transport in humans
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
Why do multicellular organisms require transport systems
high metabolic demands - diffusion distances not fast enough
Small SA:V ratio - amount of surface available to absorb substances relatively small
Hormones and enzymes needed in different region to where they’re made
Food digested by small intestine needs to be transported to every cell for metabolic reactions
Waste products need to be removed from cells and transported to excretory organs
Describe an open circulatory system
few transport vessels
Haemolymph instead of blood - doesn’t carry oxygen or carbon dioxide and comes into direct contact with cells
Describe a closed circulatory system
blood enclosed in blood vessels
Does not come into direct contact with cells of body
Heart pumps blood through vessels under high pressure
Substances leave and enter blood by diffusion
Blood flow can be diverted
Describe the function and structure of the arteries
three layers in their wall
Tunica media contains thick, smooth muscle and elastic fibres to withstand high pressure
Carries blood at high pressure from the ventricles of the heart to tissues of boduy
Describe structure and function of the veins
three layers in walls
Thin smooth muscle and elastic fibre walls allows them to be pressed flat by muscles to carry blood under low pressure
Valves to prevent backflow of blood
Wide lumen for slow flowing blood
Carry blood at low pressure from the tissues of body to the atria of the heart
Describe the structure and function of the capillaries
single layer of endothelium
Very narrow lumen (one red blood cell wide)
Permeable walls
Carry blood through tissues
Exchange of materials between cells in the tissue and the blood in the capillary
What is the role of elastic fibres
composed of elastin
Can stretch and recoil - make vessel walls flexible
What is the role of smooth muscle
Contracts and relaxes to change size of lumen
What is the role of collagen
Provides structural support for vessels, thick collagen layer in arteries helps withstand high blood pressures
Why do artery walls require elastic fibres
withstand force of blood pumped out of the heart
Stretch to take large volume of blood
Recoil evens out surges of blood pumped from heart
