BMD 310 Bone Tissue
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
What is histology?
The study of the tissues of the body and how tissues are arranged into organs
What are the two main components of tissues?
Cells and extracellular matrix (ECM)
What are the steps to make tissue slides?
Collected, Fixed (formalin, paraformaldehyde, etc.), Sectioned, Stained (H&E, methylene blue, etc.), Imaged (Brightfield, fluorescence)
What is H&E staining?
A commonly used staining method in histology
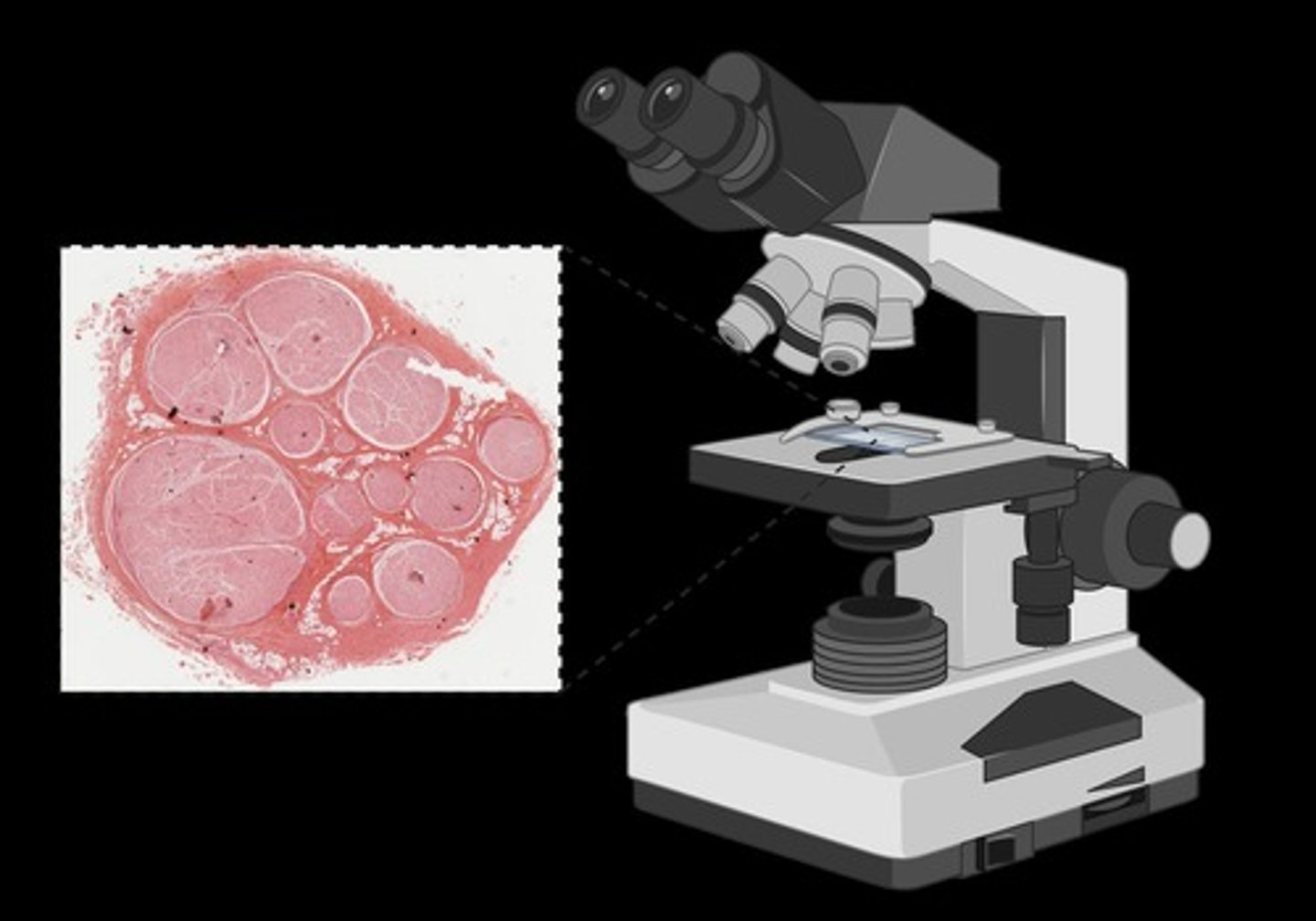
What are the two components of H&E staining?
hematoxylin and eosin
What is Hematoxylin?
basic, stains acidic things (basophilic) a purple/blue color (nucleus and RNA)
What is Eosin?
acidic, stains basic things (acidophilic), pink color (cytoplasm, proteins)
Are skeletal bones considered organs?
yes
What is bone primarily composed of?
