Mass transport
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
what is partial pressure
the concentration of gasses in a mixture of gasses
what is an erythrocyte
a red blood cell
features of erythrocytes
biconcave shape- flexible
Large SA/V ratio for diffusion of gasses
formed continuously in red bone marrow
last 120 days
contain haemoglobin
no organelles- more space for haemoglobin- can carry more O2
What are the components of haemoglobin
haem prosthetic group
4 poly peptide chains
1 oxygen molecule can bind to each haemoglobin molecule
how is oxyhaemoglobin formed
oxygen binds loosely to haemoglobin to form oxyhaemoglobin
this is a reversible reaction
haemoglobin + oxygen = oxyhaemoglobin
what makes haemoglobin efficient at transporting oxygen
readily associates with oxygen at gas exchange surfaces
readily dissociates from oxygen at oxygen requiring tissues
high affinity for oxygen
Why is oxygen associated at gas exchange surfaces
at high partial pressure of O2 haemoglobin has a high affinity for O2
there is a low partial pressure of CO2
= Oxygen associated
How is O2 dissociated at respiring tissues
at a low O2 partial pressure haemoglobin has a lower affinity for O2
High CO2 partial pressure from aerobic respiration
This causes haemoglobin to have a low affinity for oxygen because:
CO2 lowers pH of blood
CO2 combines with water to form carbonic acid
carbonic acid dissociates into hydrogen carbonate ions and hydrogen ions
hydrogen ions bind to haemoglobin causing the release (dissociation) of O2 (Bohr shift)
how does oxygen associate to haemoglobin molecules
1) there is a low partial pressure of O2, so oxygen doesn’t bind readily to haemoglobin. The binding of the first O2 molecule to the haemoglobin molecule causes a conformational change in the haemoglobin molecule, which makes it easier for other O2 molecules to bind to the haemoglobin molecule
2) there is a higher partial pressure of O2, which makes it easier for O2 molecules to bind (positive cooperatively
3) the haemoglobin molecule continues to become saturated as there is still a high partial pressure of O2
