Respiratory System
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
124 Terms
Groups of cells that have similar
structure and function together as a unit are called what?
tissues
What are the four main categories of tissues?
1. epithelial
2. connective
3. nervous
4. muscle
(Mnemonic: Emily's Chocolate Never Melts)
What kind of tissue is skin?
epithelial
(Note: epithelial tissue usually functions as a covering in some manner. )
What kind of tissue is bone and cartilage?
connective
What kind of tissue is blood?
connective
What is it called when the body brings conditions back to their normal homeostatic function?
negative feedback
(Note: the body wants to maintain balance. This is the body's most popular way to achieve that end)
What is it called when the body intensifies a condition beyond it's normal limits?
positive feedback
(Note: In a way, this still maintains balance - the difference in this case is that the body must over exceed its equilibrium to bring it back eventually)
What is the movement of gases in and out of the body called?
respiration
(Note: this term can also mean cellular respiration = production of ATP in mitochondria)
What is thermoregulation?
control of exchange of heat with the environment.
What are the three terms to describe an organism that obtains body heat from the environment?
1. ectotherm
2. poikilotherms
3. cold-blooded
What are the three terms to describe an organism that generates its own body heat?
1. endotherms
2. homeotherms
3. warm-blooded
How does evaporation act as a regulatory mechanism for animals?
body heat is removed through liquid evaporation.
