KNPE 335 Week 8-12
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
157 Terms
Neurodiversity (ND)
Identities of people with ND are diverse and include those with intellectual and/or developmental disability, autism spectrum disorder (ASD), fetal alcohol spectrum disorder (FASD), Down syndrome, among other conditions.
Interlocking oppressions
Ways in which social identities associated with categories of difference (ie. race, class, ability, gender, and age) interact to produce unique experiences of oppression and/or privilege
What are the consequences of social exclusion of people with neurodiversity?
More likely to live in poverty
Limited housing options and a lack of opportunity to engage socially
How does COVID-19 affect older adults with ND?
narrow focus on biomedical approach to care, so psychosocial needs were largely overlooked
redeployment of service providers to other sectors
lack of specialized knowledge and integrated services
How does COVID-19 affect the carers of older adults with ND?
restrictions created stress for family carers who could not enter sites to support their loved ones
Significant increase in the hours/types of care provided by family members living with an older adult with ND due to reduction of services
Recommendations for treatment of older adults with ND
Create mechanisms for collaboration between different sectors
Include older adults with ND and their family carers at the decision-making table
Move beyond physical health and functioning and prioritize emotional, psychological, social, and recreational responses and social inclusion
Consider respite an essential service
Create initiatives for service providers to debrief/discuss their work with older adults with ND and share strategies
Provide psychological, social, and emotional support to carers
Older immigrants
include people who have recently arrived in Canada, who have been here more than five years ago, and those who have aged here after spending most of their adult lives in their adoptive society
3 trends for older immigrants in Canada (from reading)
Large proportion of elderly were born abroad (larger % than the total population), however among new and recent immigrants, older people account for a relatively small proportion
There is great linguistic diversity among elderly immigrants, with most having a mother tongue other than French or English.
Nearly 40% of Canadian older immigrants identified themselves as a visible minority
Why is the cut off of “older adults are aged 65+” adhered to less strictly in racialized or ethnocultural minorities?
processes of marginalization and exclusion (including poverty and lack of access to care) often lead to premature aging
Premature aging
term that underlines the high rates of morbidity and mortality in marginalized communities
Immigrant
a person who is, or has been, a received immigrant or a permanent resident.
nonimmigrant
a Canadian citizen by birth
non-permanent resident
a migrant: a person from another country who holds a work or study permit, or a person applying for refugee status
recent immigrant
a person who has obtained the status of a registered immigrant or permanent resident in the past five years
Factors contributing to loneliness and social isolation
living alone
being 80 years of age or older
compromised health, including multiple chronic health problems
not having a child or contact with relatives
having a low income
poor knowledge of English or French
the evolution or breakdown of family structures
being abandoned by young people who migrate in search of work
life-critical transitions, such as retirement or the death of a spouse
ignorance of government services, community programs or appropriate transportation, or difficulty in accessing them
Acting as a caregiver
Which specific factors contribute to social isolation in elderly immigrant in Canada?
Older immigrants go through the cracks (don’t fit well into immigration or senior services)
limited access to services
financial precariousness
Being forced to work beyond retirement age
elderly immigrants often support family in their home country
affordable housing issues
increased risk of being displaced or confined to unsanitary housing
What are the consequences of the rights of older adult immigrants to social participation and inclusion being undermined by policies?
economic precariousness, housing instability, family breakup, social isolation
Health inequity
unjust or unfair differences in health between persons, often rooted in social, economic, environmental, or systemic conditions that disadvantage certain groups
Preventable
Health inequality
Observable or measurable (quantifiable) differences in health status or outcomes among different population groups
not necessarily “unfairness”
Diversity with aging
As people age, experiences of health, support, and well-being vary based on social determinants of health, which can lead to health inequalities
Health inequalities with aging
Measurable differences in health outcomes among older adults in various groups, such as varying levels of mobility, cognitive health, or life expectancy
example: rural vs urban adults
Health inequities with aging
Stem from lifelong disadvantages, such as poverty, racism, or limited access to healthcare, which effect older adults later in life.
social determinants of health
Includes income, housing, education, job opportunities, affects life expectancy
How do the SDOH affect older adults health?
Older adults living in disadvantaged areas have less access to health care
Disadvantaged groups have higher mortality and lower survival
Inequalities related to survival from various health conditions (i.e., cardiovascular event) are closely related to age, sex, ethnicity
What are the vulnerable and disadvantage older adult groups from the “Who’s at risk and what can be done about it” project?
