A&P test 3
1/240
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
241 Terms
What is the major function of the respiratory system?
Respiration
Supply body’s tissues with oxygen
Remove CO2 from body
What are the 3 secondary functions of the respiratory system?
Allows for speech (nasal cavity serves as a resonance chamber for sound)
Sense of smell
Immune system (mucus)
What are the four processes of respiration?
Pulmonary ventilation
External respiration
Internal respiration
Transport
Pulmonary ventilation
Bulk movement of air in and out of lungs
What must occur for pulmonary ventilation to occur?
A change in pressure
External respiration
breathing/gas exchange
the process where O2 diffuses from the lungs into the blood and CO2 diffuses from the blood into the lungs
Transport
the movement of oxygen and carbon dioxide within the body, primarily through the bloodstream, to facilitate gas exchange between the lungs and tissue
Internal respiration
the exchange of gases (oxygen and carbon dioxide) between the blood and the body's tissues
Conducting Zone vs Respiratory Zone
Conducting zone: pipes that supply air; NO gas exchange
Respiratory zone: location where gas exchange occurs
4 functions of the nasal cavity
Moistens air
Adds H2O to the air by the epithelial cells secreting H2O
Smell (olfactory receptors)
Resonance chamber for sound
Mucus, nose hairs, and cilia on cells will help filter and clear air that will help destroy viruses
What is the pharynx?
Throat (muscular tube) that serves as a passageway for air and food
Where is the larynx located?
At the top of the trachea
3 functions of the larynx