(Note: evaporation is an endothermic process- energy needs to be put in for reaction to occur)
How does metabolism act as a regulatory mechanism for animals?
muscle contraction + other metabolic activities produce heat
How can surface area act as a regulatory mechanism for animals?
1. vasodilation (increase diameter of extremity vessels) helps remove heat
2. vasoconstriction (decreasing diameter of extremity vessels) helps retain heat
What regulatory mechanism is displayed when the body increases blood flow to the ears?
using surface area for thermoregulation
(Note: sending blood to ears is an example of vasodilation and helps remove heat)
What kind of respiration occurs when air enters lungs, allowing the alveoli to exchange gas with the blood?
external respiration
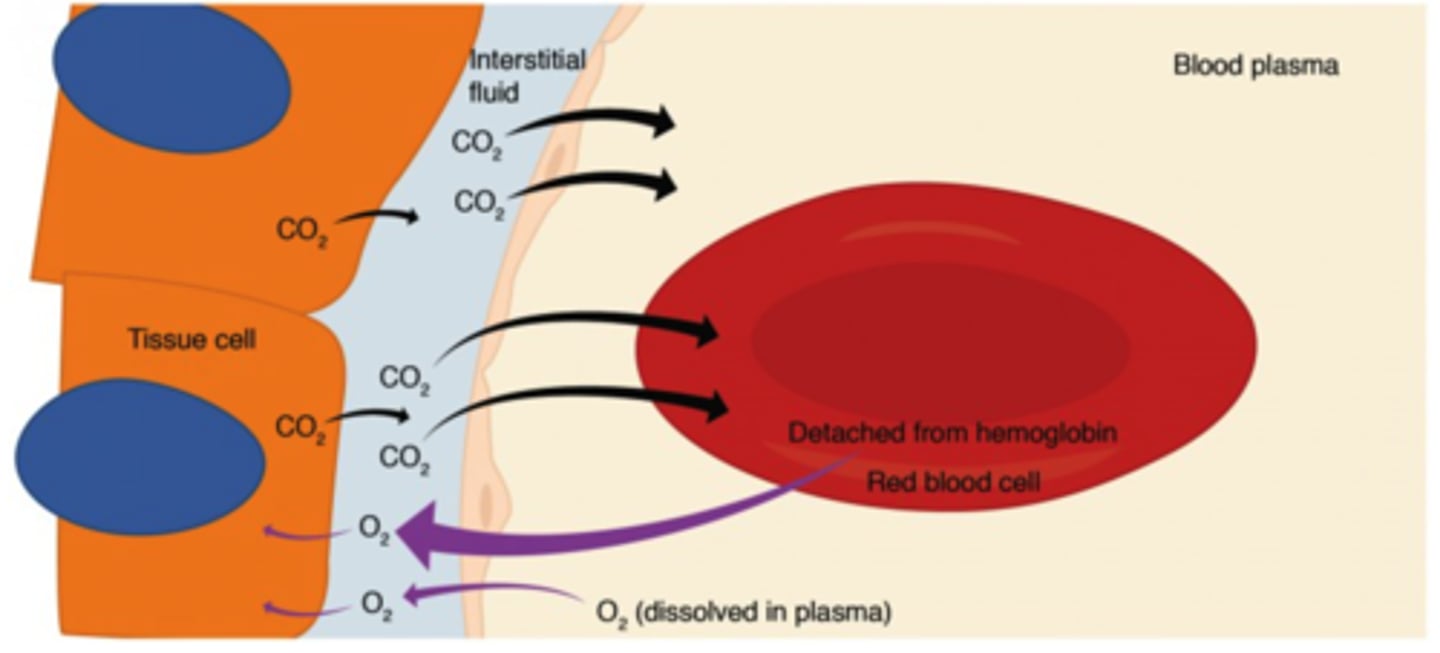
What kind of respiration occurs when the blood exchanges gas with the tissues?
internal respiration
Lungs are ______ structures.
invaginated
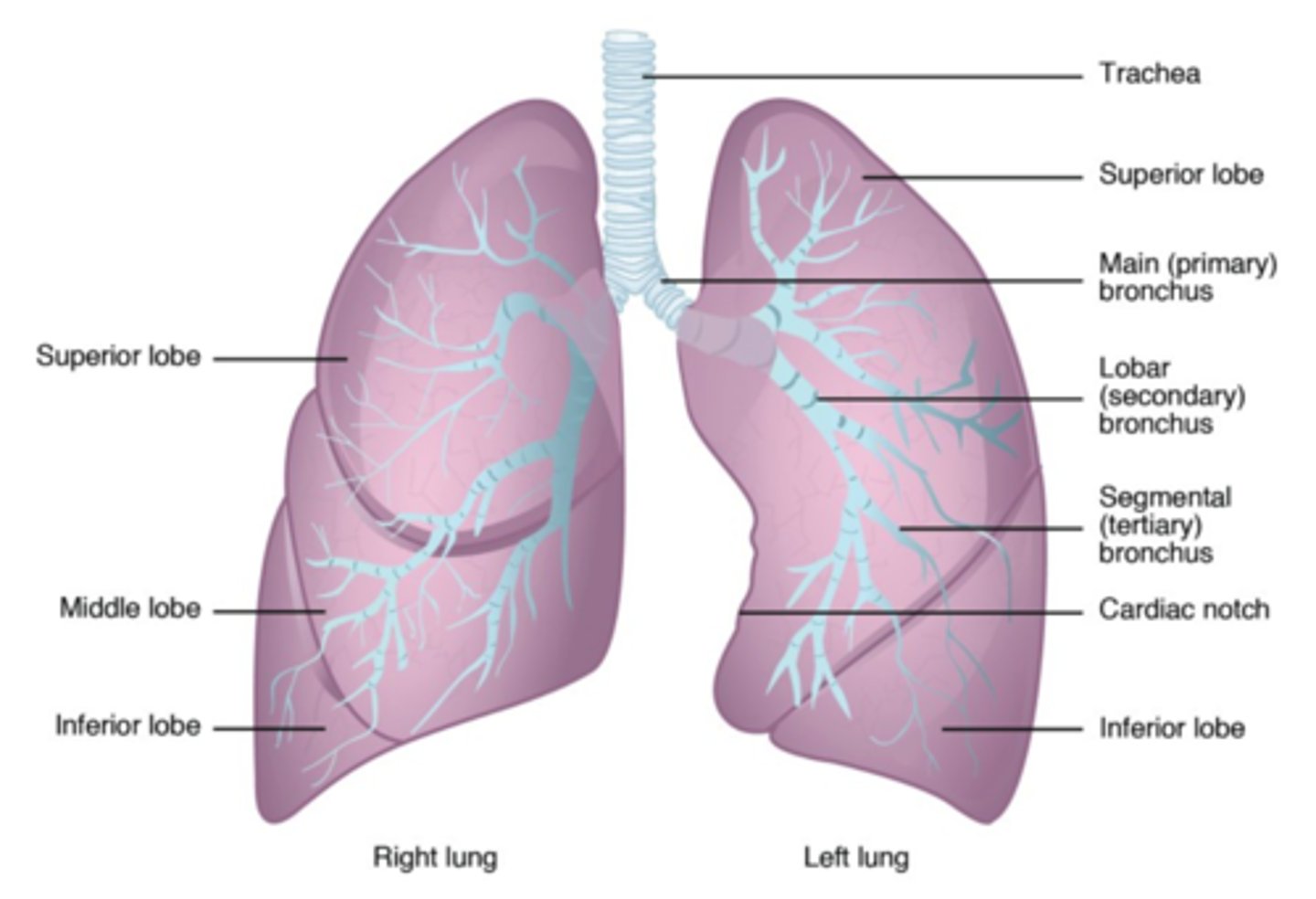
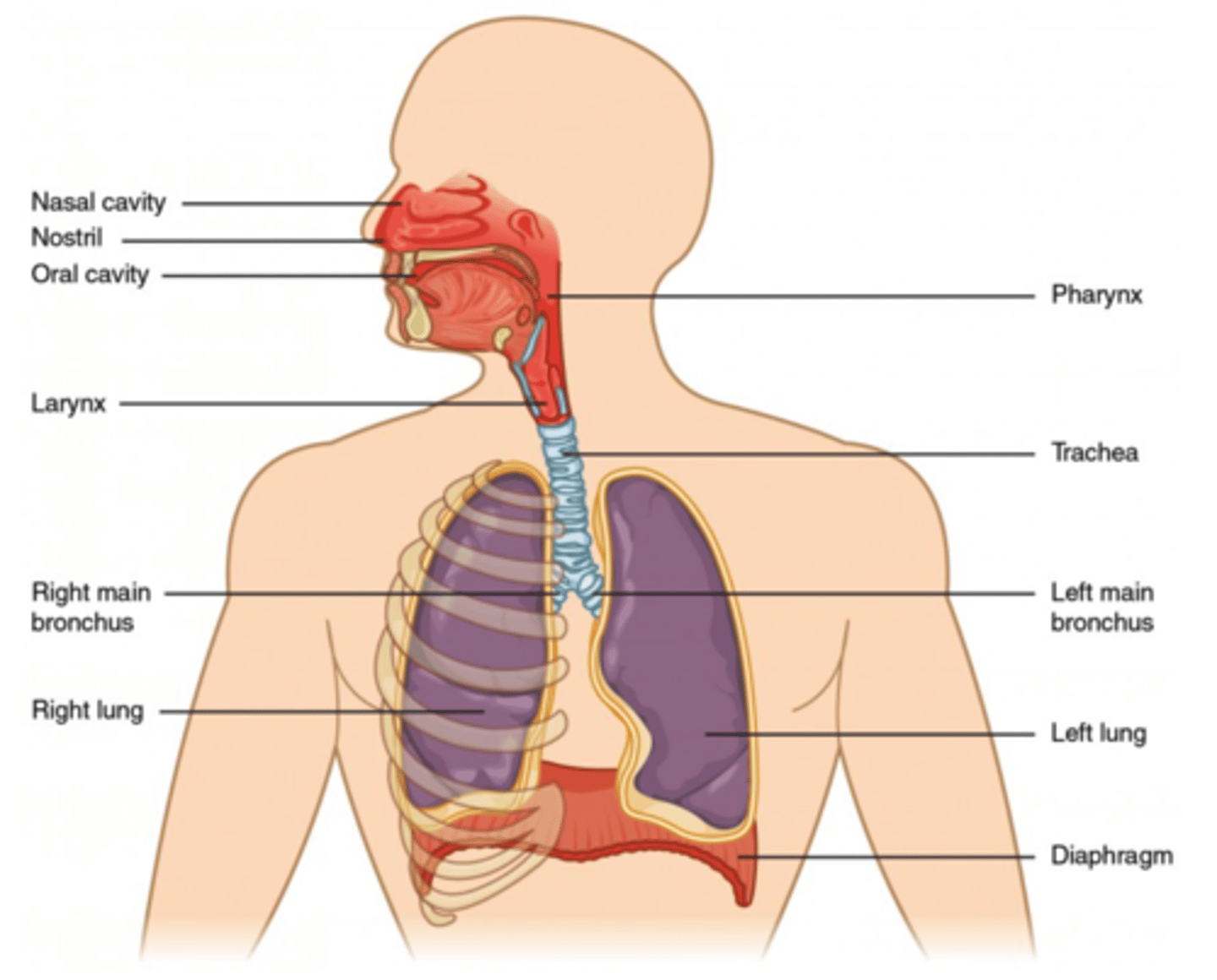
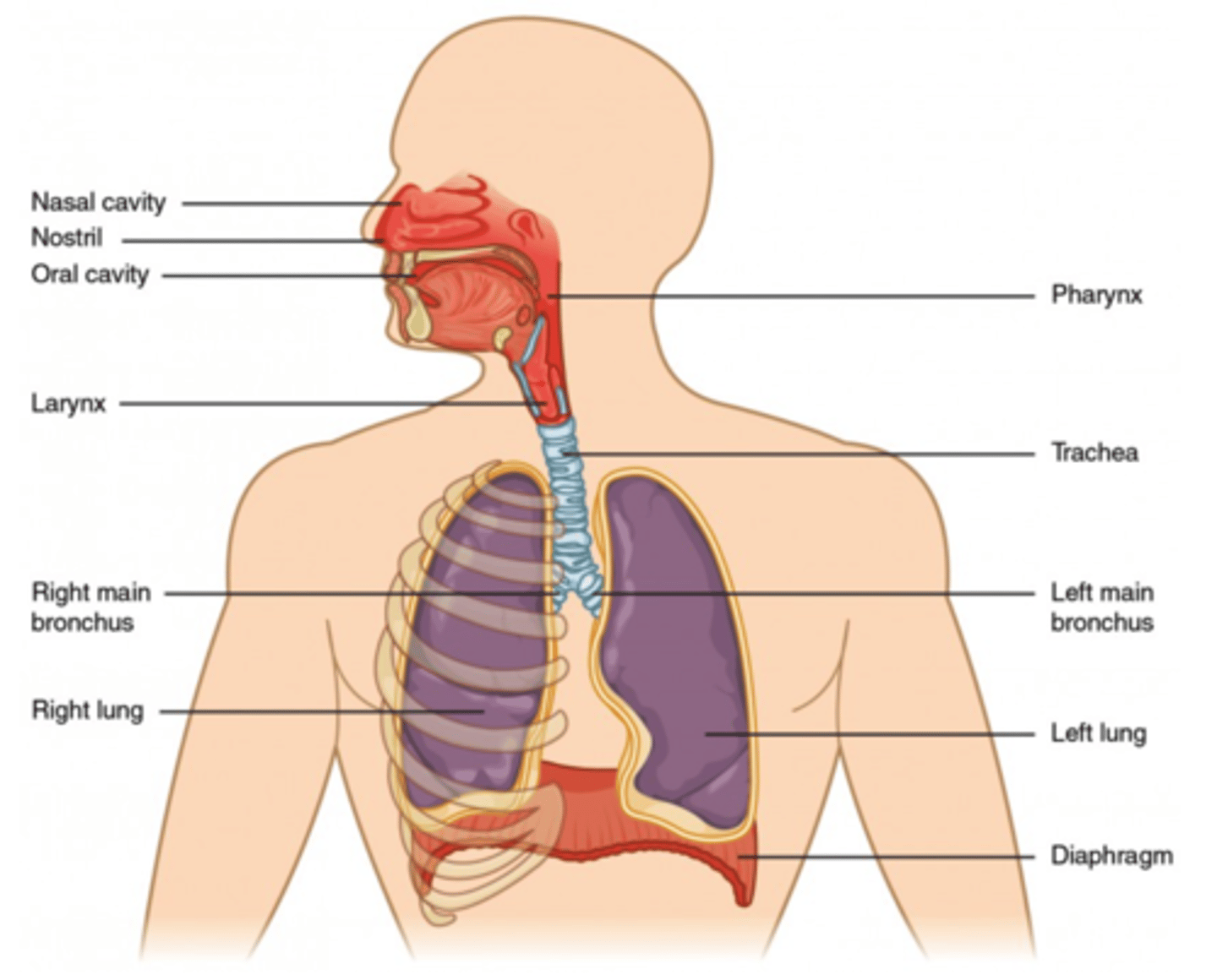
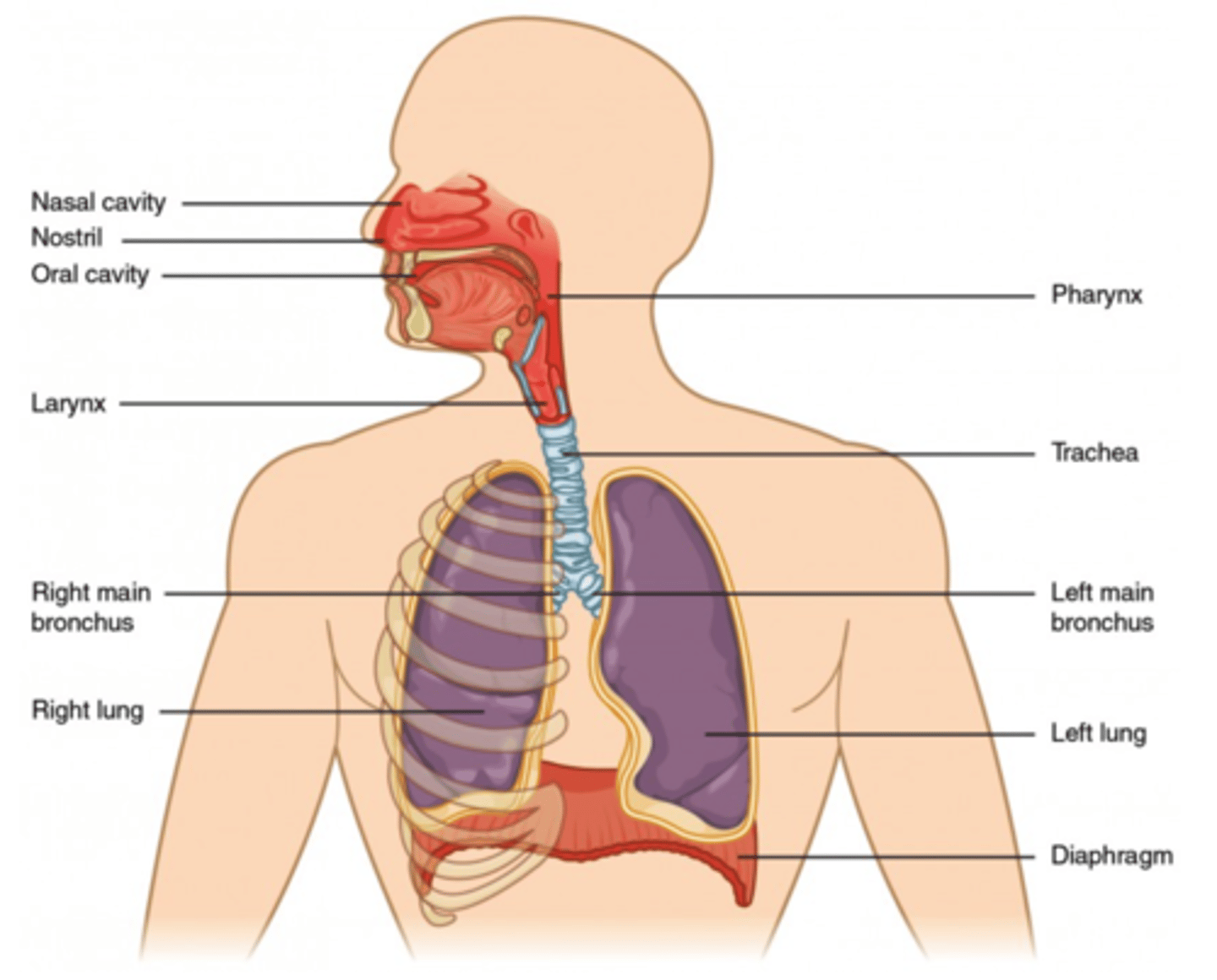
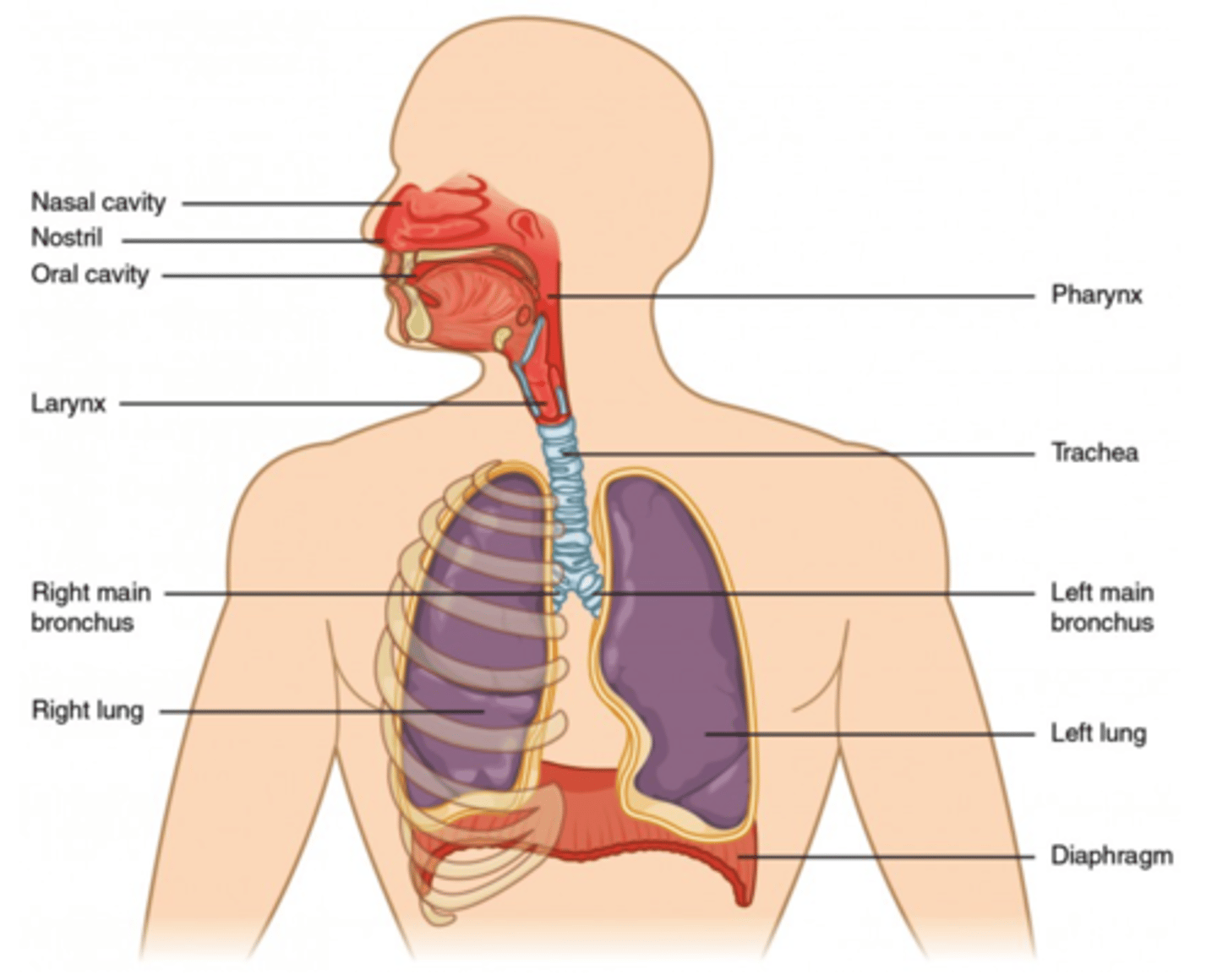
How many lobes does the left lung have?
two
(Note: the left lung has to be smaller than the right lung to make room for the heart)
How many lobes does the right lung have?
three
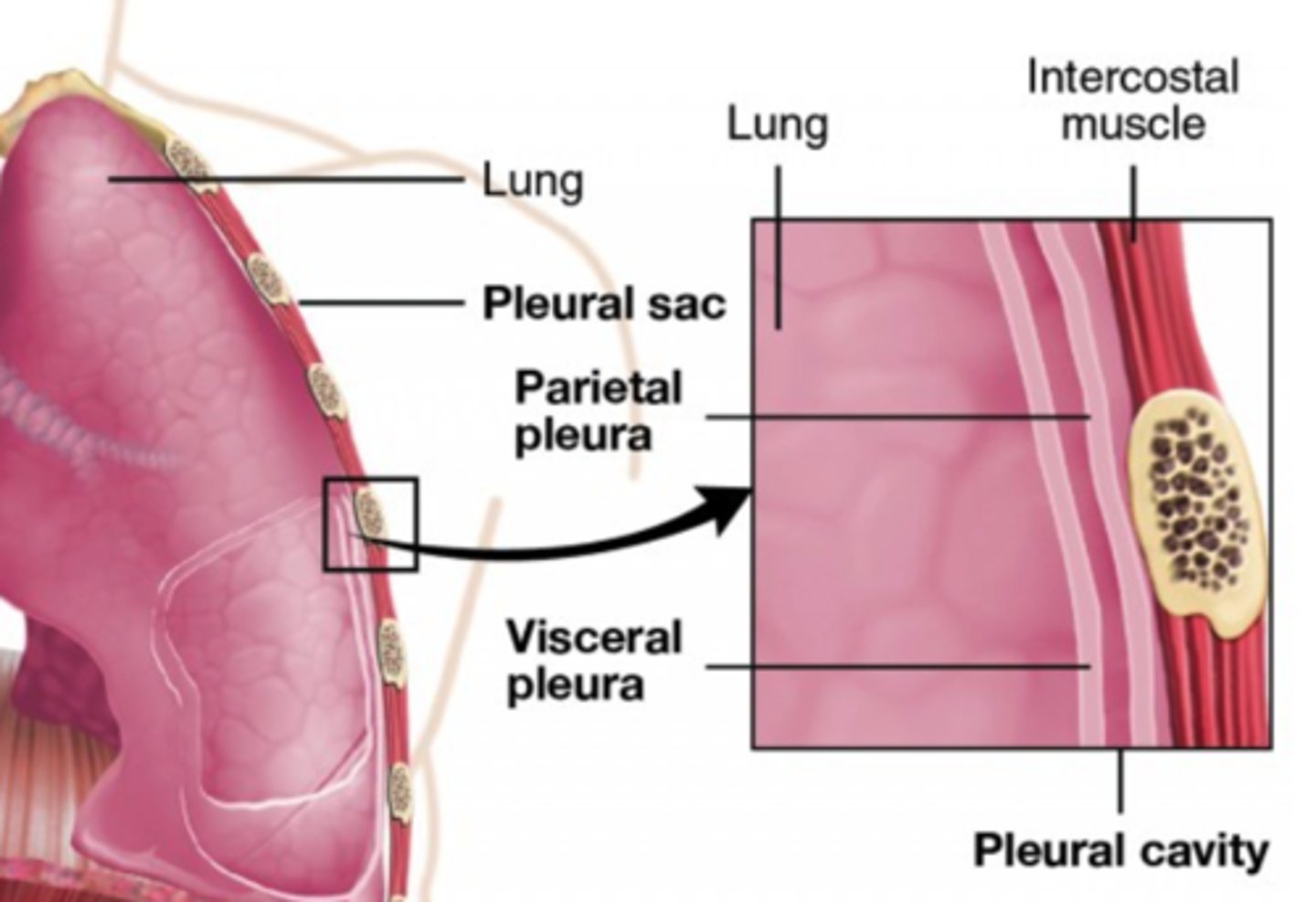
What are the membranous coverings of the lungs called?
pleurae
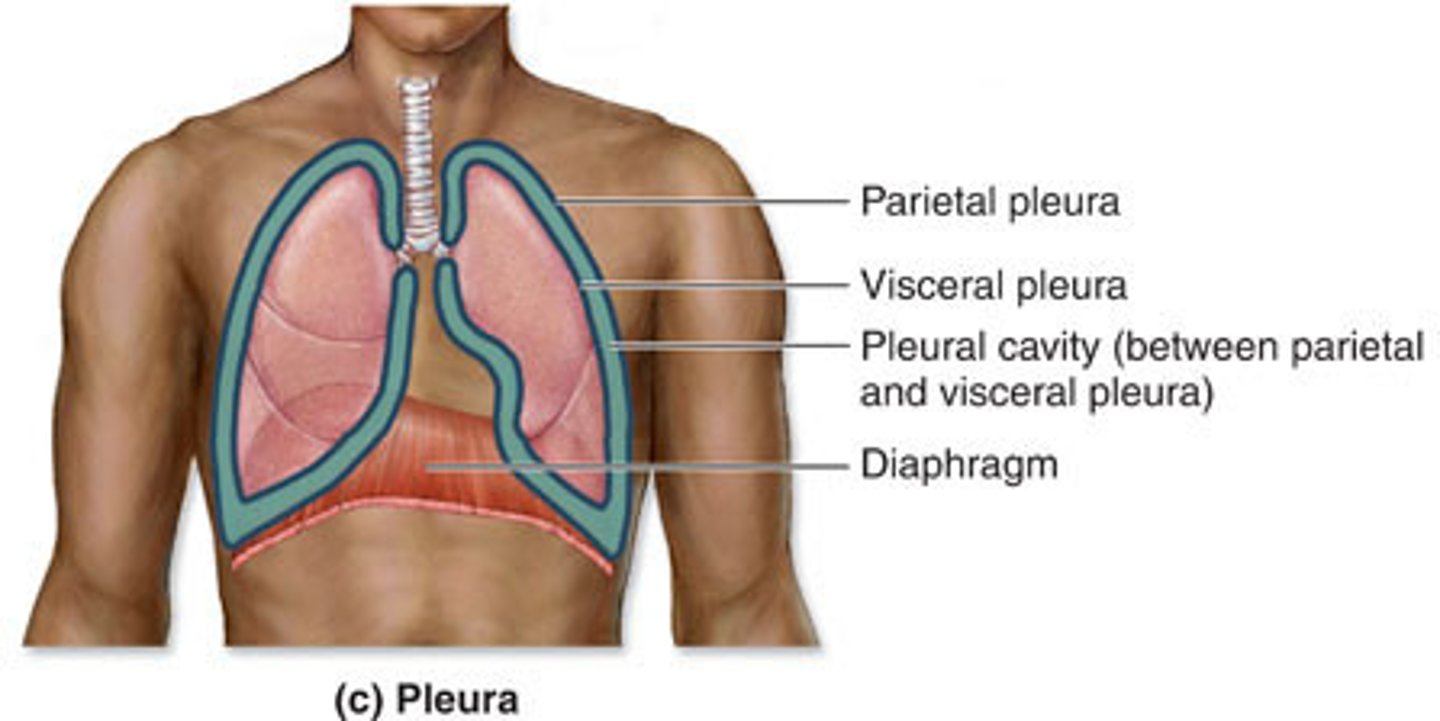
What are the two layers of the pleurae?
1. visceral pleura
2. parietal pleura
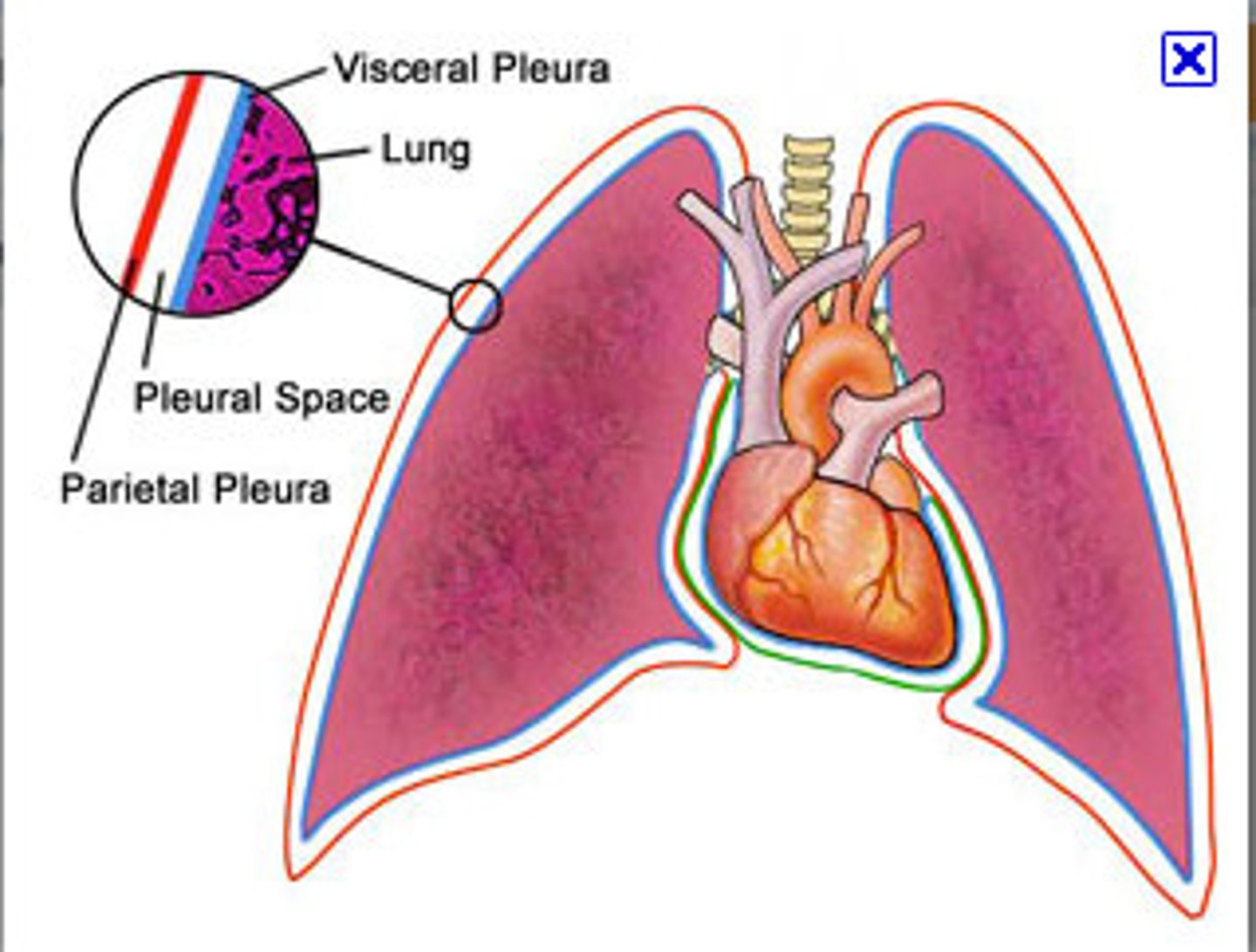
What is the space between the two layers of the pleurae called?