4) it’s harder for the 4th O2 molecule to bind because there is a lower concentration of O2 in the blood to bind at the right speed, energy and orientation to the haemoglobin molecule, due to collision theory
how does haemoglobin differ within different species
different haemoglobin have different affinities for oxygen
each species produces haemoglobin with a slightly different amino acid sequence, therefore the haemoglobin has a different tertiary and quaternary structure to other haemoglobin molecules in different species. Because the tertiary structure of the protein is different it will have different structural and functional properties, therefore different oxygen binding properties
describe fetal haemoglobin
shift to the left of the oxygen dissociation graph- has a higher affinity for O2 than adult haemoglobin
becomes saturated more easily at the same partial pressures than adult haemoglobin, but dissociates less readily than the normal oxygen dissociation curve
what is the importance of fetal haemoglobin
the foetus is fully dependent on the mother for oxygen
maternal oxygenated blood runs close to the foetal deoxygenated blood
fetal haemoglobin has a higher affinity to oxygen at the same partial pressure than maternal haemoglobin
this causes oxygen to move from the maternal haemoglobin to the fetal haemoglobin
what would happen to the baby if it didn’t have fetal haemoglobin
little to no oxygen would move from the maternal haemoglobin to the fetal haemoglobin because the haemoglobin in the mother and the foetus would have the same affinity for oxygen
describe the movement of Co2 in the blood and where it goes to
plasma (5%)
haemoglobin into carbaminohaemoglobin (10%)
Co2 dissolves in water and forms carbonic acid which then dissociates into hydrogen carbonate ions an hydrogen ions (85%)
what is the Bohr effect
when the partial pressure of CO2 in the blood is high, which causes haemoglobin’s affinity for O2 to be reduced, which means that O2 is dissociated more readily
reduces haemoglobin affinity for O2 at the same partial pressure
why does the Bohr effect occur
Occurs because CO2 lowers the pH of the blood;
CO2 combines with water to form carbonic acid
carbonic acid dissociates into hydrogen carbonate ions and hydrogen ions
