Pathophysiology II Exam 4 - CARDIO pt. 1
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
126 Terms
function of the right heart
- pulmonary circulation (pumps blood through the lungs)
- delivers blood to the lungs for oxygenation
- is a low pressure system
function of the left heart
- systemic circulation (pumps oxygenated blood through the body)
- is a high pressure system
arteries
carry blood away from the heart
capillaries
exchange fluids between the blood and interstitial spaces
veins
carry blood to the heart
mediastinum
area above the diaphragm and between the lungs where the heart is located
epicardium
outer smooth layer of the heart wall
myocardium
thickest layer of cardiac muscle that makes up the majority of the heart wall
endocardium
innermost layer of the heart wall
pericardium
- double-walled membranous sac that encloses the heart
- has a parietal (surface) and visceral (inner layer)
function of the pericardium
- protects and anchors the heart
- prevents overfilling of the heart with blood
- allows for the heart to work in a relatively friction-free environment
pericardial cavity
space between the parietal and visceral layers that contains pericardial fluid
chambers of the heart
right atrium, right ventricle, left atrium, left ventricle
what are the left and right atria separated by?
the interatrial septum
what are the left and right ventricles separated by?
the interventricular septum
what does the thickness of each heart chamber depend on?
the pressure or resistance it must overcome to eject blood
main function of the heart valves
ensure one-way blood flow
atrioventricular (AV) valves
one-way flow of blood from the atria to the ventricles
tricuspid valve
right AV valve that has 3 leaflets or cusps
bicuspid valve
aka "mitral valve;" left AV valve that has 2 leaflets or cusps
semilunar valves
one-way flow from the ventricles to either the pulmonary artery or to the aorta
pulmonic semilunar valve
prevents blood back-flow from pulmonary artery to right ventricle
aortic semilunar valve
prevents back-flow of blood into the left ventricle
function of the superior and inferior venae cavae
to bring deoxygenated blood from the systemic circulation to the right atrium
function of the right and left pulmonary arteries
- transport unoxygenated blood from the right heart to the right and left lungs
- branch into the pulmonary capillaries
function of the pulmonary veins
to carry oxygenated blood from the lungs to the left side of the heart
function of the aorta
to deliver oxygenated blood to systemic vessels that supply the body
cardiac cycle
one contraction and one relaxation makes up one heartbeat
diastole
relaxation
systole
contraction
path of systemic circulation
arteries -> arterioles -> capillaries -> venules -> veins
peripheral vascular system
systemic circulation that supplies the skin and the extremities
pressure affecting blood flow
force exerted on a liquid per unit area
resistance affecting blood flow
- the opposition to blood flow
- diameter and length of the blood vessels contribute to resistance (i.e., vasoconstriction/vasodilation)
- vessel radius or diameter greatly affects resistance
velocity affecting blood flow
the distance blood travels in a unit in time
viscosity affecting blood flow
thick fluids (i.e., a high hematocrit) move more slowly and cause a greater resistance to flow than thin fluids
vascular compliance affecting blood flow
- stiffness is the opposite
- the increase in volume a vessel is able to accommodate for a given increase in pressure
which blood vessels are more compliant?
veins
1 multiple choice option
mechanisms of arterial pressure regulating blood pressure
- effects of cardiac output
- neural control of resistance
- effects of hormones
- adrenomedullin
- nitric oxide, prostaglandins, endothelium-derived relaxing factor
effects of cardiac output on regulating blood pressure
cardiac output can be changed by alterations in heart rate, stroke volume, or both
neural control of resistance regulating blood pressure
- baroreceptors reduce blood pressure to normal by decreasing cardiac output and peripheral resistance
- arterial receptors (chemoreceptors) are sensitive to oxygen, carbon dioxide, or pH
effects of hormones on regulating blood pressure
- epinephrine and norepinephrine cause vasoconstriction
- ADH increases blood volume by reabsorption of water from tubular fluid in the distal tubule and the collecting duct of the nephron
- RAAS; angiotensin II vasoconstricts while aldosterone stimulates reabsorption of sodium, chloride, and water to increase blood volume and stimulate thirst
- natriuretic peptides cause loss of sodium, chloride, and water through their effects on kidney function, decreasing blood volume
adrenomedullin regulating blood pressure
powerful vasodilatory activity
nitric oxide, prostaglandins, and endothelium-derived relaxing factor regulating blood pressure
cause vasodilation
what is the leading cause of death in the United States and the world?