Risk factors related to health inequality and health inequity both influence older adults' risk for social isolation

The opposite of a risk factor is a […]
The opposite of a risk factor is a protective factor.
example: not having access to affordable housing is a risk factor; access to affordable housing can protect against the risk of social isolation.
What are the examples of health inequities for older adults in Canada?
Indigenous people
Immigrant older adults
Low-income older adults
Oral health
Older adults who are caregivers
Older adults in rural/remote area
Dementia care
Prescription drug access
What was the health of Indigenous people like before colonization?
Were in good health prior to colonization
Included nutritious diets, rich and diverse healing systems, and active lifestyles
How did contact with European settlers affect health outcomes of Indigenous people?
Have poorer health outcomes
Suffer from more chronic illnesses and disabilities, including heart disease and diabetes
increased type 2 diabetes levels
Why did colonization affect the health of Indigenous people?
New illnesses were introduced
Indigenous healing processes were banned
Indigenous economy collapsed
Residential schools
Unequal access to healthcare
Systemic discrimination, racism, and loss of support systems
Who is at increased risk of dementia?
Certain ethno-racial groups (Black, Hispanic/Latino, Native Hawaiian/Pacific Islander) have higher risks of developing Dementia
differences persist despite similar rates of cognitive decline across groups
Risk and expression of Dementia are influenced by […], […], and […]. Influential factors include […], […], and […].
Risk and expression of Dementia are influenced by social determinants, discrimination, and access to care. Influential factors include socioeconomic status, cultural diversity, and geographical location
There are disparities in […], […], and […] in dementia care
There are disparities in access, diagnosis, and outcomes in dementia care
How are the 12 risk factors for dementia influced by health inequities?
Individuals from marginalized or lower income groups face barriers in managing the 12 risk factors
more health inequities decreases the ability to manage risk factors that contribute to dementia
What are the health inequities in prescription drug access?
Public health doesn’t cover prescription medications, causing inconsistent access to medications, leading to health inequities and social injustice
Who is affected by health inequities in prescription drug access?
disproportionately affects those without private or provincial coverage
People with private insurance or provincial drug benefit plans (e.g., older adults, people with disabilities) may have better access to medication coverage
Many vulnerable Canadians (e.g., older adults, Indigenous people, immigrants) struggle to afford medications, leading to poor adherence & health outcomes
What are the health inequities in oral health?
Oral health coverage often not included in provincial health plans, so many older adults avoid dental care because of high costs
Poor oral health impacts older adults’ overall health:
lost or broken teeth negatively affect nutritional status
Pain and stigma around poor oral appearance affect mental health
How does the caregiver role affect older adults?
Increased burden, depression, stress, financial problems, poor health, loneliness & social isolation
Spousal caregivers at greater risk of experiencing loneliness and decreased social support
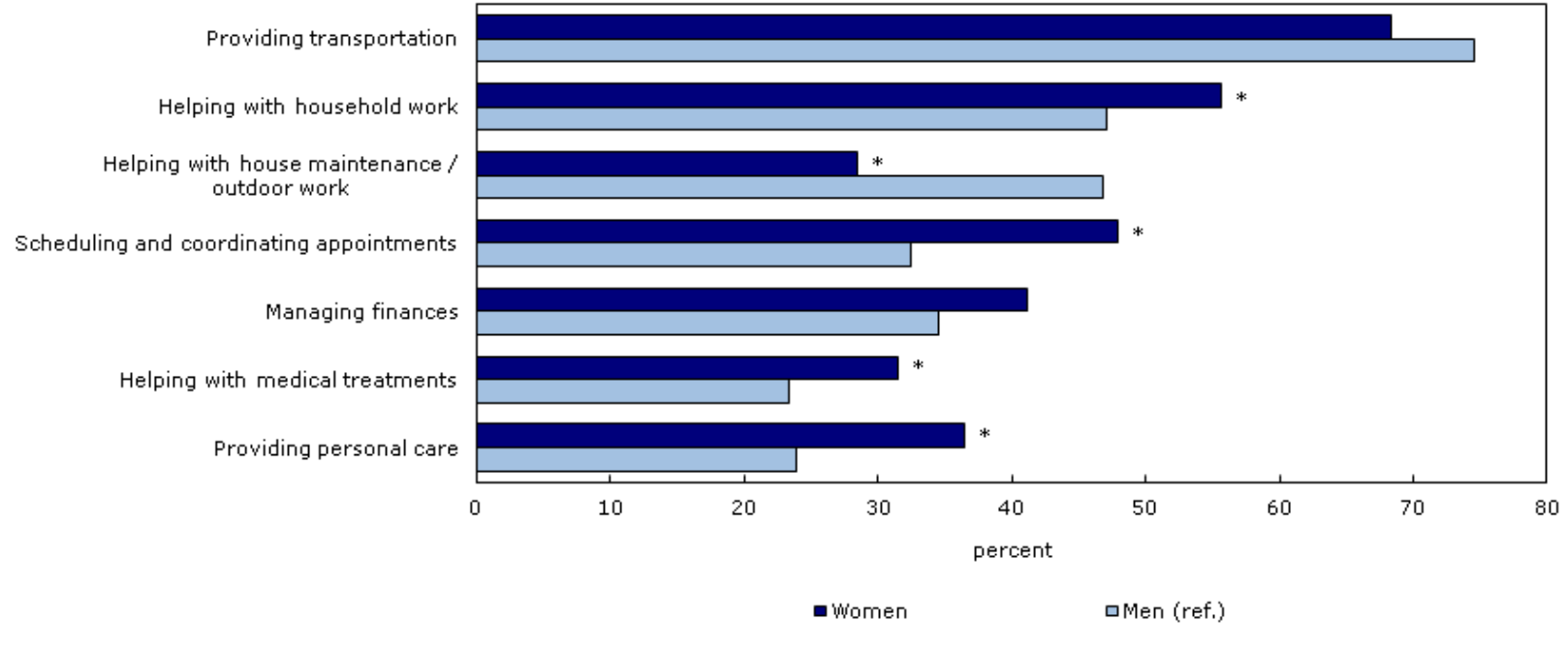
