt, KCl IV, or MgSO4 IV during general anesthesia to reduce toxicity to scavengers
Zoo and wildlife euthanasia methods
Attempts to remove the fetus from the uterus or to revive a fetus following death of the dam are likely to result in what??
serious welfare complications for the newborn
What is recommended for fetuses that have been removed from the uterus?
IP pentobarbital