hydrogen ions the combine with haemoglobin causing the release of O2
why is the Bohr effect useful
it allows O2 to dissociate from haemoglobin at the same partial pressure more readily in respiring tissues that need it for aerobic respiration, such as muscle tissues
what is the Bohr shift
the shift to the right of the oxygen dissociation graph because the partial pressure of CO2 is higher
this means that at any given partial pressure of O2 the percentage of saturation of haemoglobin is lower at higher CO2 concentrations (because haemoglobin has a lower affinity for O2 due to Bohr effect)
Label the heart
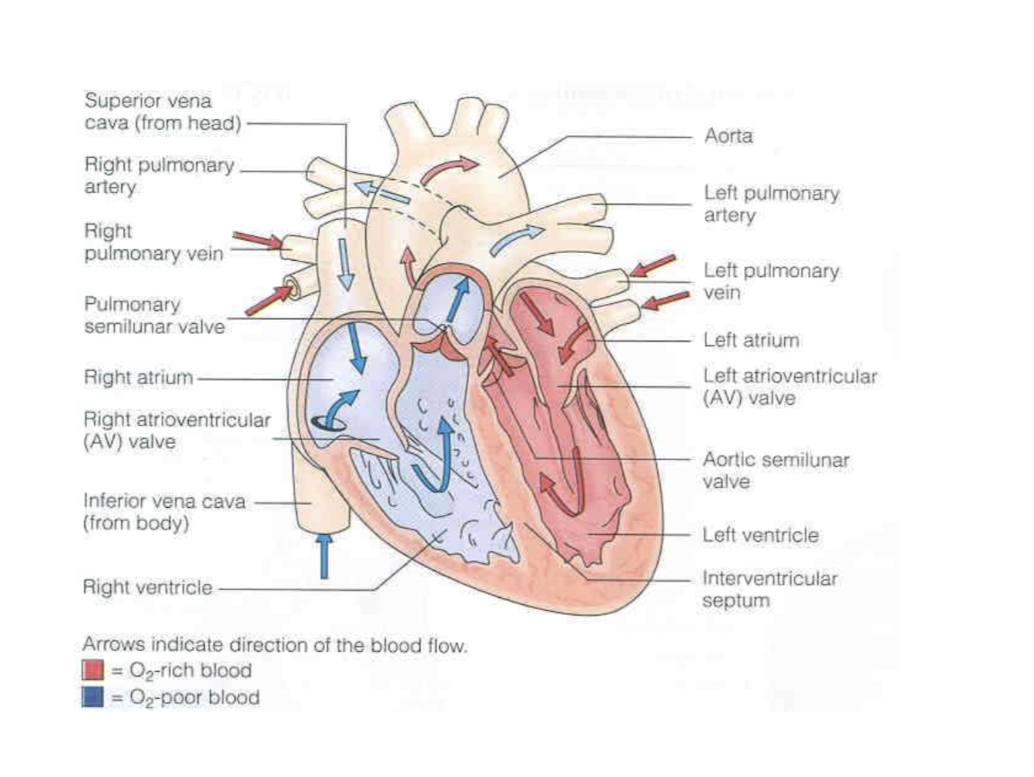
what is the epicardium
thin external membrane of the heart
what is the myocardium
thick cardiac muscle that makes up the bulk of the heart wall
what is the endocardium
flattened cells and connective tissue which lines the whole of the circulatory system
what are the properties of cardiac muscle
myogenic- it can contract on its own without external stimulation via nerves or hormones. This allows the heart to beat at its own regular intervals
it doesn’t tire or fatigue- so it allows the heart to beat continuously throughout an individuals life
the cardiac muscle fibres form a network that spreads through the walls of the atria and ventricles which allows the chambers of the heart to contract
cardiac muscle fibres are connected to each other via specialised connections called intercalated discs
why do animals meed specialised transport systems
high metabolic demand
molecules need to travel large distances
small SA:V ratio
waste products need to be removed
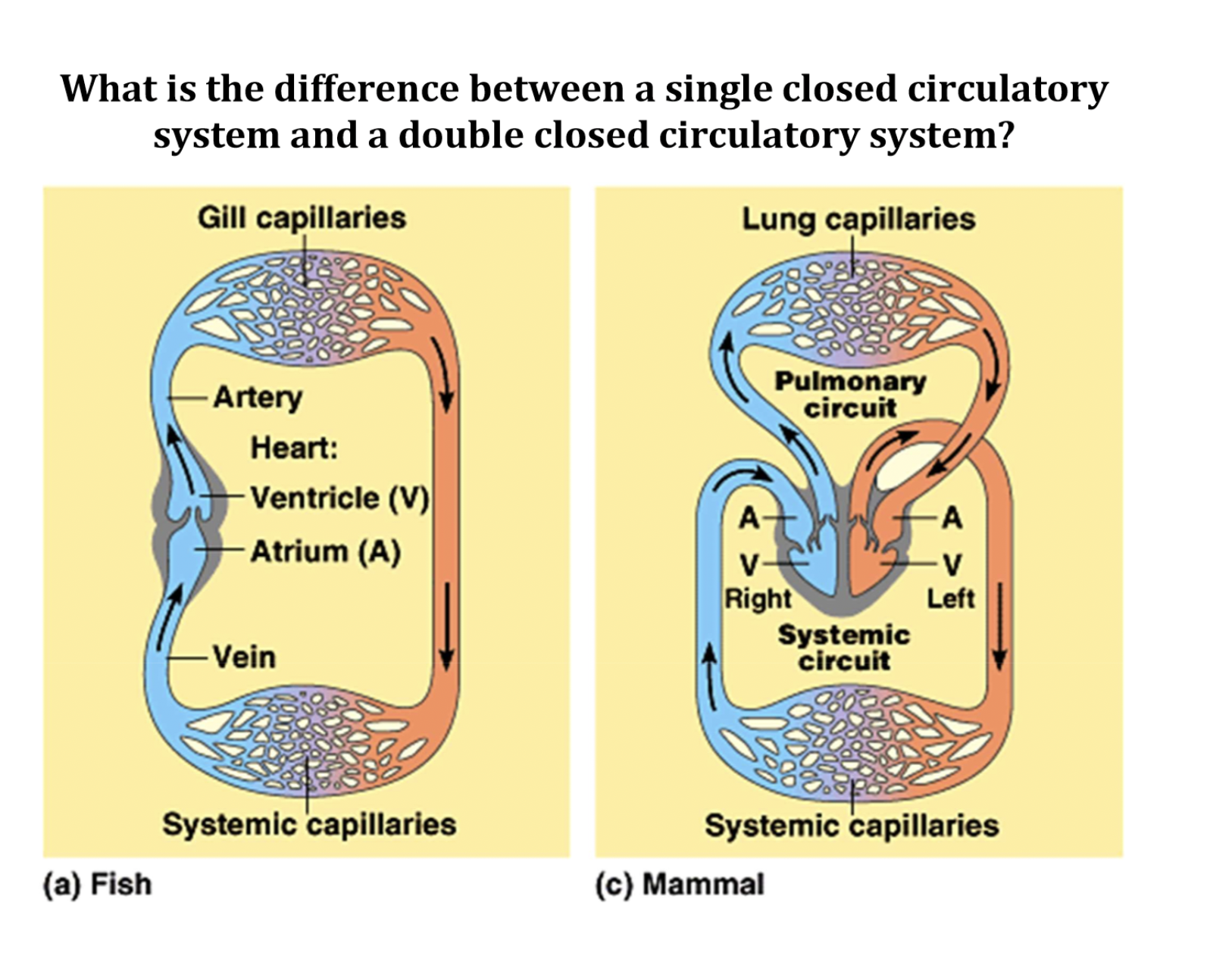
what is a double closed circulatory system
blood goes through the heart twice per cycle which allows oxygenated blood from the lungs to go back to the heart and get pumped around the body at high pressure
why do mammals have a double loop rather than a single loop
because mammals are bigger so oxygenate blood needs to travel further. In single loop systems blood is still deoxygenated as it leaves the heart and then gets oxygenated after before going to the body.
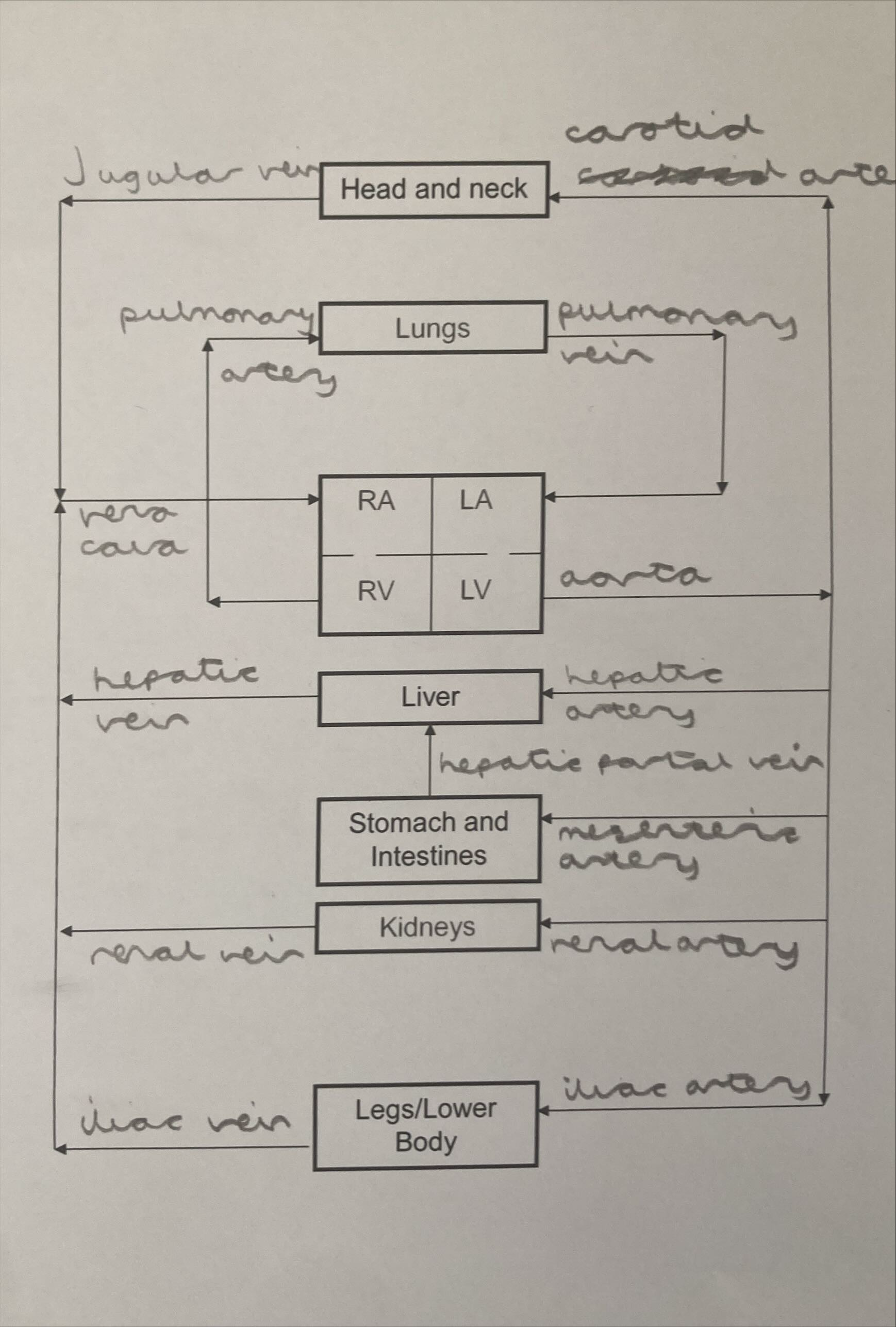