Prevents food from going down trachea
Epiglottis
Responsible for voice production
Vocal chords made of bands of cartilage
Aids in breathing
Glottis function
Traps air in lungs
Example: lifting up something heavy and you intake air and hold it and clench your core — this helps during lifting something
Laryngitis
Swelling of larynx
can be caused by excessive use of vocal chords or from infection
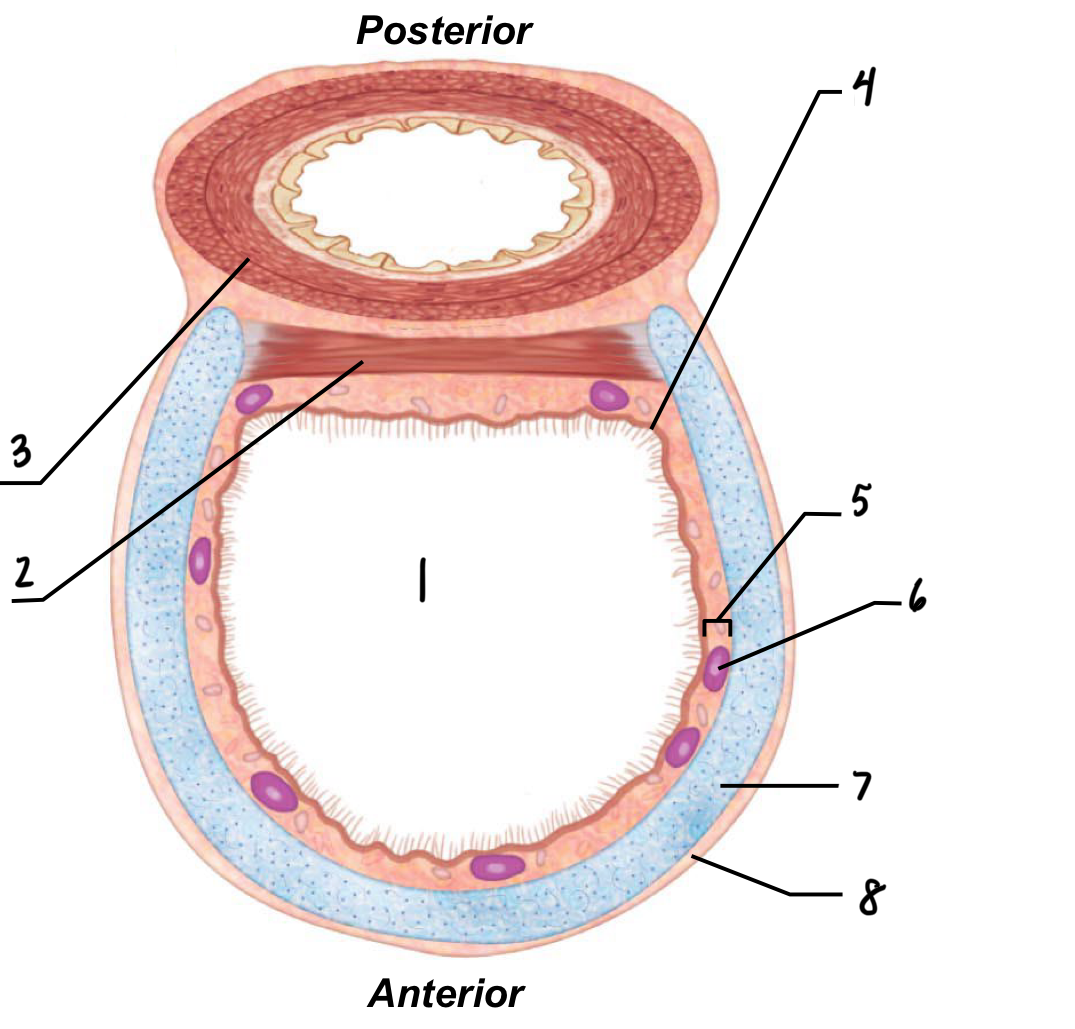
1
Lumen of trachea
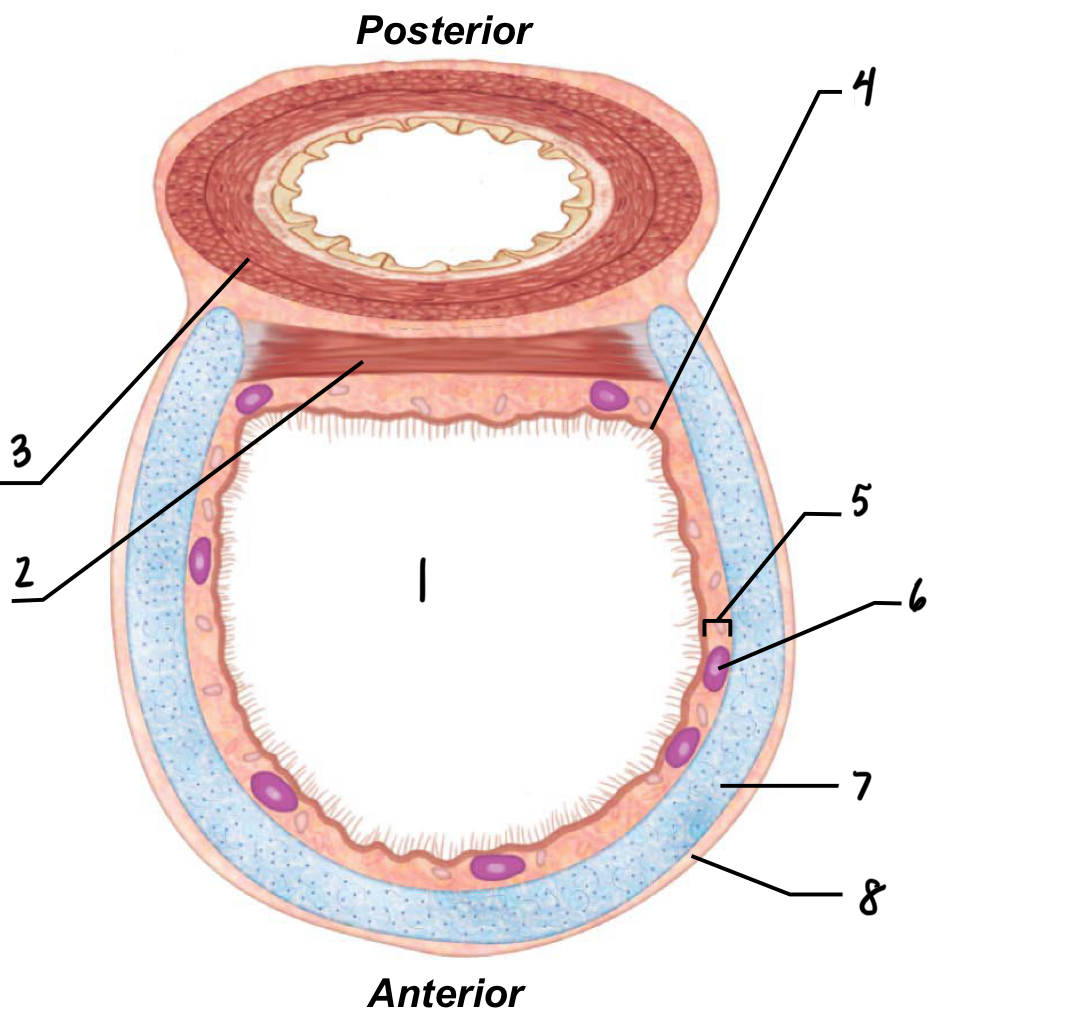
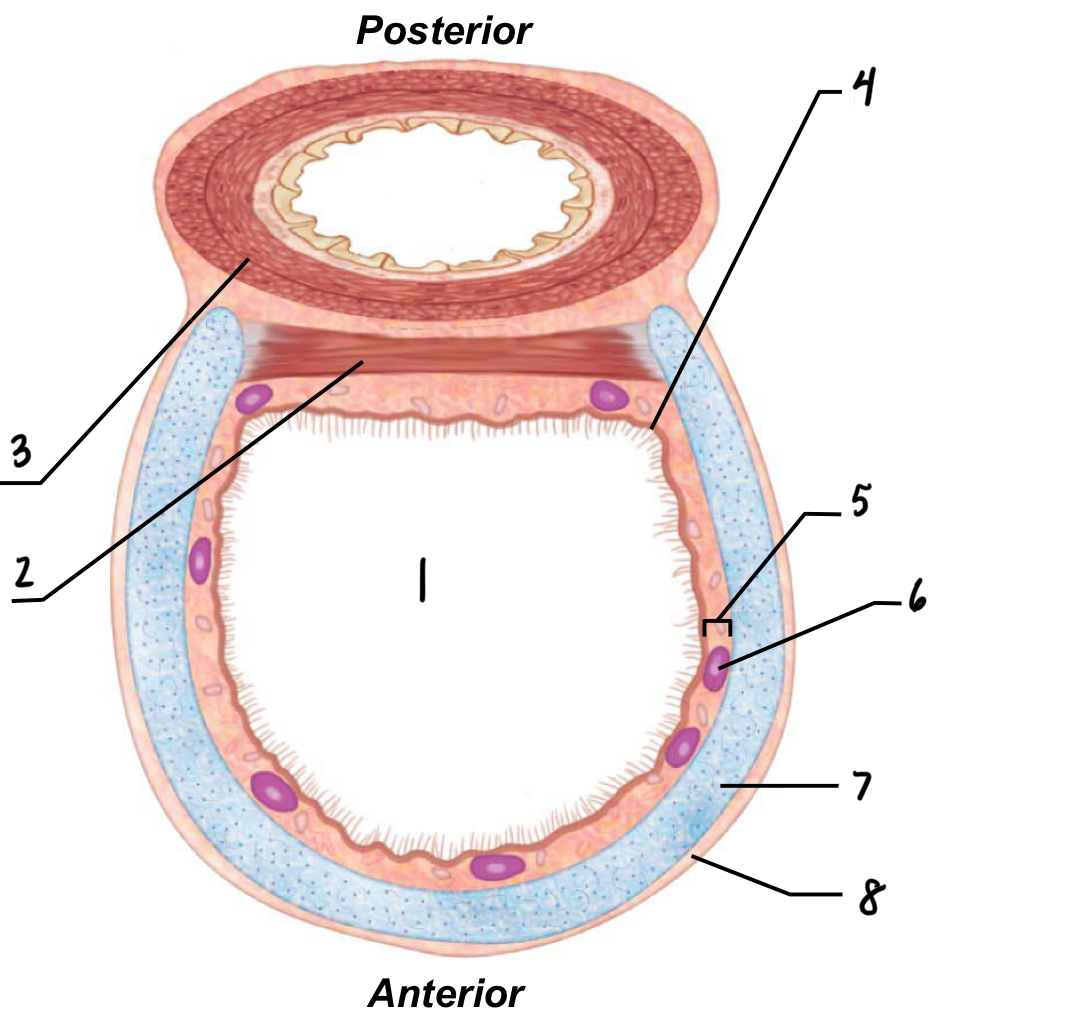
2
Trachealis muscle
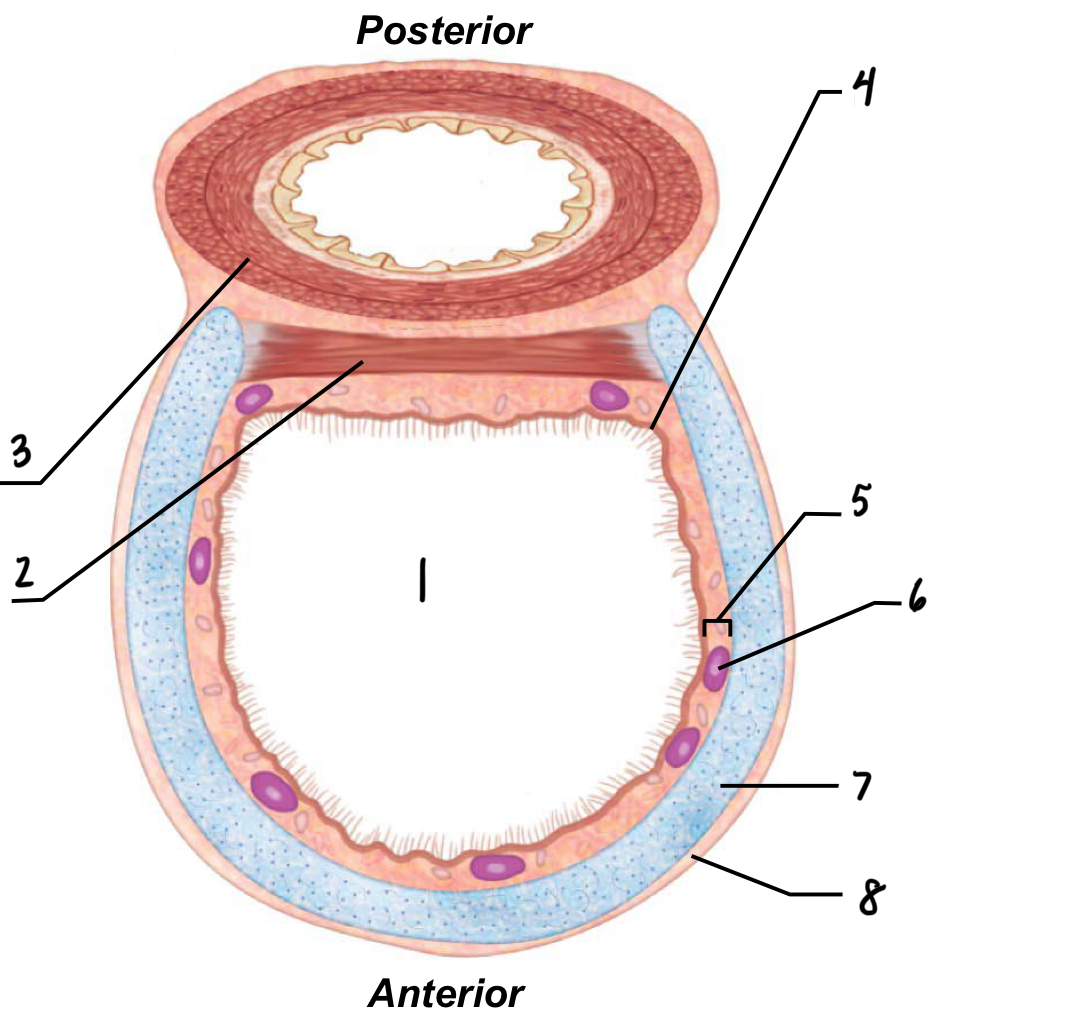
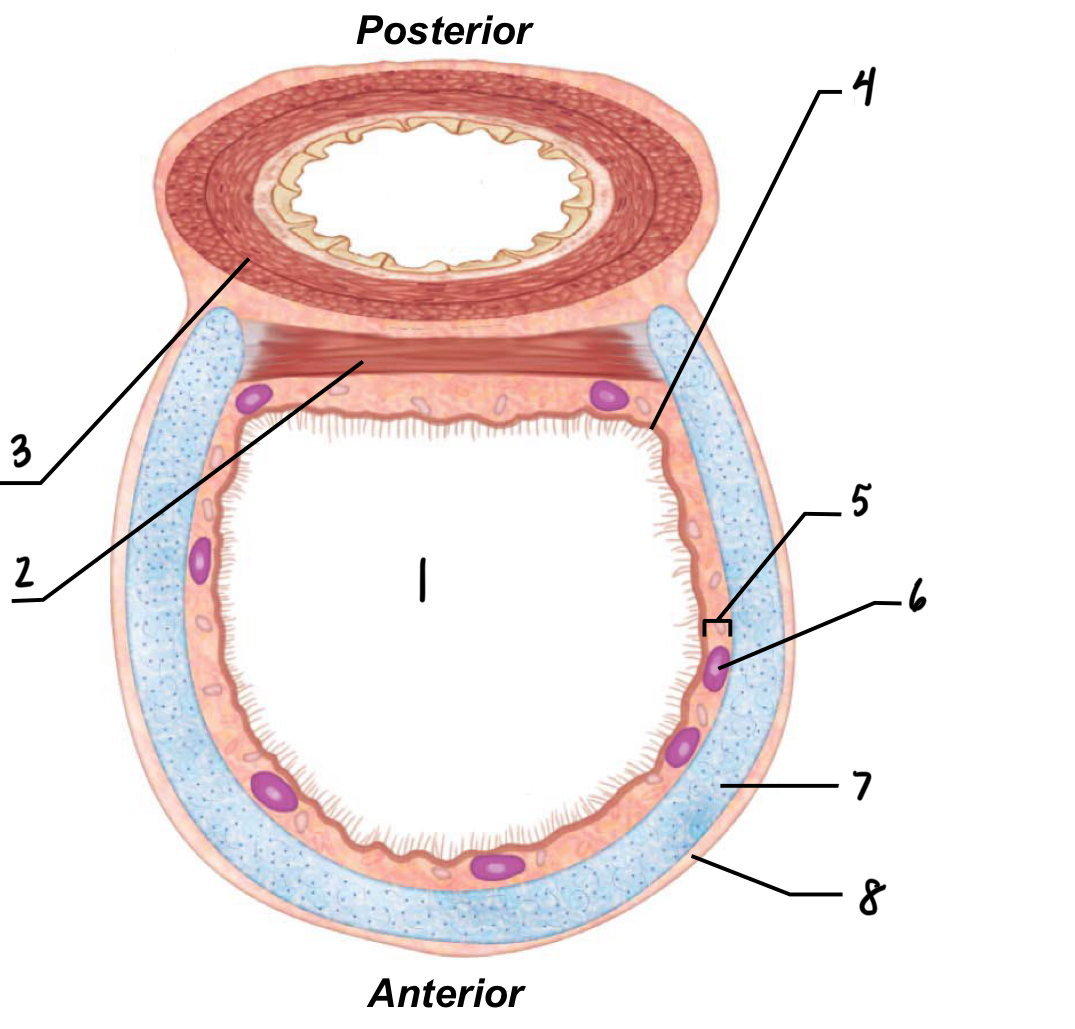
3
Espophagus
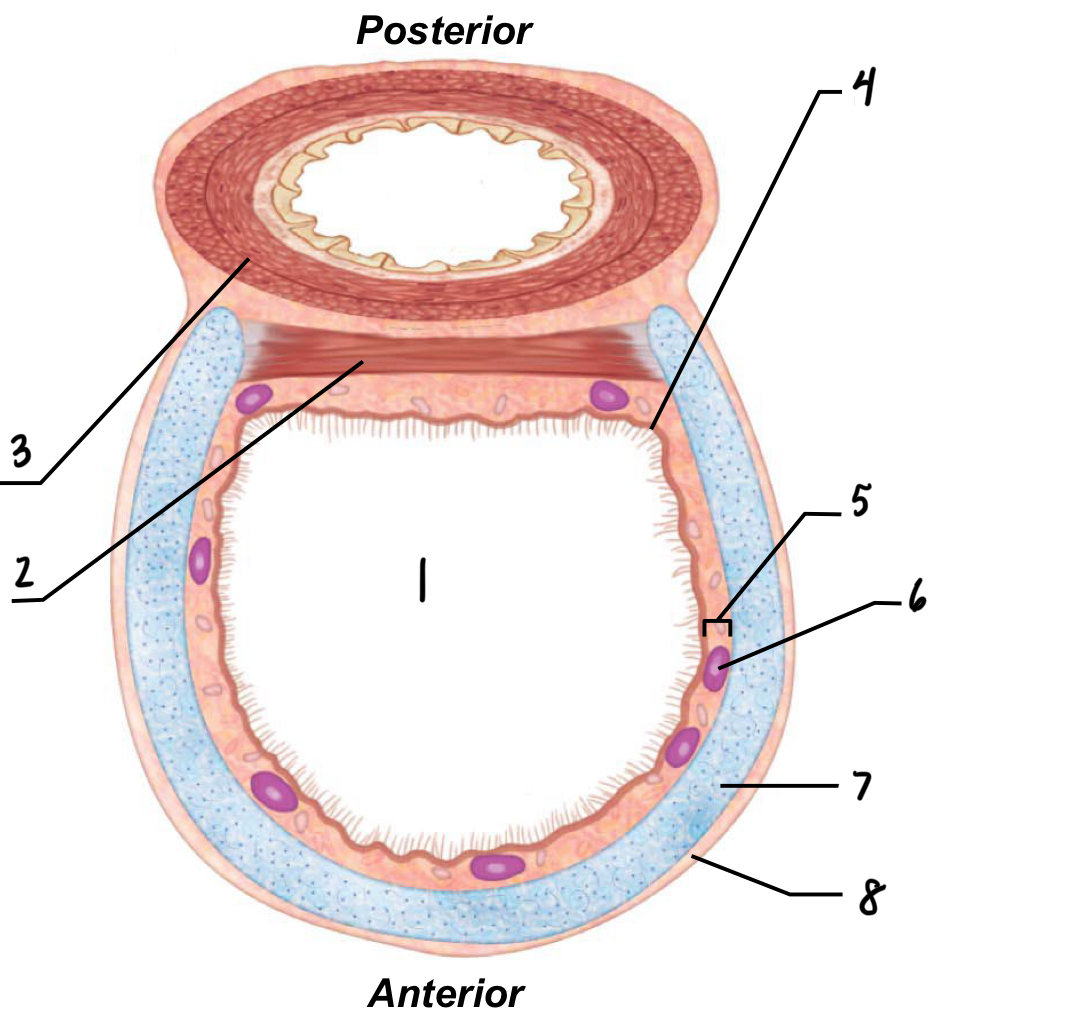
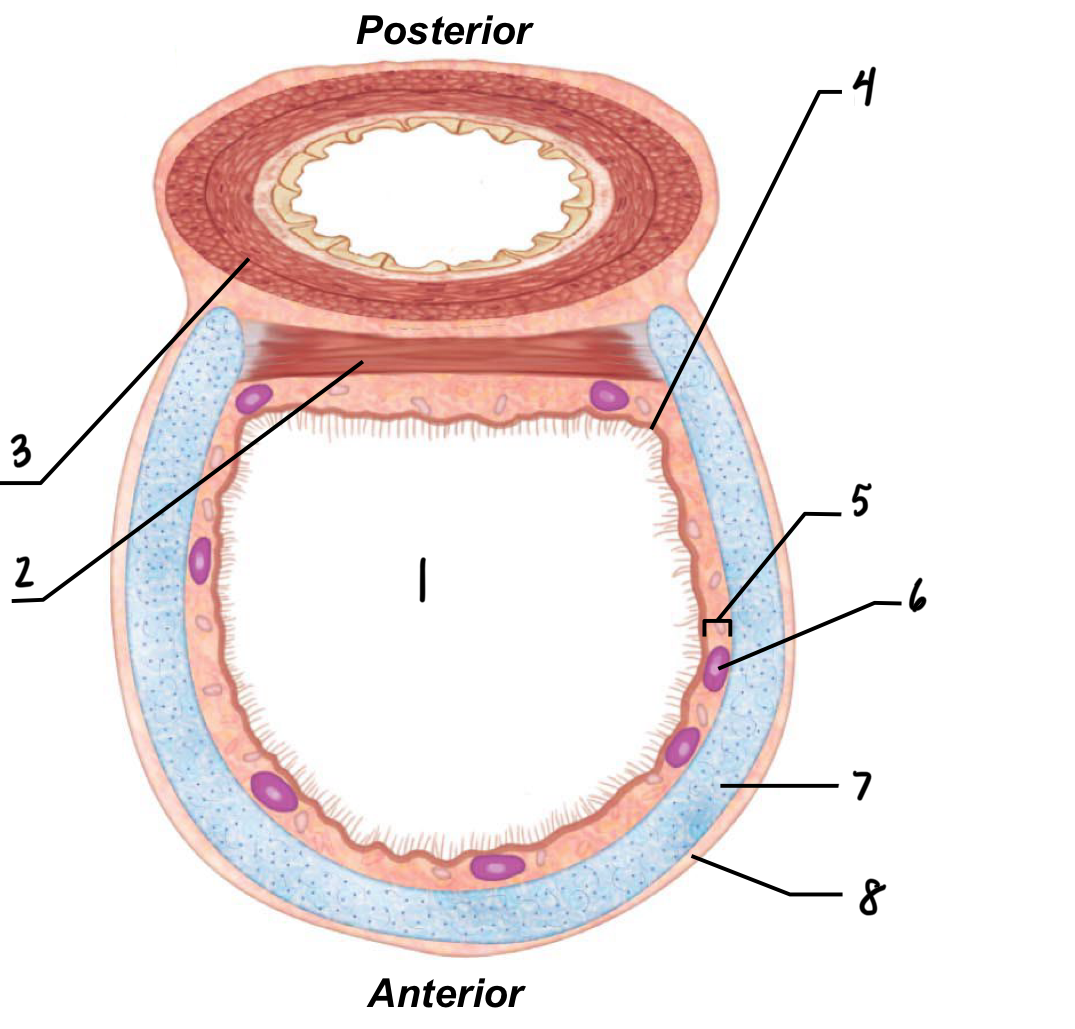
4
Mucosa
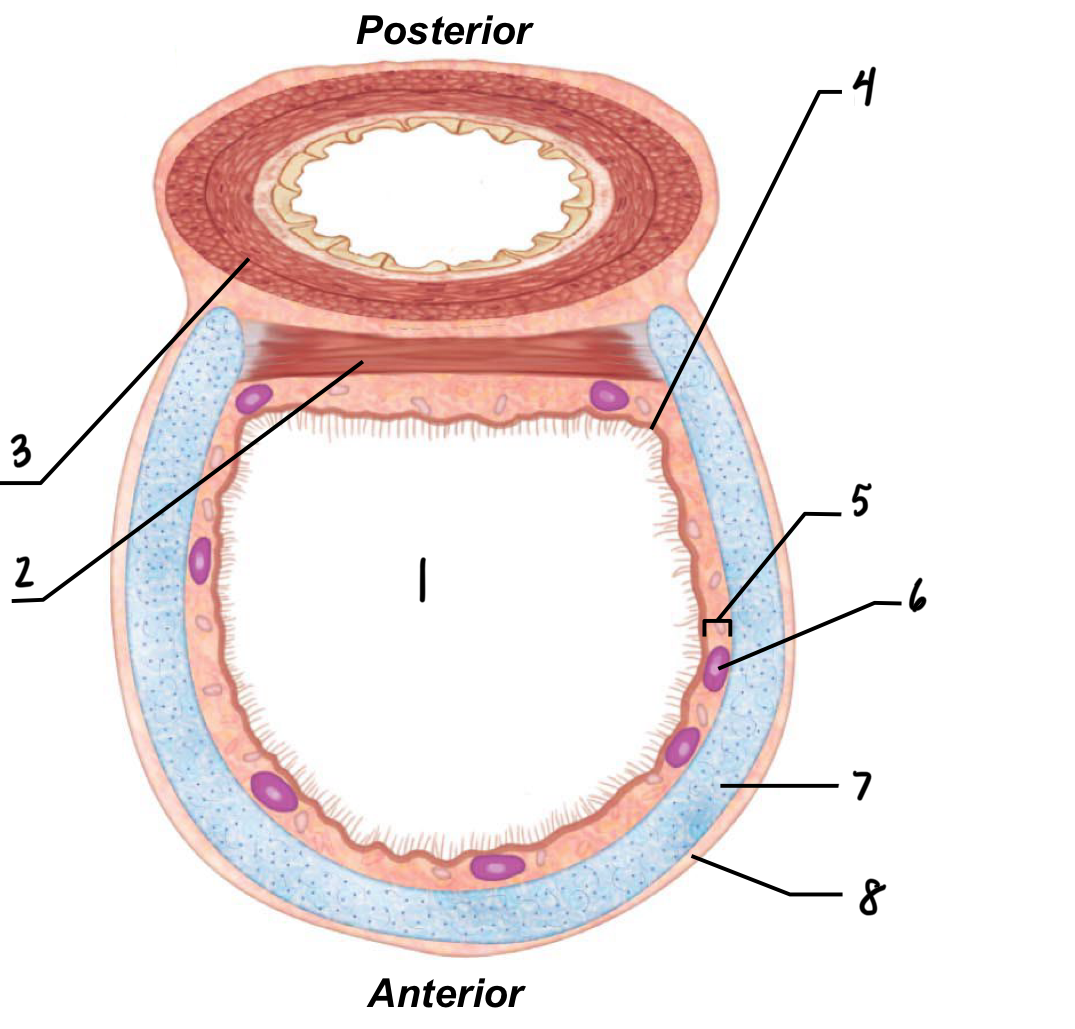
What is the mucosal layer of the trachea?