Which demographic affects seniors caregiving activities?
Seniors’ participation in caregiving activities varies by sex
Female caregivers face more health inequities than males
What are the interventions to improve health outcomes for older adult caregivers?
Education and skills training
Interactive online activities and group
Physical and financial support through informal assistance
Psychological Support
Respite services
Home care or related services
Income and tax relief programs
What has been found for immigrant older adults in Canada (from lecture)
Older immigrants are lonelier than Canadian-born older adults
immigrant older adults had lower prevalence of successful aging than their Canadian-born peers
Other research has found a “healthy immigrant effect” within Canada - meaning immigrants are generally healthier than domestic-born Canadians when they first arrive
Inclusive healthy aging interventions for Immigrant older adults in Canada
Additional data collection and research on immigrant older adults in Canada
Culturally and linguistically appropriate programs and services
What were the recommendations from the case study of the report titled “Learning from the lived experiences of aging immigrants” ?
making public transportation, health, and support systems more accessible
completing outreach sessions and education with older immigrants
creating user and aging-friendly communities specific to the needs of older adult immigrants
What are the health inequities in older adults in rural/remote areas?
Increase risk of social isolation, smaller support networks, greater loneliness, and lower utilization rates of health & social services
Higher rates of mental health concerns, chronic diseases, & worse general health
Rural older adults face increased risk of morbidity, obesity, diabetes, coronary heart disease, cancer, COVID-19, and excess mortality
What are the 6 strategies for improving healthy aging in rural and remote areas?
Reducing health inequalities by providing better access to health and social care services in rural areas
Joining transport, housing, health and social care services
Developing cost-effective transport
Improving housing and local environment to allow older people to 'age in place'
Developing volunteer and community-based initiatives to improve social integration of older adults
Stimulating social enterprises and collaborative ventures to improve the economic diversity and attractiveness of rural areas
What is the trend for low-income older adults?
Older adults are one of the most financially vulnerable populations, and the % of low-income older adults is increasing
Which older adults are at increased risk of being low-income?
less education
intermittent work histories and low wages
older immigrants
Indigenous older adults
those with chronic health conditions
those with disabilities
What are the health inequities of low-income older adults?
Increased risk of loneliness, social isolation, lower quality of life, poor health outcomes, and premature mortality
High-income experience considerably more years of good health
What are the programs and services to help low-income older adults in Canada?
Income assistance, disability assistance or hardship assistance for low-income seniors who don't qualify for public pension programs
Provincial and territorial programs (e.g; property tax deferment, prescription drug subsidies, rental subsidies)
Residential Rehabilitation Assistance Program (RRAP) for affordable housing for low-income seniors and adults with disabilities.