intrapleural space
(AKA: pleural space)
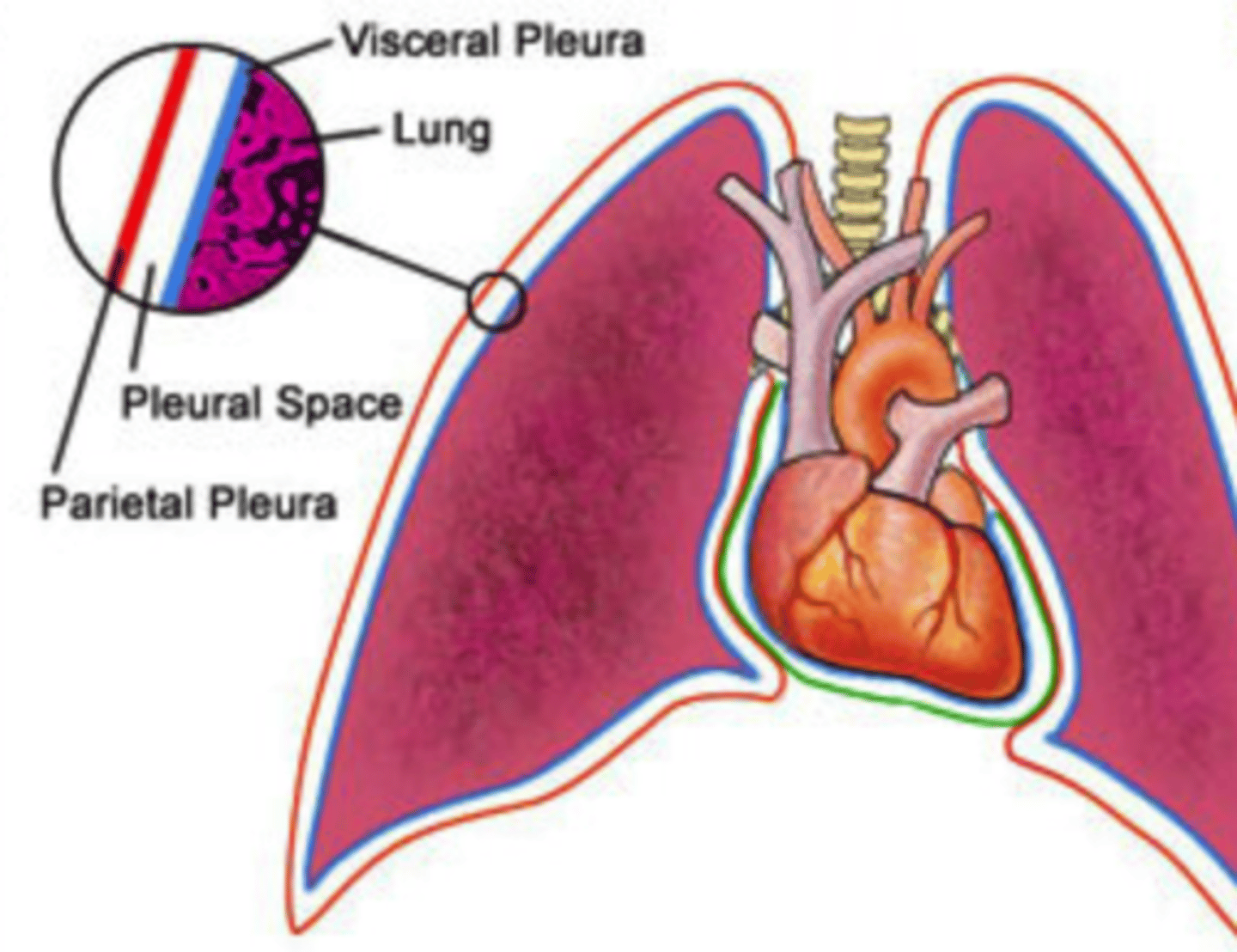
What does the visceral pleura line?
surface of the lungs
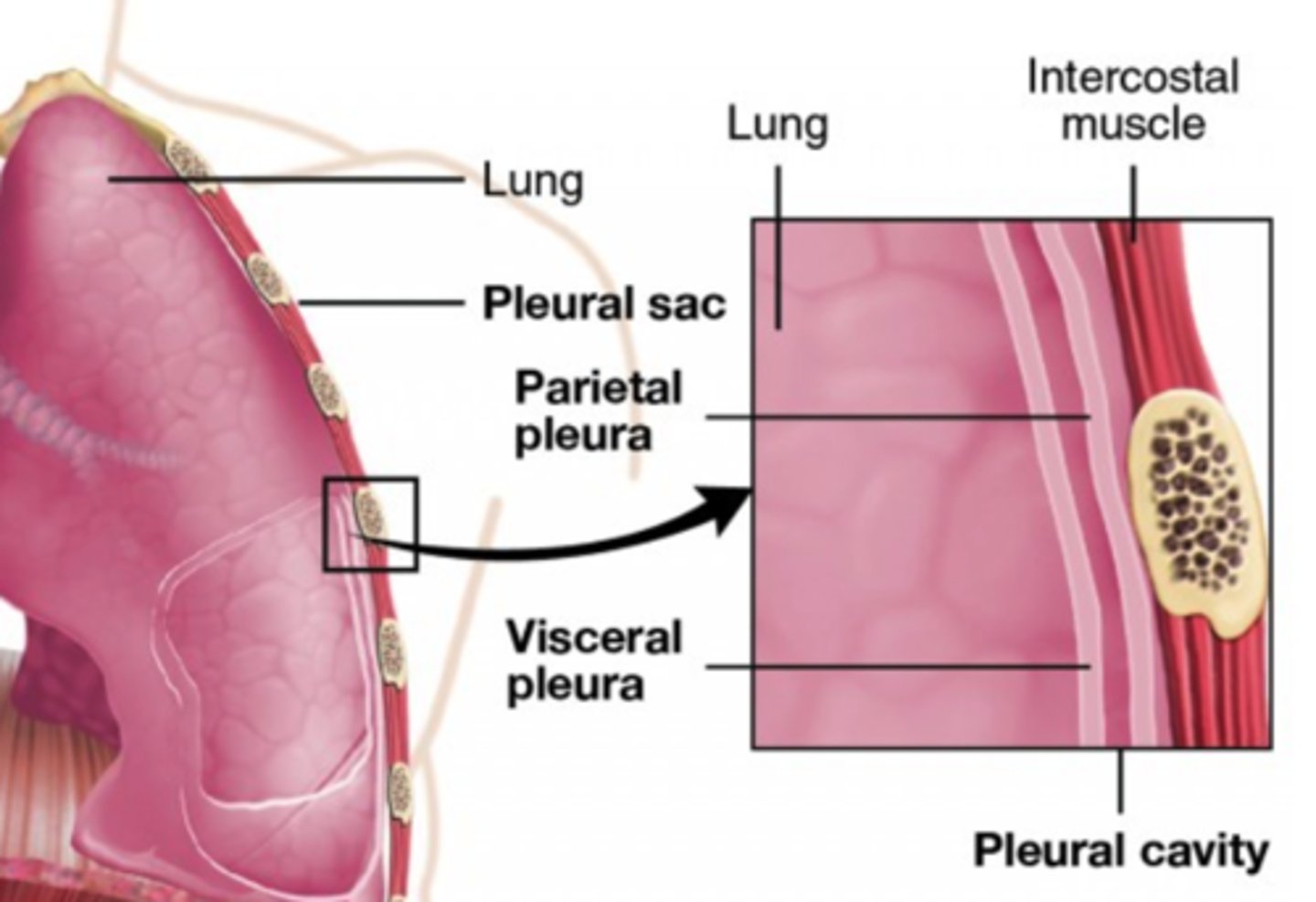
What does the parietal pleura line?
inside of the chest cavity
In the intrapleural space, how does the pressure compare to atmospheric pressure?
it has a lower (negative) pressure compared to atmospheric
(Note: this allows the lungs to remain inflated at all times)
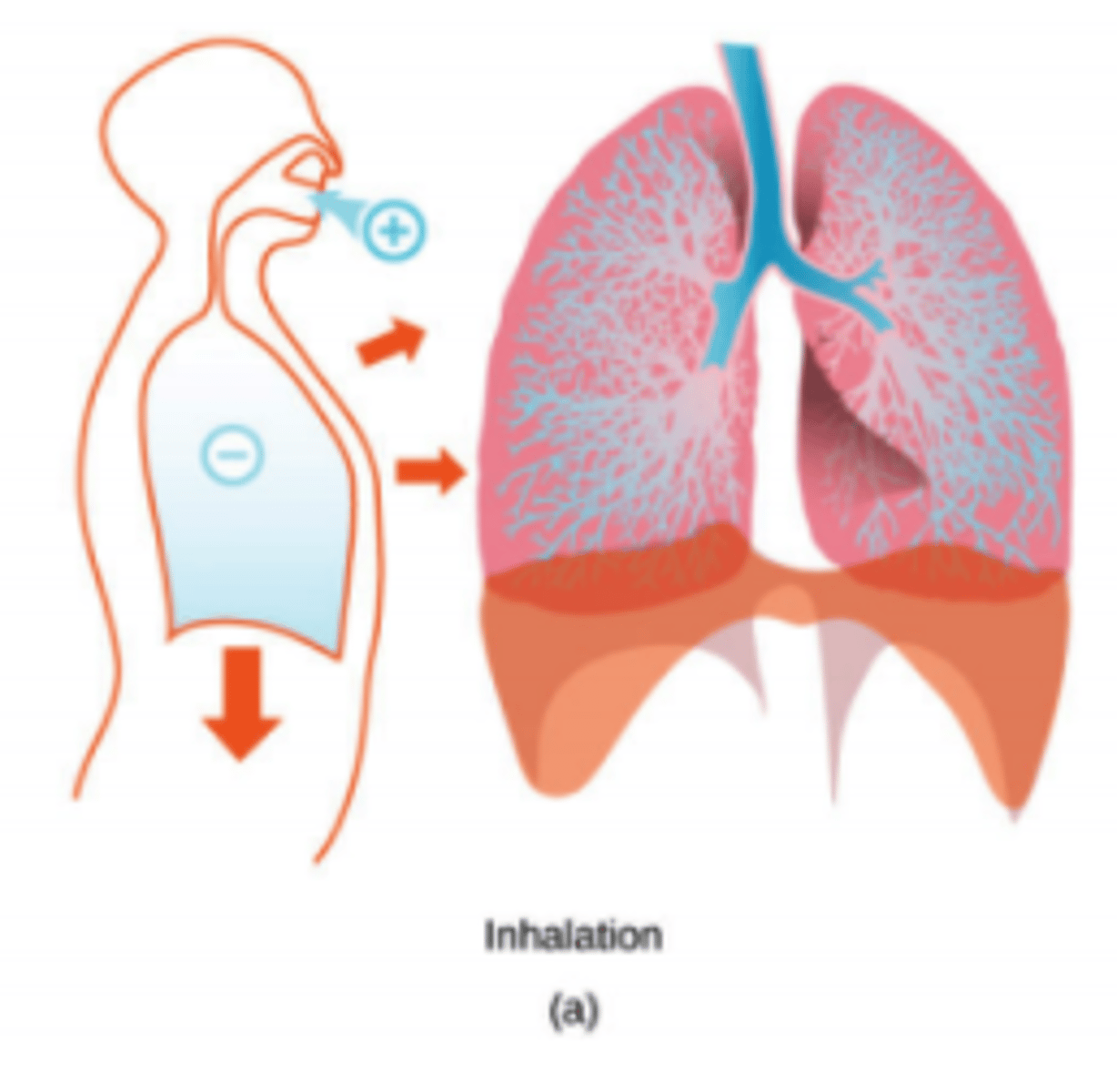
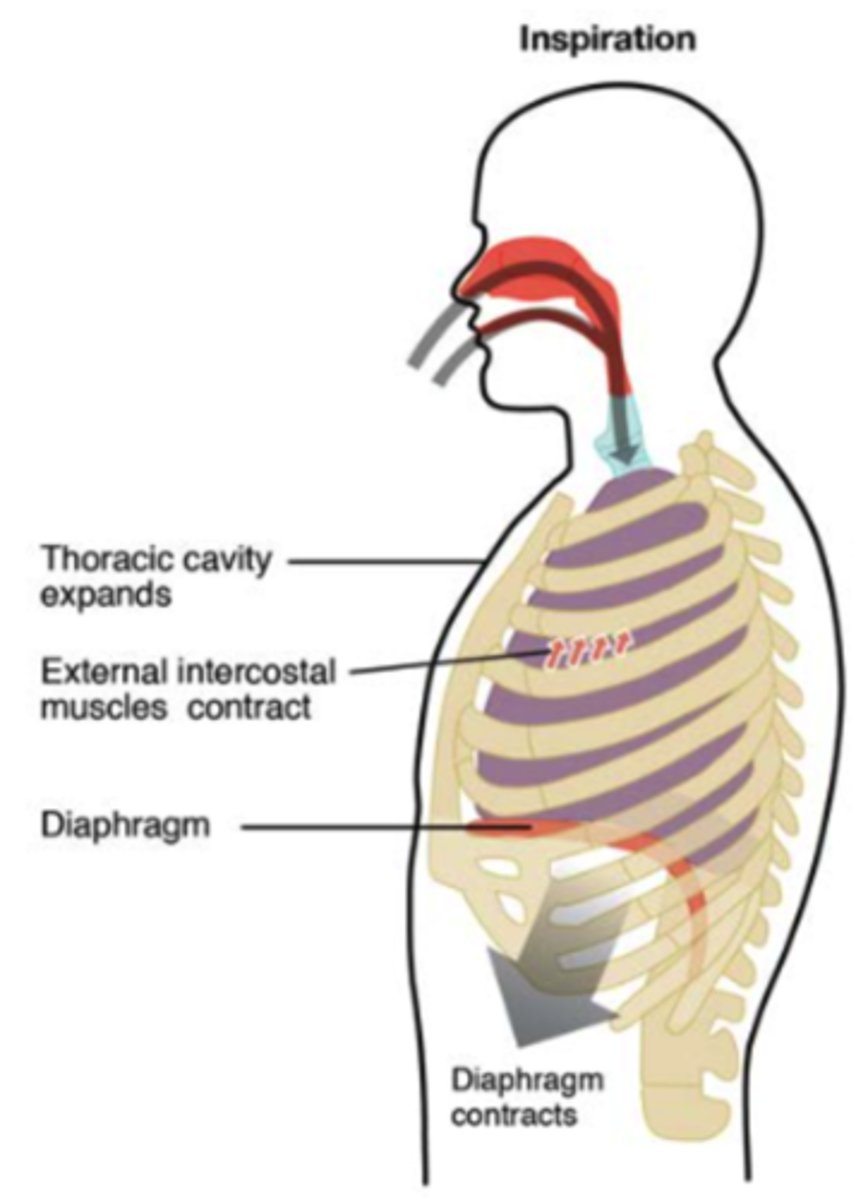
What happens to the pressure of the intrapleural space when we inhale?
the pressure decreases
What would happen to lungs if the intrapleural space was punctured?
lungs would collapse
(Note: intrapleural space is now atmospheric pressure, presses up against lungs which results in collapse)
What happens to the pressure inside the lungs when we inhale?
the pressure
decreases
(Note: diaphragm
contracts -> lung cavity
increases in volume ->
increased volume =
decreased pressure ->
air, which is higher pressure
rushes into lungs)
What happens to the pressure in the lungs when we exhale?
the pressure
increases
(Note: diaphragm
relaxes -> decreases
lungs' volume->
increases lungs'
pressure above
atmospheric->
air rushes out)
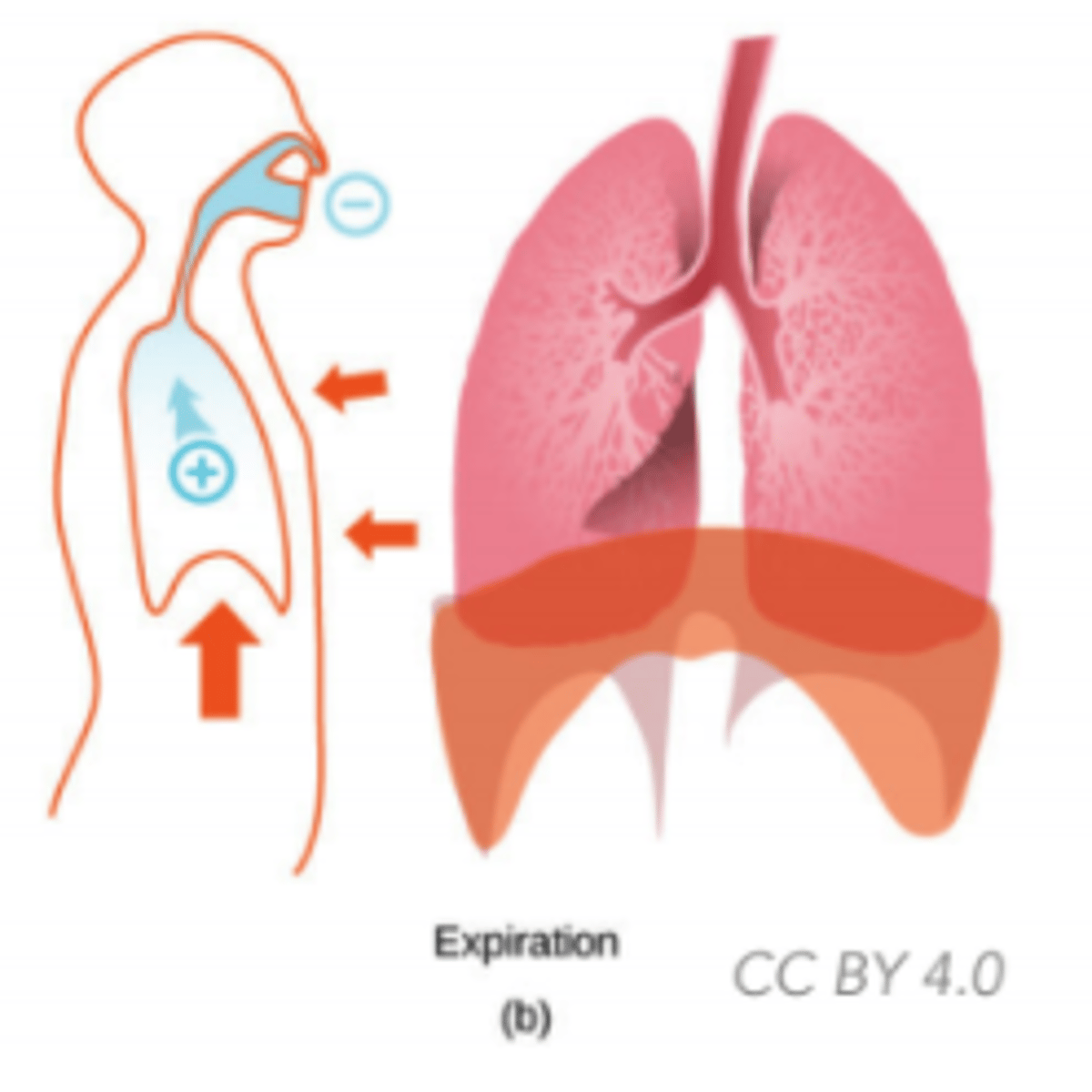
What kind of process is exhalation?
passive
What is the function of breathing?