Ciliated epithelial cells that use a “sweeping” motion to move gunk out of our lungs
long-term smoking causes peristalsis of the ciliated mucosal cells
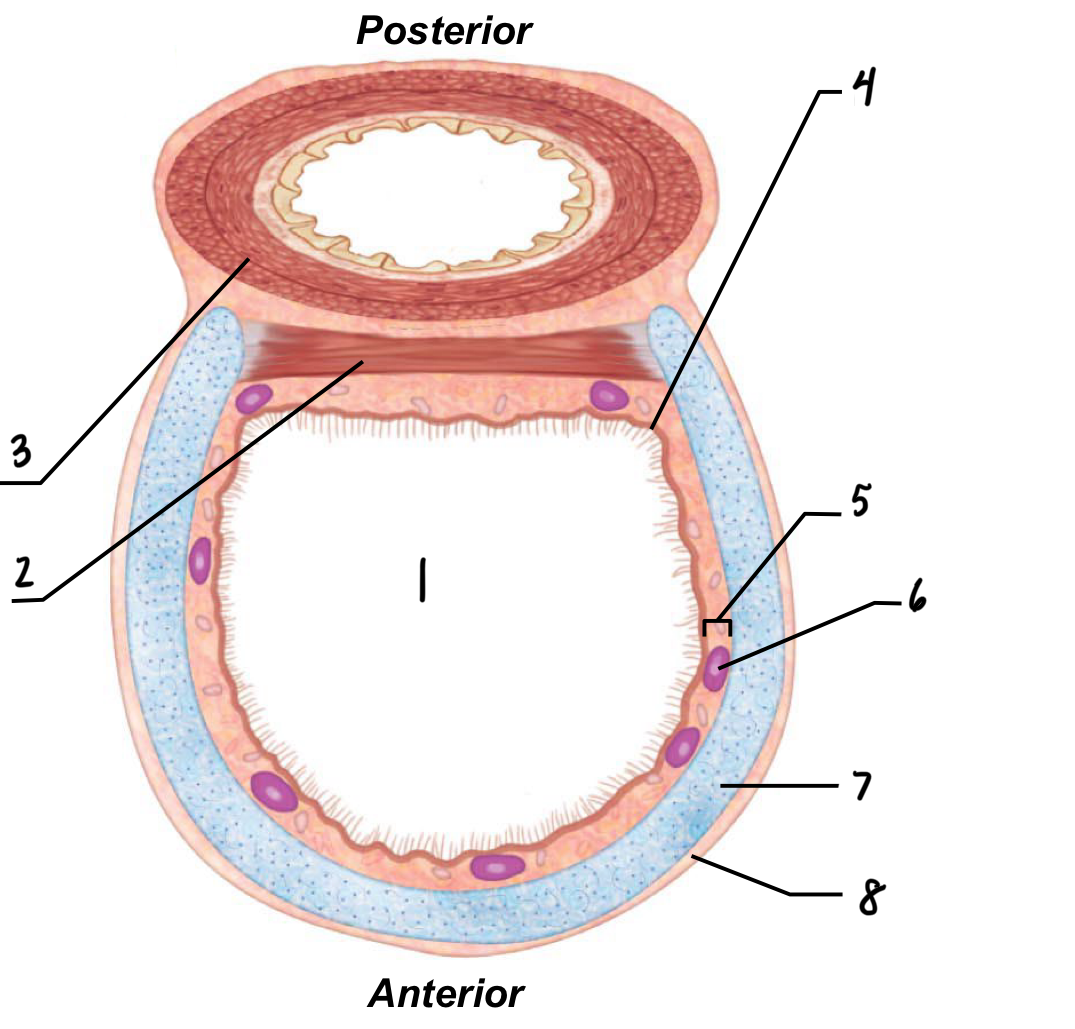
5
Submucosa
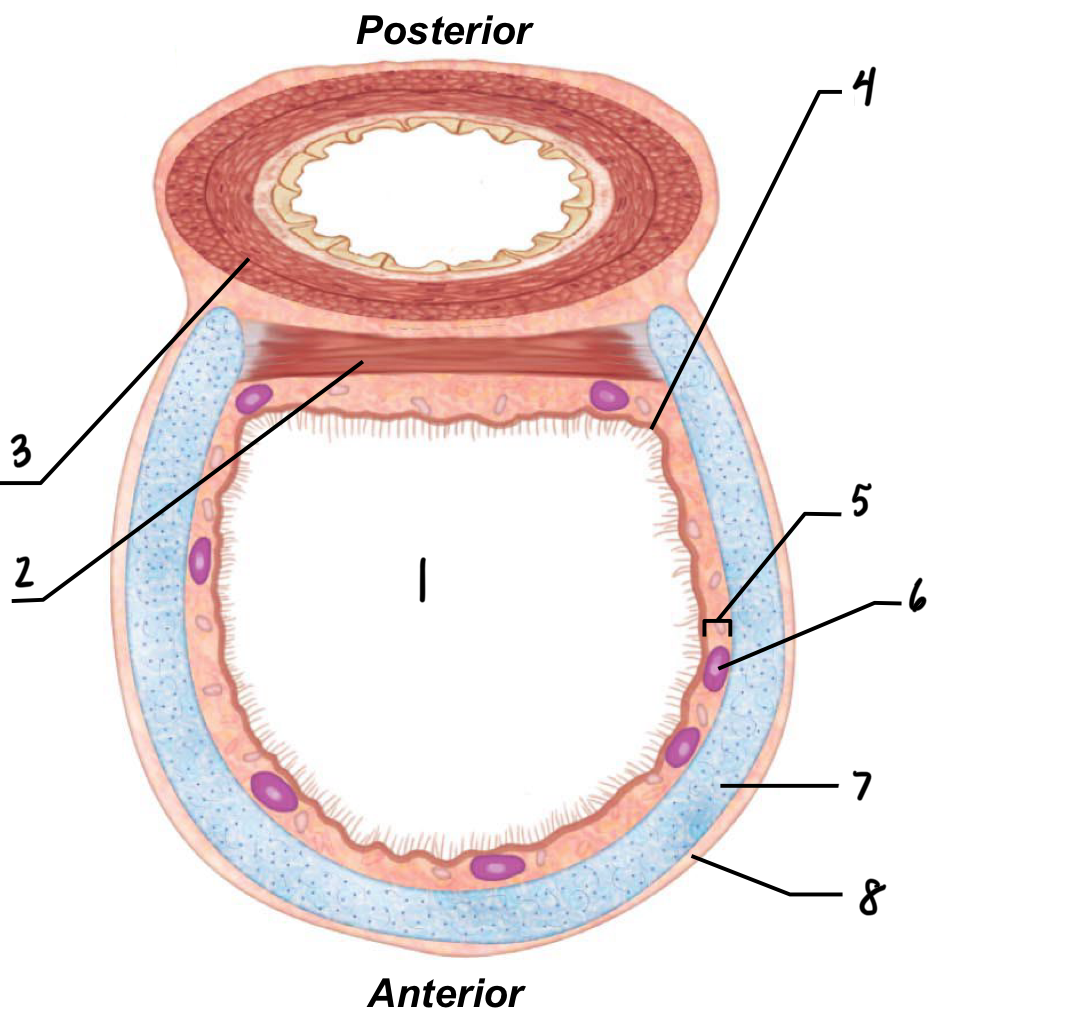
What is the submucosal layer of the trachea?