label the human circulatory system
how long does it take for one cycle of blood to pass through the heart
0.8 seconds
which is longer, diastole or systole
diastole
what is the difference between diastole and systole
systole is the contraction phase of the heart
diastole is the relaxation phase of the heart
describe the movement of blood on the right side of the heart
deoxygenated blood from the vena cava enters the right atrium at a low pressure
as the blood flows into the right atrium, pressure in the right atrium increases which causes the atrioventricular (tricuspid) valve to open and let blood pass into the right ventricle
when both the right atrium and right ventricle are filled with blood the right atrium contracts, forcing all of the blood into the right ventricle which stretches the ventricle walls
as the right ventricle contracts the atrioventricular (tricuspid) valve closes to prevent the back flow of blood into the atrium
the right ventricle contracts which decreases the volume of the right ventricle, which increases the pressure of the blood in the right ventricle
this forces the pulmonary semilunar valve to open and deoxygenated blood is pumped into the pulmonary artery
describe the movement of blood at the left side of the heart
oxygenated blood enters the left atrium through the pulmonary vein from the lungs at a low pressure
as blood flows into the left atrium pressure builds up in the left atrium which causes the atrioventricular (bicuspid) valve to open because pressure is higher in the LA than the LV. This allows blood pass into the left ventricle
when both the left atrium and left ventricle are filled up with blood the left atrium contracts (atrial systole) all the blood is forced into the left ventricle which stretches the walls of the left ventricle
as the left ventricle contracts the bicuspid valve closes to prevent the back flow of blood into the left atrium
the left ventricle fully contracts which decreases the volume of the ventricle chamber which increases the pressure, forcing the aortic semilunar valve to open because the pressure of blood in the left ventricle is higher than the pressure of blood in the aorta.
