4.1 Sexual Reproduction in Humans
1/125
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
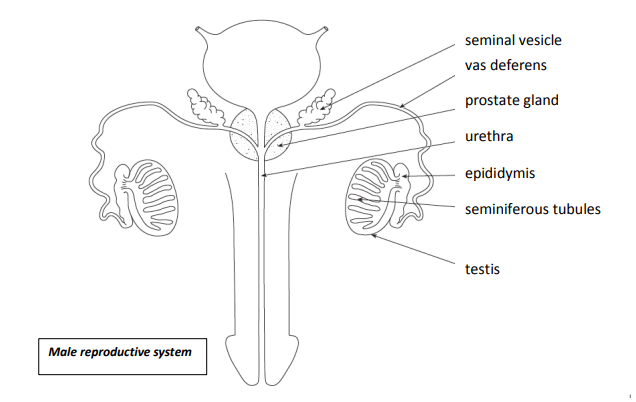
State what the male reproductive system consists of
-A pair of testes
The penis
Ducts connecting the testes with the penis
Accessory glands
Function of scrotum
• Maintains a {cool / optimum / 34oC} environment (for spermatogenesis) / Allow temperatures between 34-36 oC
• holds testes outside abdomen
Function of Epididymis
Sperm are stored here and mature to become fully mobile.
Function of testes
• Produce gametes
• Produce testosterone.
Function of Vas deferens
Carries sperm towards the penis during ejaculation.
Function of seminal vesicle
Secretes mucus into the vas deferens that contains a mixture of chemicals which make up approximately 60% of semen.
Function of seminal fluid
Provides nutrients for sperm
Alkaline to help neutralise the acidity of the urine remaining in the urethra and the acidity of the vaginal tract.
Function of prostate gland
Secretes a fluid into the vas deferens that contains a mixture of chemicals which make up approximately 30% of semen.
What does seminal fluid contain
fructose and amino acids
What does prostate fluid contain
zinc ions and is also alkaline which helps to neutralise the acidity of any urine remaining in the urethra and the acidity of the vaginal tract.
Function of urethra
• Carries semen through the penis and out of the body.
• Carries urine from the bladder through the penis and out of the body.
Function of penis
Specialised organ adapted to transfer semen to the vagina during sexual intercourse.
What do the testis contain
seminiferous tubules
What do the cells lining the seminiferous tubules undergo
spermatozoa (sperm) formation and throughout the process
What happens when sperm reaches the lumen of the seminiferous tubules
they move through the tubule and collect in the vasa efferentia
Function of vasa efferentia
coiled tubes that carry sperm to the head of the epididymis
What is fructose used for in sperm cells
they are respired for energy
Name the accessory glands
prostate gland and seminal vesicles
Name the fluid that emerges from the prostate gland
semen, a mixture of sperm, seminal and prostate fluid
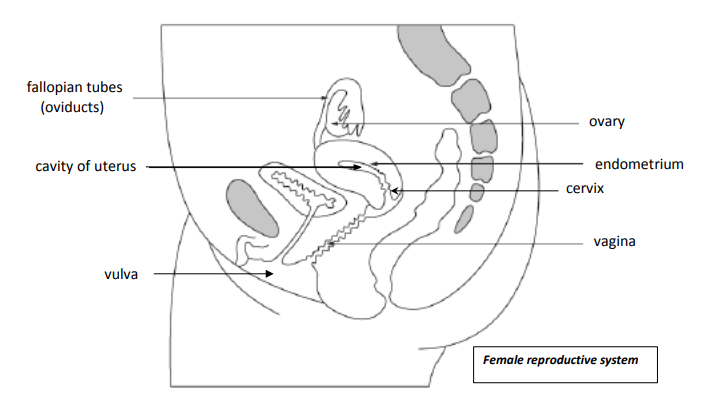
Function of ovary
• Production of gametes
• Produce oestrogen and progesterone.
Function of Fallopian tubes (oviducts)
They have a lining of ciliated epithelial cells which move the secondary oocyte to the uterus.
Function of uterus
Holds the developing foetus until birth.
Function of Endometrium
It has a good blood supply and builds up every month during the menstrual cycle. If implantation of an embryo does not happen then the endometrium is shed during menstruation.
State the 3 layers of the uterus
- Perimetrium, thin layer around the outside
- Myometrium, the muscle layer
- Endometrium, inner most layer

Function of the cervix
A narrow ring of connective tissue and muscle, it acts as a barrier between the uterus and the outside environment during pregnancy.
How does the cervix prevent entry of pathogens during pregnancy
a mucous plug forms in the cervix which helps prevent entry of pathogens.
Name the production of gametes in the sex organs
gametogenesis
Name the formation of sperm in the testis
Spermatogenesis
Name the formation of secondary oocytes in the ovary
Oogenesis
Why is it important that gametes are haploid
so that at fertilisation, the diploid number is restored and the chromosome number does not double in every generation.