Contains glands that secrete mucus that aid in protection
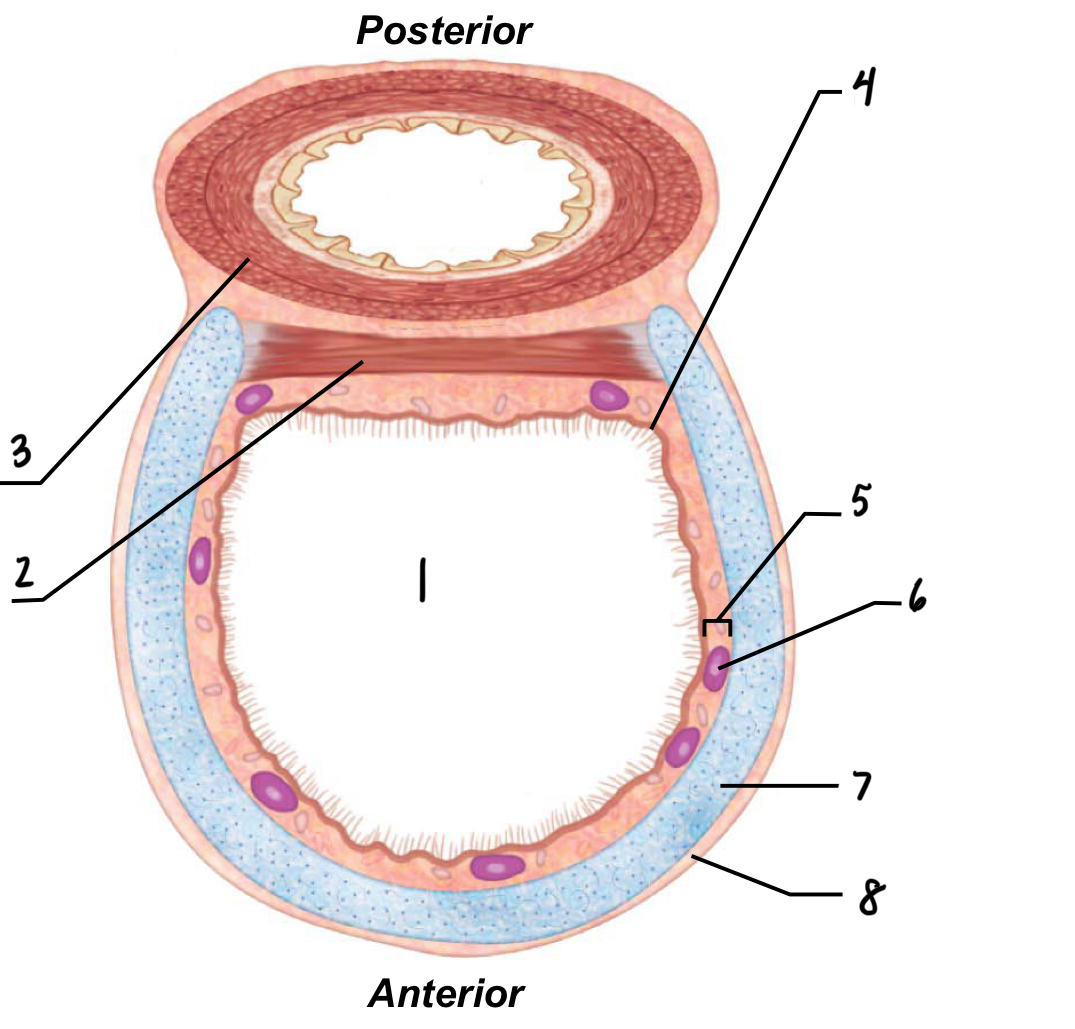
6
Serous mucous gland in submucosa
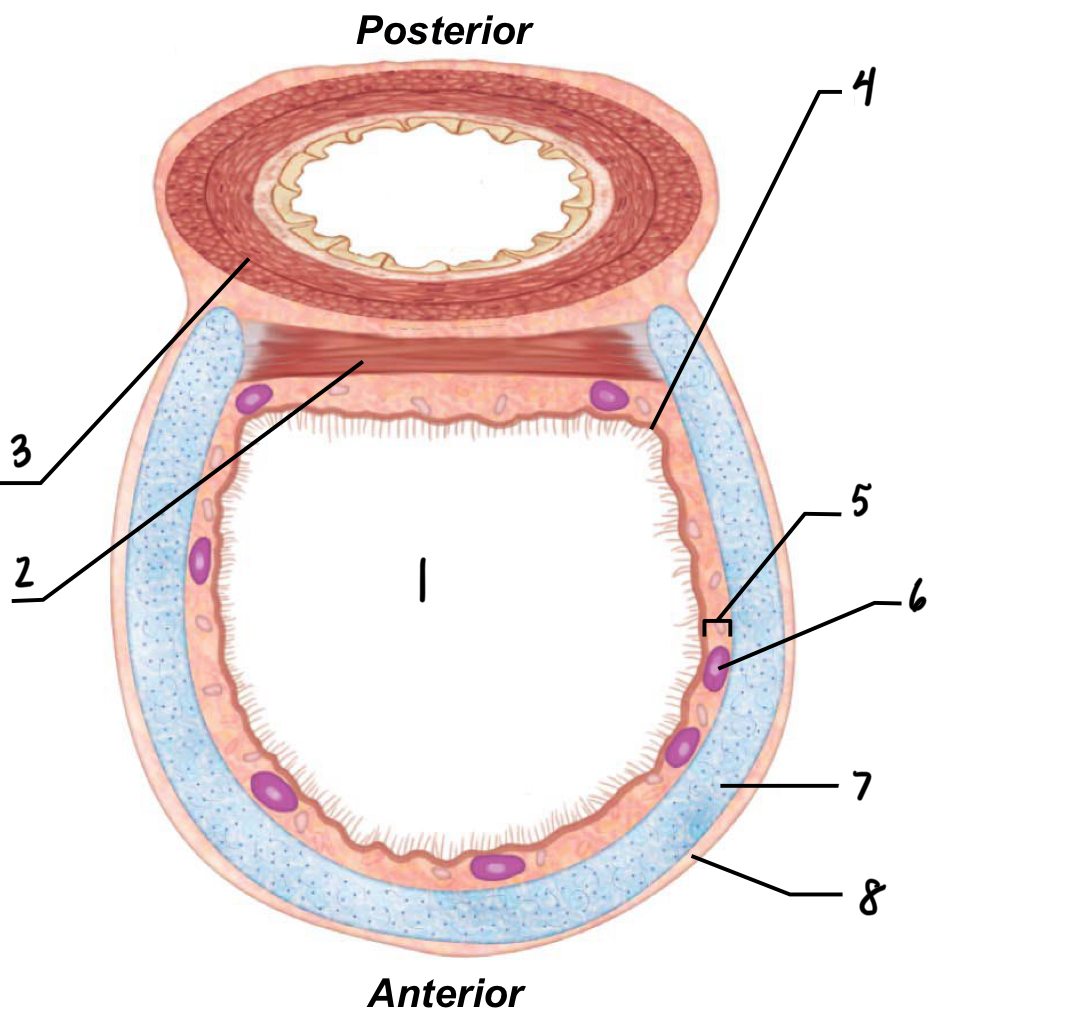
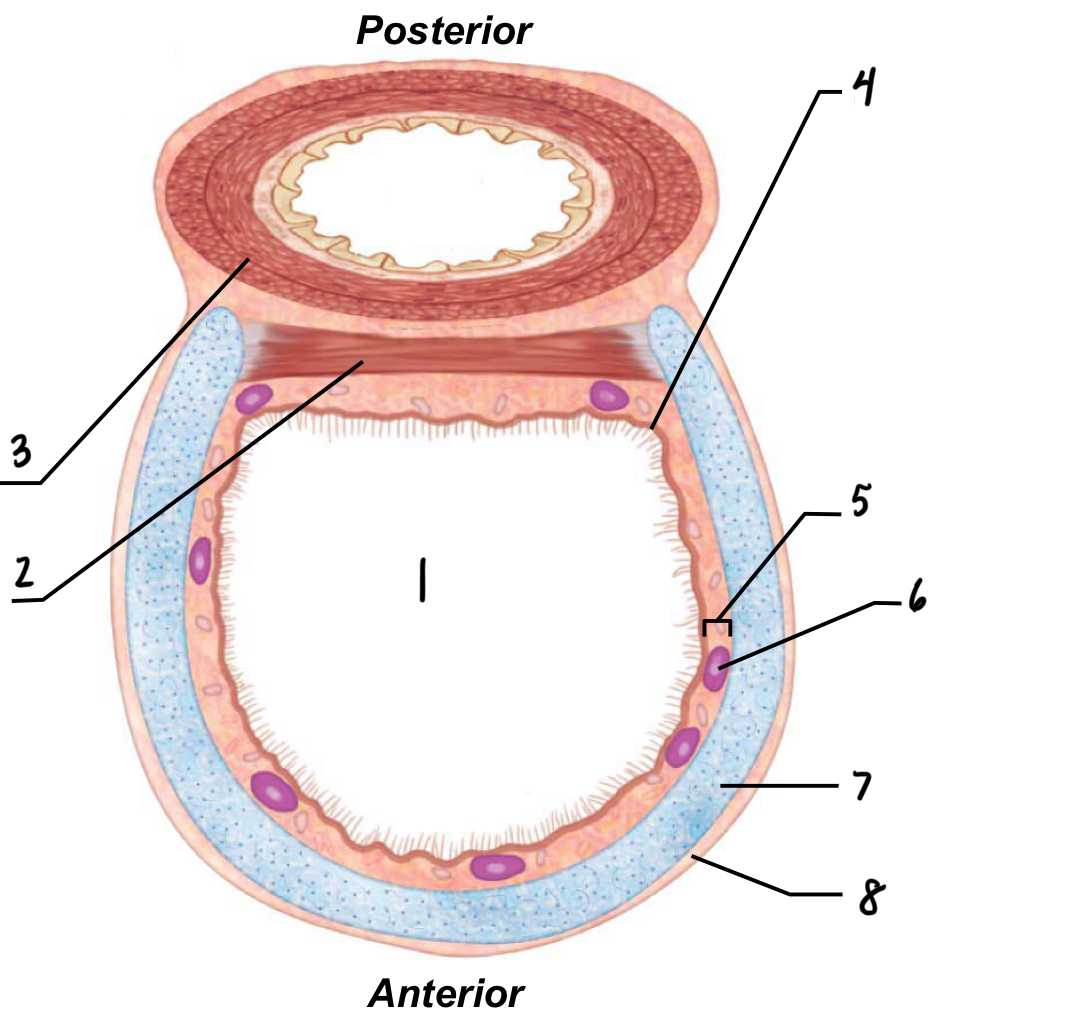
7
Hyaline cartilage
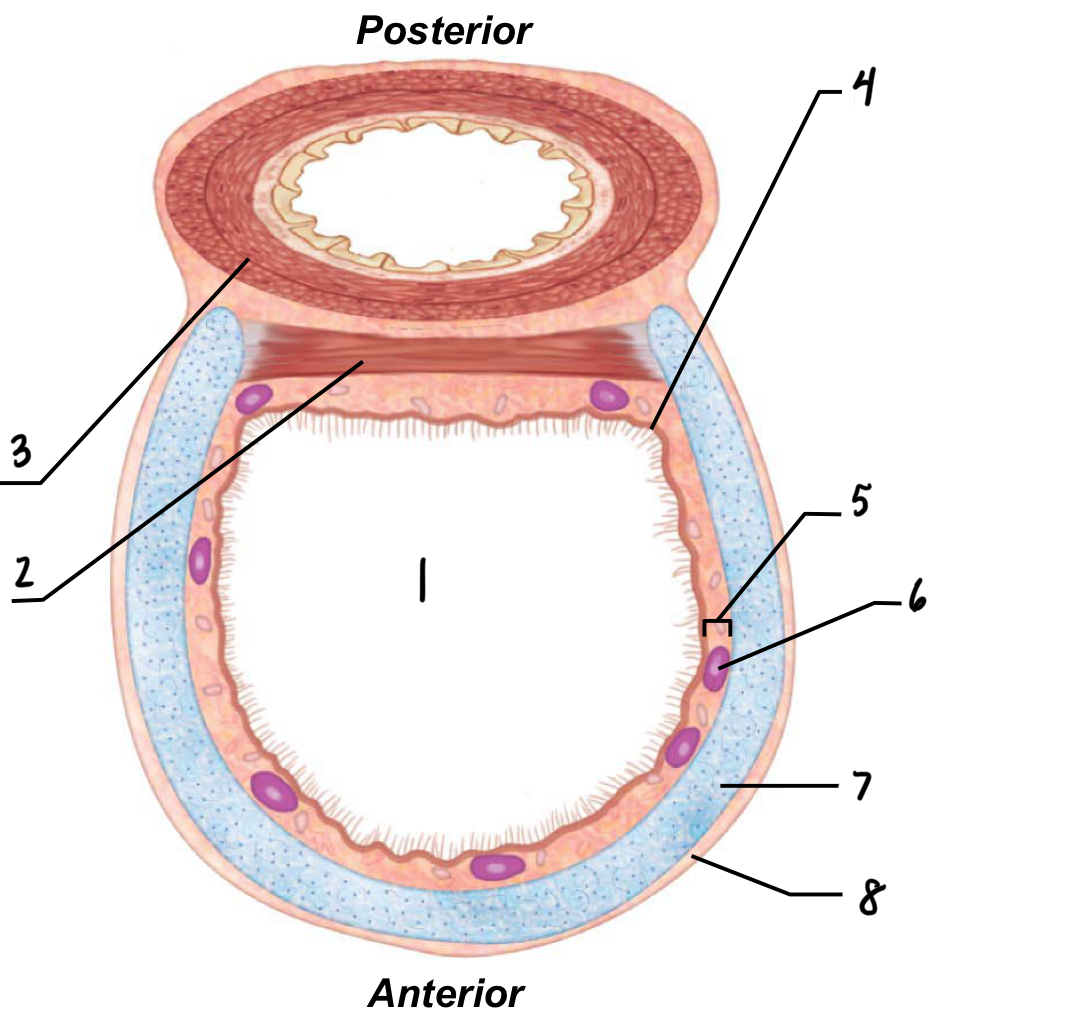