This causes oxygenated blood to be pumped through the aortic semilunar valve and into the aorta
when do valves open and close
open when pressure is higher behind the valve
close when pressure is higher in front of the valve
what is the function of a valve
to prevent the back flow of blood
How does CHD develop
atheroma formation- partial blockage of lumen- reduced blood flow and increased blood pressure
atheroma increases the risk of
aneurysm- swelling of the artery
thrombosis- blood clot
These cause interrupted blood flow to the heart which can lead to myocardial infarction (heart attack)
how can an atheroma form
damage occurs to endothelial lining of artery
white blood cells (macrophages) and lipids (from low density lipoproteins)
the higher the blood LDL level is (from diet high in fats) the more lipids are used to repair the damage
the fatty tissue builds up to form a lump (atheroma)- partially block lumen- reduced blood blow and high blood pressure
how can an aneurysm form
aneurysm- a ballon like swelling of the artery
atheroma:
weakens artery
reduce blood flow
higher blood pressure
now when blood passes through the weakned artery it may push the inner layers of the artery through the outer layer and form a ballon like swelling
this can burst and form a haemorrhage (bleeding)
how can thrombosis occur
thrombosis- formation of a blood clot
atheroma can rupture the endothelial (inner lining) of the artery
this has to be repaired by platelets and fibrin which forms a blood clot (a thrombus)
the blood clot can completly block the artery or can become disloged and block a blood vessel somewhere else
how can aneurysms and thrombosis lead to myocardial infarction
coronary arterys supply the heart with oxygenated blood- for respiration
oxygen supply to cardiac muscle can be cut off due to blood clots or bleeding
cardiac muscle recieves less O2- damage or death of cardiac muscle
what are the symptoms of myocardial infarction
pain in chest
shortness of breath
sweating
how does heart failure occur
if O2 supply is cut off to large areas of the heart
what factors can increase the risk of CHD
high concentration of LDL’s from poor diet
smoking cigarettes
high blood pressure
age
gender
being overweight
how does LDL concentration increase the risk of CHD
when damage to the endothelial lining of the coronary arteries occurs white blood cells (macrophages) and lipids from LDL’s are used to repair the damage which clump together and form an atheroma
atheromas can increase blood pressure, reduce blood flow and lead to a blood clot (a thrombus)
this can block blood from flowing to the heart and recieving oxygen which could result in myocardial infarction
how does smoking lead to CHD
carbon monoxide binds to haemoglobin instead of O2
if the heart doesn’t recieve enough oxygen for respiration then it won’t be able to produce the energy required to contract the geart which can lead to myocadrial infarction
how does high blood pressure lead to CHD
blood pressure can cause damage to endothelial lining of the coronary arterys
leads to formation of atheroma
atheroma can rupture the endothelial lining which leads to the formation of a blood clot
cuts off blood and O2 supply to the heart
heart can respire which can lead to myocardial infarction
can also lead to an aneurysm as high blood pressure may push inner layer of artery through the outer layer- forms haemorrhage which is likely to burst- less blood and O2 to heart
define cardiac output
the volume of blood pumped out of one ventricle of the heart per minute
what is the equation for cardiac output
HR (bpm) x SV (ml/beat)
explain how cardiac output can increase
initially with exercise both HR and SV will increase
at 40-60% of maximal exercise SV plateaus
any further increases in Co are due to an increase in Hr which doesn’t plateau as quickly as SV
How do you work out a persons maximum HR
220-age
how does a person gain a lower resting HR
through aerobic training, as a result of cardiac hypertrophy
why do athletes have a lower resting HR
their heart is stronger due to cardiac hypertrophy, cardiac muscle is stronger so can contract with more force which leads to a higher SV. So their heart doesn’t need to beat as many times per minute to get the same amount of blood to the body and maintain resting cardiac output
what is bradycardia
having a resting HR below 60 bpm
indicates being a trained athlete
describe the structural features of arteries
thick muscle layer to contract and dilate (vasoconstriction and vasodilation) to control blood flow
thick elastic layer to maintain high pressure and pressure changes. Stretches and recoils which smooths out blood flow
thick walls to resist high blood pressure
no valves
small lumen