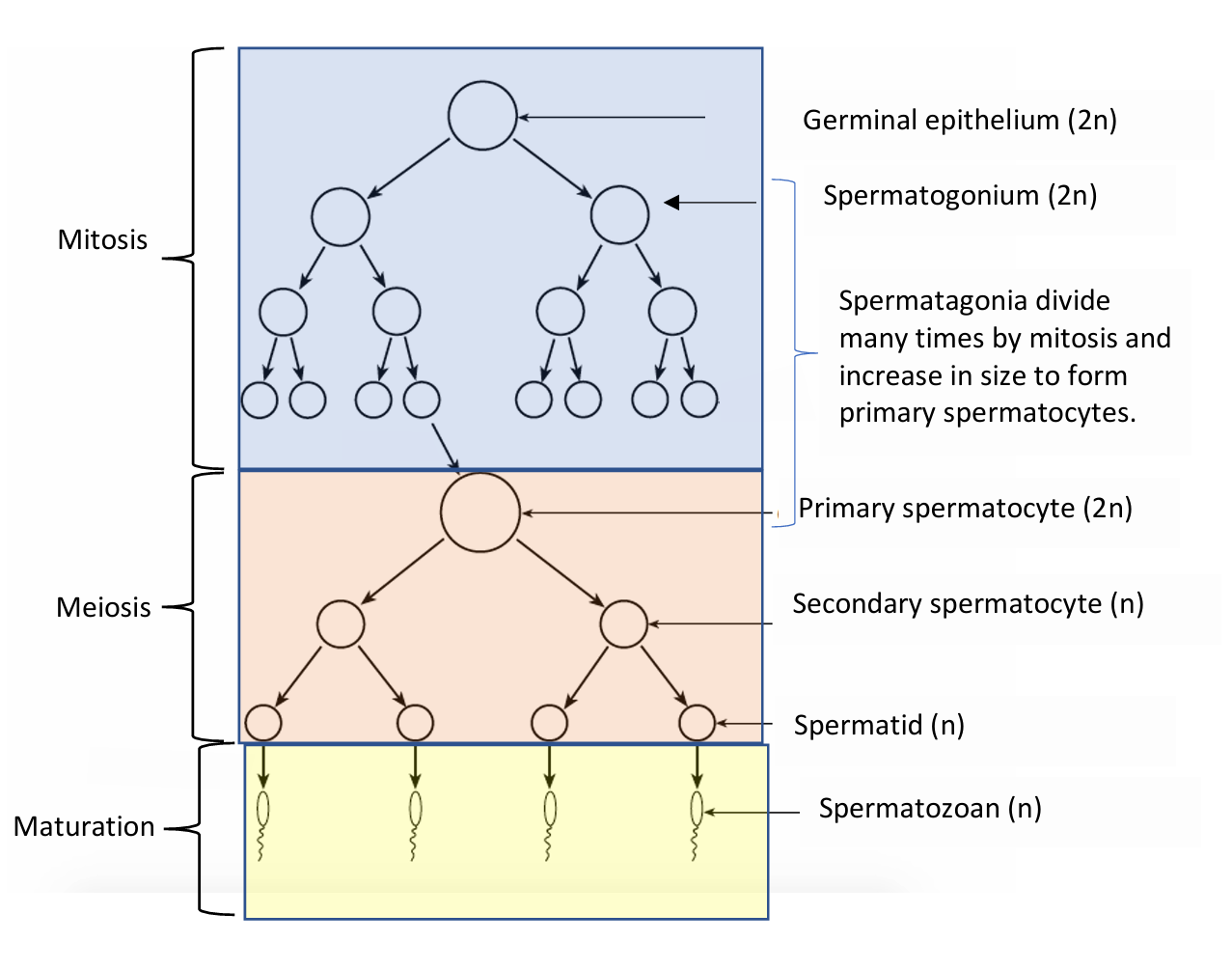
Describe Spermatogenesis
1) Cells of the germinal epithelium are diploid, They divide by mitosis to make diploid spermatogonia and more germinal epithelium cells.
2) Spermatogonia divide many times by mitosis, making more spermatogonia. Some enlarge making diploid primary spermatocytes
3) Primary spermatocytes undergo meiosis I, making secondary spermatocytes, which are haploid
4) Secondary spermatocytes undergo meiosis II, making haploid spermatids
5) Spermatids mature into spermatozoa or sperm
What does the head of a sperm cell contain
a haploid nucleus, covered at the anterior end by a lysosome, called acrosome which contain enzymes used at fertilisation

Describe the middle piece of a sperm cell
packed with mitochondria which spiral around the microtubules which extend from the centrioles into the axial filament in the tail
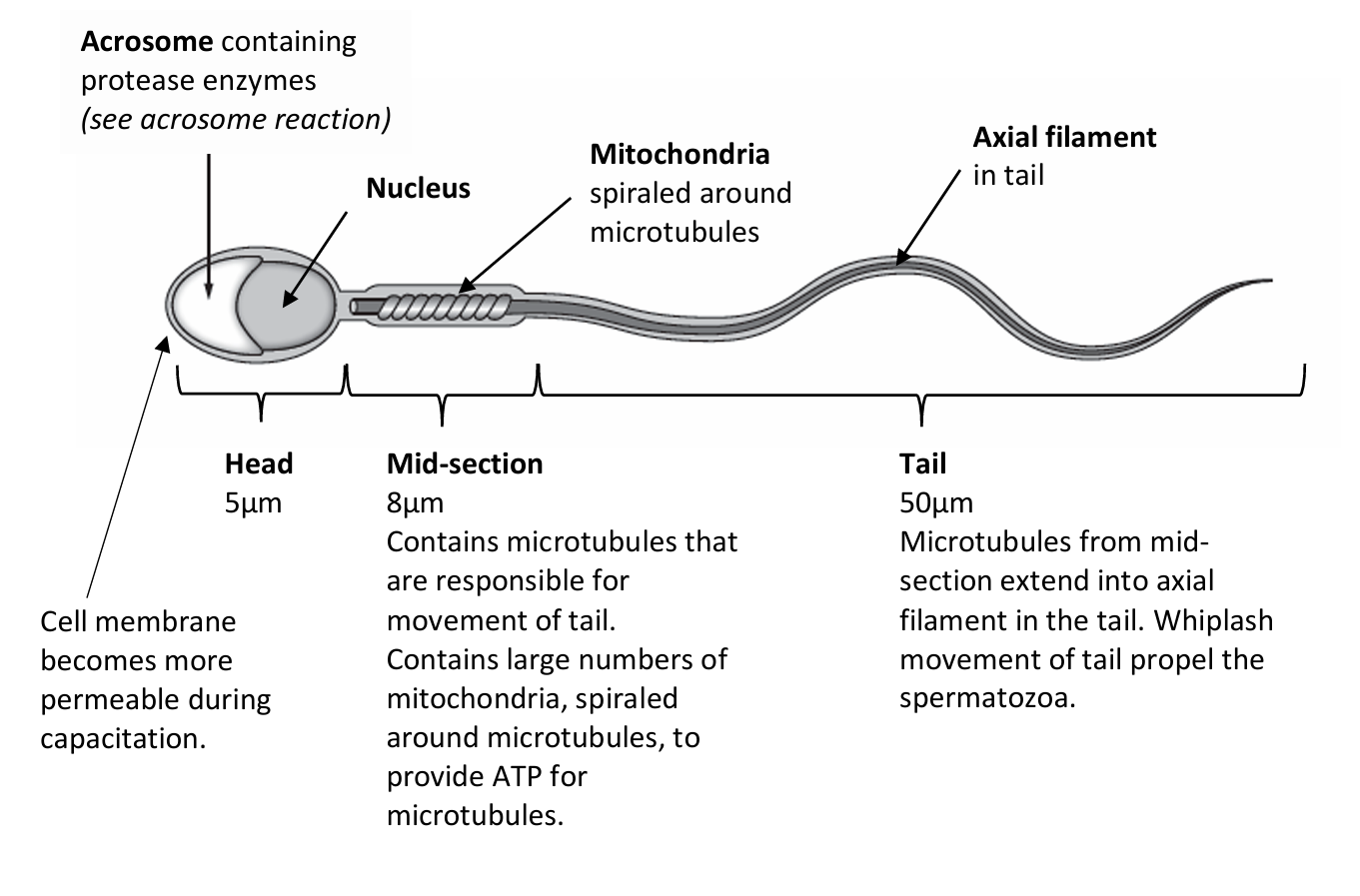