gas exchange:
1. Oxygen (O2) in
2. Carbon dioxide (CO2) and water out
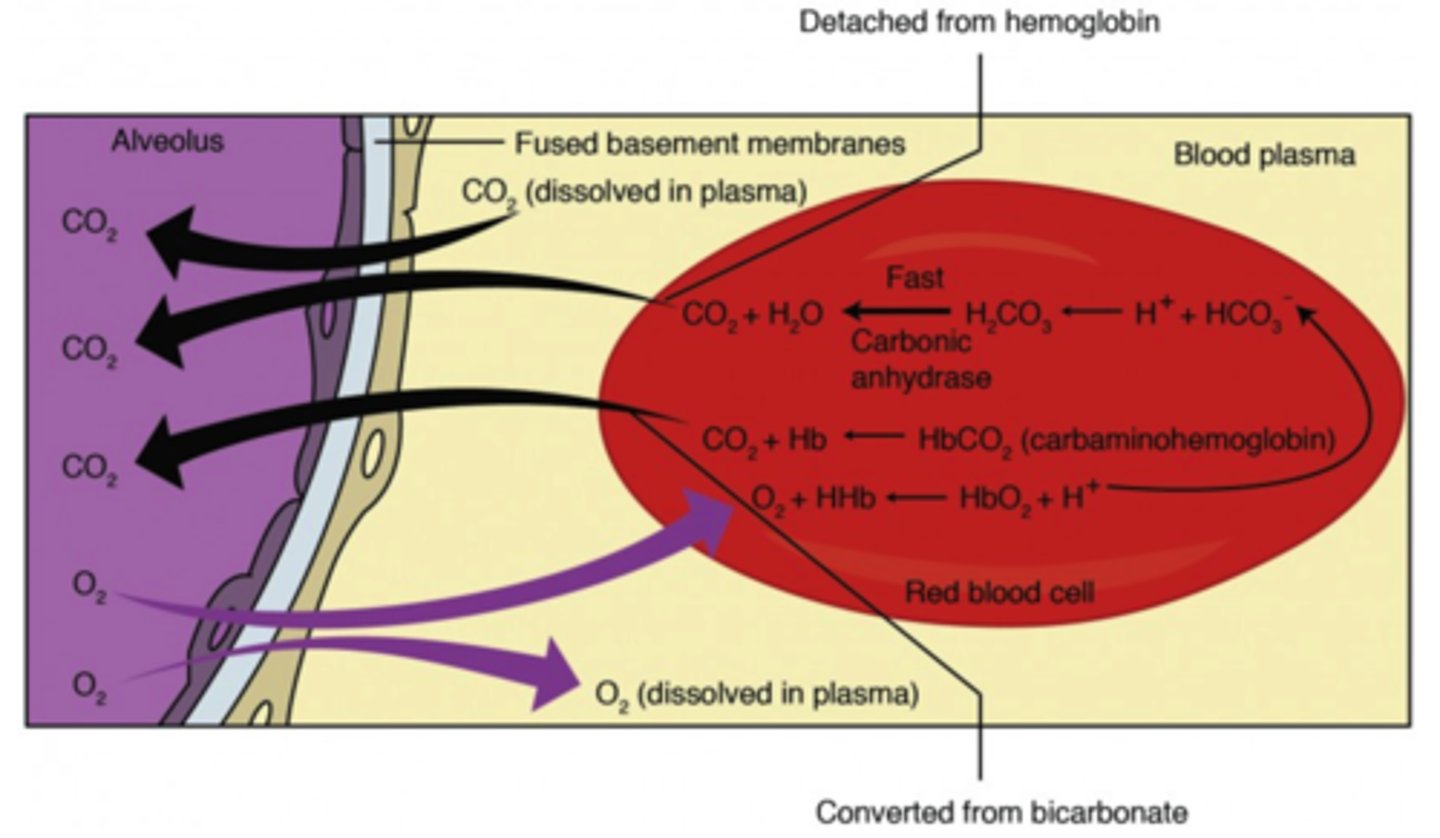
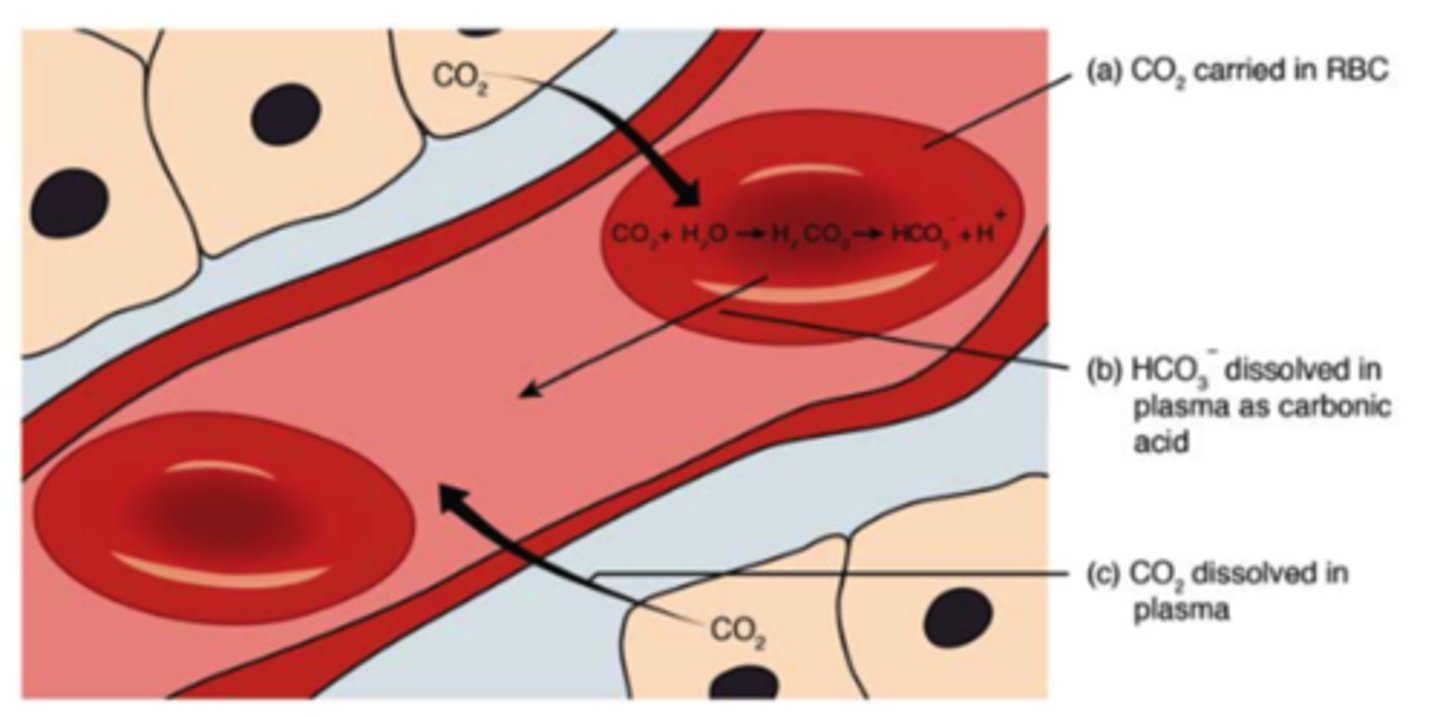
What form is CO2 mostly transported in blood?
as bicarbonate
(abbreviated as HCO3-)
What are the mechanisms by which CO2 is transported in the blood apart from HCO3-?
1. it can dissolve in the blood plasma in its gaseous form
2. it can bind to hemoglobin (called carbaminohemoglobin)
What is the reaction to convert CO2 into HCO3-?
(Note: carbonic acid intermediate)

What enzyme helps convert CO2 into HCO3-?
carbonic anhydrase
Where does the process of converting CO2 to HCO3- take place?
red blood cells (RBCs)
How is O2 carried in the blood?
hemoglobin in RBCs
What is the structure called where gas exchange occurs in the lungs?
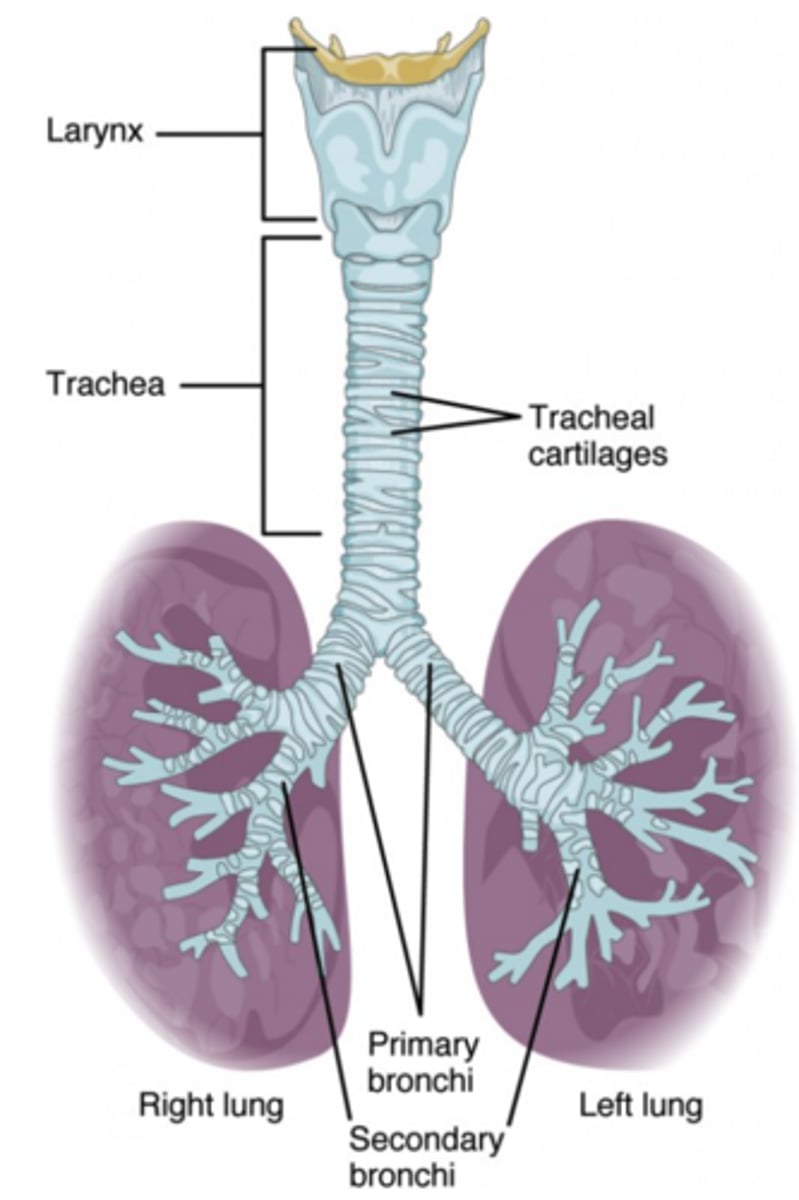
alveoli
What are alveoli coated in to reduce surface tension?
surfactant
(Note: too much surface tension from H2O would collapse the alveoli)
What are the two kinds of epithelial cells in human alveoli?
1. type 1 (structural support)
2. type 2 (produce surfactant)
What structure filters, moistens, and warms incoming air in the respiratory system
nose
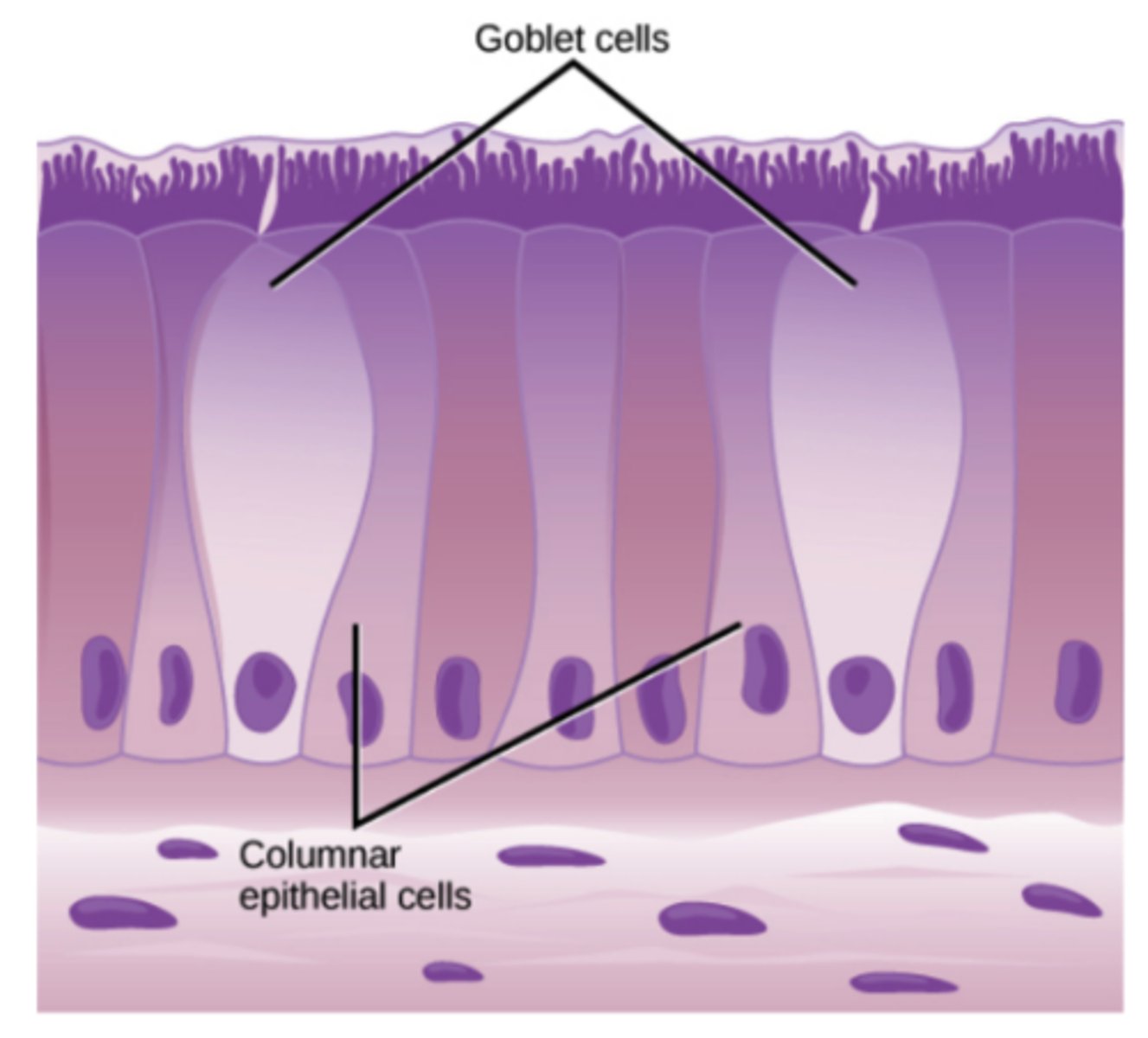
What structures secrete mucus and trap large dust particles in the nose?
goblet cells
What structure is called the throat and acts as a passageway for food and air?
pharynx
How are dust and mucous removed from the pharynx?
swept back from nose by cilia - disposed by either spitting or swallowing
What structure is called the voice box?
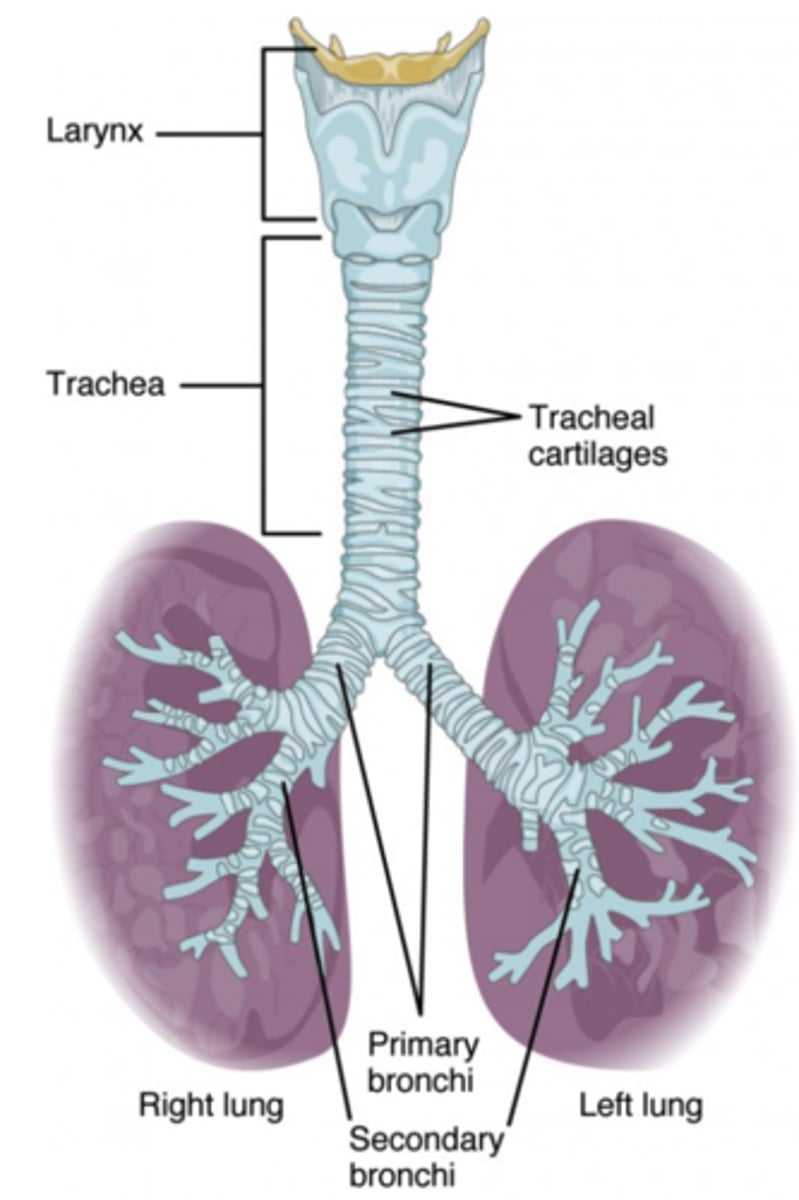
larynx
If non-gas enters larynx, what response is activated?