Bone is primarily connective tissue with a sturdy and rigid extracellular matrix due to mineral deposition (calcification)
List the functions of bone.
Support and protection of organs, movement, hematopoiesis, and storage of minerals and energy reserves.
What is hematopoiesis?
blood cell production in red bone marrow
What are the two minerals that bones store? Where are lipids (energy) stored in the bone?
calcium and phosphate, yellow marrow
What are the types of bones based on shape?
Long bones, short bones, flat bones, irregular bones, and sesamoid bones.
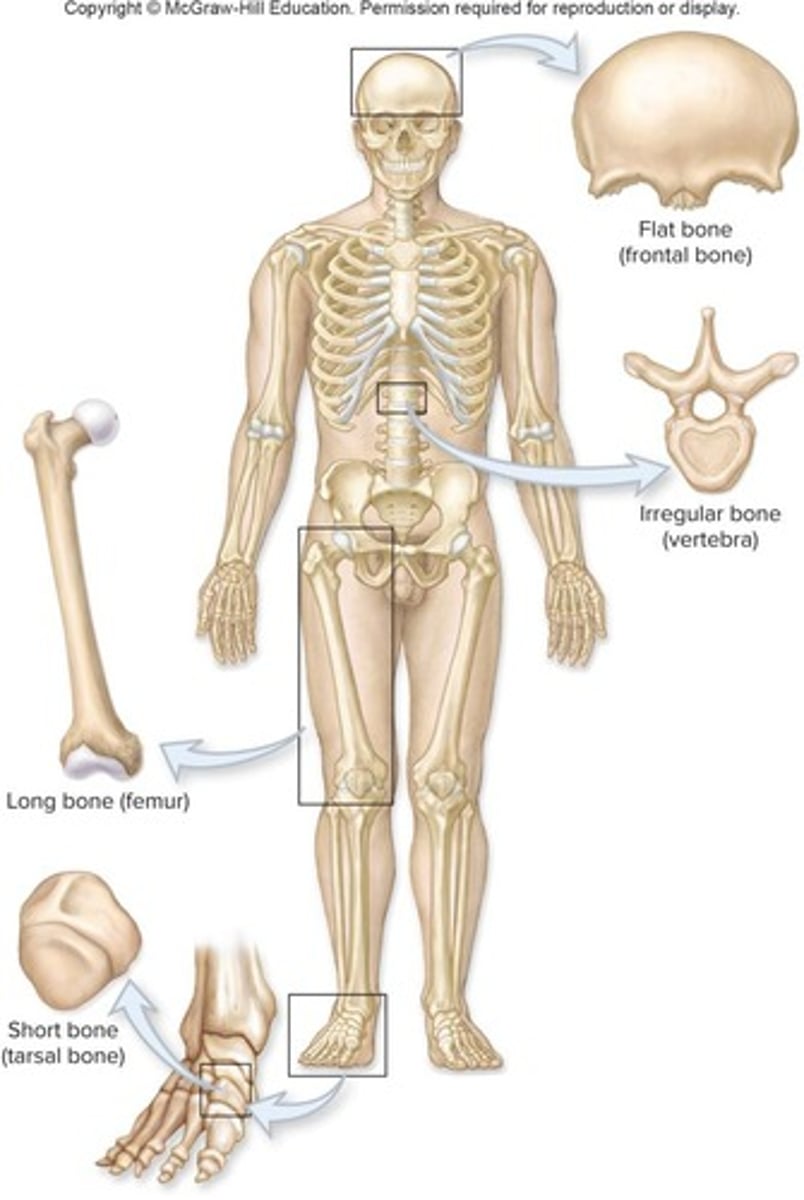
What are long bones?
longer than they are wide
What are short bones?
nearly equal length and width
Which two types of bones are very similar in general strucutre? What is the difference?
long and short (no diaphysis)
What are flat bones?
thin surfaces
What are irregular bones?
complex shapes
What are sesamoid bones?
develop within tendons (kneecap)
What is the diaphysis of a long bone?