smooth and flat endothelial lining to reduce friction which aids blood flow
collagen provides structural support to maintain the shape and volume of the artery
describe the difference in structural features of arterioles compared to arteries
thicker muscle layer because arterioles play more of a role in vasoconstriction and vasodilation than arteries do
thinner elastic layer because arterioles don’t have to resit as high pressure as arteries do (aorta) because arteries branch off into arterioles
describe the structural features of veins
thin muscle layer as blood is carried away from tissues (no need for vasoconstriction or vasodilation)
thin elastic layer because blood is at a low pressure
lack of thickness because there is a low risk of veins bursting because blood is at a low pressure. Also allows for veins to be compressed when body muscles contract to help get blood back to the heart against gravity
pocket valves to prevent the back flow of blood
how do veins get blood back to the heart at low pressure and against gravity
pocket valves close to prevent the back flow of blood
bigger veins run through muscles, muscles can contract which sequeezes the vein, increasing pressure of blood in the vein and forcing blood back to the heart
breathing pressure changes- helps move blood back to the heart
describe the structural features of capillaries
walls are made up of a 1 cell thick layer of endothelial lining, shortens diffusion distance, increases the rate of diffusion
lot of them and are branched which increases the SA for diffusion to occur
narrow diameter which decreases diffusion distance
narrow lumen so that red blood cells have to squeeze through the capillary and move slower which allows for more efficient oxidation of RBC’s and also shortens the diffusion distance, which increases the rate of diffusion
Spaces between the endothelial cells allow WBC’s to move into tissues and fight infections
what are the components of blood plasma
glucose
amino acids
mineral ions
hormones
large plasma proteins
what is tissue fluid
the fluid that surrounds cells in tissues
tissue fluid has the same composition as plasma but without the plasma proteins because they are too big to pass through the capillaries
why do we need tissue fluid
not every cell lies next to a capillary
how is tissue fluid formed and re uptaken back into the capillaries
Hydrostatic pressure at arterial end of capillary- forms
osmotic pressure at venous end of capillary- draws tissue fluid back in
how does hydrostatic pressure form tissue fluid
at the arterial end of the capillary
there is a higher hydrostatic pressure in the capillary than in the tissue fluid
this forces fluid out of the arterial end of the capillary into the spaces around the cells forming tissue fluid
how does osmotic pressure take back in water from tissue fluid
at the venous end
hydrostatic pressure ejected fluid from the capillary- decreased water potential
because of fluid loss and an increase in the concentration of plasma proteins in the venous end of the capillary
Water potential is lower in the capillary than in the tissue fluid- some water is drawn back into the capillary via osmosis
what happens to the tissue fluid than isn’t taken back into the capillary
excess tissue fluid is drained into the lymphatic system
what is the lymphatic system
a secondary circulatory system and a major part of the immune system
what is the lymphatic system made up of
lymphatic capillaries
lymph nodes
lymphatic organs
what are lymphatic capillaries
vein like lymph vessels that contain valves
what are lymph nodes
sac like organs that trap pathogens and foreign substances and contain large amounts of white blood cells
what are lymphatic organs
the spleen, thymus and tonsils which all contain large amounts of WBC’s
What is lymph
a pale yellow fluid that is similar to tissue fluid but contains more lipids
how does lymph form
Not all tissue fluid returns to the capillaries. 90% does but the excess 10% is drained into the lymphatic system where it forms lymph
where does the lymphatic system drain into
into the circulatory system near the vena cava via the thoracic duct
why do we need the lymphatic system
you would die within 24h without the lymphatic system as the rate of water loss would be too large (need to get all water back into the circulatory system)
this would lead to a build up of tissue fluid in the tissues called oedema
how do the contents of the lymphatic system transported
hydrostatic pressure of the tissue fluid that has left the capillaries
contraction of muscles that squeeze lymph vessels to ensure the fluid inside them moves away from tissues in the direction of the heart
what are the characteristics and functions of the xylem