Function of mitochondria in a sperm cell
Provide ATP for movement
Function of the flagellum in a sperm cell
makes lashing movements that move the sperm

When do sperm cells become motile
when they have been modified in the epididymis
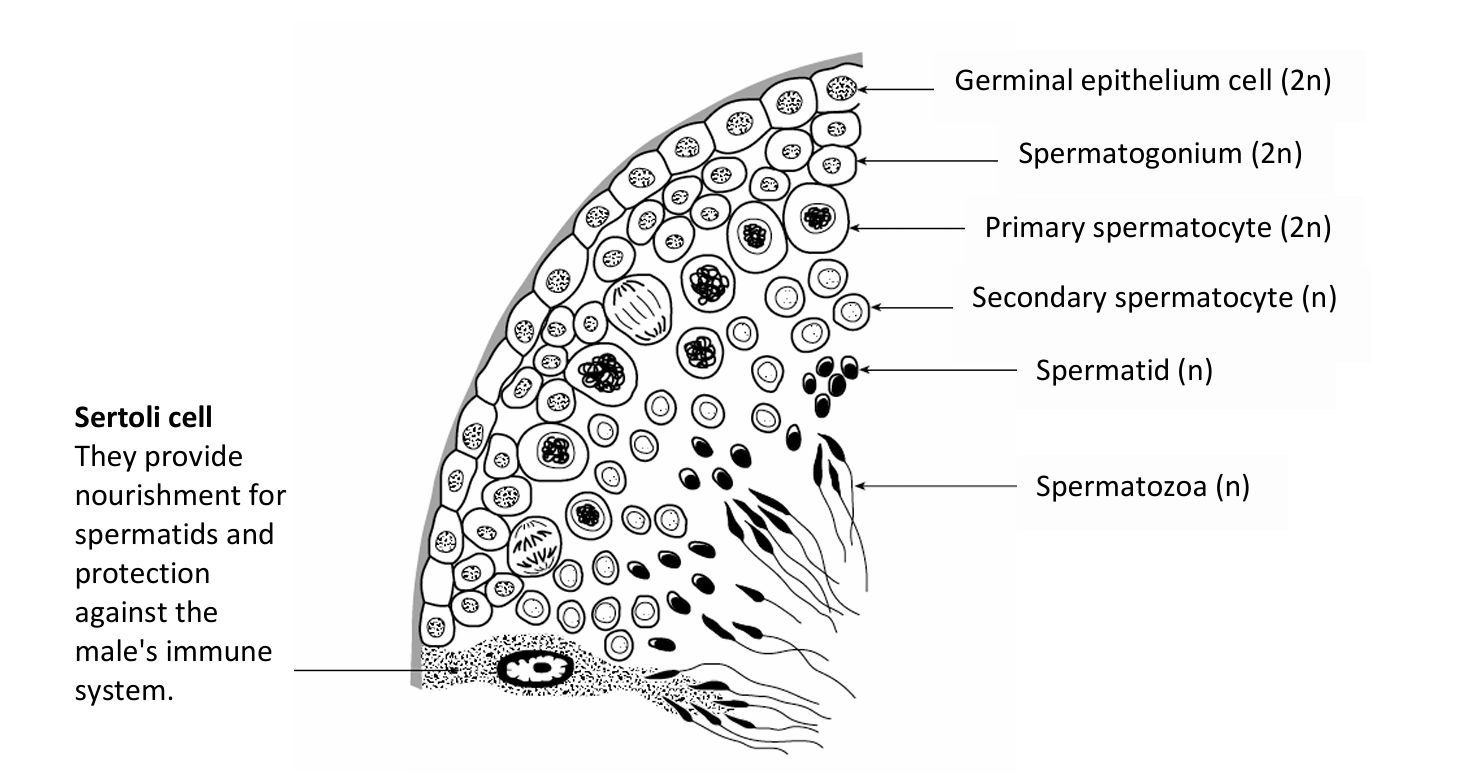
Where does spermatogenesis occur
in the germinal epithelium of the seminiferous tubules
Function of Sertoli cells
Provide mechanical support, nutritional support and immune support
Function of interstitial cells
secrete testosterone
Function of germinal epithelium
Undergo mitosis and meiosis to produce gametes
location of fimbriae
entrances of oviduct funnel
Function of fimbriae
Sweep secondary oocyte into the oviduct
Location of ciliated epithelial
Lining the oviduct
Function of ciliated epithelial
Convey the secondary oocyte to the uterus
Location of endometrium
Innermost layer of uterus
Function of endometrium
Secretes mucus to aid implantation