Describe and explain how the wall of an artery is adapted to withstand pressure
wall is thick and contains collagen which provides strength
Endothelium is folded so no damage to it as it stretches
Describe and explain how the wall of an artery is adapted to maintain pressure
thick layer of elastic fibres , cause recoil to return to original size
Thick layer of smooth muscle, narrows lumen
Why is the lining of the arteries smooth
reduces friction so less resistance to flow
How are capillaries adapted to their function
endothelial pores between cells of the wall allows passage of small molecules from blood to tissue fluid
Walls are one endothelial cell thick so give a short diffusion pathway
Narrow lumen, red blood cells/erythrocytes pass through one at a time Which slows blood down to give more time for exchange
How are veins adapted to their function
valves prevent backflow of blood
Run between muscles so contractions squeeze veins, forcing blood towards heart
Smooth endothelial lining to allow blood to flow easily
Why do veins require valves
blood under much lower pressure than arteries
No pumping from heart and little elastic recoil in veins so blood might flow backwards as it moves towards heart against gravity
Valves prevent backflow, open as blood flows towards heart and close if it flows in opposite direction
Describe the endothelial cells of the arteries and veins
Once cell thick, flattened with a smooth surface
What are the components of the blood
Red blood cells - erythrocytes
White blood cells - leukocytes
Monocytes and neutrophils (engulfs and destroys pathogens)
Lymphocytes (produce antibodies)
Plasma
Proteins - maintains osmotic pressure
Platelets - blood clotting
Describe a monocyte
Largest white blood cell with a bi-lobed (C-shaped) nucleus
Describe a neutrophil
Faintly staining granules with a multi-lobed nucleus
Describe a lymphocyte
Large nucleus
What is tissue fluid and what is its role
Fluid forced out of the blood into surrounding space around cells
It delivers oxygen and removes carbon dioxide to respiring cells, delivers amino acids, glucose and hormones to cells
Which feature of capillaries allow tissue fluid to form
Small gaps between cells - fenestrations
Which components of the blood does not make it out of capillaries
red blood cells
Most white blood cells
Plasma proteins