transport water and mineral ions up the plant
cells are joined without a cell wall end which forms a hollow tube
contains lignin to provide extra support, forms in spirals to ensure the xylem vessels don’t collapse under the transpiration pull
why do plants need water
water is a raw material for photosynthesis
mineral ions and the products of photosynthesis are transported in aqueous solutions
the loss of water via evaporation helps to keep the plant cool
turgor pressure (hydrostatic pressure) as a result of osmosis helps to form a hydrostatic skeleton to support the stem and leaves
what are the adaptations of root hair cells
large SA:V ratio
short diffusion pathway into cell
lower water potential inside the cell to maintain concentration gradient (so rate of osmosis is maintained)- water can move into the root hair cell from soil via osmosis
small size so can penetrate through soil particles easily- access water and mineral ions
lots of mitochondria to provide energy for active transport of mineral ions (higher conc of mineral ions inside root hair cell than in soil)
no chloroplast because they are underground (no sunlight)
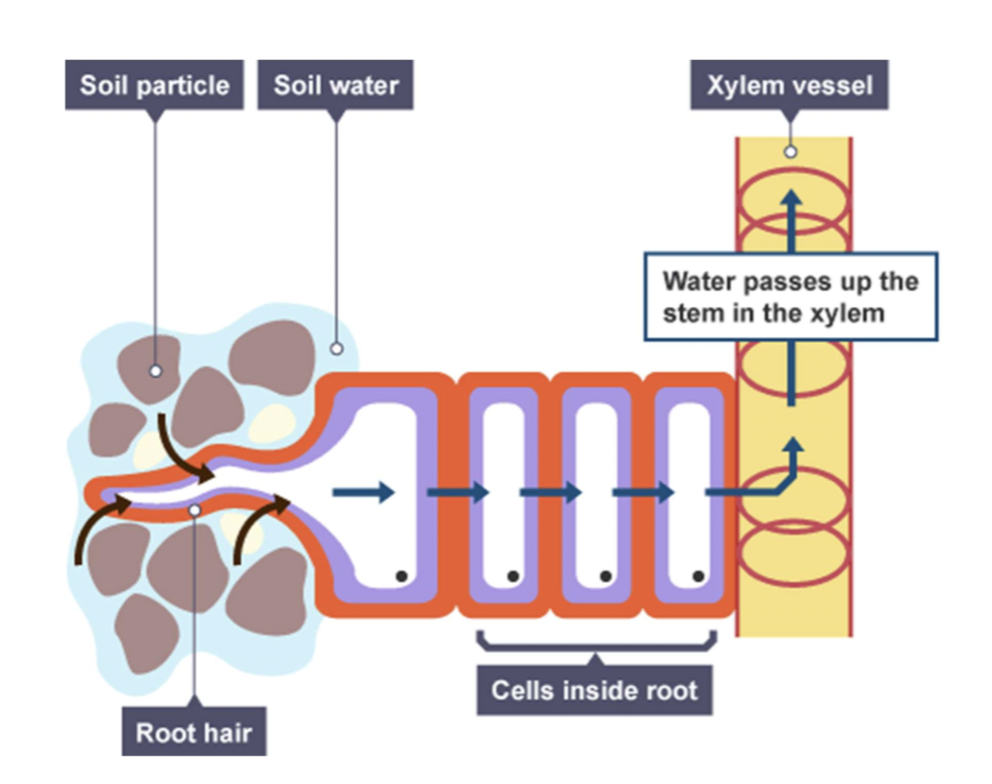
what is root pressure and how is it created
the solute concentration in the cytoplasm of the endodermal cells is lower than in the xylem cells because minerals are actively transported into root hair cells
the endodermal cells move mineral ions into the xylem via active transport. This increases the pressure in the xylem and further lowers the water potential of the xylem. This increases the rate of water movement into the xylem from the endodermal cells via osmosis. This is known as root pressure
how is the rate of transpiration controlled
by stomata
this is a turgor driven process
when there is sunlight potassium ions are actively transported into the guard cells. This lowers the water potential of the guard cells which causes water to passively move into the guard cells which makes the guard cells more turgid, which opens the pore- increases the rate of transpiration and allows for gas exchange during photosynthesis
when it’s dark photosynthesis can’t occur so the stomata must close to prevent water loss. Potassium ions are actively transported out of the guard cells which increases the water potential. This causes water to passively move out of the guard cell which makes the guard cell become flaccid. This closes the pore and reduces the rate of transpiration
describe the process of transpiration
water molecules evaporate from the mesophyll cells into the air spaces in the leaf- leads to an increase in water vapour potential
water molecules then move out of the leaf through the stomata via diffusion down the water vapour potential gradient
this lowers the water potential of the cell so water moves in through osmosis by the apoplast and symplast pathways
this carries on up through the xylem then through the leaf
what is the transpirational pull and the cohesion tension theory
water forms hydrogen bonds with other water molecules- cohesion (forms a continuous column of water)
water molecules form hydrogen bonds with carbohydrates in the walls of the xylem- adhesion
cohesion + adhesion = capillary action
water is constantly drawn up the xylem to replace the water lost via transpiration/evaporation
the transpirational pull puts the xylem under tension- creates negative pressure in the xylem (cohesion tension theory)
what research is there to support capillary action
during sunlight when trees are photosynthesising their diameter decreases
water is being used for photosynthesis, being lost via stomata during evaporation/transpiration
the water concentration gradient and capillary action cause negative pressure in the xylem and the trees diameter to reduce
what different factors affect the rate of transpiration
light intensity
temperature
humidity
wind speed
how does light intensity affect the rate of transpiration
the rate of transpiration increases in the light because stomata open- more water is lost
how does temperature affect the rate of transpiration
when temperature is higher the rate at which water is evaporated is faster
how does humidity increase the rate of transpiration
Humidity: When the air around the plant is humid, this reduces the diffusion gradient between the air spaces in the leaf and the external air. The rate of transpiration therefore decreases in humid air and speeds up in dry air
how does wind speed affect the rate of transpiration
the moving air removes any water vapour that is in the air nearby the stomata. This increases the concentration gradient between the air spaces in the leaf and the external environment- increases the rate of diffusion of water vapour out of the stomata.