cough reflex
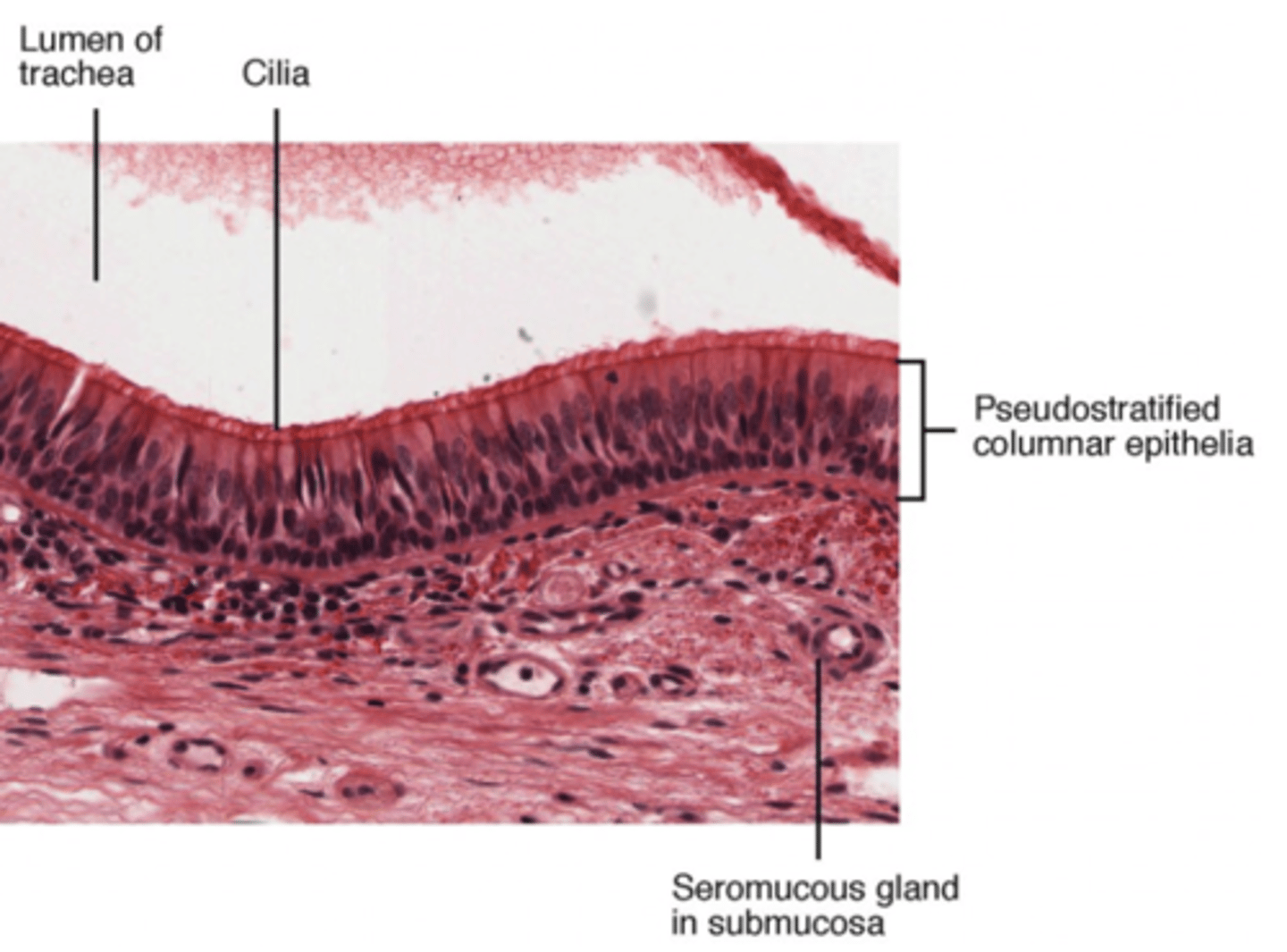
What structure contains C shaped rings of cartilage and functions to deliver air to and from lungs?
trachea
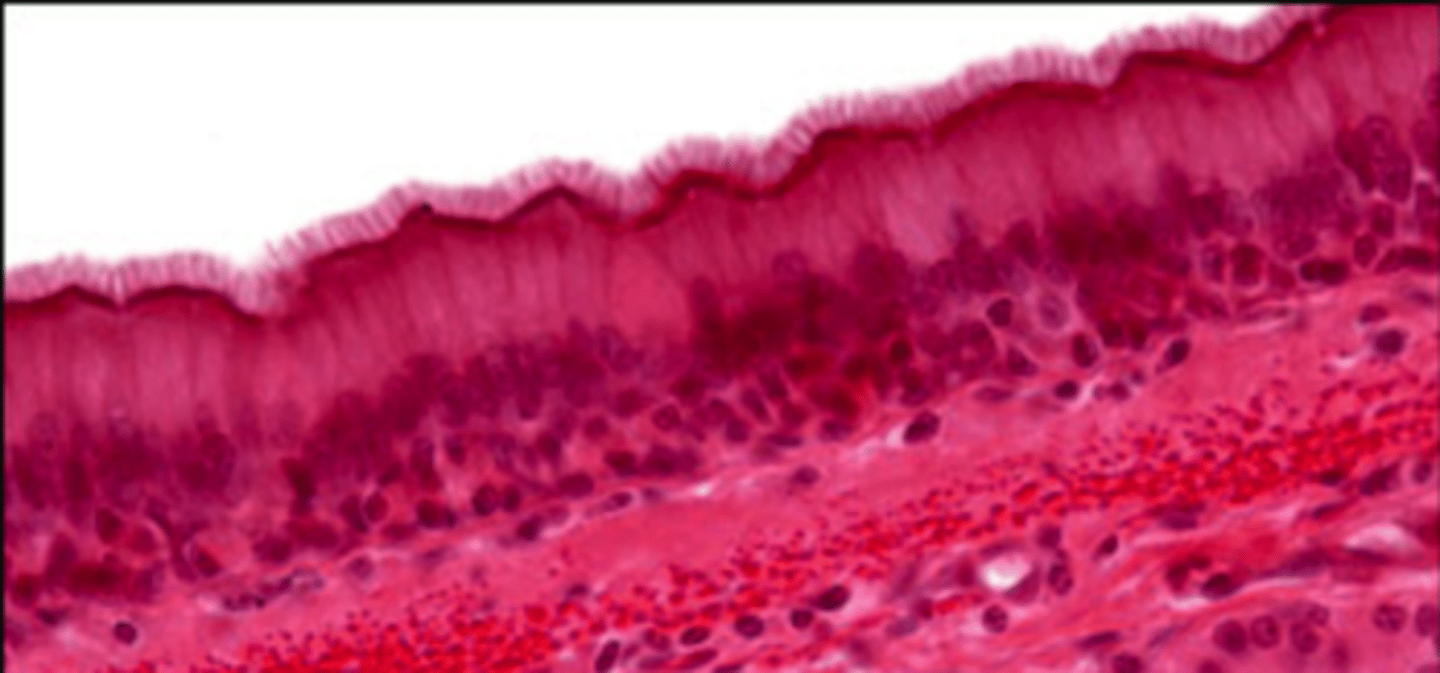
What is the trachea covered by to remove debris from the airway?
ciliated mucus cells
What are the first branches off the trachea into the lungs?
two bronchi
What are the smaller branches off the two bronchi in the lungs called?
bronchioles (AKA secondary bronchi)
What are the small sacs at the end of the bronchiole branches in the lungs called?
alveoli
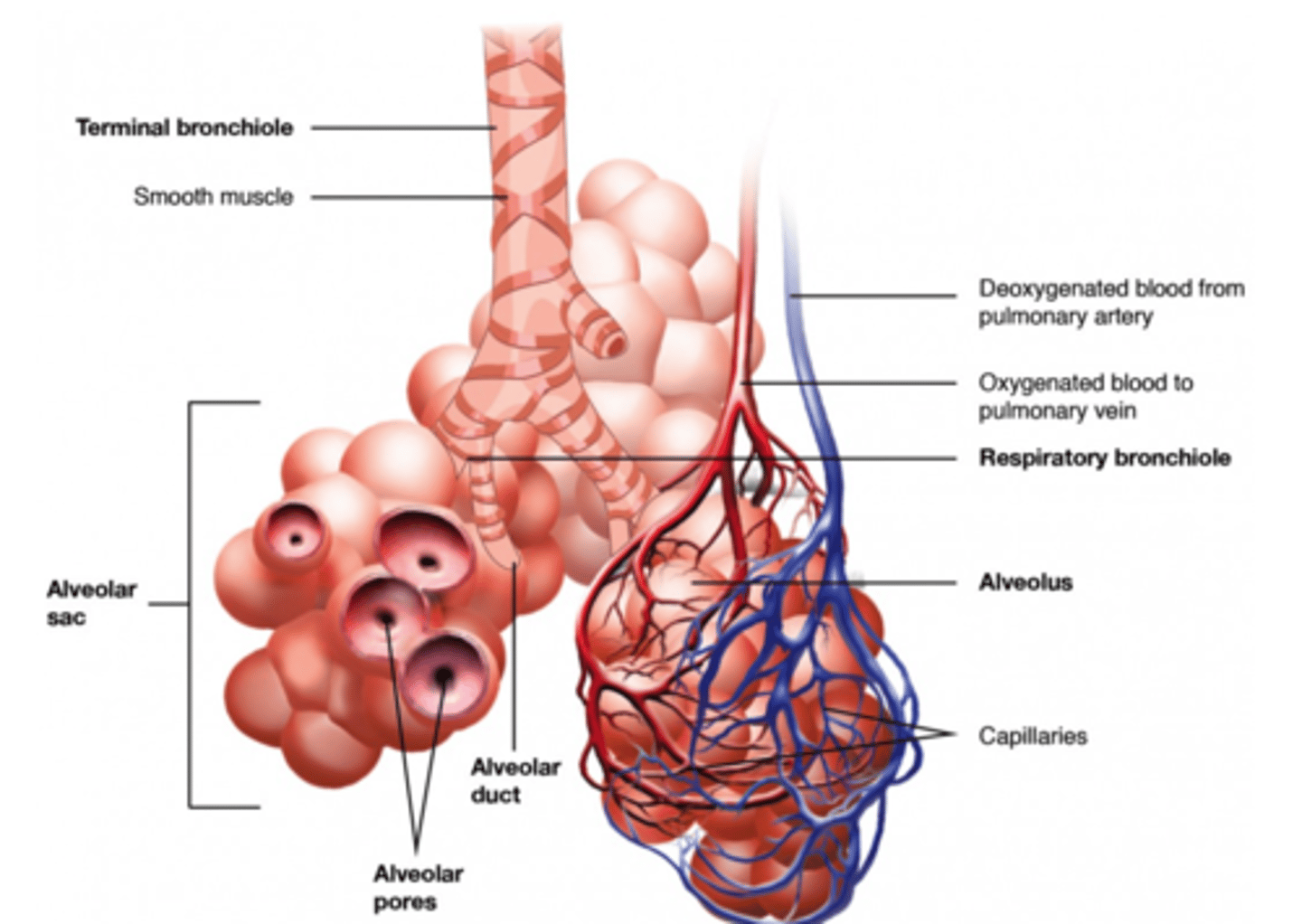
What are the alveoli surrounded by?
blood-carrying capillaries
(Note: this is the whole point of having alveoli - LOTS of surface area to exchange gas with blood)
How does gas cross the moist, sac membranes of the alveoli?
simple diffusion
How does O2 transfer into the tissues?
diffuses out of RBCs-> capillary wall->interstitial fluids->cell membranes->cytoplasm
(Note: process for CO2 is the same steps in reverse)
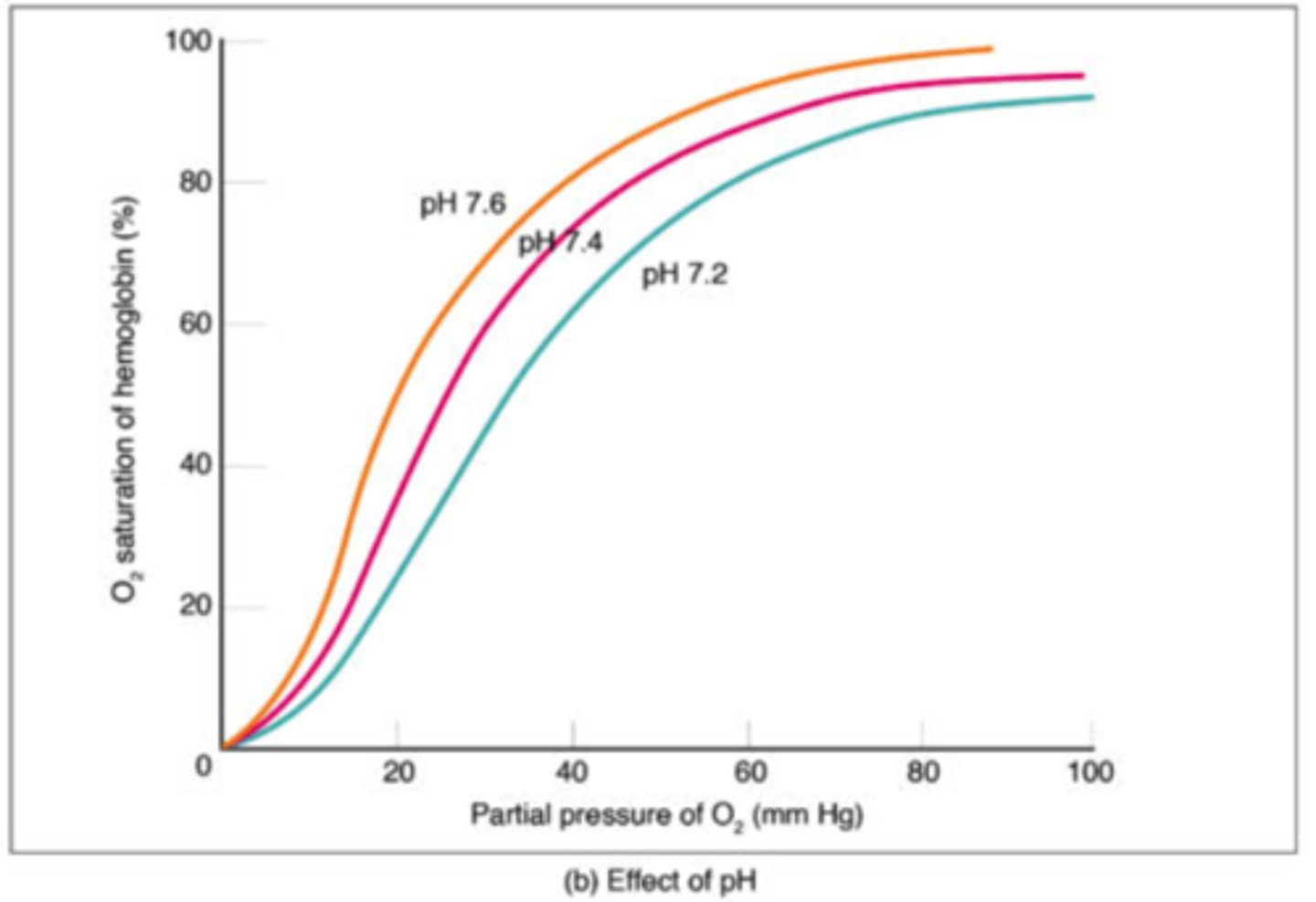
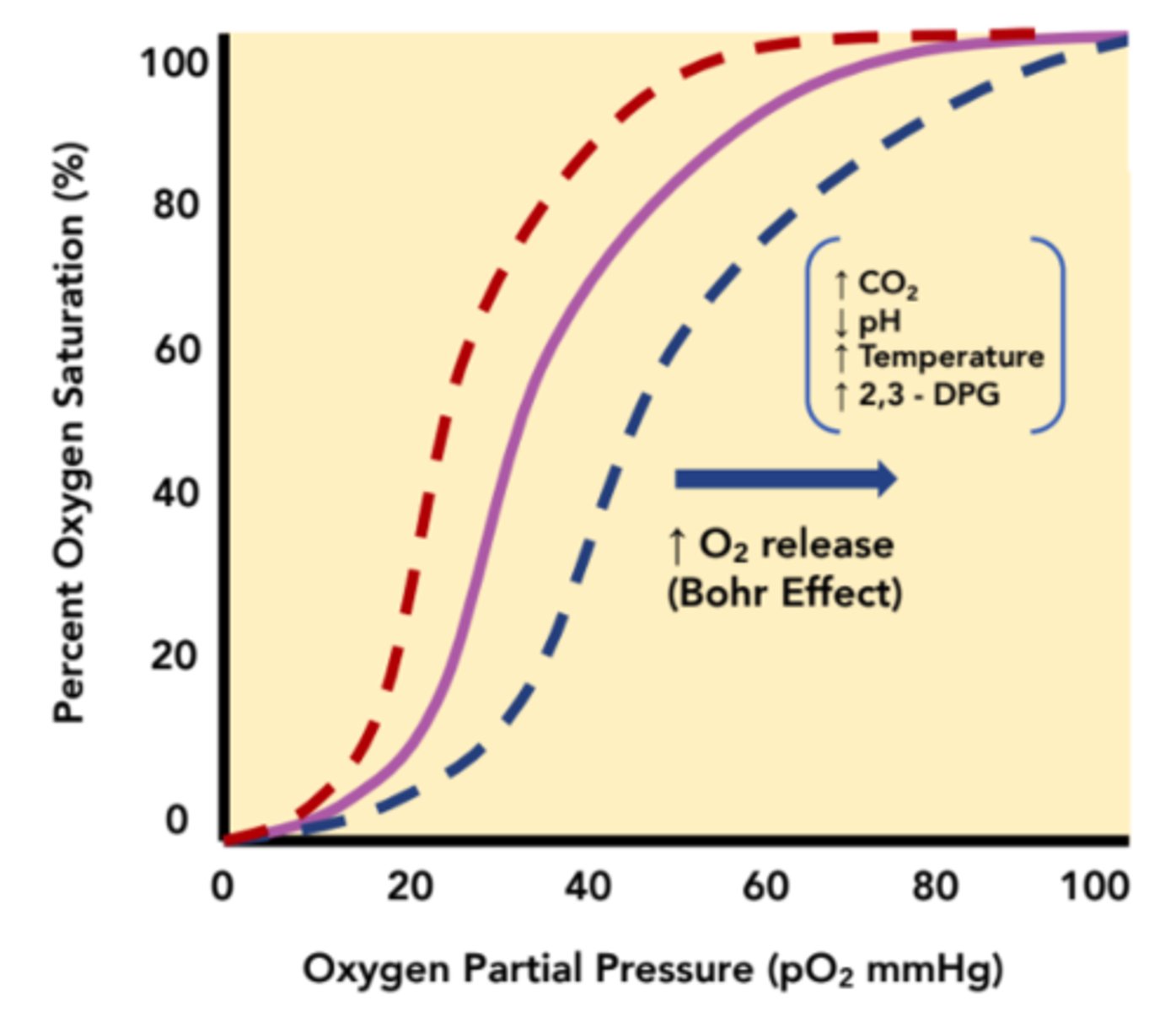
What describes an important phenomenon that refers to the shift in the oxygen dissociation curve caused by changes in the concentration of CO2 or pH?