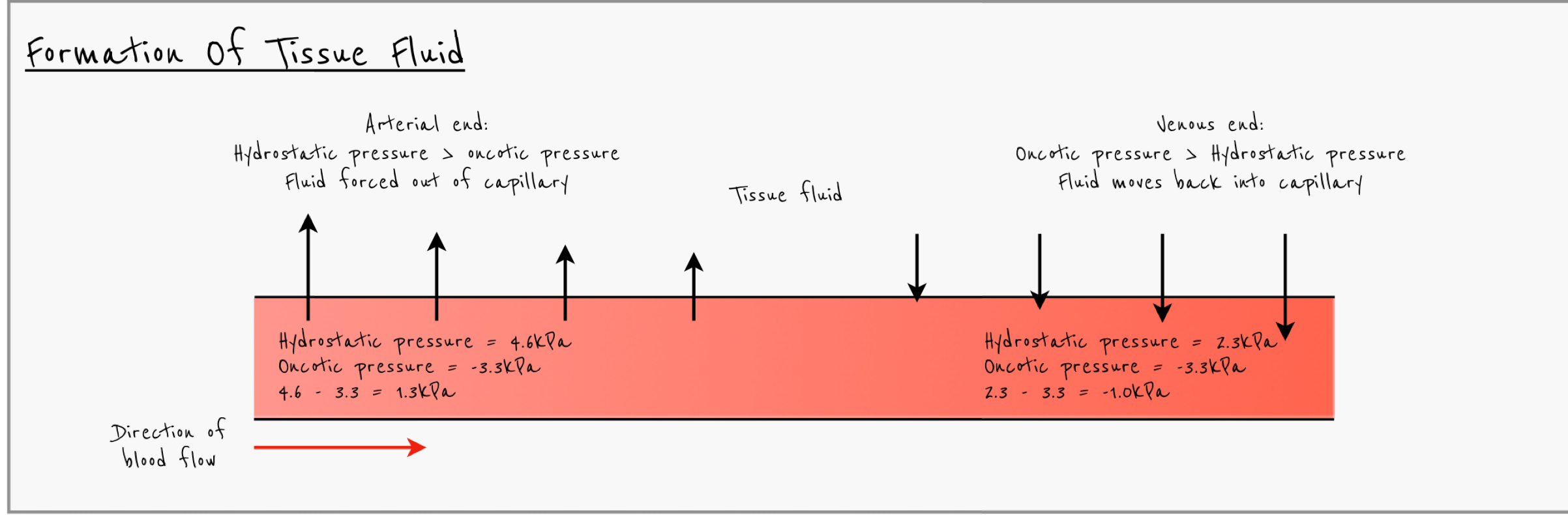
Explain how hydrostatic pressure and oncotic pressure affect the movement of fluids into and out of capillaries
hydrostatic pressure (from heart beat) forces liquid out of capillaries and is higher than oncotic pressure at arterial end of capillary so water is forced out of capillary forming tissue fluid
As blood moves along capillary more fluid moves out so hydrostatic pressure decreases and by venous end of capillaries hydrostatic pressure falls while oncotic pressure remains the same
Plasma proteins are too large to leave capillary so water potential remains constant
Water moves back into capillary by osmosis at venous end and most tissue fluid moves back into capillaries
What is lymph
The small amount of tissue fluid that does not make it back into capillaries
Describe the lymph system
lymph vessels - blind ended tubules with valves to prevent backflow
Lymph nodes containing lots of lymphocytes
Where does lymph return to the blood
Subclavian veins
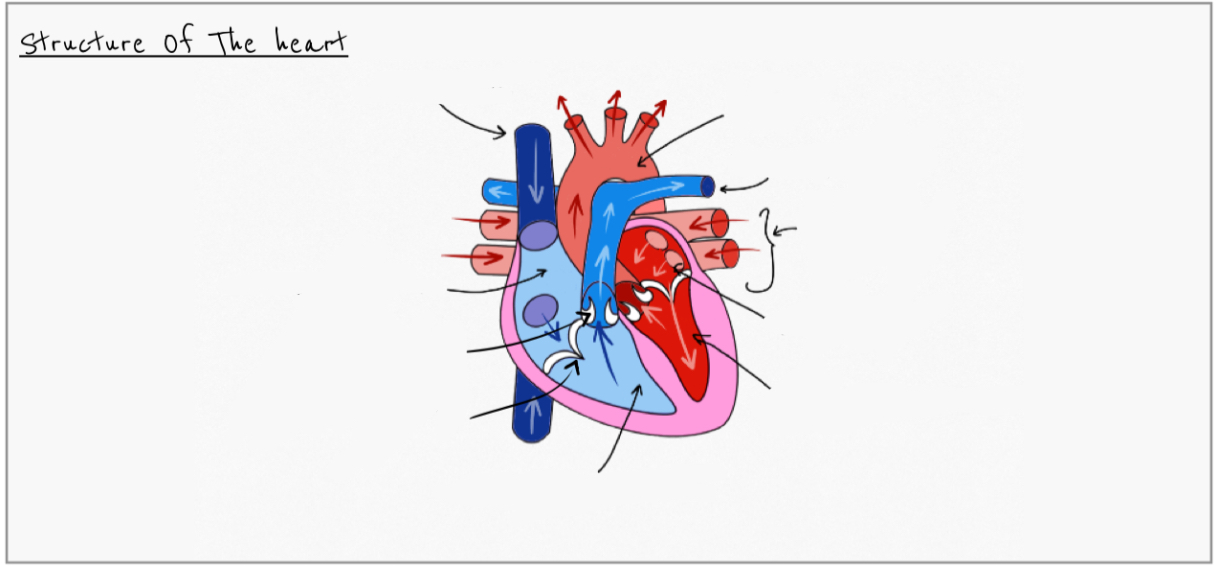
label

Explain why the left ventricle wall is thicker than the right
requires more muscle to create more force
Needs to create higher pressure to pump blood further
Right ventricle only pumping blood to lungs
To produces a higher pressure to overcome the greater resistance to flow in the systemic circulation
explain why ventricles have thicker walls than atria
atria receive blood with lower pressure as they only have a short distance to pump the blood into the ventricle
Ventricles have to contract strongly to pump high pressure blood to lungs or rest of body
what is the role of the valves in the heart
prevents blood flowing backwards and valve tendons prevent inversion
how do coronary arteries maintain a regular heart rhythm
supply blood carrying glucose and oxygen to heart
Heart cardiac muscles require oxygen and glucose for respiration
ATP from respiration needed to contract muscle with regular rhythm
Describe the structure of cardiac muscles
myogenic - can contract automatically
Coronary arteries to supply oxygen and nutrients to the heart
Valves prevent the backflow of blood
Interconnecting cells separated by intercalated discs which allows waves of electrical excitation to pass easily between them
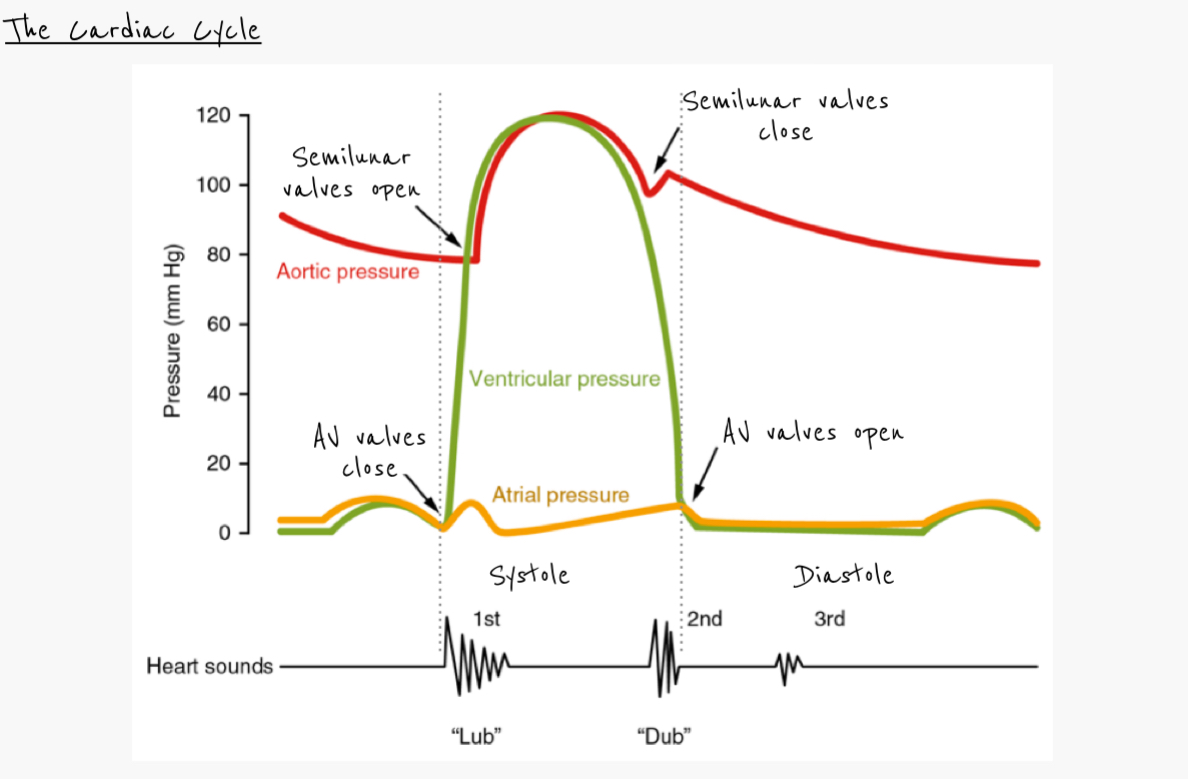
describe the cardiac cycle