The elongated, cylindrical shaft of the bone
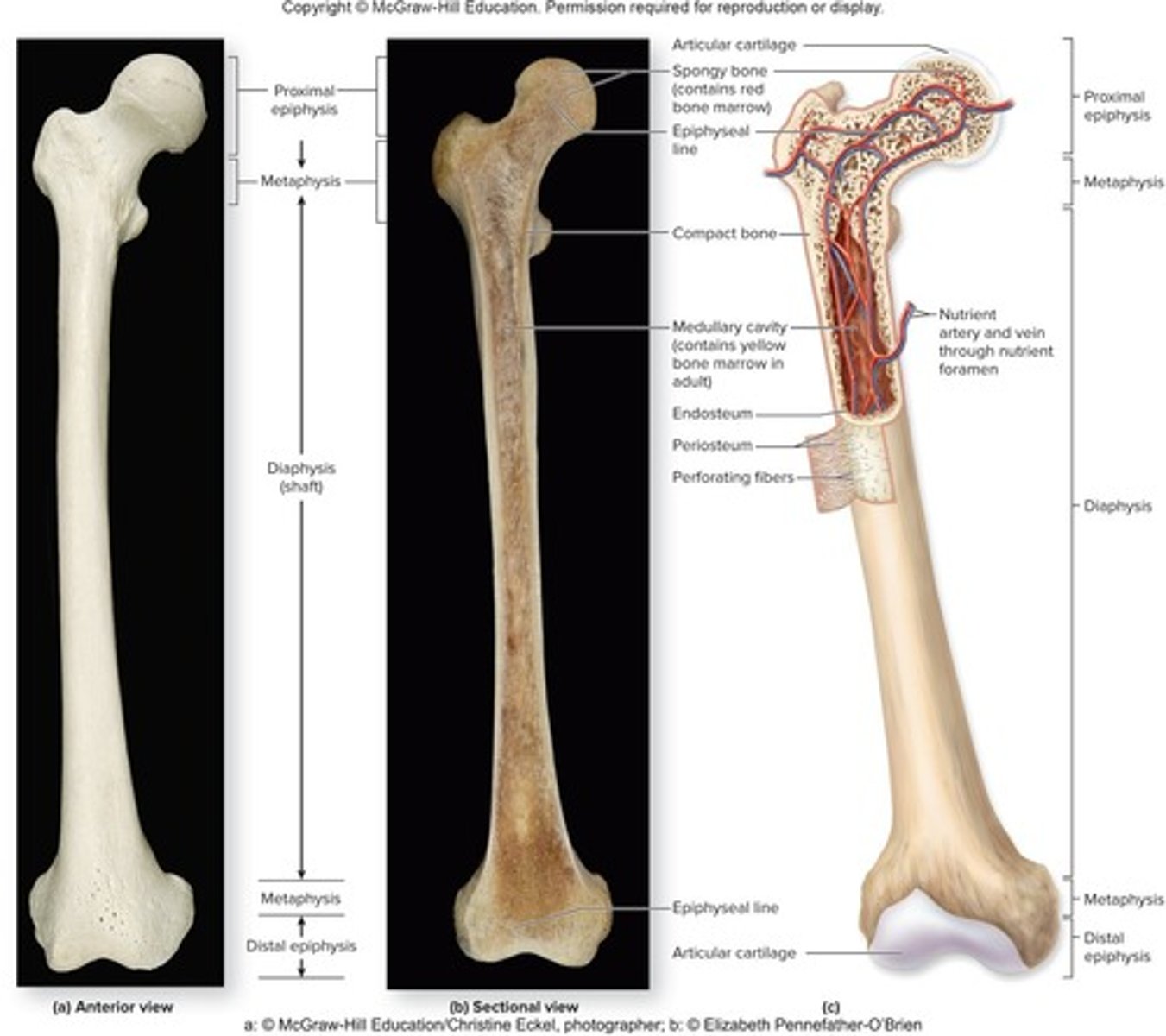
What is the epiphysis of a long bone?
The knobby, enlarged regions at each end of the bone that strengthen joints and serve as attachment sites for tendons and ligaments
What is the metaphysis in a long bone?
The region between the diaphysis and epiphysis that contains the epiphyseal (growth) plate.
What is articular cartilage?
A thin layer of hyaline cartilage covering the epiphysis that reduces friction and absorbs shock in movable joints.
What is the medullary cavity?
Hollow, cylindrical space in diaphysis; in adults, it contains yellow bone marrow
For the flat bones in the skull, how are the bones layered?
two layers of compact bone with spongy bone in between
Cartilage is a strong, ________ connective tissue that protects your joints and bones. Also supports soft tissues: Examples include the _______ in respiratory system and ________ of ear. Provision of ________ surface at articulations (reduction of friction where bones meet). Provision of a ______ for the formation of bone growth.
flexible, airways, auricle, gliding, model
Hyaline Cartilage
most abundant, at joints to make a smooth surface, on the end of bones
Fibrocartilage
very strong to support and join structures together
Elastic cartilage (function)
strength and flexibility
What is compact bone?
Solid and relatively dense, External surfaces of long and flat bones
What is spongy bone?
Open lattice of narrow plates called trabeculae, Internal surface of bones
What is an osteon?