What lines the basement membrane inside the seminiferous tubule
spermatogonia
What kind of cell is spermatogonia
stem cells
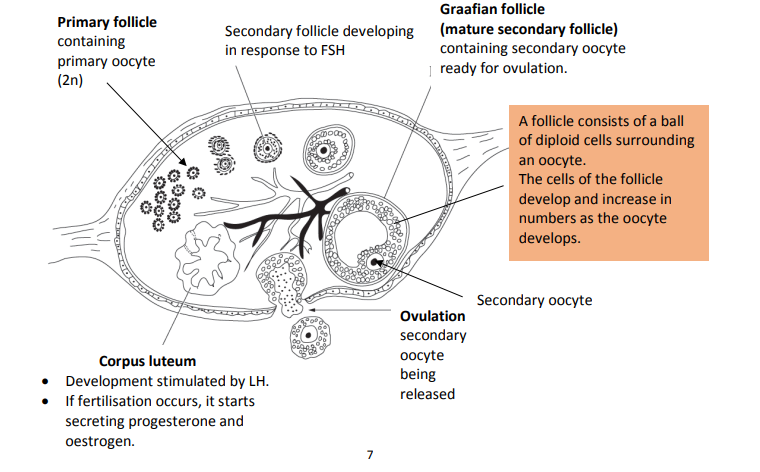
Outline what happens in oogenesis before birth
1) Cells of the germinal epithelium of the ovary, which are diploid, divide by mitosis to make diploid oogonia and more germinal epithelium cells.
2) The oogonia divide many times by mitosis and enlarge, making diploid primary oocytes and more oogonia
3) The primary oocytes begin meiosis I but are arrested in its progress at prophase I
4) Germinal epithelium cells divide to form diploid follicle cells which surround the primary oocytes, making primary follicles
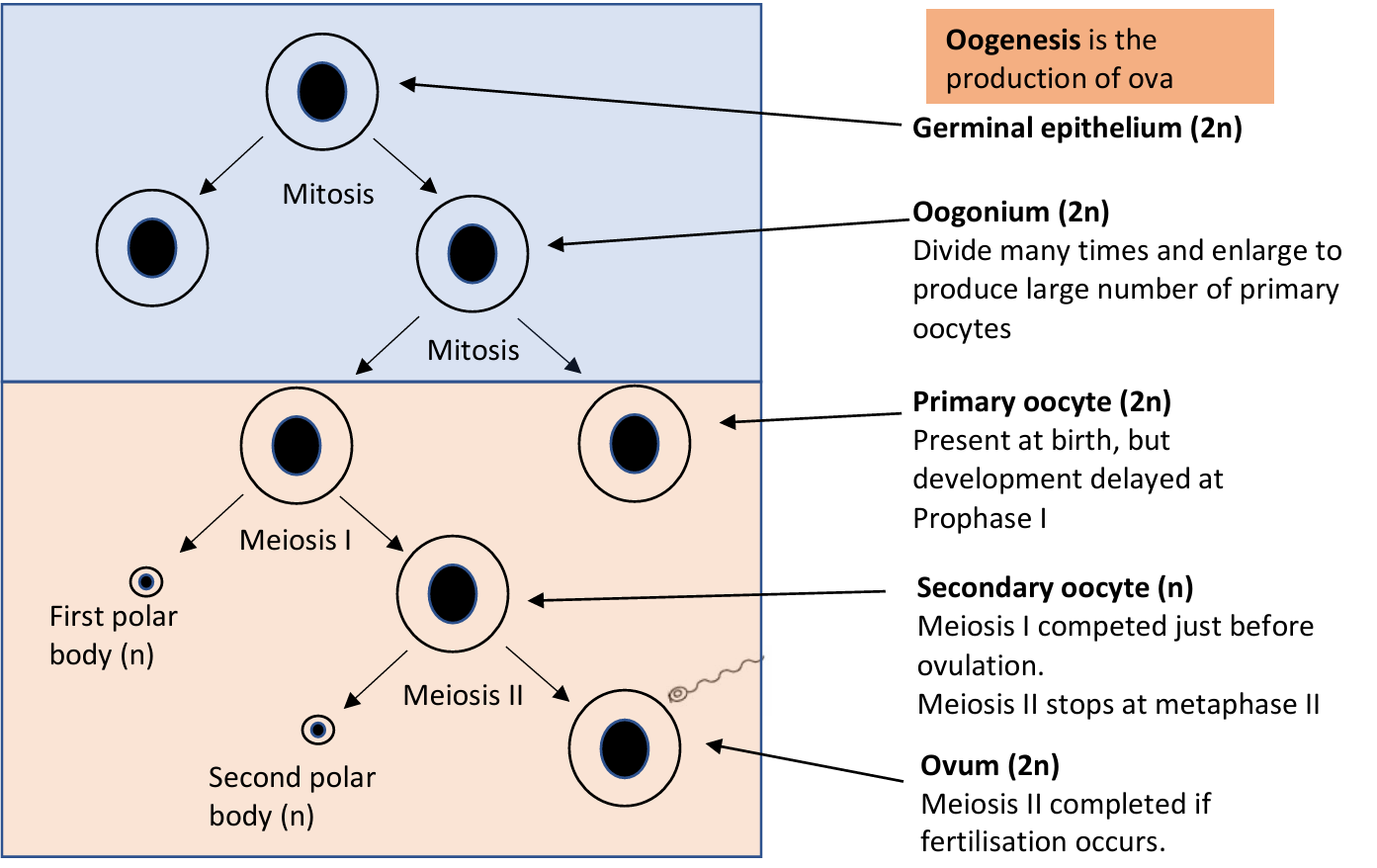
Outline the stages of oogenesis after puberty
1) Hormones stimulate the primary follicles to develop further. A primary oocyte completes meiosis I, making a secondary oocyte. The other product is the first polar body.