Atrial systole
walls of atria contract
Blood forced from atria into ventricles via atrioventricular valves
Semilunar valves closed
Ventricular systole
walls of ventricle contract
Atrioventricular valves closed, semilunar valves open
Blood empties into arteries
Atria start to refill
Diastole
Ventricles stop contracting, pressure falls
Semilunar valves closed preventing backflow from the arteries
When ventricular pressure drops below atrial pressure, atrioventricular valves open
Blood entering atria flows into ventricles
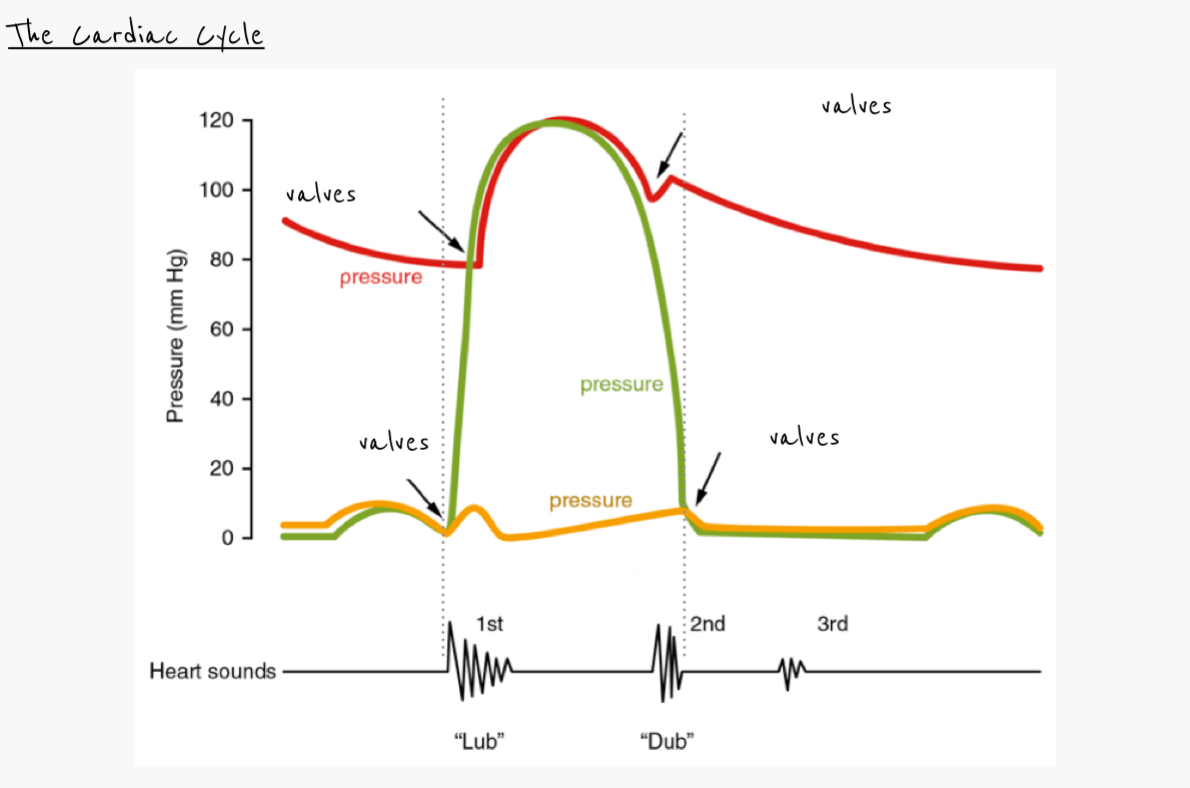
Annotate this graph
What can a blocked coronary artery lead to
Myocardial infarction
Describe diastole
Blood enters from pulmonary vein and vena cavae
Blood fills atria, pressure forces open the atrioventricular valves allowing blood to flow into the ventricles
Muscular walls of atrial and ventricles relaxed
Pressure in arteries is greater than in the ventricles
Therefore semi-lunar valves are closed
Explain atrial systole
Atrial walls contract, increasing pressure, forcing remaining blood into the ventricles
Atrioventricular valves are open
Semi-lunar valves are closed
Explain ventricular systole
walls of ventricles contract
Increases pressure in ventricles, forcing atrioventricular valves to close
Semi-lunar valves are forced open allowing blood to flow into aorta or pulmonary artery
Explain how pressure changes in the heart bring about the closure of the atrioventricular valve
Ventricular systole raise ventricular pressure
Ventricular pressure higher than atrial pressure
Valve tendons prevent inversion with the help of papillary muscles
Why does the aortic pressure remain high throughout the cardiac cycle
Thick muscle and elastic fibres in the artery wall
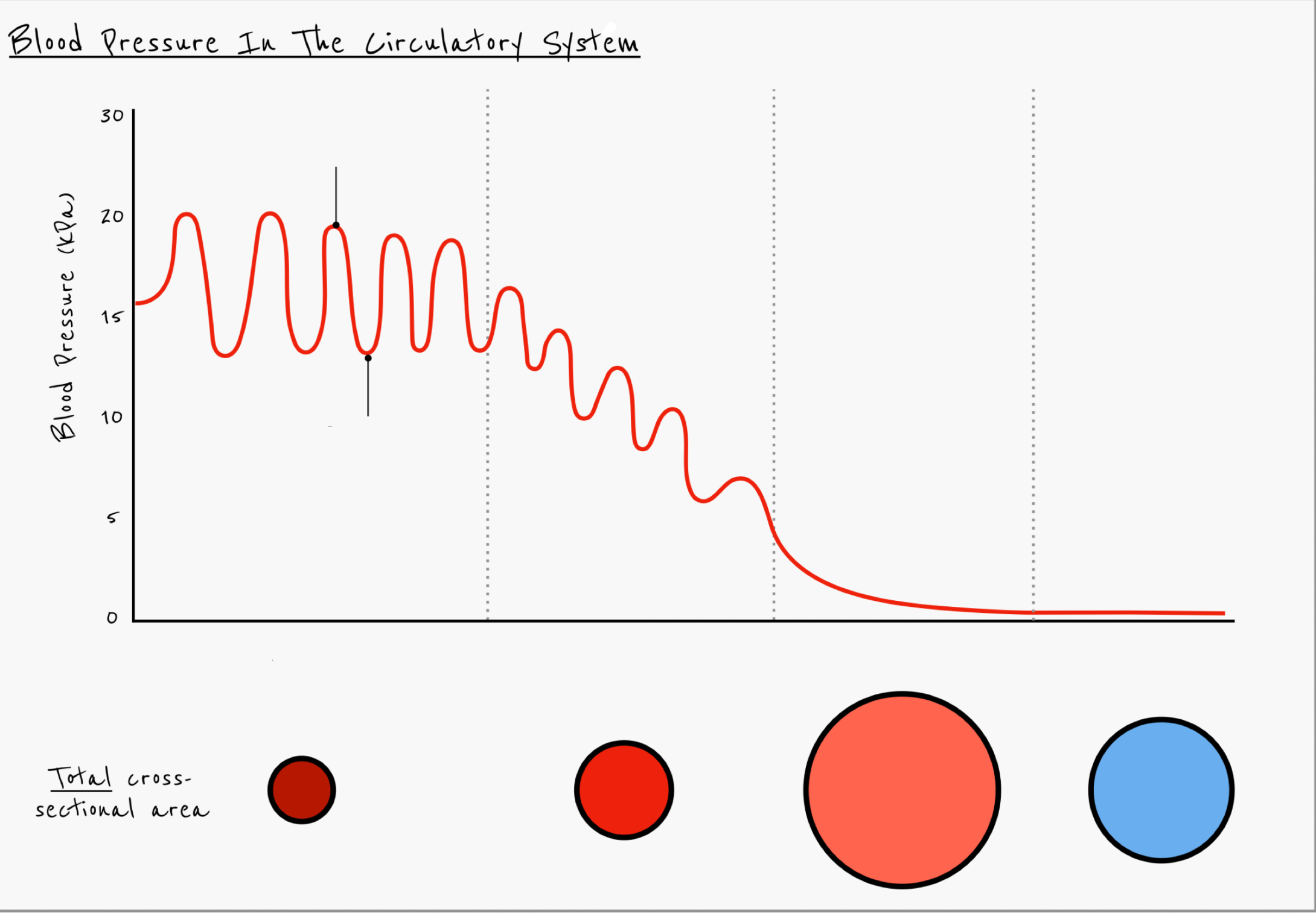
Describe the pressure changes in the blood as it flows through the circulatory system from the aorta to the veins
Pressure drops as distance from the heart increases
Greatest pressure drop while blood is in the arteries
Pressure constant in veins
Amplitude of fluctuation decreases from aorta to arteries
No fluctuations in capillaries and veins
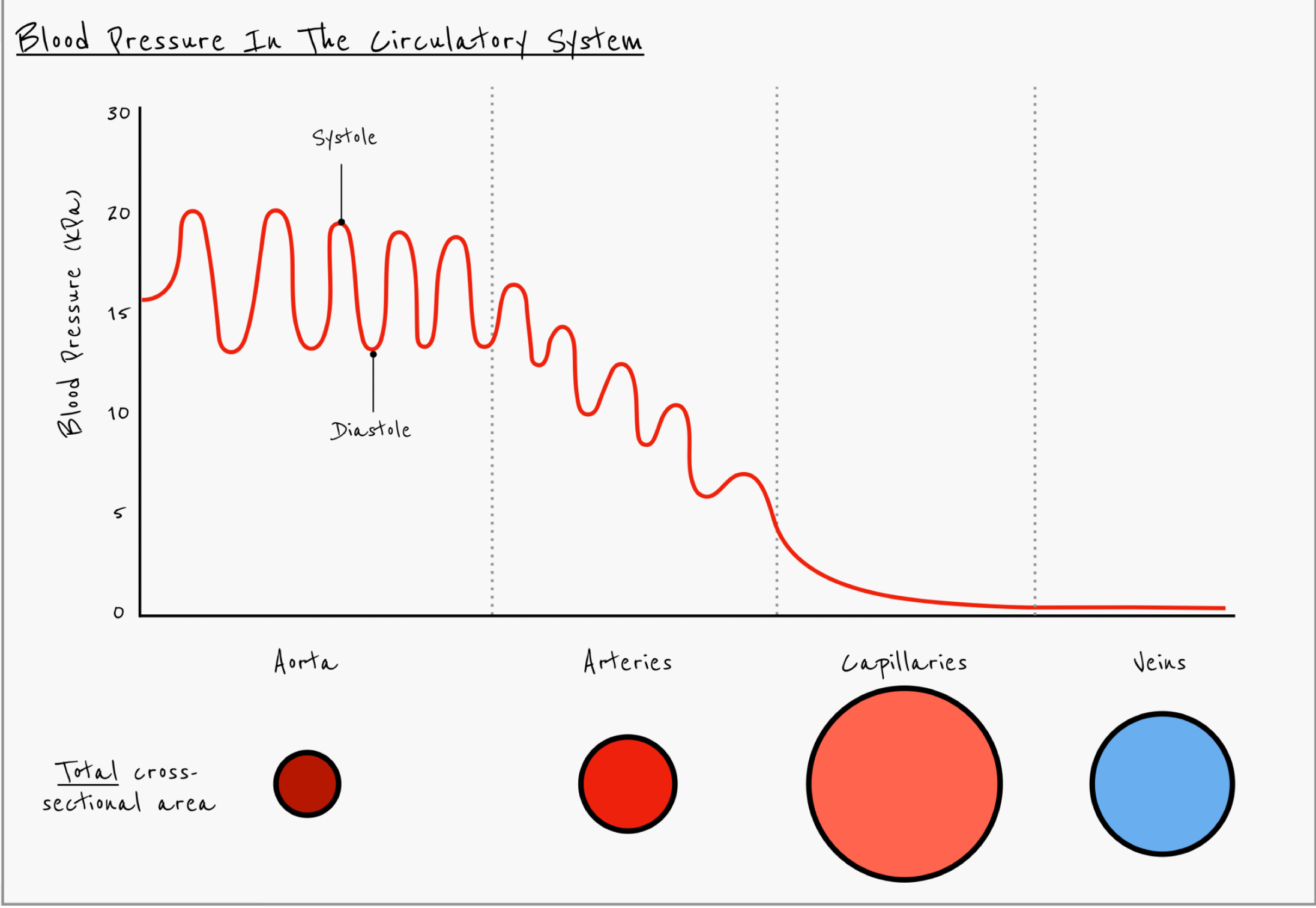
Explain what causes the overall change in pressure as blood flows from the aorta to arteries to capillaries
blood flows into larger bumber of vessels