Advanced life deferred annuities (ALDAs)
Variable life payment annuities (VPLAs) to ensure retirees have income at older ages.
What are the 3 factors for healthcare professionals to consider when increasing cultural competence in healthy aging?
Awareness, Knowledge, Skills
What are the 4 components of culturally sensitive healthcare?
Professionals should have cultural competence
Focus on under-served needs
Use patient-centered care and increase patient health literacy
Cultural targeting in care
U-curve of happiness
People are happiest at the beginning and at the end of life. As people grow old, they fear death less.
Age-related stereotypes
Cognitive structures embedding beliefs and expectations about different age stages
include assumptions and generalizations about how people at or over a certain age should behave
Explicit attitudes
Previously learned information that is consciously endorsed or believed
direct and deliberate and can be acknowledged
Implicit priming
Associations outside of conscious awareness; unconscious and effortless, indirect and automatic and involuntarily active
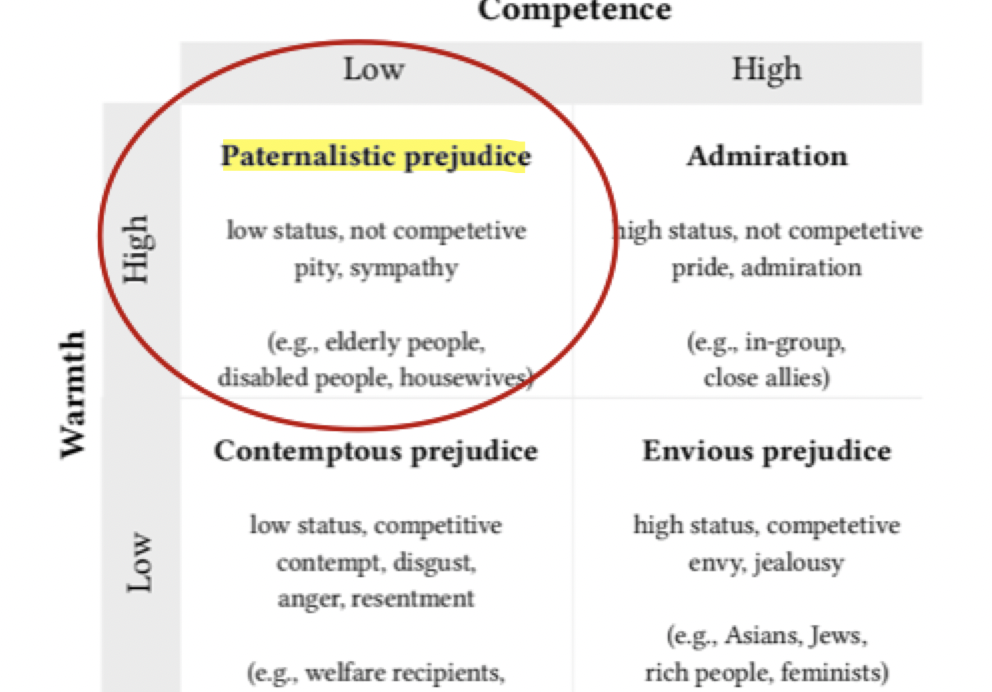
Stereotype content model (SCM)
All group stereotypes and interpersonal impressions form along two dimensions
warmth dimension: based on the notion that people are evolutionarily predisposed to first assess a stranger's intent to either harm or help them
Competence dimension: to judge the stranger’s capacity to act on that perceived intention
Where do older adults fall in the stereotype content model?
older adults are seen as paternalistic prejudice - high warmth and low competence
What do the results of the case studies by Stone & Baker (2017) and Barber et al. (2020) reveal?
When primed with positive stereotypes about older adults stair usage, they are more confident, quick, and efficient. However, stereotype threat can impair older adults’ physical performance when they are primed with negative stereotypes.
Ageism
how we think (stereotypes), feel (prejudice) and act (discrimination) towards others or ourselves based on age
Everyday ageism
occurs in day-to-day lives through interpersonal interactions and exposure to ageist beliefs, assumptions, and stereotypes.
What are the 3 dimensions of ageism?
Cognitive (stereotypes): How we think about aging and older adults
Emotional (prejudice): How we feel about getting older/older adults
Behavioural (discrimination): Actions in relation to aging, getting older and older adults
What are the meso + macro affects of ageism?
