🛡️ Immunosurveillance & Immune Editing – Flashcards (16)
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
What is the Immunosurveillance Theory?
The idea that the immune system constantly monitors the body for "transformed" (cancerous) cells and eliminates them before they can form a detectable tumour.
What are the three main pieces of evidence for the immune system’s role in cancer?
Immunodeficient individuals have a significantly higher risk of developing cancer.
Tumour-infiltrating lymphocytes (TILs) are associated with better survival rates.
Spontaneous regression (tumours disappearing without treatment).
What is "Immune Editing"?
A dynamic process where the immune system both protects the host from tumour growth and "sculpts" the tumour by killing the most visible cancer cells, leaving behind the "hidden" ones.
What are the three phases of Immune Editing (The 3 Es)?
Elimination: The immune system successfully detects and destroys cancer cells.
Equilibrium: The immune system and tumour are in a "stalemate"; the tumour is held in check but not eradicated.
Escape: The tumour mutates sufficiently to avoid immune detection and begins to grow rapidly.
How does Peter Medawar’s experiment relate to cancer?
Medawar demonstrated that skin graft rejection is an immune response. This same principle—that the body recognises "non-self" tissue—is used by the immune system to identify mutated cancer cells.
Why do immunocompromised patients have higher rates of cancer?
Because their "surveillance" system is impaired, allowing mutated cells that would normally be destroyed (such as those caused by viruses like EBV or HPV) to survive and multiply.
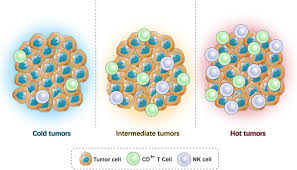
What are "Immune Hot" tumours?
Tumors with high levels of CD8+ T cells and Th1 CD4+ T cells (TILs). These are "inflamed" and usually respond well to modern immunotherapy.
What are "Immune Cold" tumours?
Tumors that lack immune cell infiltration. They have "hidden" from the immune system or created a barrier that prevents T-cells from entering.
What is the significance of MHC downregulation in cancer?
It is a key "escape" mechanism. If a tumour stops expressing MHC Class 1, it cannot present its antigens to CD8+ T-cells, effectively becoming "invisible."
What is the "equilibrium" phase of tumour evolution?
The longest phase of immune editing. The tumour cells are alive but dormant because the immune system is killing them as fast as they can divide.
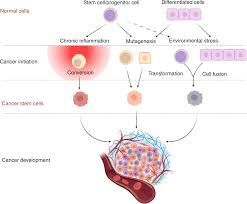
How does chronic inflammation promote cancer?
Inflammation (like a "wound that doesn't heal") recruits macrophages and neutrophils that release growth factors, ironically helping the tumour grow rather than killing it.
. What is "antigenic loss"?
A mechanism of escape where tumour cells that express highly visible antigens are killed, leaving only the cells that don't express those antigens to survive and form the tumour.
What is PD-L1 expression in tumours?
An "escape" mechanism where the tumour expresses a "stop signal" (PD-L1) that binds to T-cells and switches them off, preventing an attack.
What is the role of CD8+ T-cells in tumour elimination?
They are the primary "assassins." They recognise specific tumour antigens on MHC Class I and kill the cancer cell directly via perforin and granzymes.
Why is tumour rejection in immunodeficient mice important evidence?
Tumours from immunodeficient mice often regress when transferred into healthy mice, proving that a healthy immune system can recognise and reject cancer.
How does the immune system "shape" tumour evolution?
By killing the "easiest" targets, the immune system acts like a filter, ensuring that only the most aggressive and "stealthy" cancer cells survive to become a clinical problem..