Bohr Effect
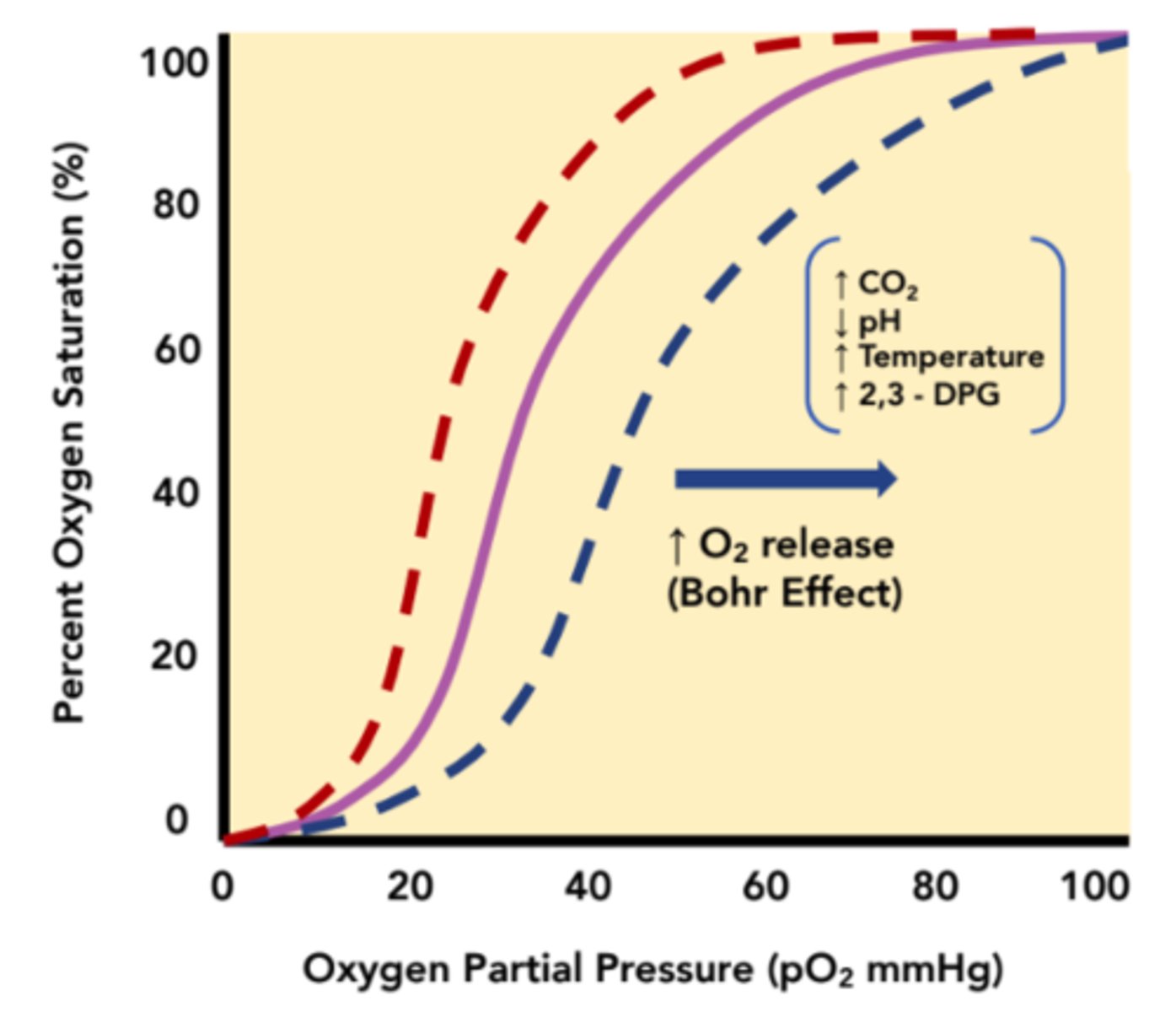
What shift on an oxygen dissociation curve corresponds with a decrease in hemoglobin's affinity for oxygen?
right shift
(Note: dotted blue line)
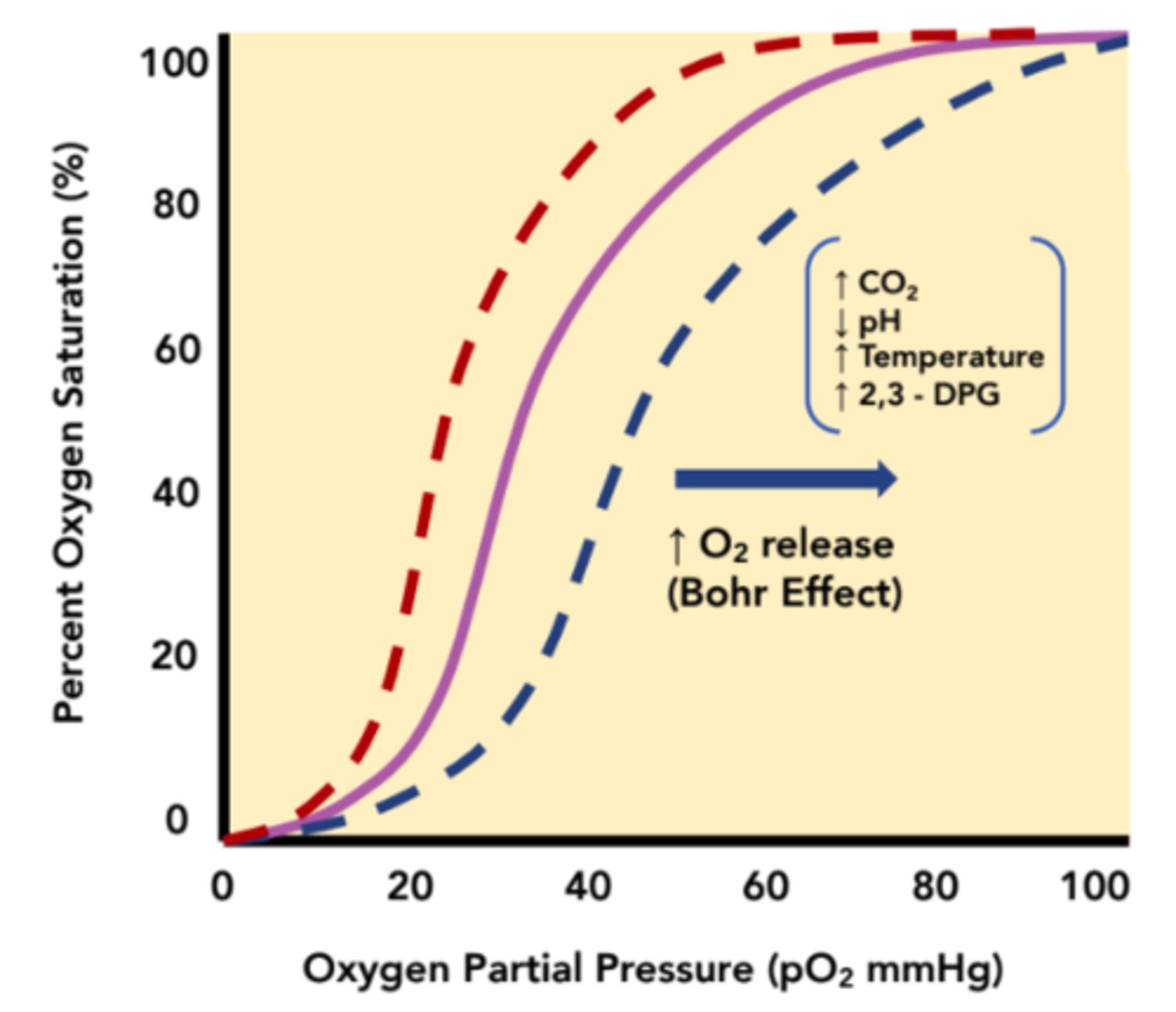
What shift in an oxygen dissociation curve corresponds with an increase in hemoglobin's affinity for oxygen?
left shift
(Note: dotted red line)
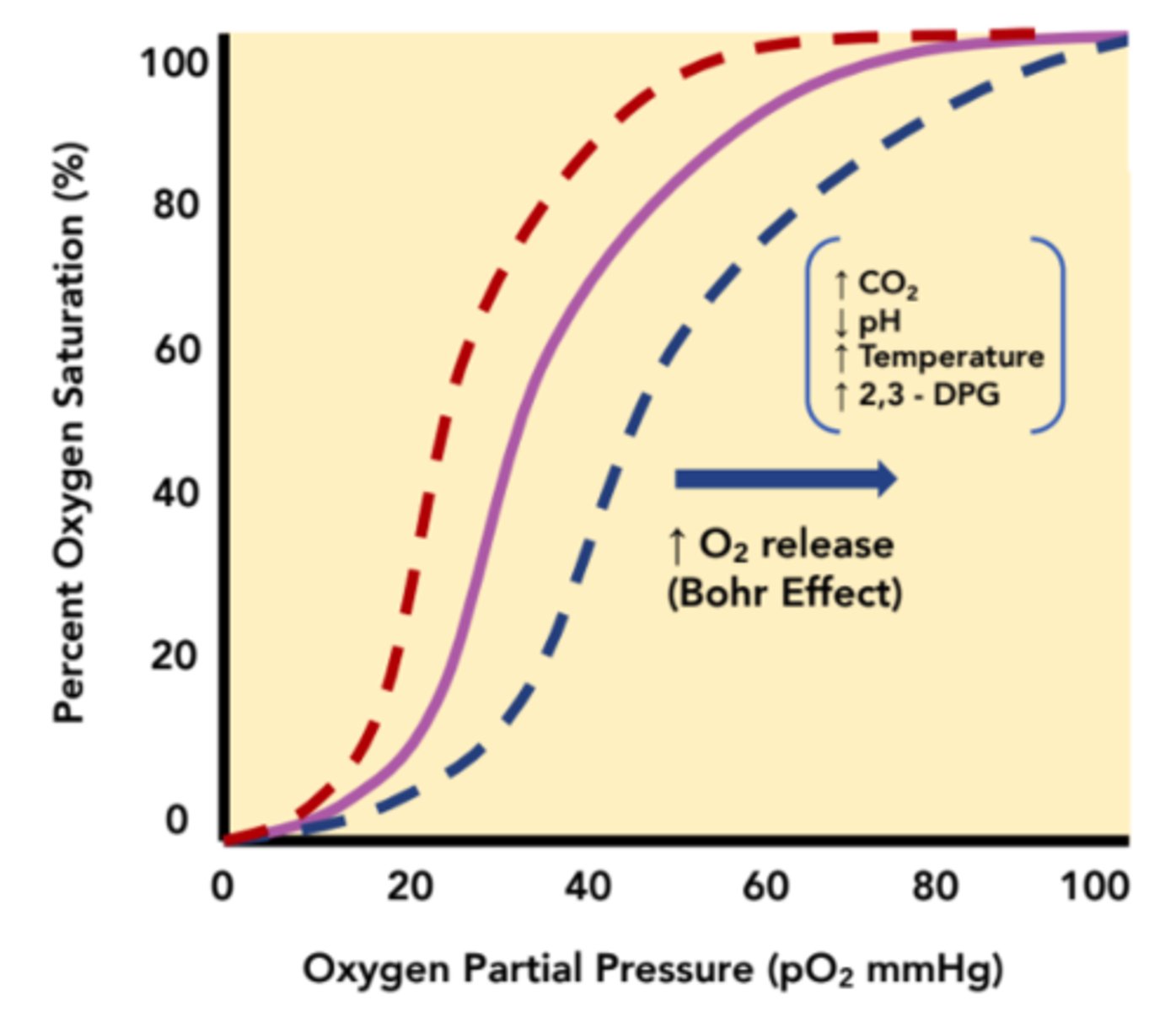
What shift does increased CO2 cause in the oxygen dissociation curve?
right shift
(Note: increased CO2 in tissues
- lot of respiration
- more acidic
- and require more O2)
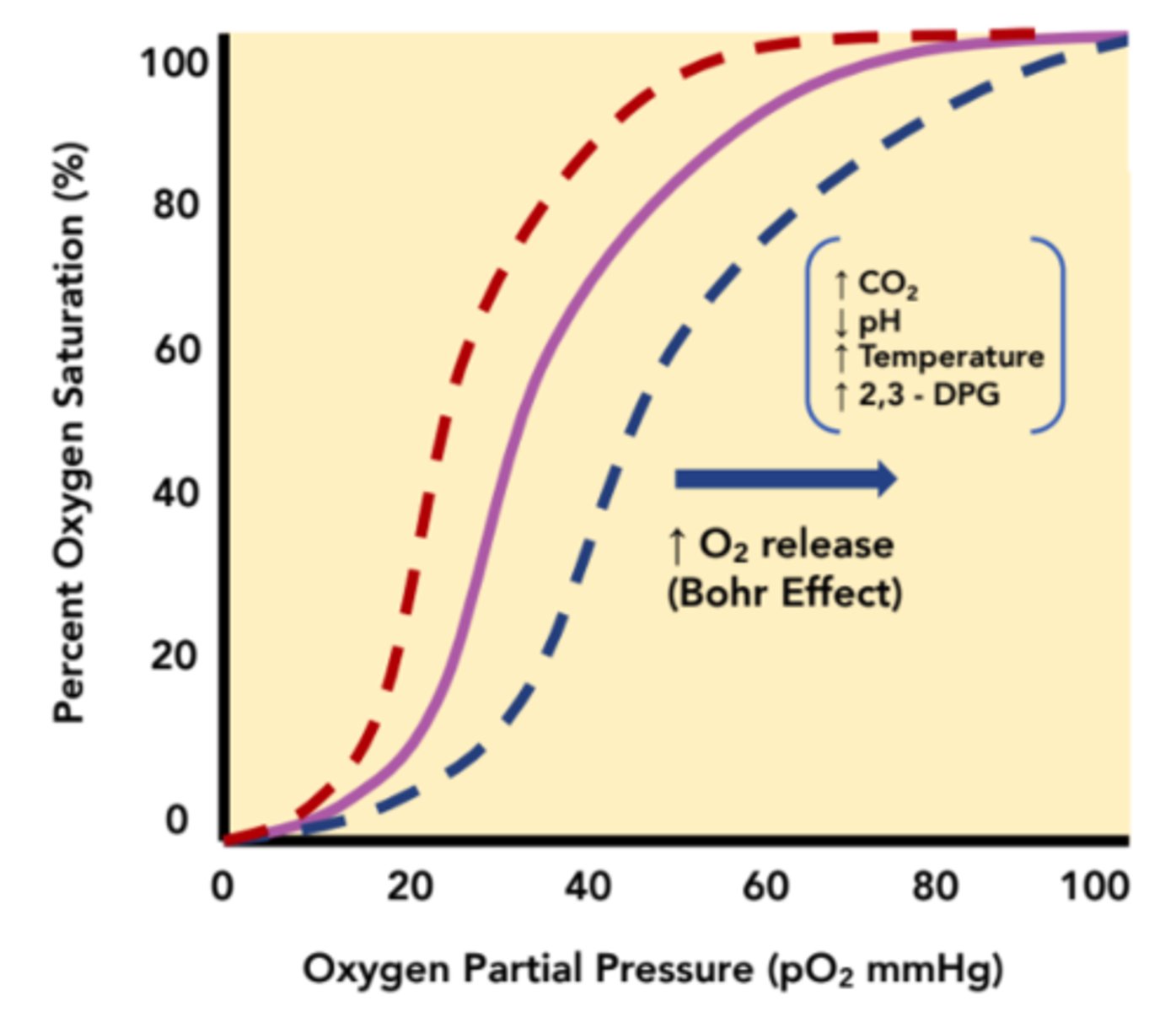
What shift does increased pH cause in the oxygen dissociation curve?
left shift
(Note: increased pH
means less acidity in
tissues = less respiration
taking place =
less oxygen requirements)
What shift does increased temperature cause in the oxygen dissociation curve
right shift
(structure of
hemoglobin favors
its deoxygenated state
in high temperature)
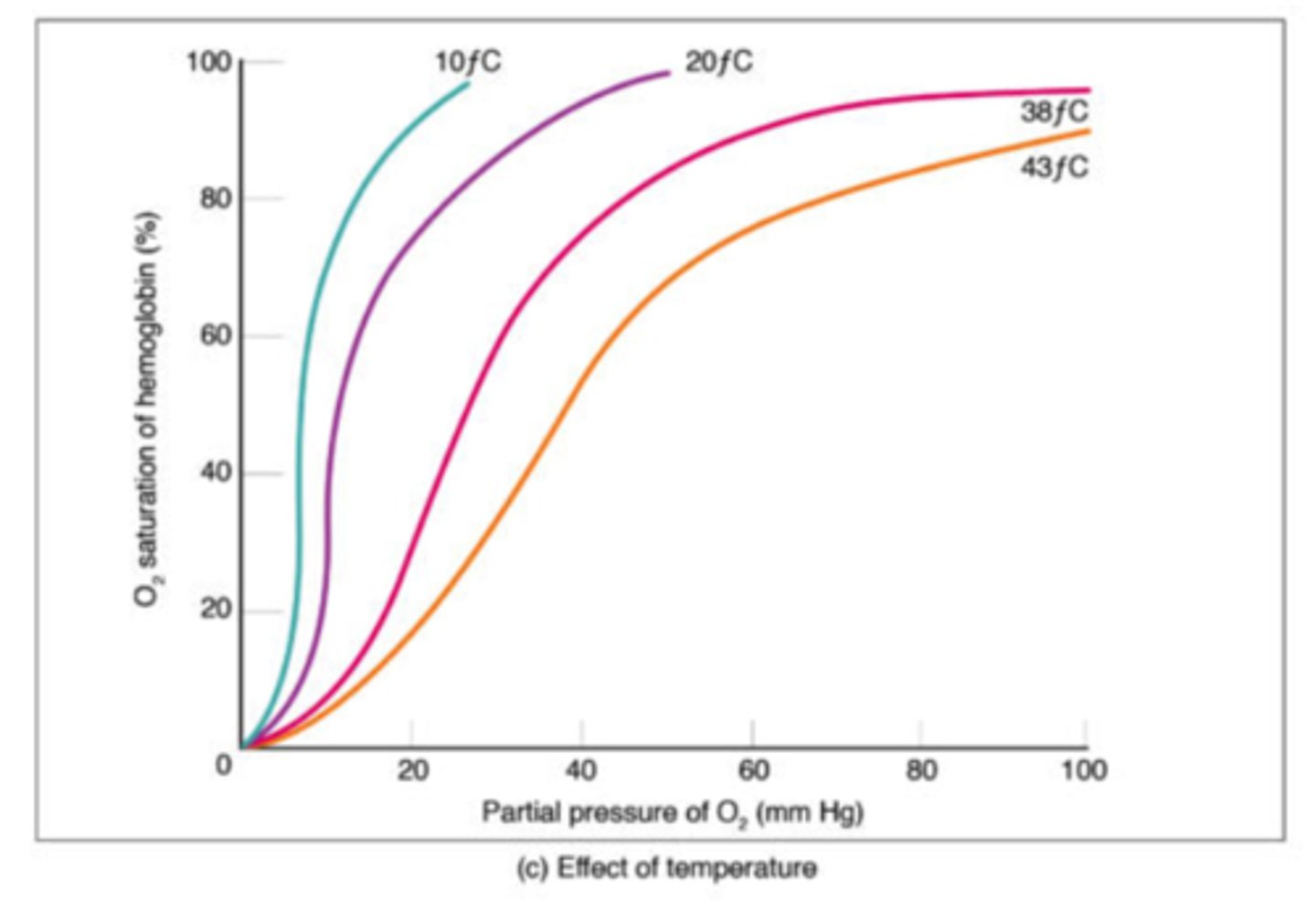
What shift does increased 2,3-DPG AKA 2,3-BPG cause in the oxygen dissociation curve?
right shift
(binds to hemoglobin
and stabilizes its
deoxygenated state =
more O2 release)
How is 2,3-DPG produced?