2) The primary follicle develops into a secondary follicle. It migrates to the surface of the ovary where it bursts and releases the secondary oocyte, in a process called ovulation
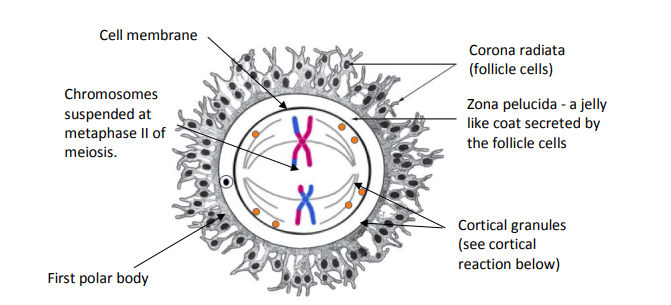
3) The secondary oocyte begins meiosis II but stop s at metaphase II unless fertilisation takes place
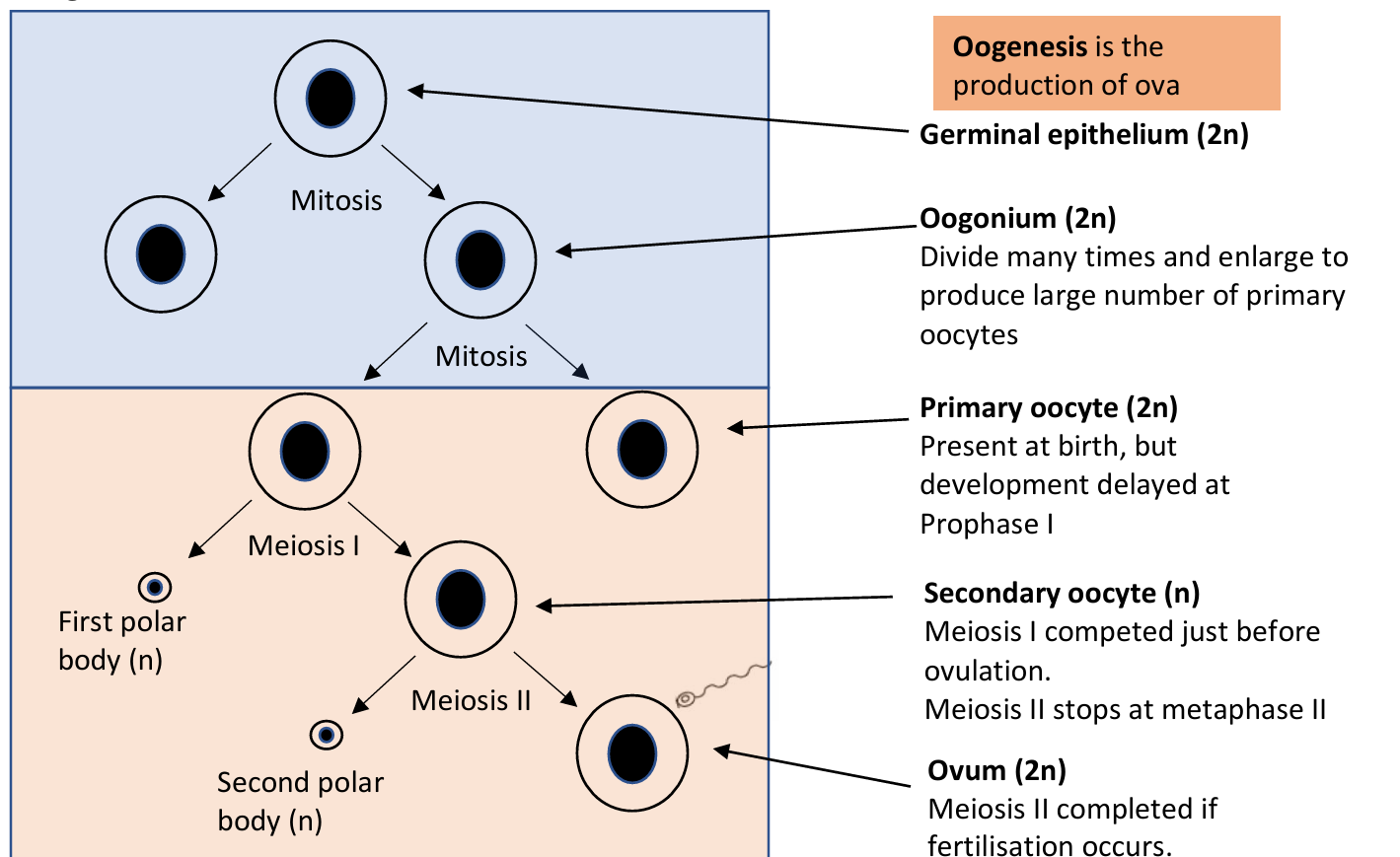
Outline the stages of oogenesis after fertilisation
Meiosis II is completed, making an ovum containing most of the cytoplasm. The other product of meiosis II is the second polar body
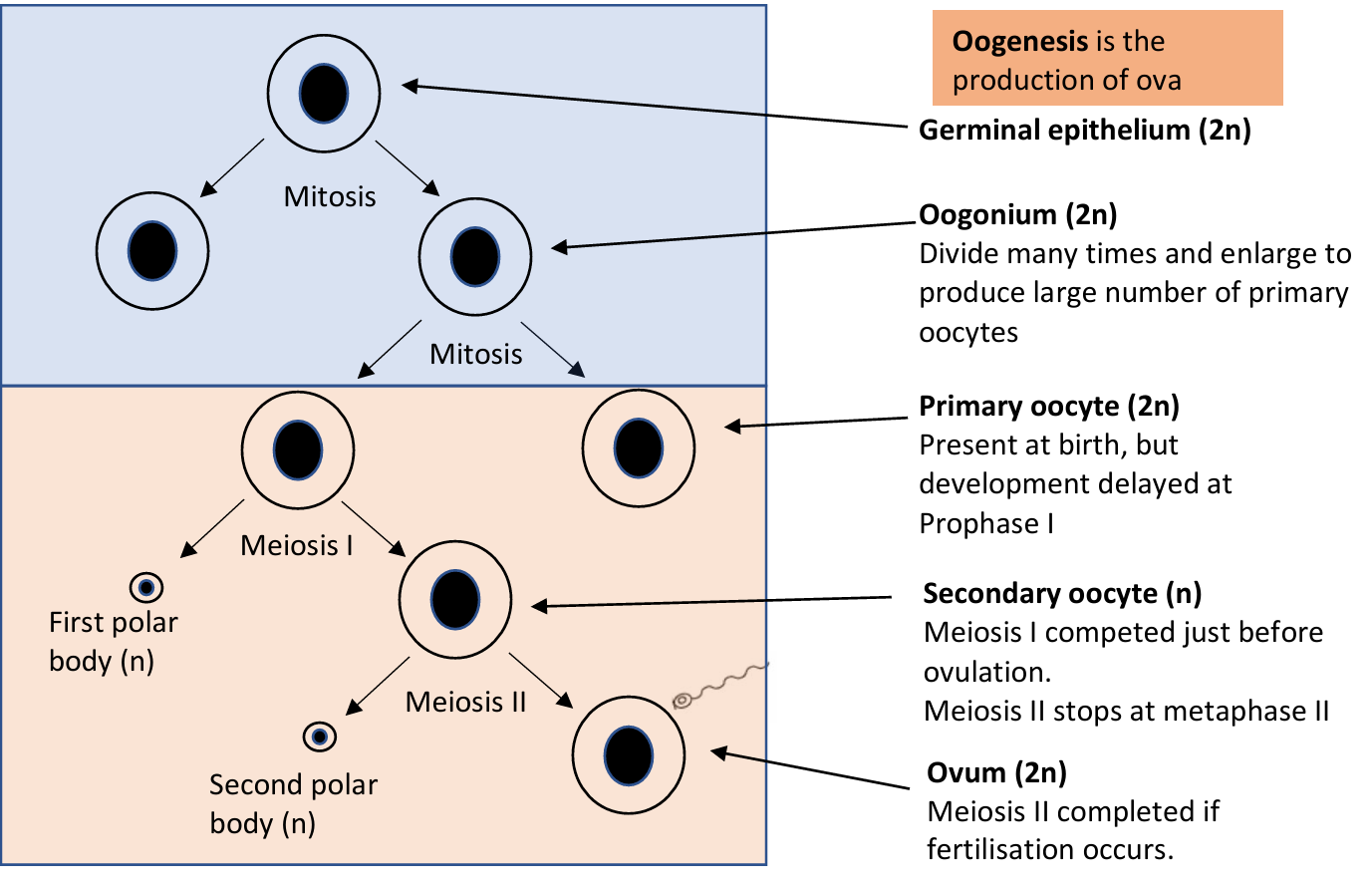
Outline the stages of oogenesis after ovulation
The mature secondary follicle (Graafian follicle) becomes the corpus luteum (yellow body)
What usually happens to the first polar body