The basic unit of compact bone, also known as a Haversian system, consisting of cylindrical structures running parallel to the diaphysis, very small in diameter
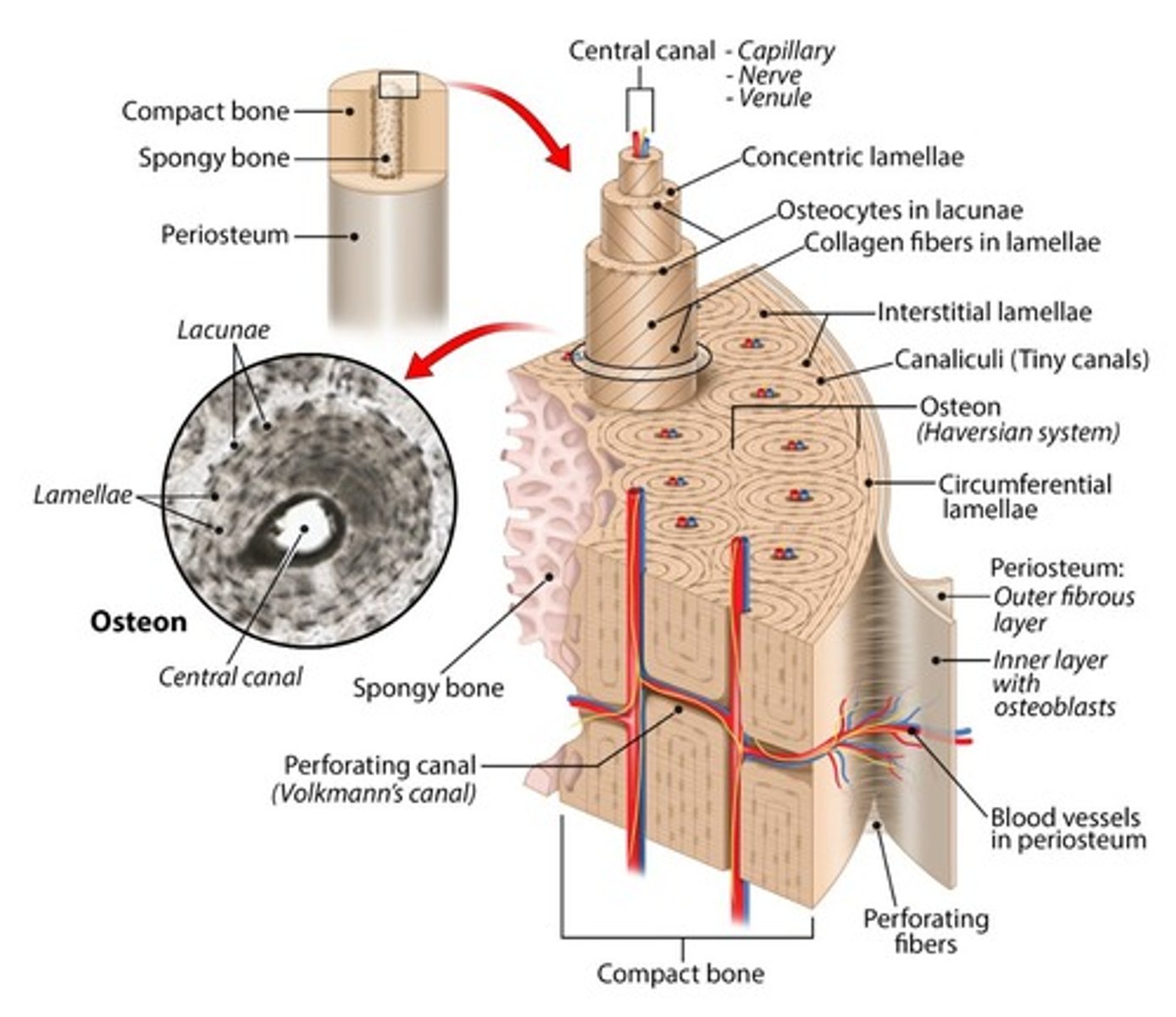
What are osteons so small?
the space contains blood vessels that have to keep the living cells close to the blood supply
Do osteons run the entire length of the bone?
yes
What is the central canal in an osteon?
carries blood vessels and nerves in the center of the osteon
What are the perforating canals in an osteon?
run perpendicular to and help connect multiple central canals; Passageways for blood vessels and nerves
What are osteocytes?