Total cross sectional area increases
What is the sinoatrial node (SAN)
group of specialised muscle cells in right atrial wall
Trigger impulses - myogenic
Causes cardiac muscle to contract
Acts as a pacemaker
How is a heartbeat initiated
SAN sends out electrical impulse that stimulates contraction of atrial muscle
Impulse stimulated atrioventricular node (AV node)
AV node delays impulse, sends impulses down septum via Bundle of His
Stimulates Purkyne fibres in ventricular wall, causing ventricular contraction from apex
Explain the role of the atrioventricular node in the cardiac cycle
acts to relay impulses to ventricles via purkyne fibres
Introduces delay to ventricular systole to prevent simultaneous contraction of atria and ventricles
Explain why the excitation wave is carried to the apex by the purkyne fibres
So ventricular contraction starts at the bottom (apex) and pushes blood upwards into the arteries
What are erythrocytes
Red blood cells
What is the role of erythrocytes
Transport oxygen around the body
What is haemoglobin
a pigment in red blood cells
Globular protein made of four polypeptide chains (2 α-alpha chains and 2 β- chains)
Each chain has a haem prosthetic group contain iron
Oxygen binds to haemoglobin to form oxyhemoglobin in a reversible reaction
What are the three ways which carbon dioxide is transported in the blood
5% dissolved in blood plasma
10-20% combines with haemoglobin to form carbaminohaemoglobin
75-85% converted into hydrogen carbonate ions (HCO3-) in the cytoplasm of erythrocytes
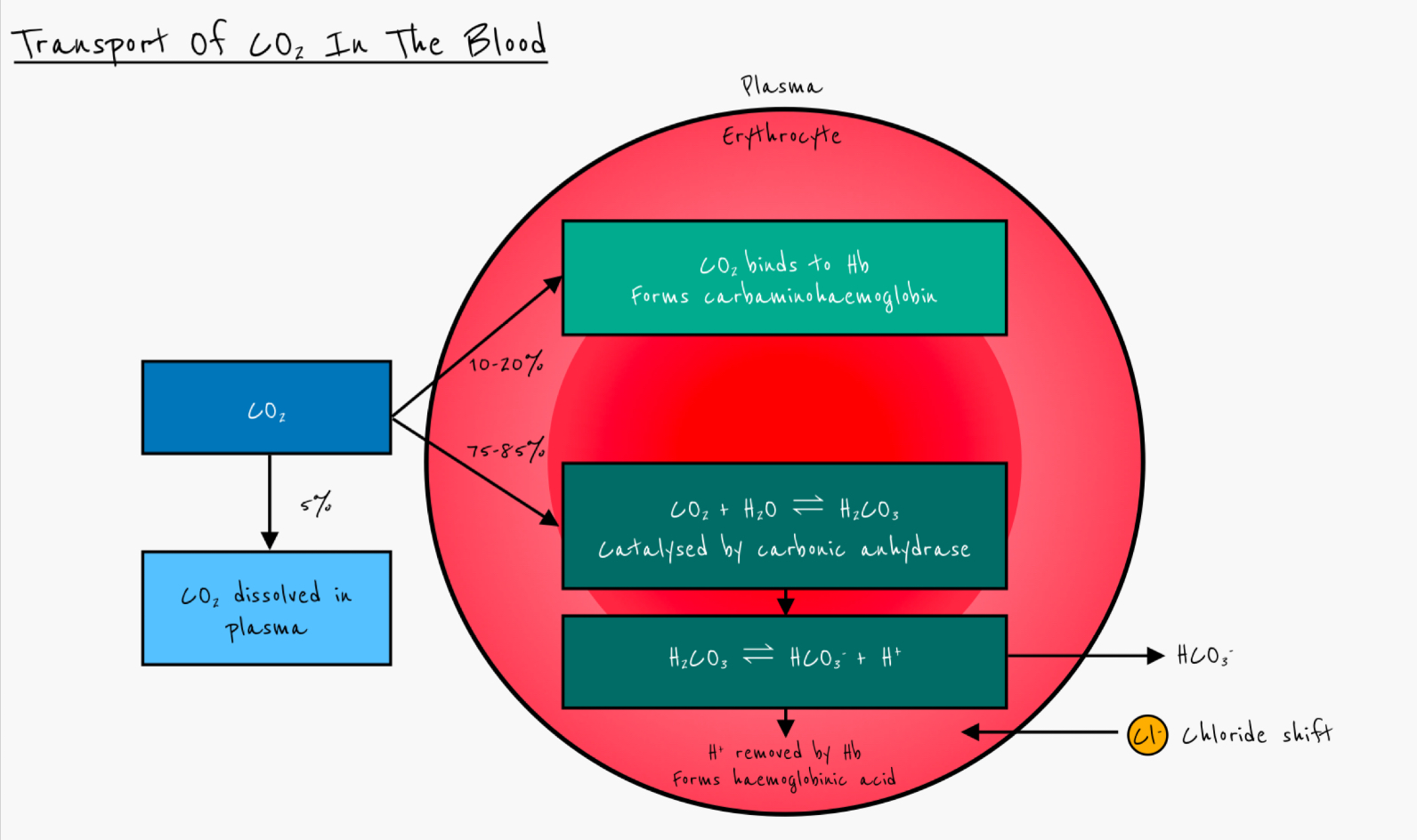
Which enzyme catalyses the production of hydrogen carbonate ions
Carbonic anhydrase
Describe how hydrogen carbonate ions are produced in erythrocytes
carbon dioxide diffuses into erythrocytes
Reacts with water, catalysed by carbonic anhydrase
Forms carbonic acid (H2CO3)
Carbonic acid dissociates to form hydrogen carbonate ions and hydrogen ions
Give the equation for the conversion of CO2 to HCO3-
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
What happens to hydrogen carbonate ions after they have been produced
diffuse down concentration gradient
Out of red blood cells and into plasma
What is the chloride shift
The movement of Cl- ions into erythrocytes to balance the electrical change due to the negative hydrogen carbonate ions leaving.