Workplace: ageism affects financial security and mental health from discrimination in the workplace
Healthcare: communication, diagnosis and treatment decisions
Media: negative portrayals, underrepresentation, and framing aging as the problem
Legal system: ageism language, age restrictions, and accessibility
How does ageism affect health?
Ageism shortens older adults’ lives
Increased social isolation and loneliness
Lower quality of life
Decreased mental health
Poor physical health
Delay in injury or illness recovery
What are the consequences of ageism?
Ageism costs society billions of dollars
Ageism causes conflict between generations
Ageism causes loss of productivity in the workplace
Ageism causes elder abuse
How does media portray older adults?
96% positive portrayal for individuals under 50 years old but only 72% positive portrayal for individuals 50+ years old
Only 15% of images in the news are of individuals over 50+ years old
in Disney only 39% of older adults had major role and many portrayed as negative
How does the beauty standard portray older adults?
Idea of “defeating aging”
Beauty norms focus on youth, aging is associated with loss of beauty, especially for women, and increases exposure to ageism
Autonomy debate: people should have the 'choice' to look younger if they want to vs "is that actually what they want or is that just what society influences them to want”
Grey hair effect
older men with grey hair are viewed favorably, whereas woman with grey hair are viewed as old, not beautiful, not worthy, etc
Categories of everyday ageism
Exposure to ageist messages
Ageism in interpersonal interactions
Internalized ageism
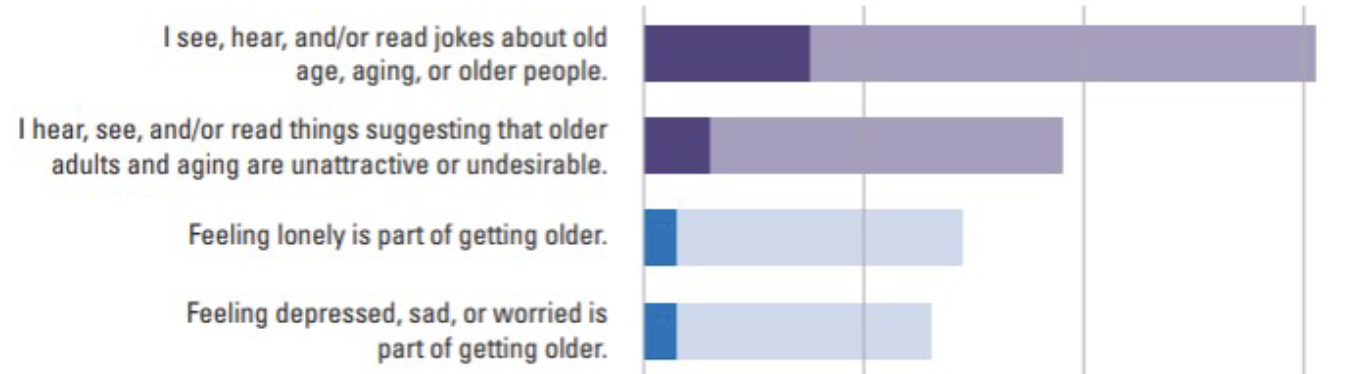
What are the 4 most common exposures of ageism in society (in order from most to less common)?
jokes about old age, aging, or older people
things suggest that older adults are unattractive or undesirable
Feeling lonely is part of getting older
Feeling depressed, sad, or worried is part of getting older.