1. made from an intermediate compound in glycolysis
2. made from an enzyme catalyzed reaction at low O2 levels.
What effect does increased exercise have on CO2 levels?
increases CO2 production
(Note: this result drops blood pH because CO2 is converted to HCO3- and H+ in RBCs)
What is the mnemonic to help remember all the factors that shift the oxygen dissociation curve right?
a CADET faces right
C - CO2
A - Acid
D - DPG
E - Exercise
T - Temperature
(Note: an increase
in all of these things
shifts the curve right)
How do you know what shifts the oxygen dissociation curve left?
think CADET but opposite!
(Note: decrease in all the factors results in shift left = increasing hemoglobin's affinity for oxygen)
What effect does high CO2 and H+ have on hemoglobin?
structural change to reduced form = release O2 to tissues and preferentially binds to CO2
How does hemoglobin release CO2 back at the lungs?
1. at lungs conditions are high O2, low CO2
2. hemoglobin structure shifts to non-reduced state
3. unloads CO2, picks up O2
What term describes how the deoxygenation of blood increases its ability to carry CO2?
Haldane Effect
What does the Haldane Effect say about oxygenated hemoglobin?
decreased ability to hold CO2
When hemoglobin is reduced, what state does it have the capacity to form?
carbaminohemoglobin = non-oxygen carrying kind
(Note: this is the mechanism for how the Haldane effect works)
What is the best way to summarize the Haldane effect?
[O2] affects hemoglobins binding to CO2 and H+
(note: process works in synchrony to facilitate the liberation of O2 and uptake of CO2 and H+)
What percent of blood oxygen binds rapidly and reversibly to hemoglobin in RBC's?
98%
(Note: called oxyhemoglobin)
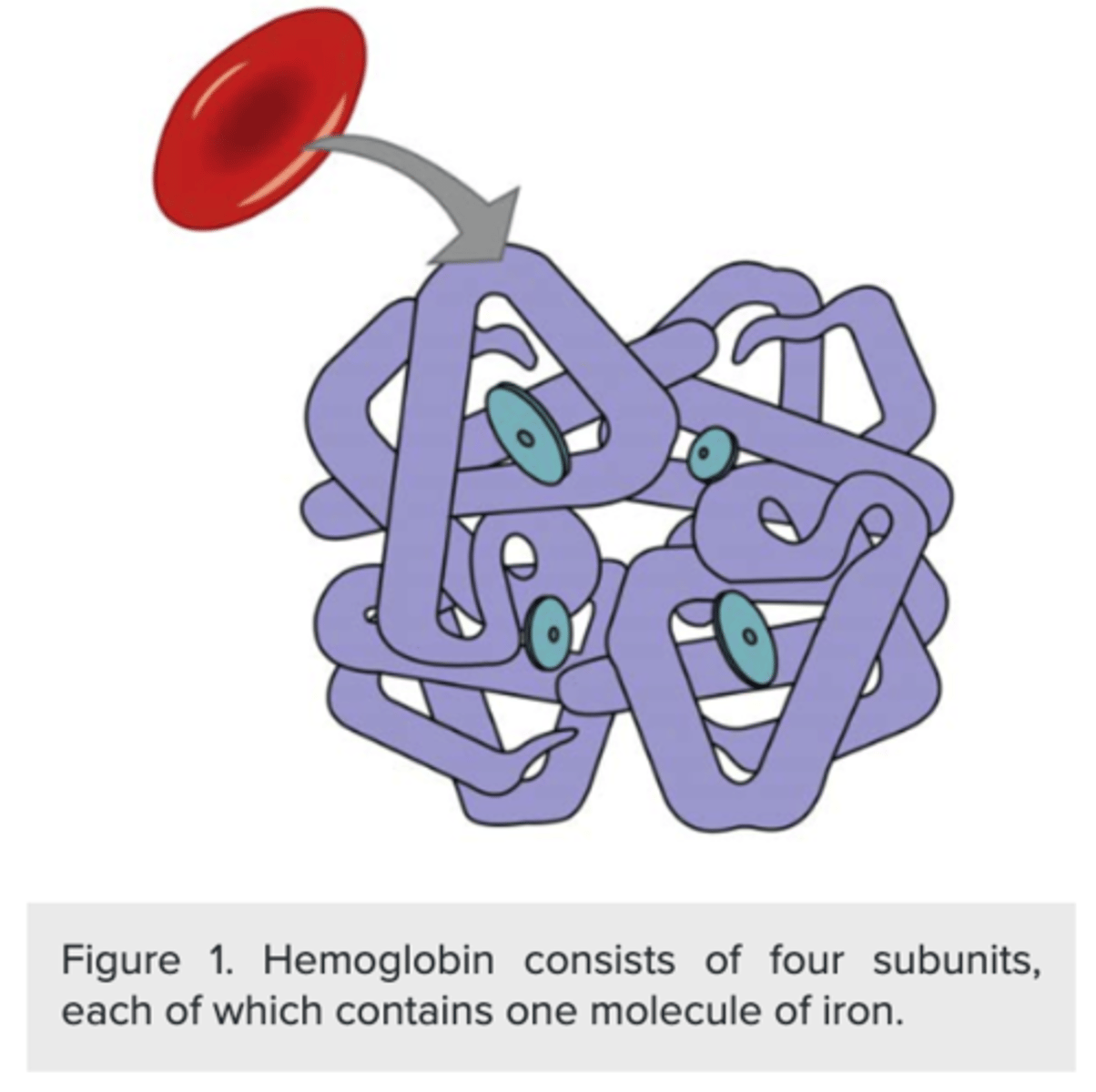
How many subunits does hemoglobin have?
four
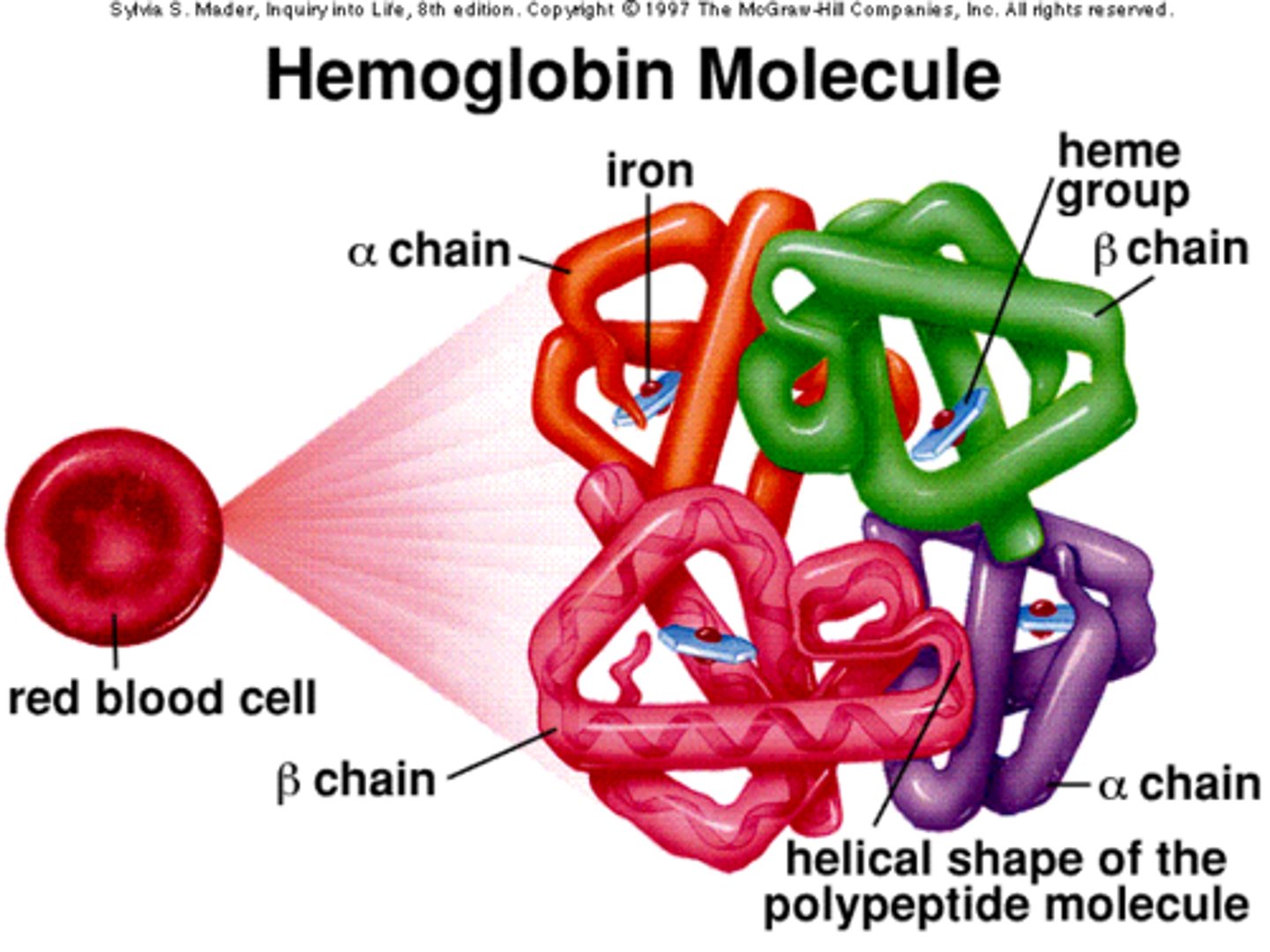
Each hemoglobin subunit houses a _____ cofactor
heme
(Note: organic molecule
with an iron atom in the center)
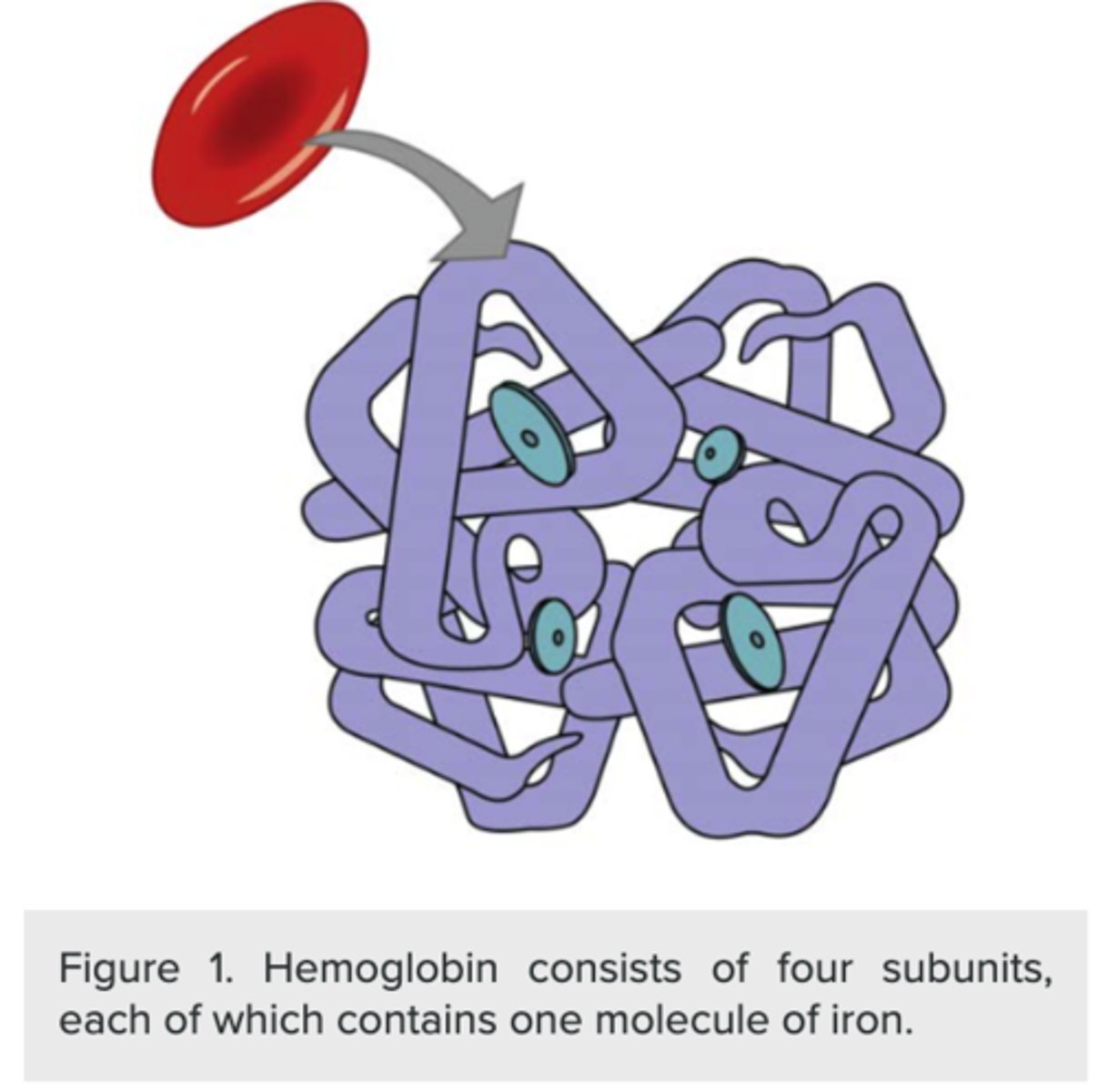
How many O2 molecules can the iron atom in a heme cofactor bind?