Mature bone cells that maintain metabolism and are housed in lacunae between lamellae, like a sensory organ (squeeze when pressure) and maintain the boney matrix (through their secretions0
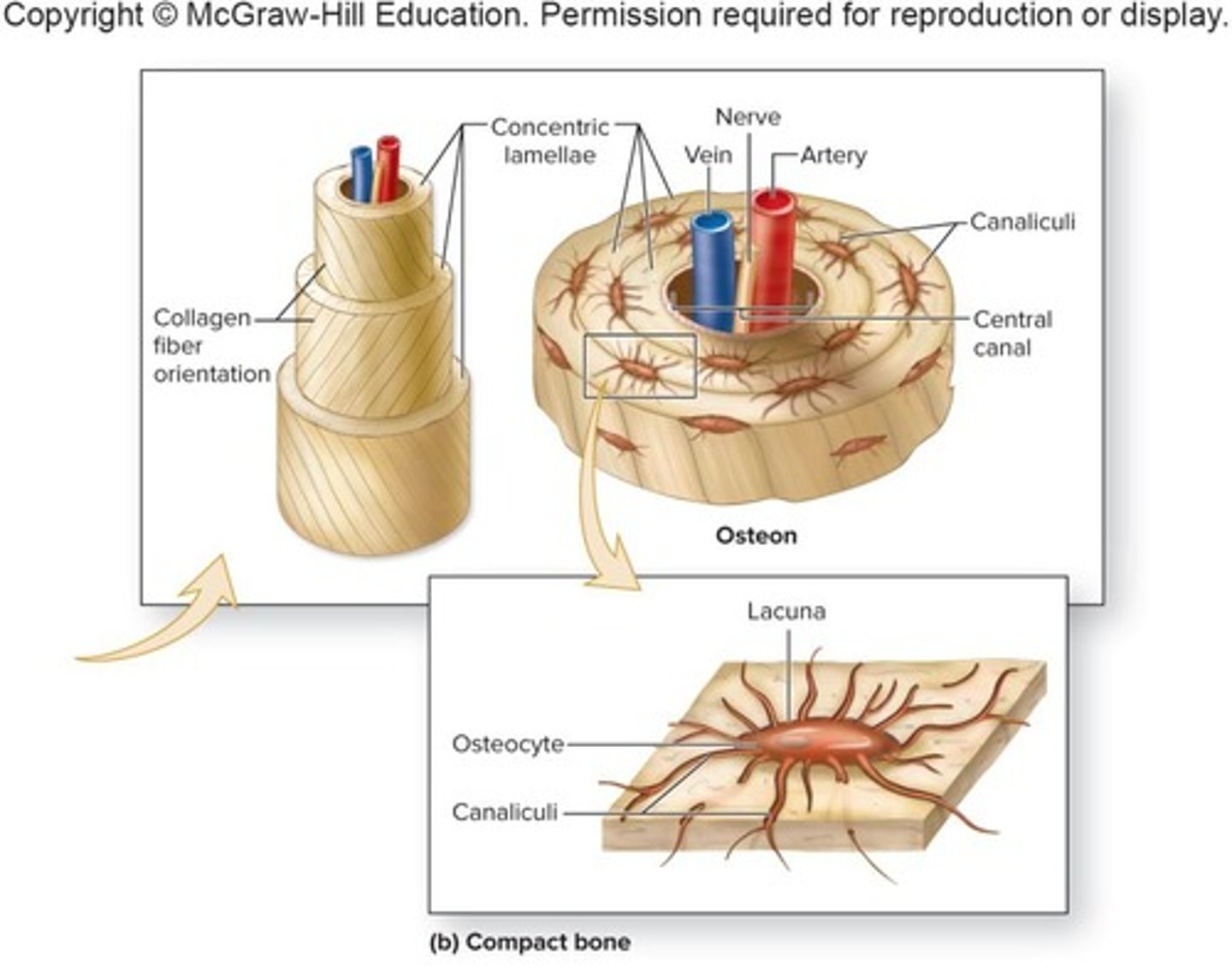
What are Lacunae in an osteon?
spaces within bone which contain osteocytes
What are canaliculi in an osteon?
tiny, interconnecting channels that extend between lacunae and allow osteocytes to connect and communicate
What are concentric Lamellae?
Rings of bone around central canal
Are bones vascular or avascular?
vascular
How to the cells that do not directly touch the blood vessels get nutrients in the bone?
cytoplasmic sharing
How are bone slides prepared for microscopic view?
grinded really thin so it is see through and then dyed black (black spots are holes)
Does spongy bone contain osteons? Trabeculae contain ________ lamellae in spongy bone. Does the space around spongy bone contain blood vessels? Does spongy bone contain central canals?
no, parallel, yes, no
What are the three components of the extracellular matrix in bones?
water, collagen fibers, crystallized mineral salts
What two minerals make up hydroxyapetite in the bone's ECM?
calcium phosphate and calcium hydroxide
What is the significance of hydroxyapatite in bone?
is a mineral form of calcium phosphate that contributes to the rigidity and strength of bone.