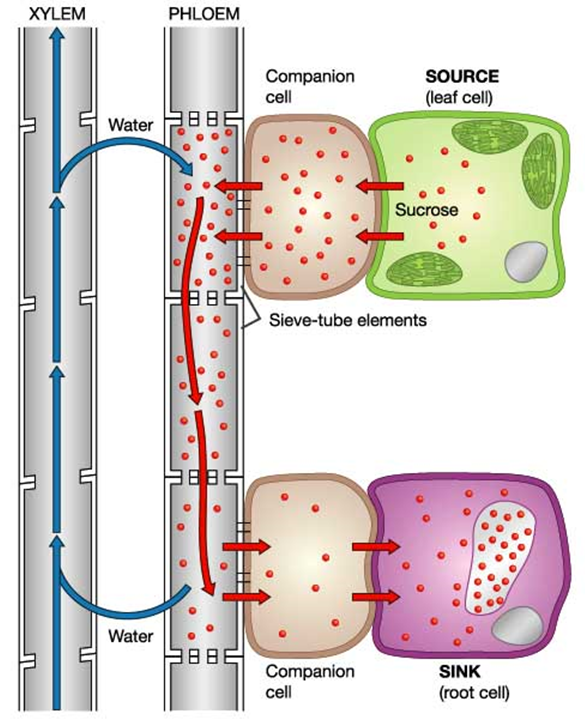
what is translocation
the transport of the products of photosynthesis (assimilates) from parts of the plant where assimilates are produced/stored (sources) to where they are needed (sinks)
what are the different sources
leaves and stem
food stores in seeds upon germination
storage organs
what are the different sinks in plants
meristem (plant stem cells)
roots that are absorbing ions or growing
what is a source
parts of the plant which produces or possesses more carbohydrates than it requires
what is a sink
part of a plant where carbohydrates are required for growth, active transport, or storage
what are assimilates
glucose is converted into sucrose which is then transported
When sucrose arrives at sink:
converted into glucose for respiration
converted into starch for storage
connected into amino acids for growth
why is glucose converted into sucrose before it’s transported
sucrose is less soluble in water than glucose
so sucrose is less likely to be metabolised when being transported
what is the phloem tissue made up of
sieve tube elements:
living cells that form the tube which transports assimilates
have sieve plates between them
they have no organelles or nucleus- need companion cells (less resistance for mass flow)
Companion cells:
provide the energy needed for the active transport of assimilates
describe the mass flow theory
Sucrose produced from glucose in leaves by photosynthesis (source)
Sucrose moves by facilitated diffusion into companion cell
Companion cell actively transports sucrose into the phloem (sieve tube element)
This lowers the water potential in the phloem which draws water into the phloem from the xylem by osmosis
This increases the volume of fluid in the phloem which increases the pressure.
Higher pressure in the phloem near the source is greater than lower pressure near the sink (the root cells)
This different in pressure forces the sap down the phloem by mass transport/ bulk transport
Sucrose moves out of the phloem into the companion cells then into the root cells (sink) by facilitated diffusion
This increases the water potential in the lower part of the phloem
Water moves back into the xylem by osmosis lowering the volume and hence pressure in the lower part of the phloem.
provide evidence for translocation
sap is released when the phloem is cut suggesting that there is high pressure in the phloem
the concentration of sucrose is higher in leaves (sources) than in the roots (sink)
metabolic toxins (that stop the production of ATP), and lack of O2 inhibit the movement of sucrose through the phloem
companion cells have high concentrations of mitochondria for ATP production
give some evidence against the mass flow theory
sieve plate function is unclear (may have a structural role), but their design would seem to hinder mass flow in the phloem
not all solutes in the phloem move at the same rate (would mean it’s not mass flow)
describe ringing experiements
the phloem lies just underneath the bark
in a ringing experiment the phloem is removed
this causes the region above the removed section to swell up, and parts of the plant blow this will die
suggests that the phloem transports sugars (sucrose)
describe tracer experiements
uses radioactive CO2 from radioactive C14
C14 is then incorporated into sugars produced from photosynthesis
the sugars movement around the plant can be tracked by autoradiography (thin sections of tissue are placed on x-ray film and C14 appears black