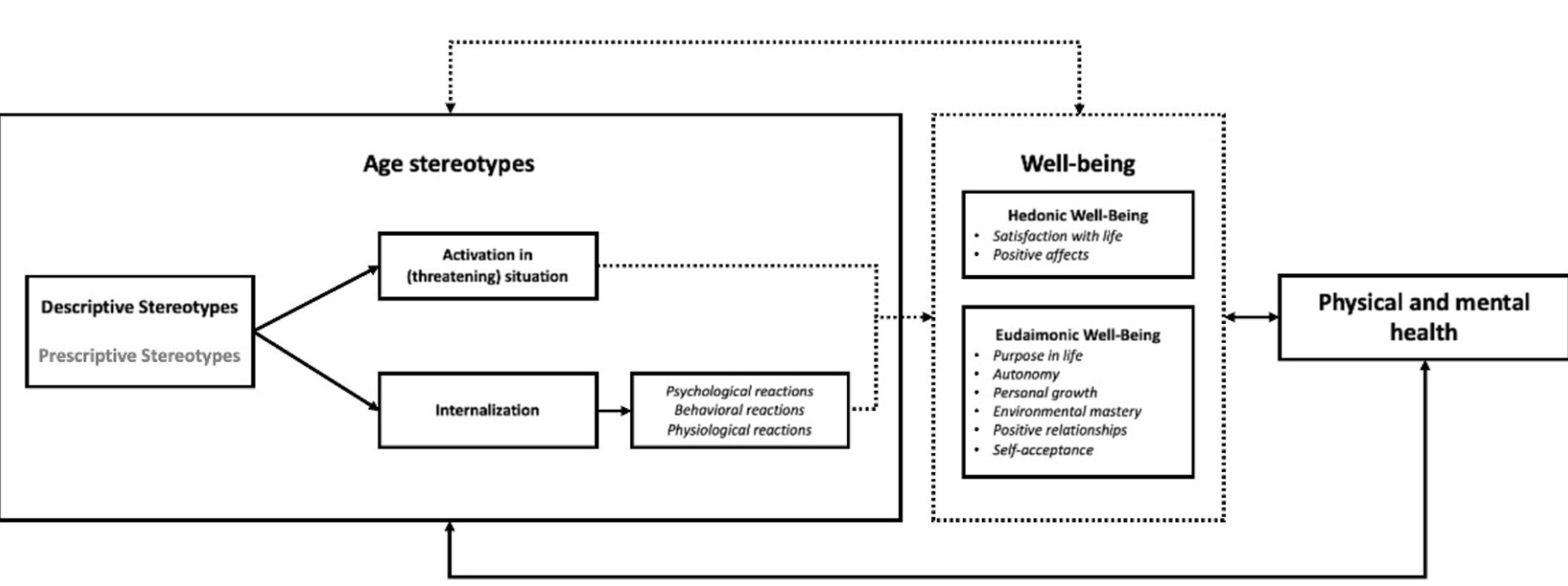
How are stereotypes and ageism related to our course in a broad perspective?
age stereotypes influences individuals' well-being like autonomy, self-acceptance, but also physical and mental health (i.e; illness, recovery, injury)
ppl w/ cognitive issues are more likely to experience ageism and less likely to understand ageism
What are the recommendations from the WHO for combatting ageism?
Policy and Law: can address discrimination and inequality based on age and protect human rights of everyone, everywhere
Ex; Australian Age Discrimination Act
Education: activities can transmit knowledge and skills and enhance empathy
Ex; Age Well Nice program in Canada
Intergenerational interventions contribute to the mutual understanding and cooperation of different generations
Ex; grand pals
How can research combat ageism?
How can community work combat ageism?
Engage: respond to and incorporate voices of the community through participatory action research
Involve: a range of government structures (Middle-out approach & work with partners to enable effective use of resources)
Include representatives from affected communities in workshops, marketing, and feedback, create co-researchers
self-ageism
when older adults believe stereotypes and negative views about older people and aging
might lead to a “self-fulfilling prophecy”
What are the most common sources of age discrimination?
Younger people
health care professionals
government policies
employers
Discussion guide on ageism in Canada - ageism and employment key findings
Employers often believe stereotypes about older workers, which can lead to age-based discrimination in hiring and training practices.
Negative stereotypes about older workers may lead older adults to doubt their value as employees and result in them choosing to exit the workforce earlier.
The inclusion of older adults in the workforce can provide financial benefits to older adults, improve the performance of businesses, and strengthen Canada’s economy
Discussion guide on ageism in Canada - ageism and health and healthcare key findings
ageism impacts the health of older adults, it may contribute to declines in memory function, increased risk of developing dementia, and decreased life expectancy.
Ageism may lead to poor communication between health care providers and older adults, misdiagnosis of health conditions, and different recommendations for treatments
ageism costs healthcare $
What are the three pathways through which ageism may directly affect the health of individual older adults?
Psychological: Ageist attitudes become a “self-fulfilling prophecy” where people come to believe that ageist stereotypes are true.
Behavioural: When older adults accept negative stereotypes about their health, they may believe poor health is unavoidable and not engage in healthy behaviours.
Physiological: Exposure to negative stereotypes causes stress and triggers cardiovascular stress responses, which negatively impacts cardiovascular health when repeatedly triggered
Discussion guide on ageism in Canada - ageism and social inclusion key findings
Ageism is a barrier to the social inclusion of older adults.