What are the four main cell types of bone?
Osteoprogenitor cells, osteoblasts, osteocytes, and osteoclasts.
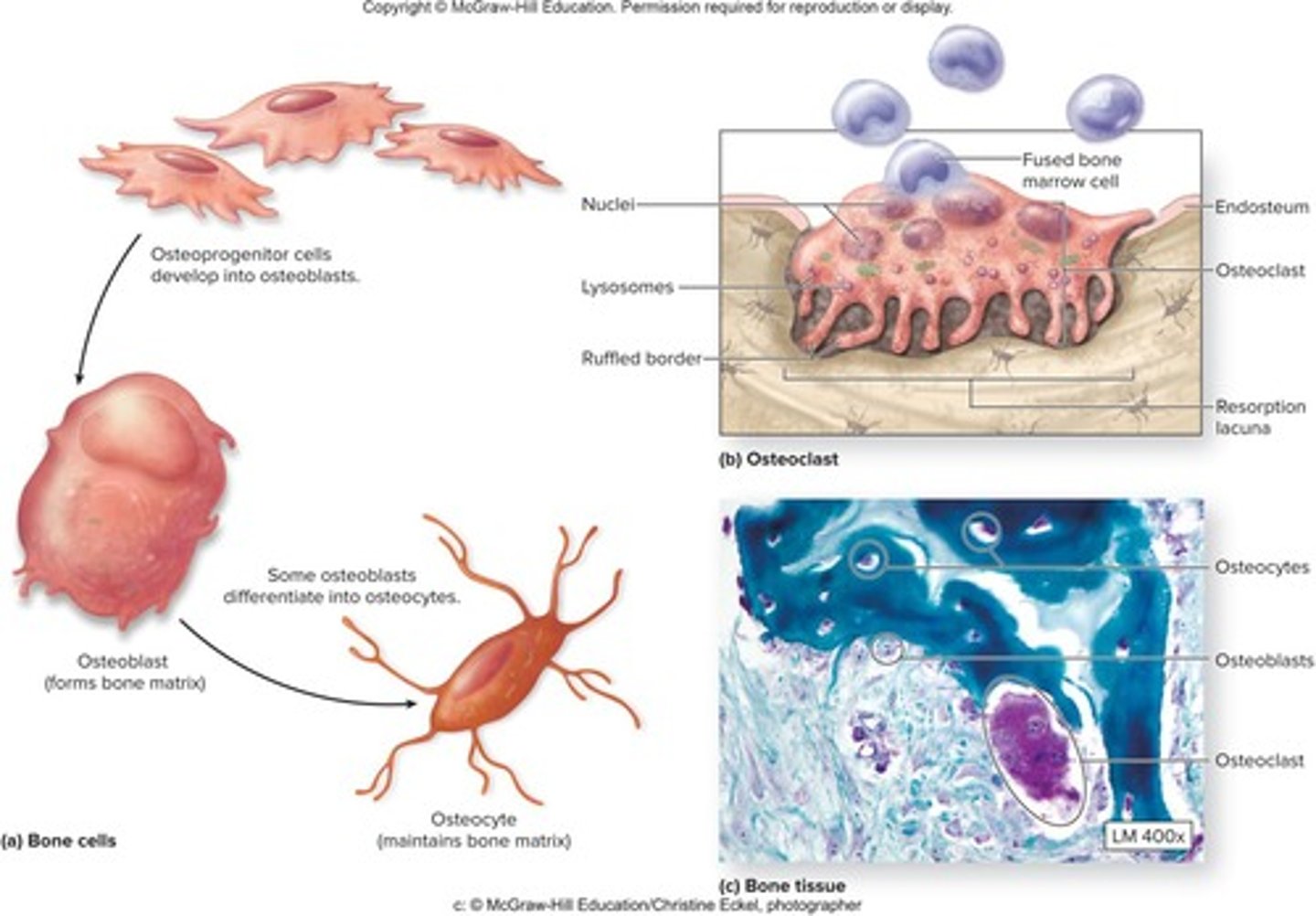
What are osteoprogenitor cells? stem cells of bones, only one that _______ divides
Unspecialized bone stem cells from mesenchyme, Only bone cells to undergo cellular division, Inner portions of periosteum, endosteum and the blood vessel canals, mitotically
What is the function of osteoblasts?
bone builders that help in ossification
Which type of bone cell types do not have the same lineage as the other bone cell types?
osteoclasts
What role do osteoclasts play in bone health?
derived from up to 50 monocytes, release lysozymes and acids to resorb bone, break down bone (bone resorption) and help regulate serum calcium levels
What is red bone marrow? more common in infants
blood cell production, contains hematopoietic stem cells
What is yellow bone marrow? more common in adults
blood vessels and adipocytes
What is the role of cartilage in the body?