How does haemoglobin act as a buffer
Prevents changes in pH by accepting 3 H+ ions to form haemoglonobic acid
Define partial pressure
The contributing pressure of a single gas to the total pressure of a mixture of gases
What happens to hydrogen carbonate ions at the lungs
low partial pressure of carbon dioxide (pCO2) at lungs
HCO3- diffuses back to erythrocytes
Reacts with H+ to form H2CO3
Carbonic anhydrase catalyses conversion of H2CO3 back into water and CO2
CO2 diffuses out of blood into lungs
Cl- ions diffuse out of erythrocytes into plasma
Describe the movement of oxygen in the lungs
high partial pressure of oxygen (pO2) in alveoli
Lower partial pressure of oxygen in blood in capillaries
Oxygen diffuses from alveoli to blood
Describe the movement of oxygen at respiring tissues
high partial pressure of oxygen in blood
Lower partial pressure of oxygen in respiring tissues
Oxygen diffuses from blood to respiring cells
Describe the role of haemoglobin in transporting oxygen around the body
Haemoglobin has a high affinity for oxygen so it binds to haemoglobin in lungs (high pO2) forming oxyhemoglobin.
Oxygen is released in respiring tissues (low pO2)
By what process does oxygen bind to haemoglobin to produce the sigmoidal shape of the oxygen dissociation curve
Cooperative binding
Explain how the binding of one oxygen molecule to a haem group affects haemoglobin
binding of first oxygen molecule causes conformational change altering tertiary structure of haemoglobin (slightly)
Affinity for oxygen increases so further loading of oxygen molecules is easier
Explain how removal of the first oxygen at respiring tissues affects haemoglobin
removal of first molecule causes conformational change
Affinity for oxygen decreases (next molecule can leave more easily)
Explain the significance of the oxygen dissociation curve
High pO2 in lungs so haemoglobin rapidly loaded with oxygen
Relative small drop in pO2 at respiring tissues leads to rapid dissociation of oxygen so it is free to diffuse into cells.
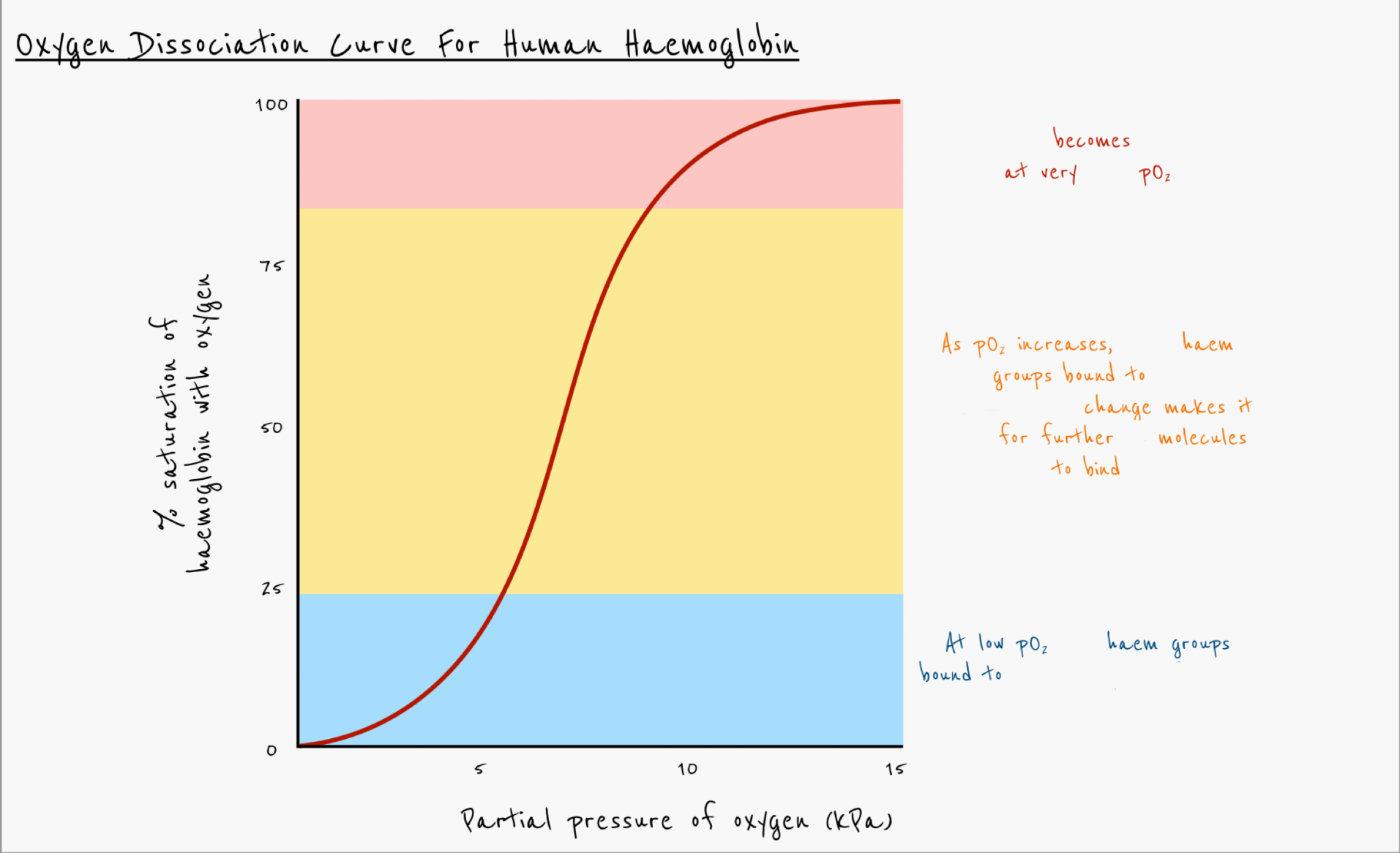
Explain the oxygen dissociation curve for human haemoglobin
Haemoglobin becomes saturated at very high pO2
As pO2
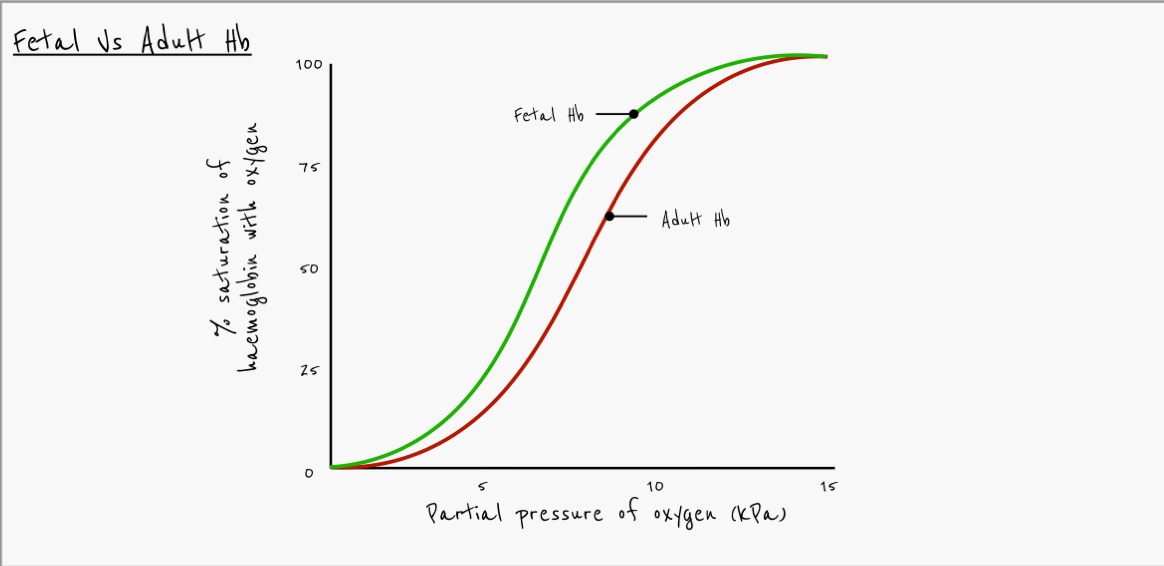
Describe difference in oxygen affinity between fetal haemoglobin and adult haemoglobin
Fetal haemoglobin has a higher affinity for oxygen
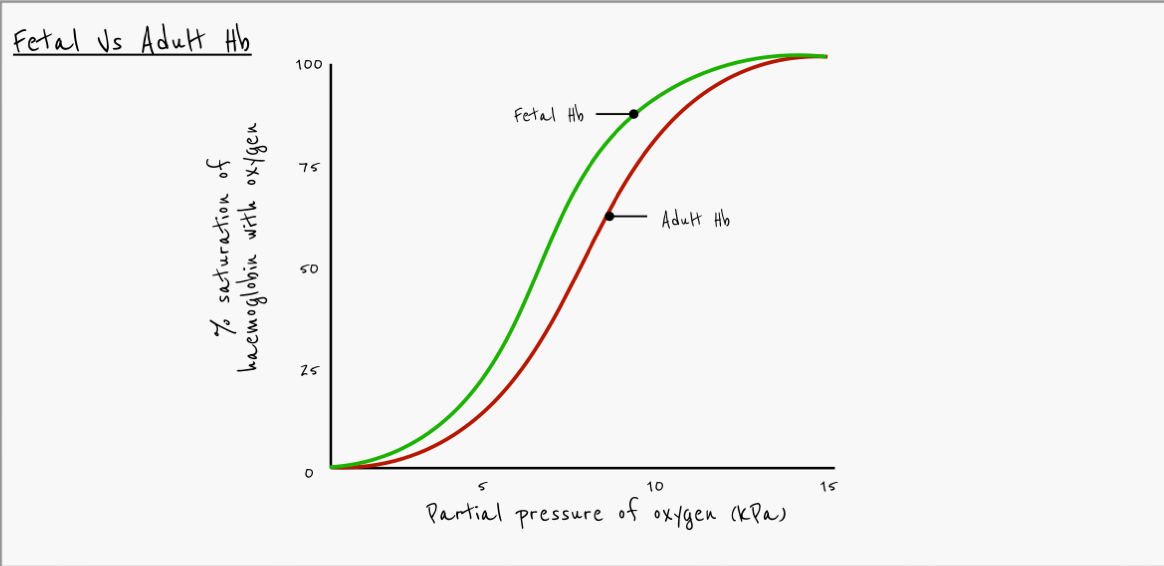