one O2 molecule
(Note: total of four in
one molecule of hemoglobin)
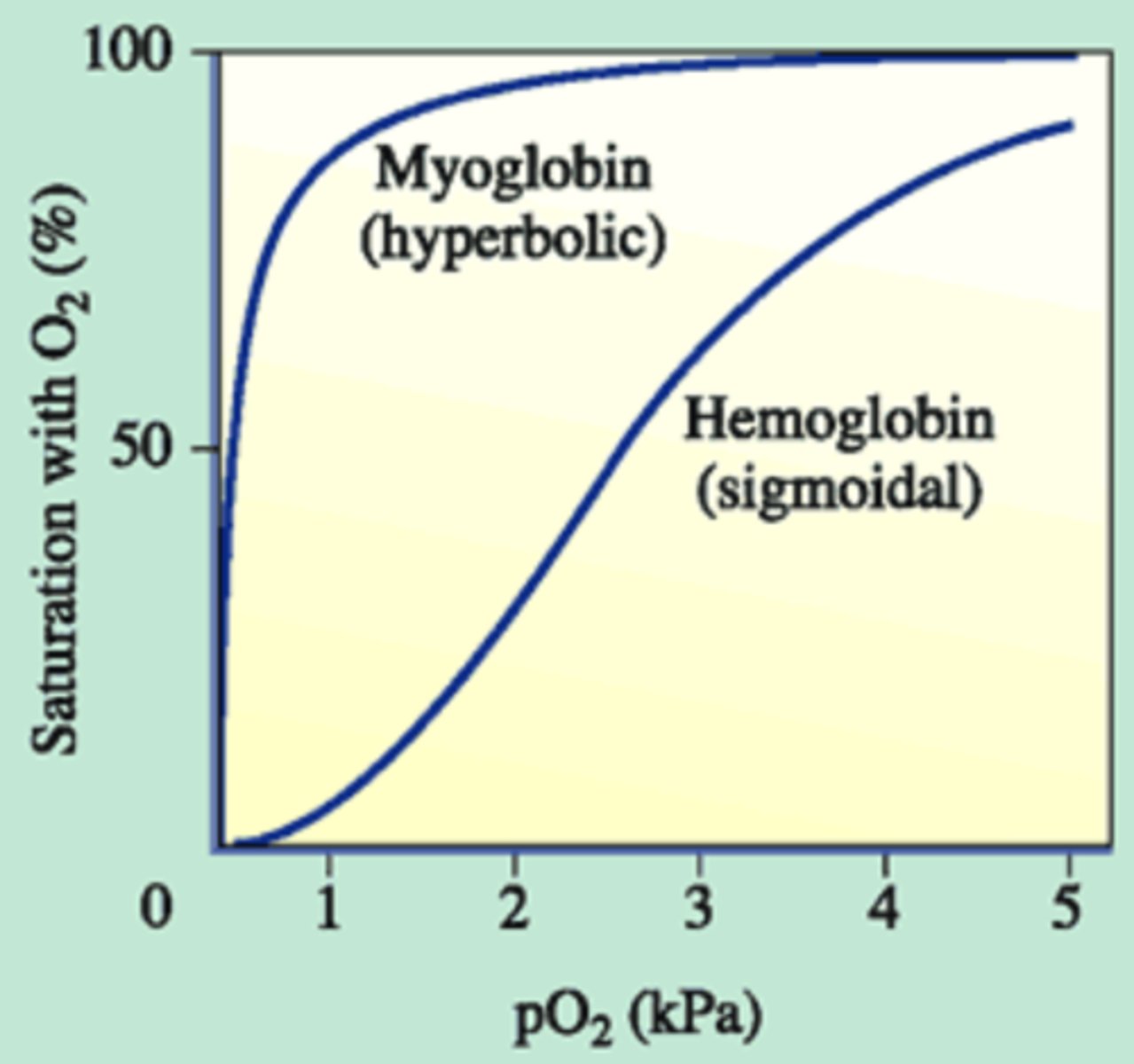
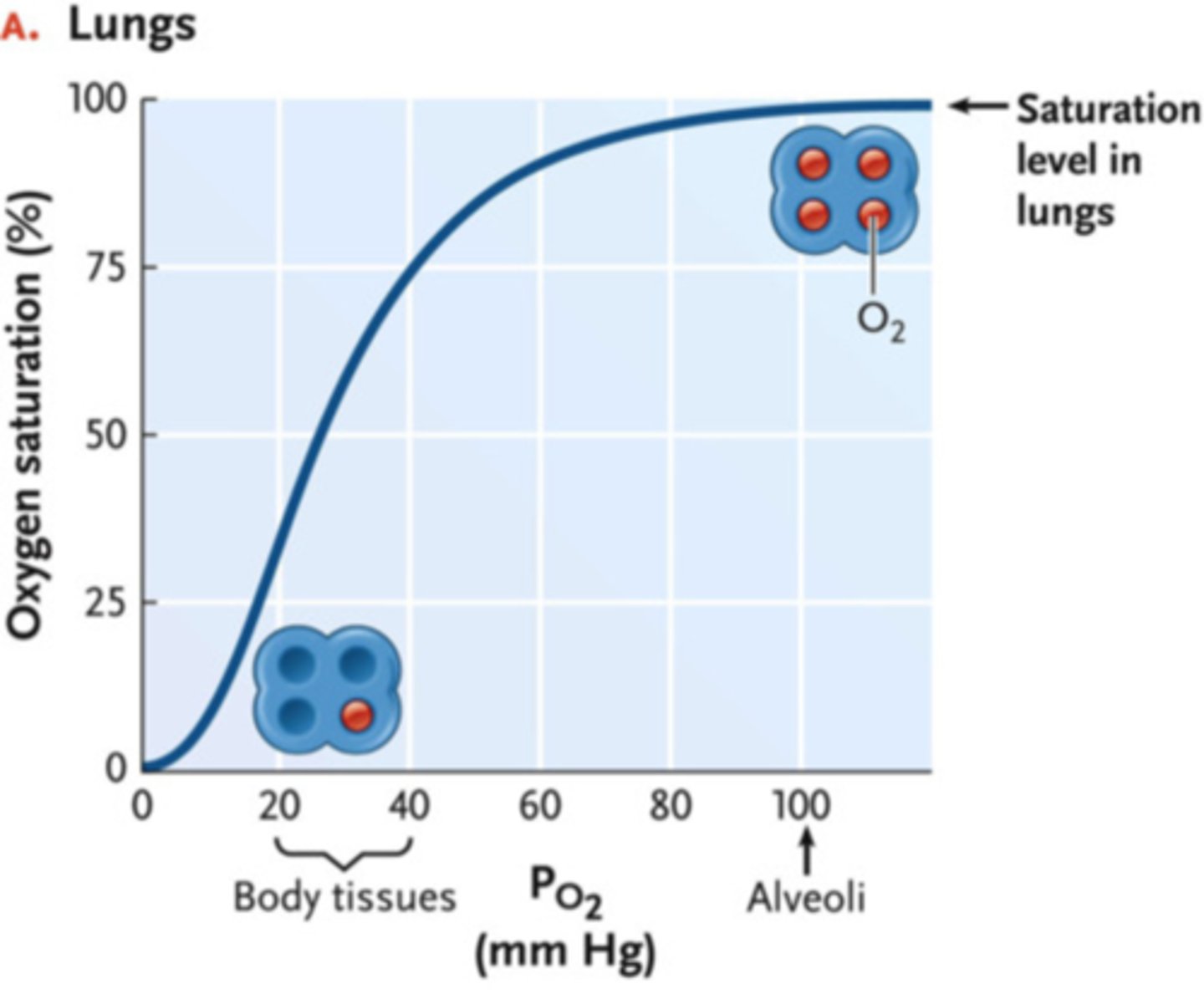
What is cooperativity in hemoglobin?
when one molecule of
O2 binds, other O2
molecules can bind easier
(Note: explains sigmoidal
shape for oxygen
dissociation curve because
O2 binding changes
hemoglobin's affinity for
other O2 molecules)
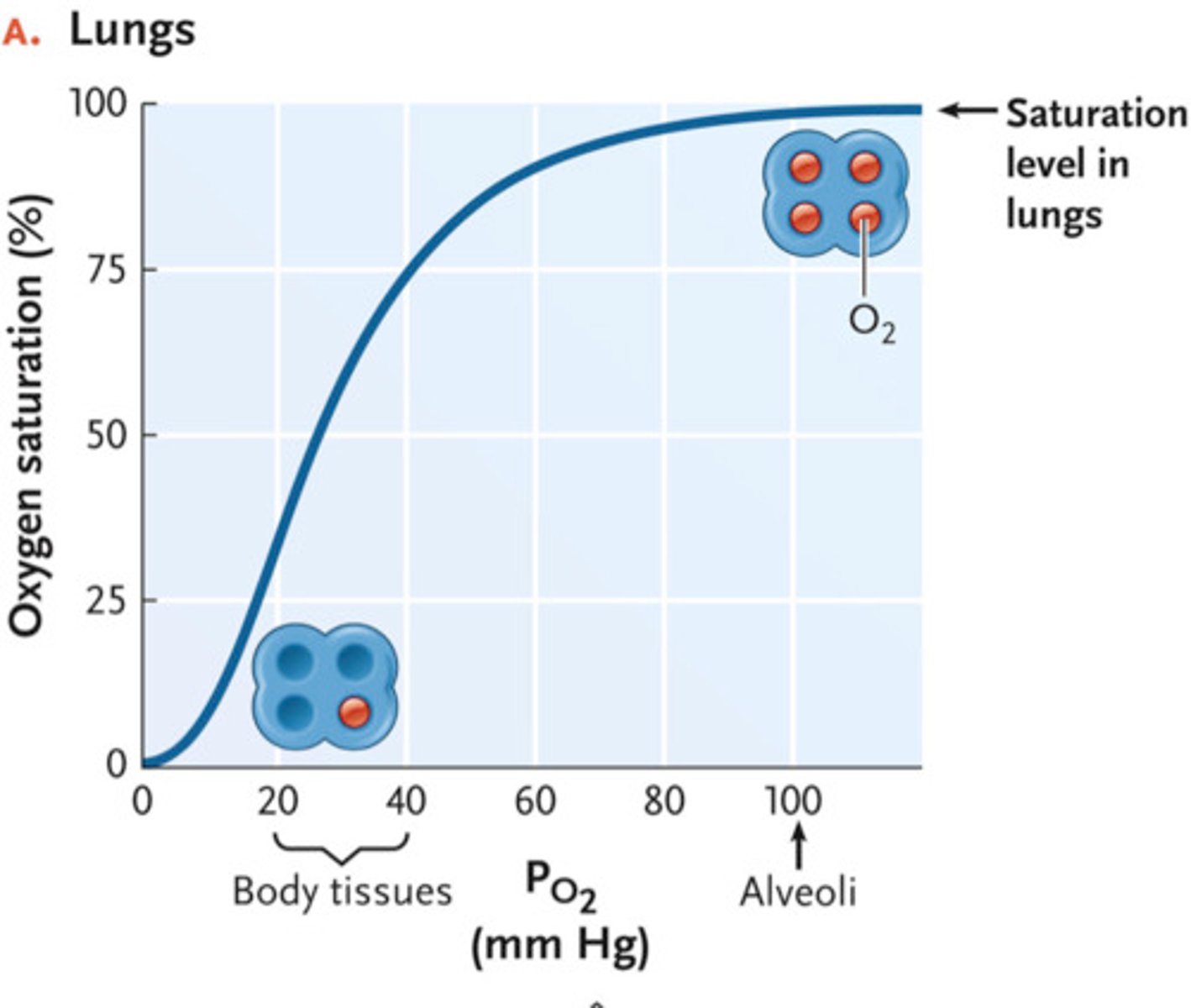
What effect does increased O2 pressure have on cooperativity?
O2 saturation of
hemoglobin increases
(Note: this makes sense!
It is ideal to have
hemoglobin want to hang
onto oxygen in the lungs
and let go of oxygen in the tissues)
According to the Bohr Effect, why do conditions of low pH decrease hemoglobin's affinity for O2?
1. O2 and H+ compete for binding sites on hemoglobin
2. low pH means high CO2 and high H+
3. result is more O2 is unloaded at tissues
What is the chloride shift?
the exchange of Cl- for HCO3- ions in erythrocytes
What is the chloride shift intended for?
balance HCO3-
entering and leaving cells
(Note: both Cl- and
HCO3- carry the same
charge (-1), so they are
transported oppositely
in direct proportion)
What is the part of the brain that primarily controls breathing?
medulla oblongata
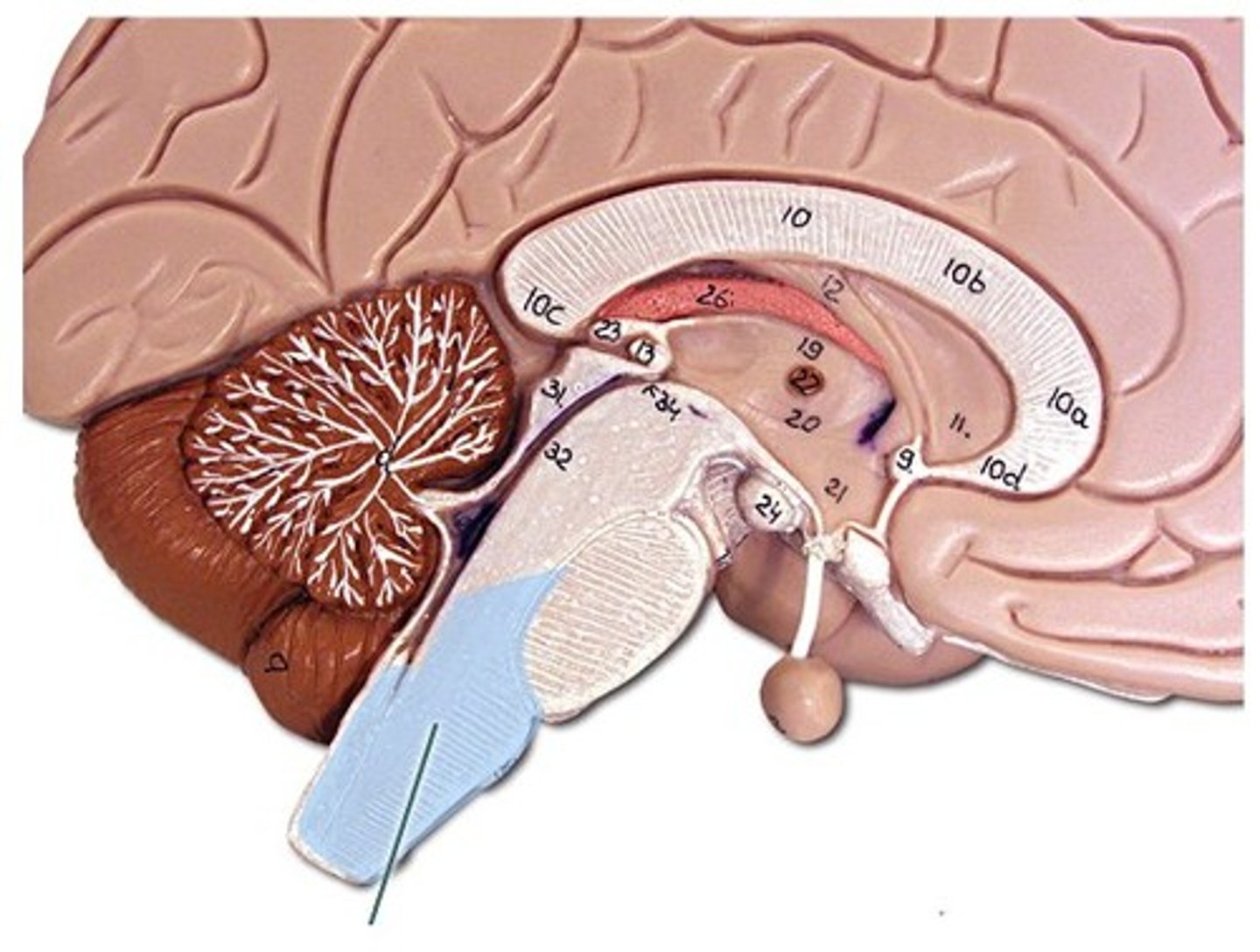
What does the medulla oblongata do when the partial pressure of CO2 increases?
increases breathing
When the medulla stimulates a breath, what happens to the diaphragm?
contracts
What nerve innervates the diaphragm primarily?
phrenic nerve
What structure contains central chemoreceptors?
medulla oblongata
What do central chemoreceptors detect?
indirectly monitor [H+] in the cerebrospinal fluid
What structure contains peripheral chemoreceptors?
heart
(specifically, carotid arteries and aorta)
What do peripheral chemoreceptors detect?
monitor the atrial concentrations of CO2, O2, and pH via [H+]
What type of cell is found in the trachea and upper respiratory system?
ciliated pseudostratified
columnar epithelial cells
(Note: tall = pack close
together = protect from
outside environment =
goblet cells are often
present to produce mucus)
What disease is marked by the destruction of alveoli?
emphysema
(Note: often caused by smoking)
What effect can smoking cause in ciliated pseudostratified columnar cells in the respiratory tract?
paralyze cilia
(Note: allows toxins to stay in lungs)
What effect can smoking cause in goblet cells?
increased mucous production
(Note: this, in tandem with damaged cilia results in a constant, yet unproductive cough)
What diseases can the effects of smoking lead to?
bronchitis, emphysema, and lung cancer
What condition does respiratory acidosis result from?
inadequate ventilation
(Note: don't blow off enough CO2, increased CO2-> increased H+ -> lower pH)
What does the body do to compensate for respiratory acidosis?
increase breathing rate
(Note: attempt to clear more CO2)
What condition does respiratory alkalosis result from?
breathing too rapidly
(Note: losing too much CO2 -> HCO3- and H+ combine to make CO2 -> replenish CO2 but lose H+, so increased pH)
how does the body compensate for respiratory alkalosis?
decrease breathing rate
(Note: clear less CO2)
What kind of O2 dissociation curve does myoglobin possess?
hyperbolic
(steep!)
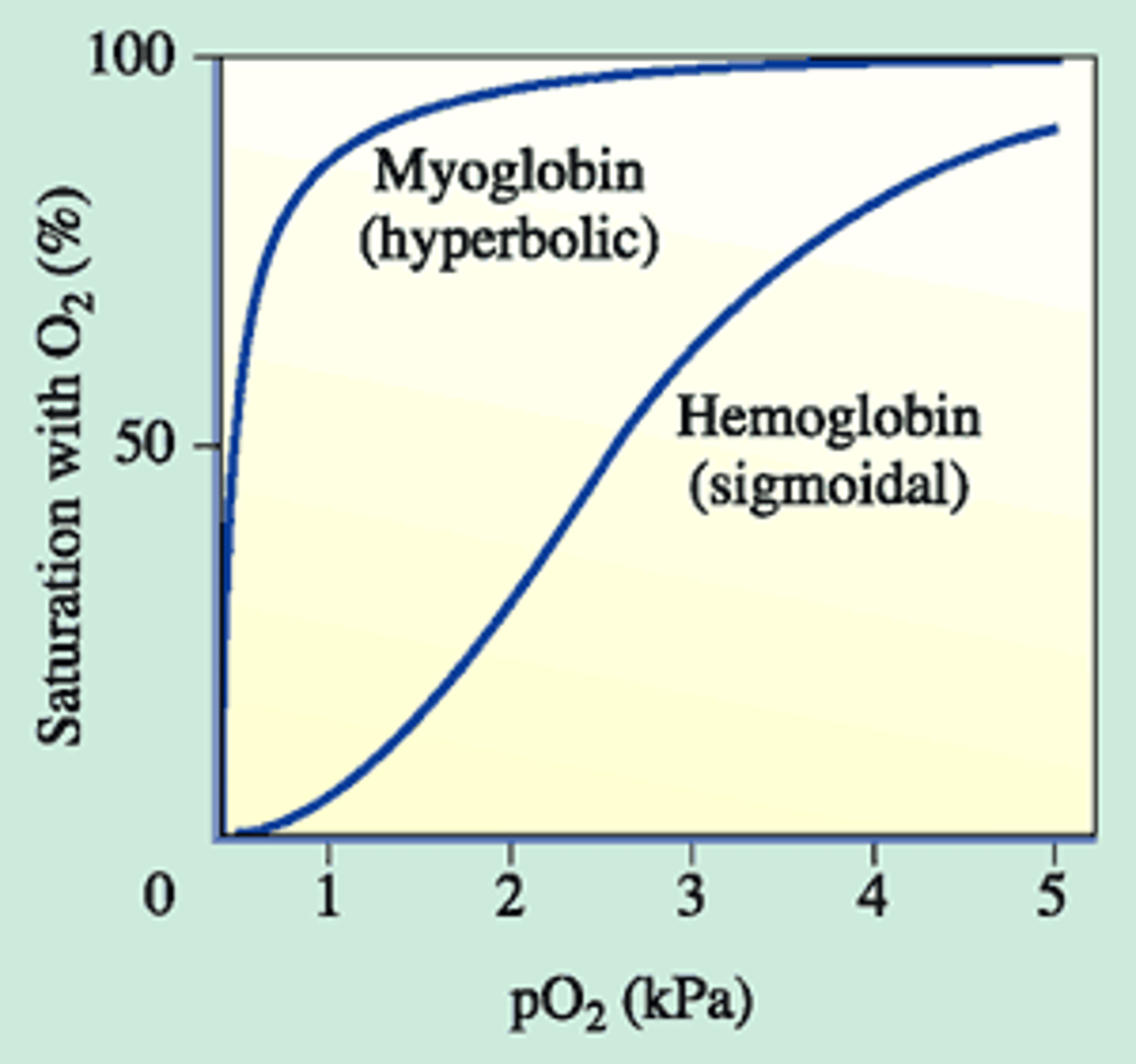
What is the reason for myoglobin's hyperbolic dissociation curve?
Only one binding site!
No cooperativity!
(Note: useful in
emergency situations -
when ppO2 gets extremely low)