disintegrates immediately
What's the germ cell in females called
oogonium
Where does fertilisation take place
in the fallopian tube
What process needs to happen before a sperm cell can fertilise a secondary oocyte
Capacitation
Describe what occurs in capacitation
Cholesterol and glycoproteins are removed from the cell membrane over the acrosome of the sperm head.
The membrane is thinned becomes more fluid and more permeable to calcium ions
The tail motion changes to a whipping motion, increasing sperm motility
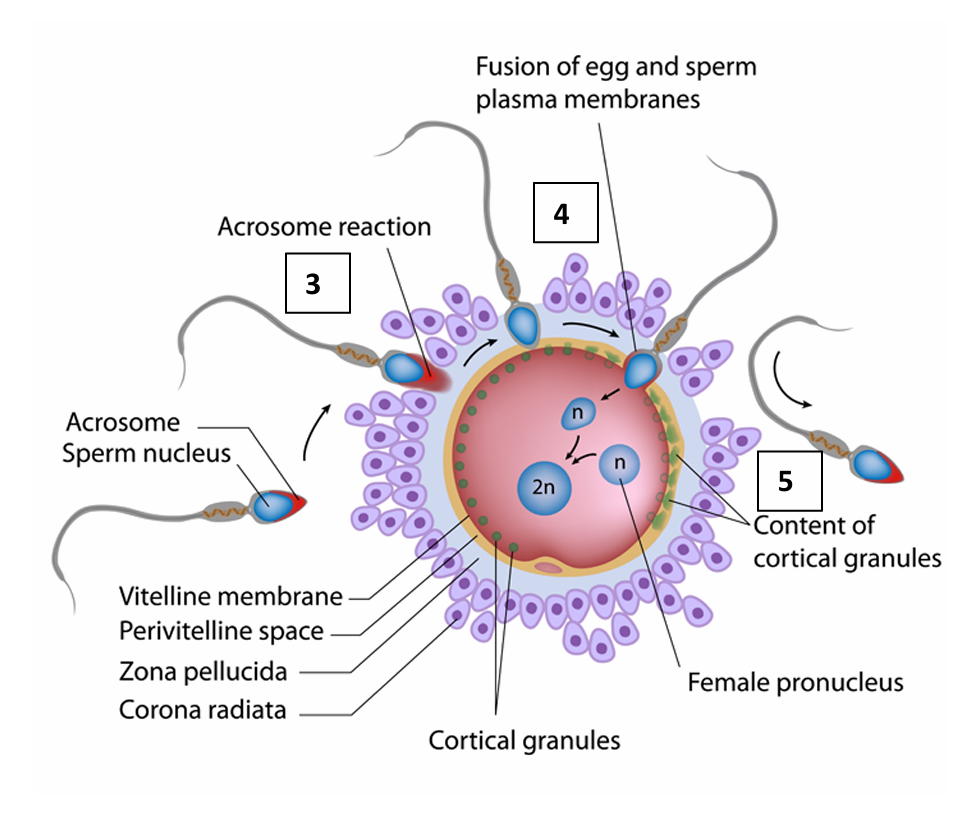
Describe the acrosome reaction
Sperm bind to receptors in the zona pellucida which initiates the reaction
The acrosome releases several lysosomal enzymes which digest the cells of the corona radiata.