Ageism may contribute to social isolation and feelings of loneliness experienced by older adults
Discussion guide on ageism in Canada - ageism and safety and security key findings
ageist policies and practices make houses and neighbourhoods poorly designed to meet the needs of an aging population
Discrimination in the rental market may hinder the ability of older adults to access housing.
Ageism is a risk factor for senior abuse
Discussion guide on ageism in Canada - ageism and media and social media key findings
Media play a key role in shaping the views of society and can influence younger people who may have limited contact with older adults.
Older adults are underrepresented in the media
Media may spread both negative and positive age-based stereotypes.
Both negative and positive stereotypes can be harmful to older adults, as positive stereotypes can result in unrealistic expectations
Discussion guide on ageism in Canada - initiatives to address ageism
Intergenerational programs and initiatives (ex; GeriActors, Canada homeshare)
Initiatives to support older workers (ex; Encore careers, Wage Subsidy for Older Workers)
Ageism education and awareness campaigns (ex; Global Campaign to Combat Ageism, Let’s Stop Ageism, Every Age Counts, ageism and Media Project, Anti-Ageism in the Workplace, Future Us Strategy)
Age-friendly initiatives (ex; Age-Friendly Communities Grant Program, Age-Friendly Ottawa, Allies in aging, Age-Friendly Healthcare: Interprofessional Training Program)
Intersectionality
interconnection between different social categories (e.g; race, gender, disability, etc)
How does intersectionality relate to healthy aging barriers?
Marginalized groups face additional barriers on top of the general barriers to healthy aging
What is the top perceived barrier to healthy aging?
Multi-morbidity, living with 2+ chronic conditions, was ranked the highest barrier to healthy aging, and older adults are more likely to have multimorbidity
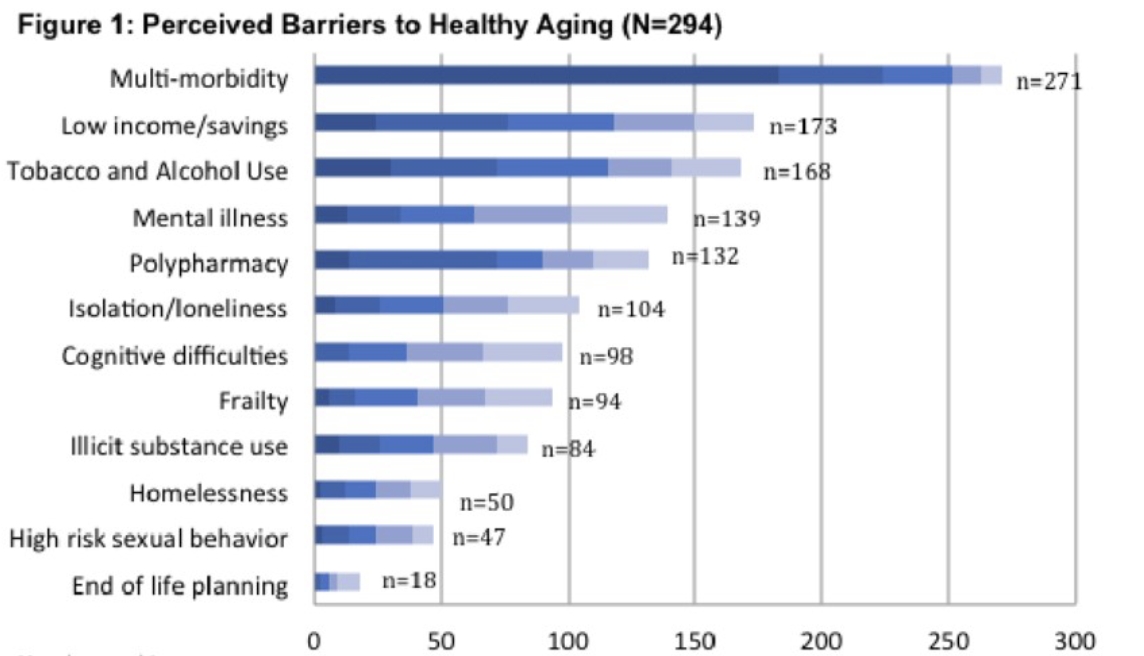
What is the least important perceived barrier to healthy aging?