What is hyaline cartilage in the trachea?
Rings of cartilage that covers and protects the front of the trachea
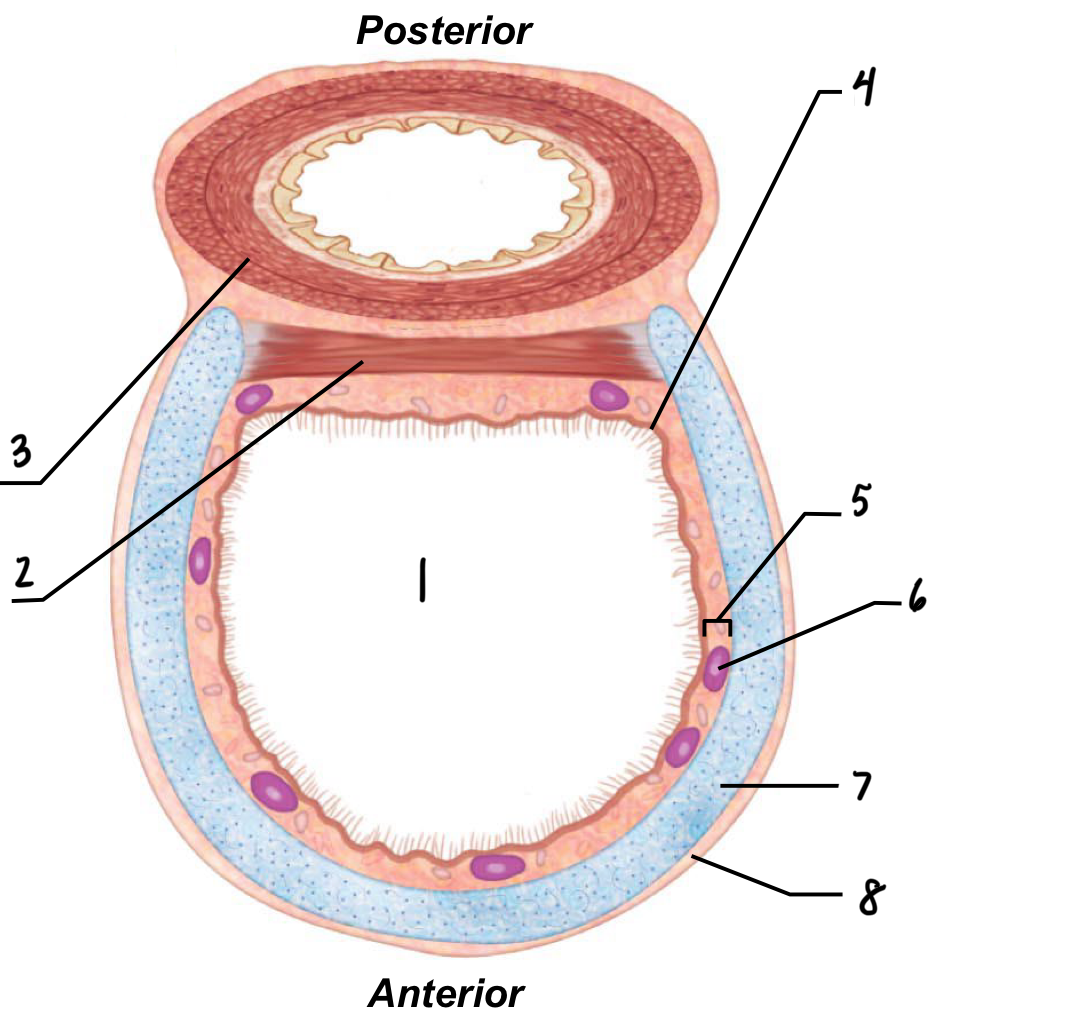
8
Adventitia
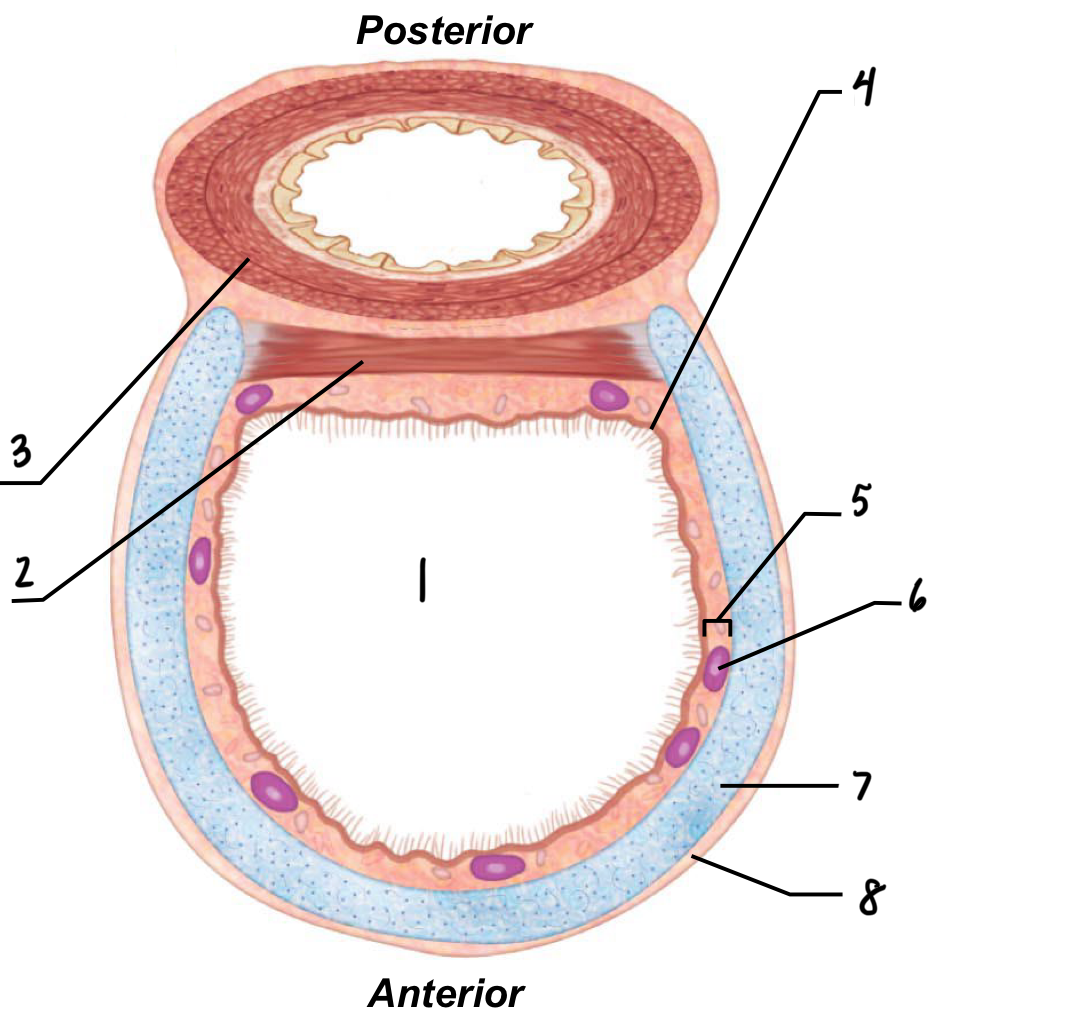
What is the adventitia of the trachea?