Then on contact with the zona pellucida, the acrosome membrane ruptures and releases more lysosomal enzymes which hydrolyses the zona pellucida
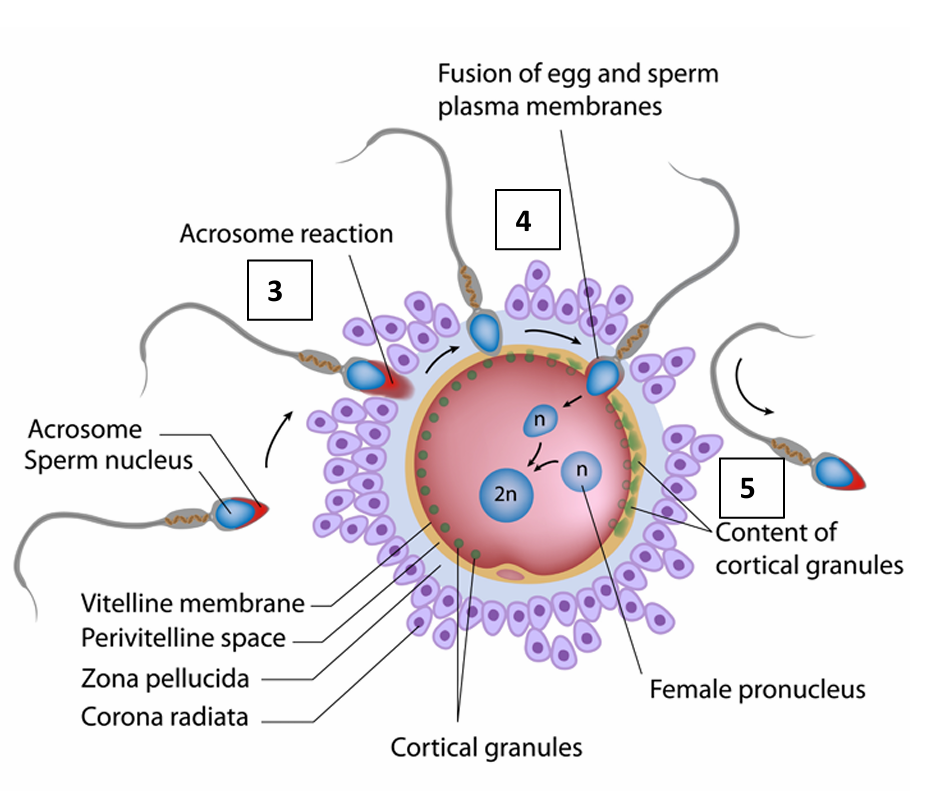
Name on enzyme that is releases from the acrosome rupturing
acrosin
What are the 2 protective layers the sperm must penetrate
Corona radiata and the zona pellucida

State the outcome of the acrosomal reaction
a single sperm contacts one of the sperm binding receptors on the oocyte’s plasma membrane
The plasma membrane of the sperm fuses with the plasma membrane of the oocyte.