Cartilage protects joints and bones, supports soft tissues, and provides a model for bone growth.
What are the types of cartilage?
Hyaline cartilage (most abundant), fibrocartilage (very strong), and elastic cartilage (strength and flexibility).
What are the two patterns of ossification?
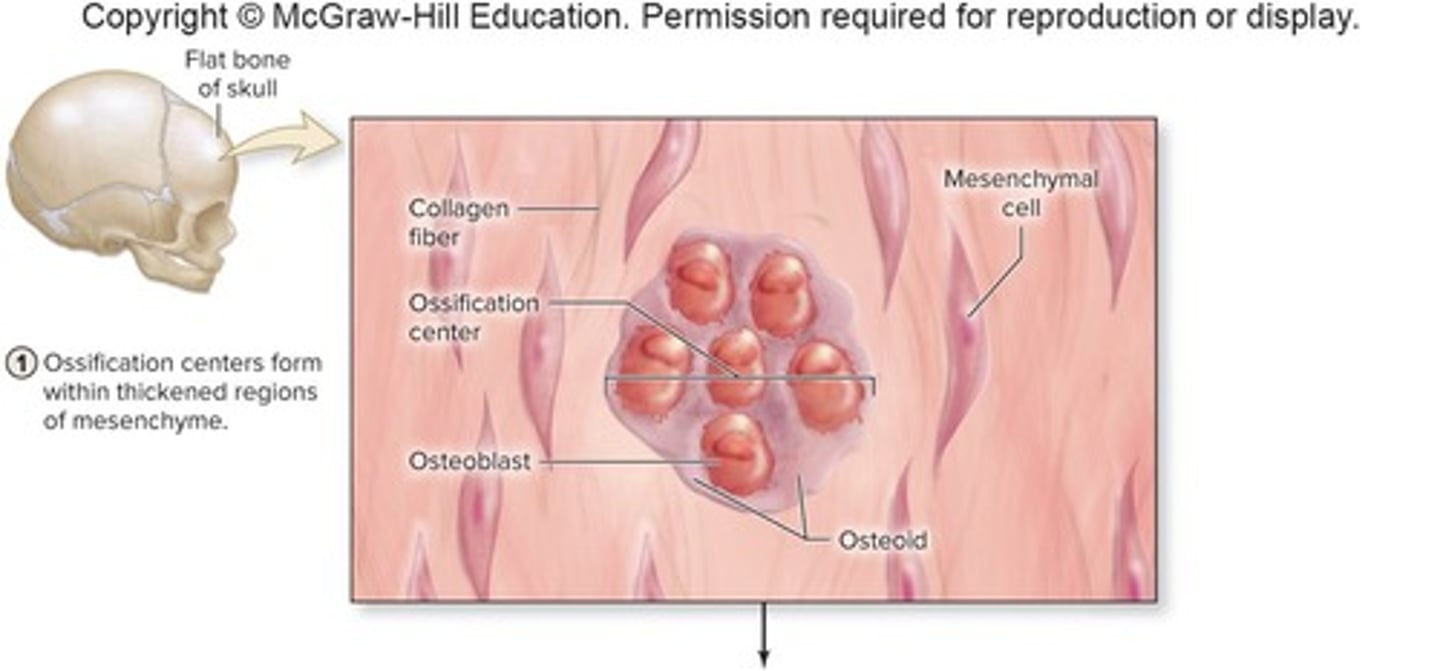
intramembranous and endochondral
What is intramembranous ossification?
A process that develops from mesenchyme (membrane of CT) and produces flat bones of the skull, some facial bones, mandible, and central portion of clavicle.
What is endochondral ossification?
A process that begins with a hyaline cartilage model and produces the majority of bones in the body.
What is interstitial growth in bones?
Growth in length that occurs at the epiphyseal plate
What is appositional growth in bones?
Growth in diameter that occurs at the periosteum
What are the steps of intramembranous ossification?
1. _________ centers form within mesenchyme.
2. Osteoid undergoes _________.
3. _____ bone and surrounding ___________ form.
4. ________ bone replaces woven bone.