Outer layer of connective tissue
What are the 5 parts of the conducting zone?
Larynx
trachea
Bronchi (1, 2, 3, smaller)
Bronchioles
Terminal bronchioles
Deeper into the conducting zone, the inner diameter…
Decreases
Deeper into the conducting zone, the # of ciliated cells… because…
Decreases because in smaller tubes the cilia could block them
Deeper into the conducting zone, the # of goblet cells…because…
Decrease because they secrete mucus, which will cause clogging in the smaller tubes
Deeper into the conducting zone, the amount of cartilage…because…
Decreases because protection isn’t needed that far down
Deeper into the conducting zone, smooth muscle…
Increases — regulates diameter of tube
What are respiratory bronchioles made of?
Alveoli
Why is it important to have many alveoli?
More alveoli creates more surface area, allowing for increased gas exchange
Increased SA = more capillaries for more gas exchange
What do capillaries on the outside of alveoli allow for?
Allows for O2 and CO2 exchange
What are the three factors that make gas exchange so efficient?
Huge surface area — many alveoli
Vast blood supply — many capillaries
Thin respiratory membrane
Type I cell (pneumocyte I) function
facilitate gas exchange in the lungs by forming the thin air-blood barrier in the alveoli
Type II cell (pneumocyte II) function
Secretes surfactant
Function of surfactant
helps the lungs stay inflated by reducing surface tension
secretes a protein/lipid mix to prevent alveoli collapsing in on each other
Surface tension
Attraction of liquid molecules to one another at a gas-liquid interface
produces surface tension
Water attracts water by hydrogen bonds
Results in the alveoli pulling together
T/F: The respiratory zone has abundant amounts of mucus
producing cells
False
As you move deeper into the conducting zone the amount of smooth muscle
a. Increases
b. Decreases
c. Does not change
a - increases
The type of alveolar cell that prevents the formation of hydrogen bonding of water molecules on the alveolar surface are
a. macrophages
b. Type 1 pneumocytes
c. Type 2 pneumocytes
c. Type 2 pneumocytes
What are the membrane layers of the lungs (external to internal)?
Parietal membrane (connected to the chest wall)
Pleural cavity (between parietal and visceral membranes; interpleural pressure)
Visceral membrane (contact with the external surface of the lungs)
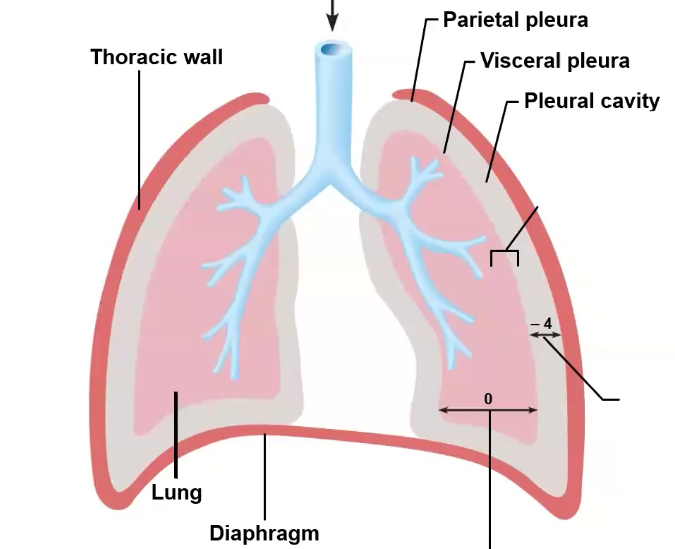
What are the 3 types of pressure in the lungs?
Intrapleural pressure
Intrapulmonary/intra-alveolar pressure
Trans pulmonary pressure
Interpleural pressure
Pressure in the pleural cavity of the lungs
Always negative pressure
Pressure that prevents lungs from collapsing in or pushing out
Fluctuates with breathing
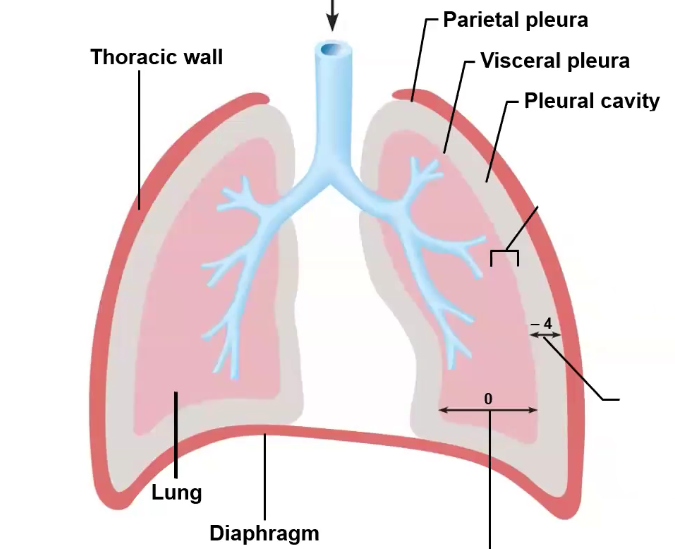
Intrapulmonary (intra-alveolar) pressure (IAP)
The pressure of air within the alveoli of the lungs
Right after inhalation, but before exhalation
Fluctuate with breathing — contracting diaphragm
Why does contracting the diaphragm cause a change in intra-alveolar pressure?
Diaphragm contracting makes the size of the lungs bigger. If the size of your lungs becomes bigger, pressure is going to decrease (lower pressure in lungs than outside of lungs)
When your relax your diaphragm and your lungs get smaller, the pressure increases and is higher than outside of lungs
Trans pulmonary pressure
Difference between intra-alveolar pressure and intrapleural pressure
will always be positive because subtracting a negative number (intrapleural pressure is always negative) makes a positive number
The larger your inhalation is, the higher the transpulmonary pressure is
Indication of how much air we have intaken
To pull air into our lungs, we need to ____ IAP because…
To pull air into our lungs, we need to decrease IAP because pressure drives flow
What will IAP always return to?
0 mm Hg (relative to ATM)
equalizes with pressure of atmosphere (Patm)
How is negative intrapleural pressure established?
Anatomy — parietal membrane, visceral membrane, and pleural cavity (fluid filled)
Natural tendencies for…
Chest wall to recoil outward
Lungs to recoil inward
Pneumothorax
Loss of negative intrapleural pressure
usually due to trauma
What are the 2 phases of ventilation?