Explain why fetal haemoglobin curve is to the left of the adult haemoglobin curve
placenta has low pO2
Adult haemoglobin will release O2 at the placenta
Foetal haemoglobin has a higher affinity for oxygen at low pO2
It is able to take up oxygen in the placenta
What effect does carbon dioxide have on haemoglobin
at higher pCO2, haemoglobin gives up oxygen more easily
What effect does higher pCO2 have on the oxygen dissociation curve
shifts to the right
Bohr shift
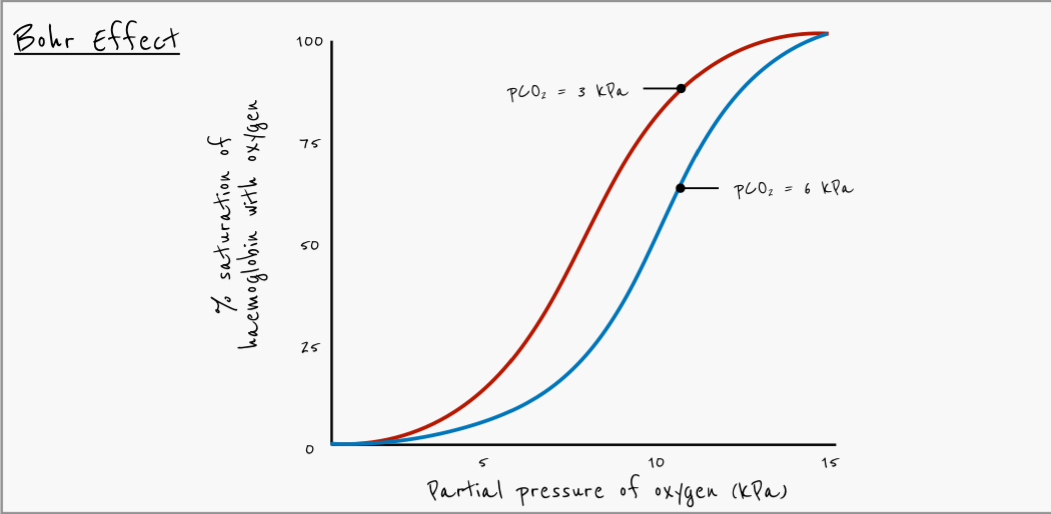
Why is the bohr effect important
Actively respiring tissues have high pCO2, haemoglobin gives up oxygen more easily
Lungs have lower pCO2, haemoglobin binds to oxygen more easily
Explain how an increase in CO2 in the blood leads to the release of more O2 from red blood cells
more carbon dioxide diffuses in to red blood cells
More carbonic acid is formed by carbonic anhydrase
More hydrogen ions formed
Haemoglobin has a high affinity for hydrogen ions
Haemoglobin binds to hydrogen ions to form haemoglobinic acid (HHb)
Formation of HHb decreases the affinity of haemoglobin for oxygen
Carbon dioxide binds to -NH2 of polypeptides to form carbaminohaemoglobin
Causes change in tertiary structure, releasing more oxygen
Outline the benefits of the bohr shift to actively respiring tissue
Actively respiring tissue requires more oxygen for aerobic respiration
Actively respiring tissue produces more CO2
Haemoglobin involved in transport of CO2 so there’s less haemoglobin available to combine with O2
Bohr shift causes more oxygen to be released
What effect does pH have on Hb’s affinity for oxygen?
Affinity decreases as pH decreases (more H+ ions)
What is the SAN and its role?
sinoatrial node is the pacemaker, sends out waves of excitation
What route does the electrical impulse take?
AVN —> Bundle of his —> Purkyne fibres
where in the heart is the bundle of His?
septum
Where in the heart is the Purkyne TIssue?
apex
What is the role of the AVN?
Causes a 0.1s delay in the electrical impulse and allows atria to finish contracting and pump all the blood into the ventricles before the ventricular systole.
what happens at the arteriole end of the capillary?
At the arteriole end there is a high hydrostatic pressure which is greater than the pull from the water potential so the net movement is out
what happens at the venule end of the capillary?
There is a low hydrostatic pressure - water potential of blood is much lower than tissue fluid so water moves in