The sperm nucleus is transferred to into the secondary oocyte
The completion of the second meiotic division of the oocyte nucleus occurs
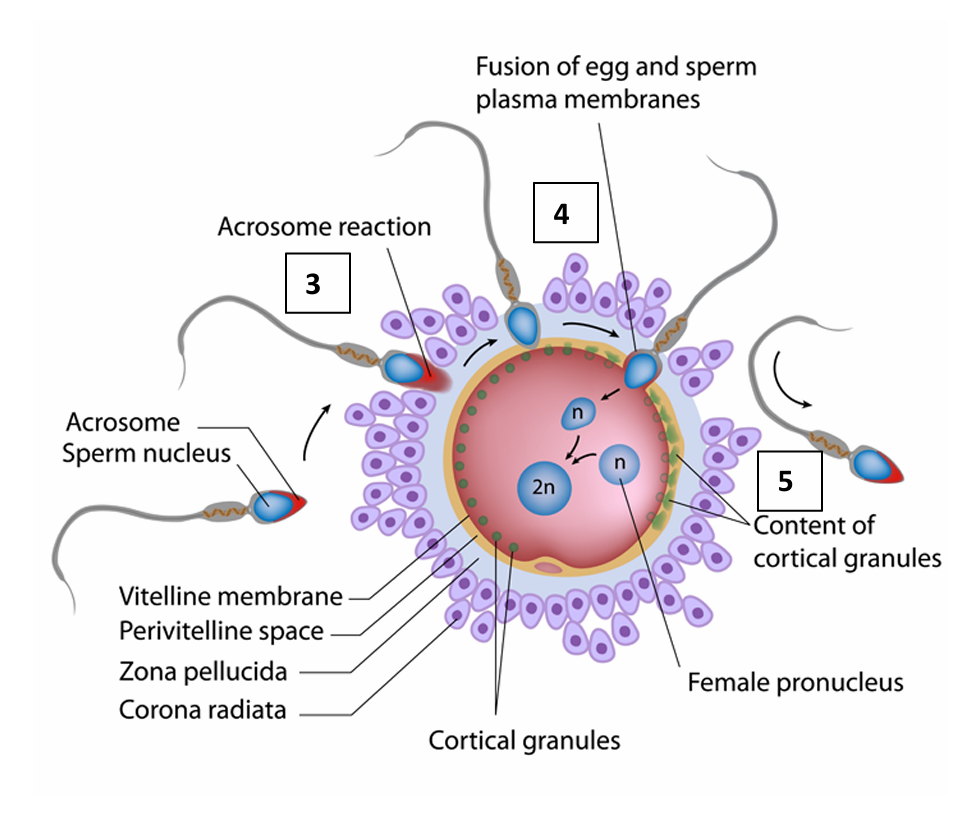
After the entry of the sperm head what is the secondary oocyte called
ovum
How does the oocyte prevent polyspermy
Cortical reaction
Produces a fertilisation membrane
The oocyte’s smooth ER releases calcium ions into the cytoplasm
Cortical granules fuse with the cell membrane and release their contents of enzymes.
The zona pellucida hardens and expands
What does the fusion of the ovum and sperm form
diploid zygotic nucleus
Define polyspermy
Entry of additional sperm
How is the zygote projected toward the uterus
by peristalsis and beating cilia
What results in the zygote having more cells
Cleavage
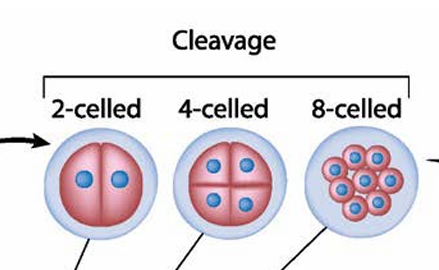
What is each daughter cell that is produced by cleavage is called
blastomere
What is the name given to the structure made by the 16-cell embryo that reaches the uterus
morula

Once inside the uterus what does the morula do
it secretes fluid
organises around a fluid filled cavity, the blastocoel
What is the name of the morula after it organises around the blastocoel
blastocyst
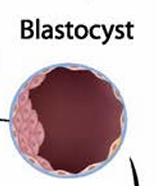
What does the group of cells within the blastocyst form
inner cell mass
What is the name of the cells that from the outer layer of the blastocyst
trophoblast
What do the trophoblasts develop into
the chorionic sac and the foetal portion of the placenta
The inner mass of embryonic cells is …… in implantation
totipotent
Define totipotent
Each cell has the potential to differentiate into any cell type in the human body
How do the outer layers of the blastocyst grow into the endometrium
by digesting the endometrial cells and wound healing of the endometrium to close up the blastocyst into the tissue
What does the chorion layer of the blastocyst release
Human chorionic gonadotropin
What does HCG do
keeps the corpus luteum active
Structure of Female Reproductive System
Structure of Male Reproductive System
Structure of Ovary
Structure of Secondary oocyte
Structure of Blastocyst
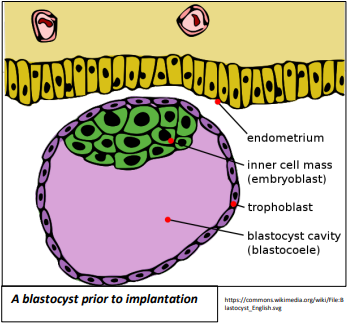
State the function of trophoblastic villi on the blastocyst
increase surface area for the absorption of nutrients from the endometrium
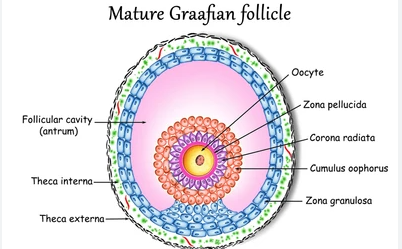
Structure of Graafian follicle
How does the placenta connect to the conceptus
umbilical cord
In the umbilical cord , what is deoxygenated blood and metabolic waste carried through
Through two umbilical arteries away from the foetus
In the umbilical cord what is nutrients and oxygen carried through
The single umbilical vein returning to the foetus
What does the trophoblast develop into
The amnion and chorion
What does the chorion develop
finger-like processes called chorionic villi
Properties of the chorionic villi
Microvilli which increase surface area
Thin walls for a short diffusion distance
Counter current flow between the foetal and maternal blood which maintains a concentration gradient.
How does the foetal and maternal blood not commingle
Blood cells cannot move across the placenta
Why is it important that the foetal and maternal blood doesn’t commingle
Separates mother’s cytotoxic T cells from destroying the foetus
Ensures Foetal red blood cells do not enter the mother’s circulation and trigger antibody development
Why is it important that there is a physical barrier between the foetal and maternal circulation
Protects the fragile, foetal capillaries from damage by the higher blood pressure of mother.
Protects developing foetus from the changes in maternal blood pressure
Describe the placenta’s role as an endocrine gland
During the second trimester the placenta has taken over the production of oestrogen and progesterone from the corpus luteum which has degenerated
How does the placenta provide immunity to the foetus
maternal antibodies cross the placenta and attack pathogens
Where does the umbilical cord develop from
the placenta
What are hormones
Chemical messengers produced by endocrine glands
How are hormones transported
by the blood