Inspiration: gases flow into lungs
Expiration: gases exit lungs
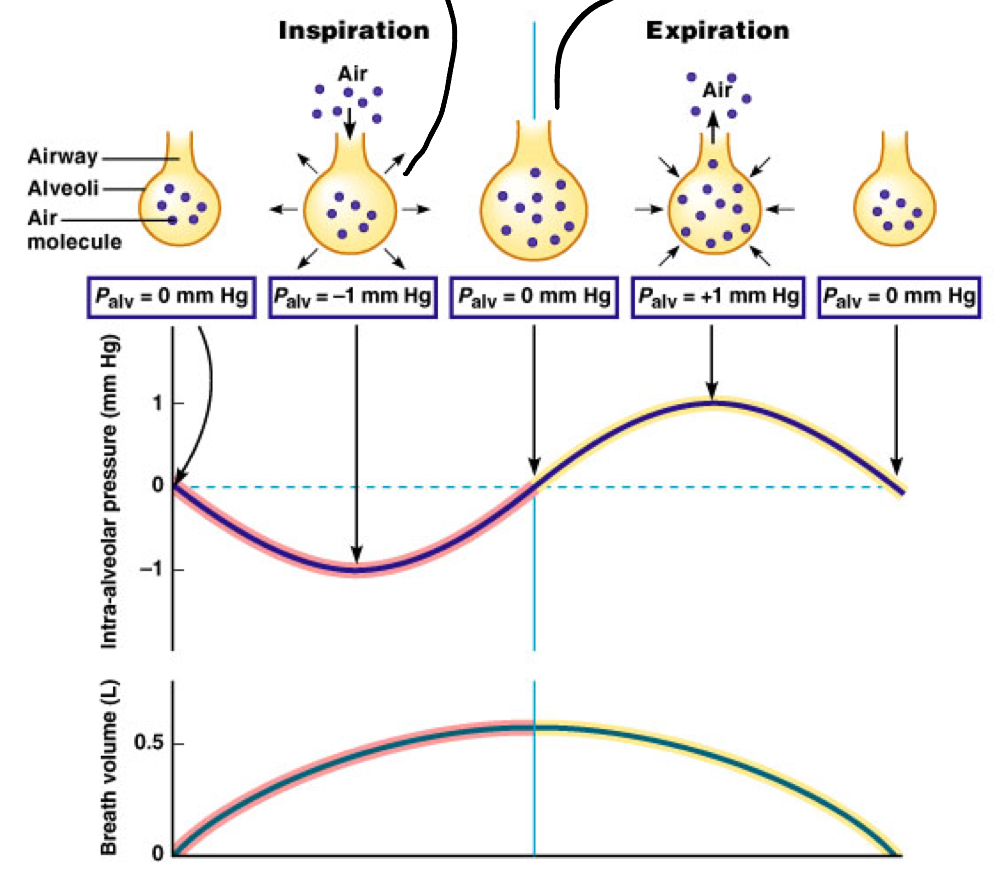
Volume changes lead to _____ changes, which leads to…
Volume changes lead to pressure changes, which leads to gas flows to equalize pressure
Boyles law
Pressure varies inversely of volume
inhalation (more air) = decreased pressure (because larger cavity)
Sequence of events for inspiration (5)
Inspiratory muscles contract (diaphragm descends and rib cage rises)
Thoracic cavity volume increases
Lungs stretch; Intrapulmonary volume increases
Intrapulmonary pressure drops (to -1 mm Hg)
Air flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to Patm)
Sequence of events for expiration (5)
Inspiratory muscles relax (diaphragm rises and rib cage descends due to recoil of costal cartilages)
Thoracic cavity volume decreases
Elastic lungs recoil passively; Intrapulmonary volume decreases
Intrapulmonary pressure rises (to +1 mm Hg)
Air flows out of lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to Patm)
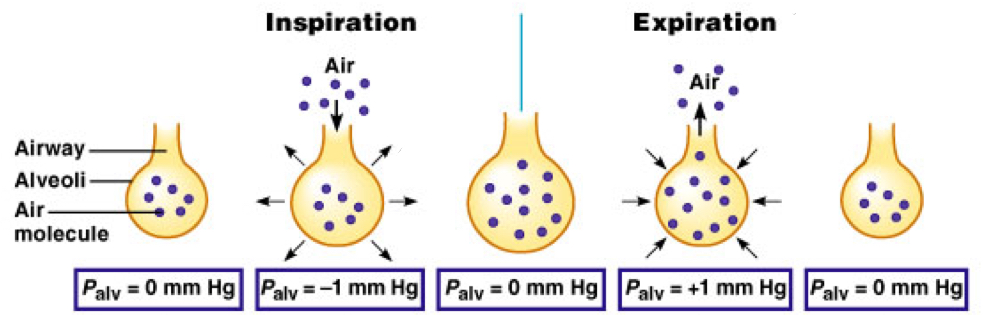
What does a graph for the intra-alveolar pressure look like? Why does it look like that? What about breath volume?
The IAP is curved like that because the alveoli will change their size before intaking/expelling air
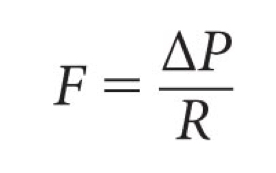
Relationship (equation) between flow (F), pressure (P), and resistance (R)
Flow has an inverse relationship with resistance
How does ΔP change (via physical mechanisms)?
ΔP changes due to respiratory muscles changing lung size
How does resistance change?
Decrease in flow (rate of which air goes into/leaves the lungs) and/or ΔP
Is bronchiolar smooth muscle wired to the PNS or ANS?
PNS
Bronchoconstriction vs bronchodilation
Bronchoconstriction: contraction of smooth muscles in bronchi, making the airway smaller
Bronchodilation: dilation of smooth muscles in bronchi, making the airway larger
What 2 controls impact the contractile states of bronchiolar smooth muscle?
Extrinsic controls
Intrinsic controls
Extrinsic vs Intrinsic controls
Extrinsic — whole body control (nervous system)
Intrinsic — local control/autoregulation
Extrinsic control factors (2)
SNS
Hormones
Intrinsic control factors (2)
CO2
Histamine
What two factors cause bronchodilation?
Extrinsic: SNS activation causes release of epinephrine
Intrinsic: CO2 increase
What two factors cause bronchoconstriction?
Extrinsic: PNS activation causes release of acetecholine
Intrinsic: increase in histamine release (from cells in lungs)
Bronchodilation control factors (extrinsic control) (2)
SNS activation (i.e., bear chasing you)
Extrinsic hormone release
How does extrinsic hormone release occur with bronchodilation?
SNS activation acts on the adrenal gland to release epinephrine, while goes to the bronchioles and causes bronchodilation
Bronchoconstriction control factors (extrinsic control) (1)
Regulated by PNS activation
PNS innervates bronchiolar smooth muscle, causing bronchoconstriction
Acute asthma cause
Caused by spastic contractions of bronchiolar smooth muscle
Triggers for asthma (3)
Cold air
Allergens
Sickness
3 methods to help with asthma
Inhaler
Flo-vent
Medications that are acetecholine inhibitors
How does an inhaler work?
It contains albuterol, which is a Beta2 agonist, acting like epinephrine to bind to Beta2 receptors. This results in SNS activation, and therefore bronchodilation
Chronic obstructive pulmonary disease (COPD)
Long lasting airway obstruction
Examples of COPD (2)
Chronic bronchitis
Emphyzema
What are COPDs usually caused by?
Smoking and airborne pollution + toxins
The pressure that is always less than atmospheric pressure is:
a. Intrapulomonary or Intra-alveolar pressure
b. Intrapleural pressure
c. Transpulmonary pressure
b. Intrapleural pressure — always negative
Inhaling a beta 2 agonist would result in:
a. Bronchodilation
b. Bronchoconstriction
a. Bronchodilation — acts like epinephrine
Inhaling an acetylcholine antagonist would result in:
a. Broncho-dilation
b. Broncho-constriction
c. No change
a. Bronchodilation
Ach antagonists inhibit the action of Ach, resulting in bronchodilation (since Ach causes bronchoconstriction)
Tidal volume
Volume of air that you breathe in during one respiratory cycle
Minute ventilation
Total air moved into and out of your lungs over a minute
Tidal volume x respiratory rate = minute ventilation
Respiratory rate
Number of breaths per minute
Anatomic dead space
Dead space in the conducting zone
Air in these tubes are not involved in respiration
Respiration is NOT happening in the dead space
Alveolar ventilation
The volume of air that reaches the alveoli in the lungs for gas exchange per minute
External respiration location
occurs at alveoli
Internal respiration location
Occurs at the level of the cells and tissues
Gases diffuse ____ their own ____ ____
Gases diffuse down their own pressure gradient
Capillaries around alveoli have a ___ O2 gradient, and a ___ CO2 gradient. This means that O2 will ____ the alveolar capillaries, and CO2 will ___ the alveolar capillaries.
Capillaries around alveoli have a low O2 gradient, and a high CO2 gradient. This means that O2 will enter the alveolar capillaries, and CO2 will exit the alveolar capillaries.
At sea level, ATM pressure is 760 mm Hg . At the top of Mt. Everest, ATM pressure is only 250 mm Hg. Given that the air in both places is 21% oxygen, what is the partial pressure of oxygen at the top of Mt. Everest?
250 × 0.21 = 52.2
Henry’s Law
Describes how much gas will dissolve in a liquid
3 features of Henry’s law
Each gas dissolves in proportion to its partial pressure
At equilibrium, partial pressures in gas and liquid phases will be equal
Amount of each gas that dissolves depends on solubility of the molecule
Is CO2 or O2 more soluble in blood? Why is this and what does this mean?
CO2
CO2 interacts more with water than O2 does, making it more soluble in blood
Means that CO2 doesn’t need as much of a pressure gradient (in alveoli) to make the CO2 leave the capillaries
Easier for CO2 to go from gas to liquid, and visa versa
SLIDES 9-11 — RESPIRATORY SYSTEM, LECTURE B (watch video)!
What 3 factors make external respiration very efficient?
Many capillaries surrounding alveoli
Thin respiratory membrane
Vast surface area because of alveolar number and shape