Describe how the structure of a capillary is adapted for the exchange of substances between the blood and the tissue fluid.
squamous endothelium is one cell thick - short diffusion distance.
walls contain fenestrations (pores) between the endothelial cells - allows for bulk flow of water and small solutes
Is the water potential greater in blood or tissue fluid?
in tissue fluid
what can pass through the endothelium in the capillary?
water , glucose , amino acids, ions , urea and oxygen
what cannot leave the capillary into the tissue fluid?
RBC’s , Plateleets and large plasma proteins (fibrinogen)
what does the Bohr shift do to the affinity of Hb for O2>
Decreased affinity for O2 at the same partial pressures, resulting in more o2 released to actively respiring tissue
formula for carbonic acid
H2co3
what causes the sigmoidal shape of the Oxygen dissociation curve?
co operative binding
Explain co-operative binding
Haemoglobins 3D structure makes it difficult for the first O2 to bind to one of the four haem groups
once one O2 molecule binds there is a conformational change of the haemoglobin protein and the shape opens up increasing the affinity for o2
easier to bind next 2 o2 molecules
plateaus at top due to high saturations
Describe the sequence of events that occurs inside a red blood cell to transport carbon dioxide as hydrogencarbonate ions, including the role of the chloride shift?
co2 diffuses from respiring tissue into the RBC down concentration gradient
co2 is added h20 and catalysed by carbonic anhydride to form carbonic acid
carbonic aid breaks down to form HCO3- and H+
HCO3- diffuses out of the RBC into the blood plasma to be transported into lungs
CL- ions diffuse into RBC from plasma to replace lost ions
Difference between affinities of haemoglobin to O2 in fetus and adult
Fetal haemoglobin has a higher affinity for oxygen than adult haemoglobin at all partial pressures
Explain haemoglobins affinity for O2 in fetuses?
Haemoglobin has a higher affinity for O2 in fetus compared to adult, allowing fetus to load oxygen from mothers blood across placenta (mothers hamoeglobing releases O2 at placenta)
What is the product formed when hydrogen ions (H+) bind to haemoglobin?
Haemoglobinic acid
The Bohr effect results in a rightward shift of the oxygen dissociation curve. What is the physiological advantage of this?
oxygen is more readily released at respiring tissues