Ossification, calcification, woven, periosteum, Lamellar
The steps of bone growth: endochondral ossification:
1. ________ cartilage model
2. Growth of model with primary __________ center developing and __________ (bone collar)
3. ________- bone develops with associated blood vessels; bone has ________ most of the cartilage in the diaphysis region (primary center)
4. Secondary ____________ develops (in the epiphyses) as well as in the __________ cavity (secondary centers)
5. _________ plate and __________ cartilage have formed; potential for further growth in length
6. Mature bone; epiphyseal plates have ________ and the potential for growth in length _______
Hyaline, ossification and periosteum, Compact and replaced, ossification and medullary, Epiphyseal and articular, calcified and ceases
What is the significance of the epiphyseal plate?
It is the site where bone lengthening occurs through the processes of proliferation and hypertrophy of chondrocytes.
What are the zones of the growth plate?
1. Resting Cartilage, 2. Proliferating Cartilage, 3. Hypertrophic Cartilage, 4. Calcified Cartilage, 5. Ossification.
Zone 1; Resting Cartilage
Near the epiphysis; composed of small chondrocytes
Zone 2; Proliferating Cartilage
Chondrocytes proliferate; align into stacks
Zone 3; Hypertrophic Cartilage
Chondrocytes stop proliferating, but enlarge (hypertrophy)
Zone 4; Calcified Cartilage
Minerals are deposited, which kills the chondrocytes
Zone 5; Ossification
Matrix of bone is deposited on the remaining calcified cartilage matrix
What is bone remodeling?
The ongoing process of bone resorption via osteoclasts and new bone formation via osteoblasts.
What triggers bone remodeling?
Exercise, lifestyle, and diet.
As new bone is exposed to _________ loads, it will be stronger. New bone is ______ resistant to fracture than older bone
heavier, more
What role do vitamins play in bone health?
Vitamin A activates osteoblasts, Vitamin C is required for collagen synthesis, and Vitamin D stimulates calcium absorption from GI tract into blood so that Ca2+ is available for bold building
Exercise:
•Mechanical stress stimulates increase in bone density by increased __________ activity
•Bones of athletes become _______ and _______ as the result of repetitive and stressful exercise
•Bones lose mass with age, but this can be slowed or reversed with _______-bearing exercise
osteoblast, thicker and stronger, weight
Fractures:
•Break in any _____
•Named according to _______, shape, position or by the physician who discovered it!
•Fractures may occur and not be visible on _____
25% involve the tibia
bone, severity, x-ray
What is a stress fracture?
A fracture resulting from repetitive, strenuous activity, often seen in athletes.
What is an avulsion fracture?
complete severing of a body part (typically a toe or finger)
What is a comminuted fracture?
A fracture where the bone is splintered, crushed, or broken into small pieces.
What is a complete fracture?
bone is broken into two or more pieces
What is an open/compound fracture?
A fracture where the broken ends of the bone break through the skin.
What is a displaced fracture?
fractured bone parts are out of anatomic alignment
What is a greenstick fracture? bent wet stick
partial fracture; one side of bone breaks-the other side is bent
What is a closed/simple fracture?
A break in the bone where the ends do not protrude through the skin.
What are the two types of fracture reduction?
1. Closed reduction: manual realignment without surgery. 2. Open reduction: realignment with surgery.
What are the phases of physiological fracture repair?
1. Reactive Phase: blood clots and inflammation. 2. Reparative Phase: formation of a fibrocartilaginous callus and bony callus. 3. Bone Remodeling Phase: dead bone is resorbed and compact bone replaces spongy bone.
General Fracture Repair:
- Varies with ______, type of fracture, and specific bone
- Goal is to ______ the bone fragments to restore function (reduction)
--A period of __________ is required
-Two types of reduction (fixing fracture/displacement):
age, realign, immobilization, closed - all in the skin and open - surgery
What are the three phases of physiological fracture repair in order?
reactive phase, reparative phase, bone remodeling
Reactive phase: (blood clot/scab)
•Blood vessels crossing fracture line _______
•Blood clots resulting in a fracture ___________ within 8 hrs after injury
•Nearby bone cell _______
•Swelling, _______________
•Last up to several weeks
break, hematoma, death, inflammation
Reparative phase: Formation of a ___________ callus and then a bony _____ (spongey bone) - collagen support (soft)
fibrocartilaginous, callus
Bone remodeling:
•Dead portion of original bone _________ by osteoclasts
•_________ bone will replace spongy bone surrounding the fracture site
resorbed, compact
What is osteoporosis?
A condition where bone resorption occurs faster than deposition, leading to decreased bone mass and increased fracture risk, mostly affects the middle aged and elderly (women - hormonal changes)
What are common treatments for osteoporosis?
Dietary increases in calcium and vitamin D, weight-bearing exercise, and medications to slow bone loss or build bone.
What is the impact of aging on bone density?
Bone mass decreases with age, but this can be slowed or reversed with weight-bearing exercise.