End of life planning is the lowest perceived barrier to aging
Social comparison theory
Process through which people come to know themselves by evaluating their own attitudes, abilities, and beliefs in comparison with others relates to self-evaluations and self-enhancement
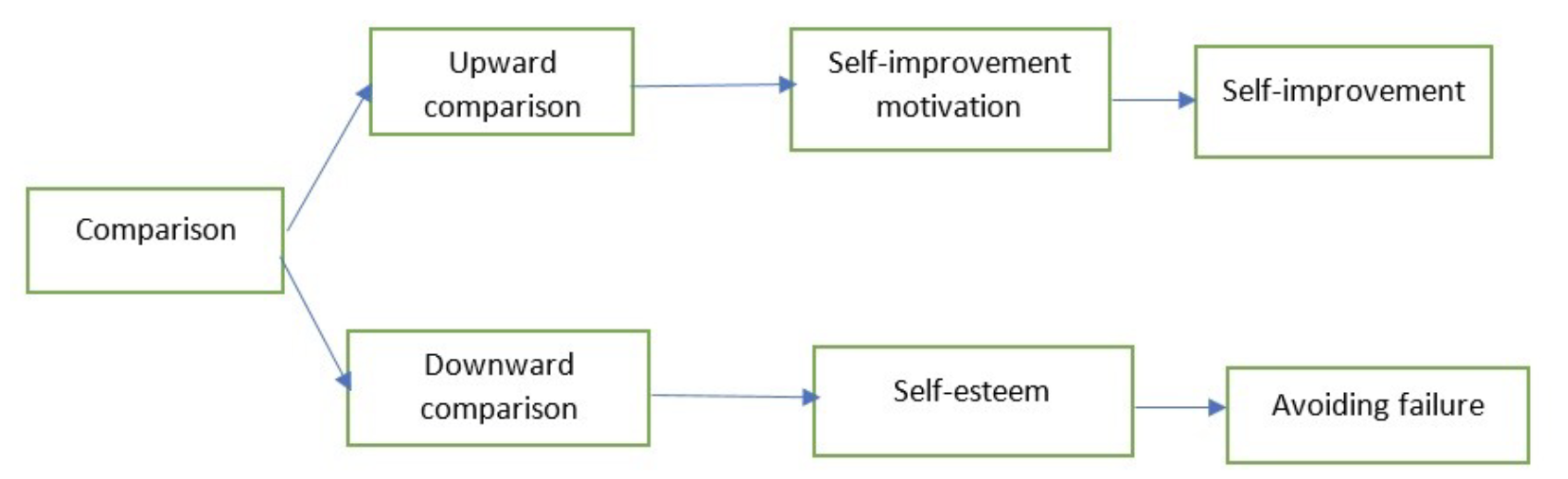
How does social comparison theory affect our own internal healthy aging?
social comparison constructs our self belief which constructs our in or out group stereotypes
By comparing yourself, you develop beliefs about yourself
Shapes which stereotypes you think you fit into
Upward comparison
Comparison to someone who appears to have things better. “You are better than me.”
Downward comparison
Comparison to someone who appears to have things worse. “I feel sorry for you.”
What are the outcomes of upward comparison?
Increases motivation for self-improvement which results in self-improvement
What are the outcomes of downward comparison?
Increase in self-esteem but also avoidance of failure (avoiding situations because you don't want to be like the person you are downwardly comparing youself to)
[…] is the most frequent social comparison
Physical health status is the most frequent social comparison
Either people with better or worse physical health status
[…] is the most impactful social comparison and is more likely to be […]
Social comparison is the most impactful social comparison and is more likely to be a positive comparison that results in better mental health outcomes
strongest result in improving health and perception of healthy aging even though its less common than physical health status comparison
Negative social comparison can also have negative impacts on health and mental health
You are more likely to compare yourself to […]
You are more likely to compare yourself to people who are more similar to you (age, race, gender) because it is easier
[…] and […] influence how you compare yourself
Social biases and stereotypes influence how you compare yourself
What are the types of barriers to healthy aging?
Physical
Social
Emotional
Spiritual
Environmental
What is a frequently overlooked barrier to healthy aging? Explain
Knowledge because a lack of understanding of healthy aging results in barriers which decreases chance of successful aging
Knowledge
Understanding of health and healthy aging, personal health status, and how to improve healthy aging
What are some physical barriers to healthy aging?
lack of exercise
poor nutrition
poor sleep
Comorbidities
illness, disability, disease, disorders
Frailty
Falls
Addiction
Age or Advanced age
Gender
Medical events