cardiovascular diseases
mechanisms of cardiovascular diseases
- genetic, neurohumoral, inflammatory, and metabolic
- underlying tissue and cellular alterations
varicose veins
distortion, leakage, increased intravascular hydrostatic pressure, and inflammation of the veins due to the pooling of blood
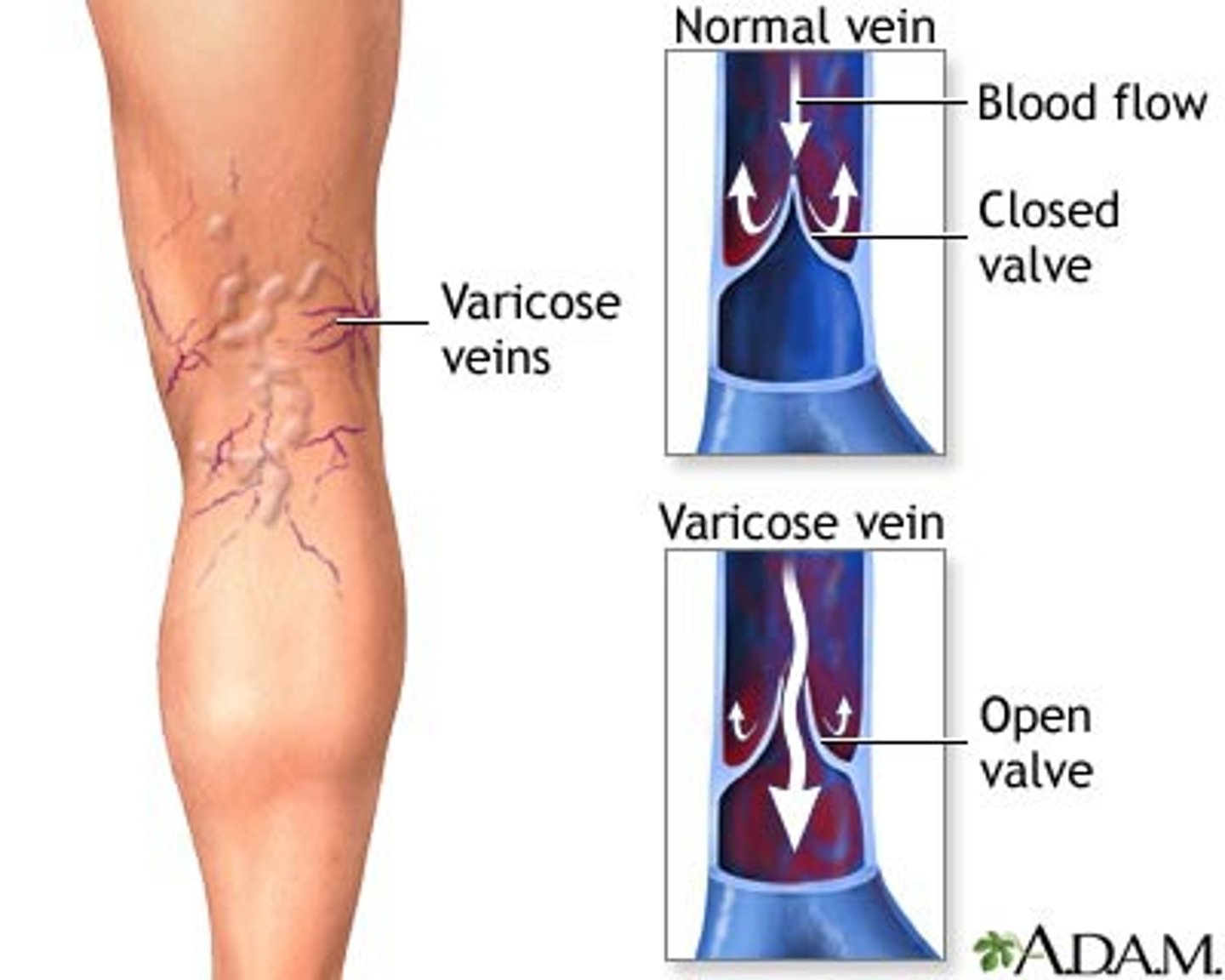
causes of varicose veins
- incompetent valves
- venous obstruction
- muscle pump dysfunction
- or a combination of these
patho of varicose veins
associated with an increase in transforming growth factor beta and basic fibroblast growth factor in vessel walls
how do varicose veins develop?
- skeletal muscle pumps blood up the vessel
- gravity pulls blood down
- overtime damages occur or the valves separate
- when valves fail, pressure increases leading to further valve failure
chronic venous insufficiency
persistent ambulatory lower extremity venous hypertension

patho of chronic venous insufficiency
venous hypertension, circulatory stasis, and tissue hypoxia lead to an inflammatory reaction in vessels and tissue
clinical manifestations of chronic venous insufficiency
- lower extremity edema
- pain
- skin changes
- necrosis
thrombosis
blood clot
deep venous thrombosis (DVT)
- detached thrombus becomes thromboembolus that can lead to pulmonary emboli
- clot in a large vein leads to obstruction of venous flow leading to increased venous pressure
- postthrombotic syndrome
Virchow's triad
- venous stasis
- venous intimal damage
- hypercoaguable state
superior vena cava (SVC) syndrome
progressive occlusion of the SVC that leads to venous distention in the upper extremities and head
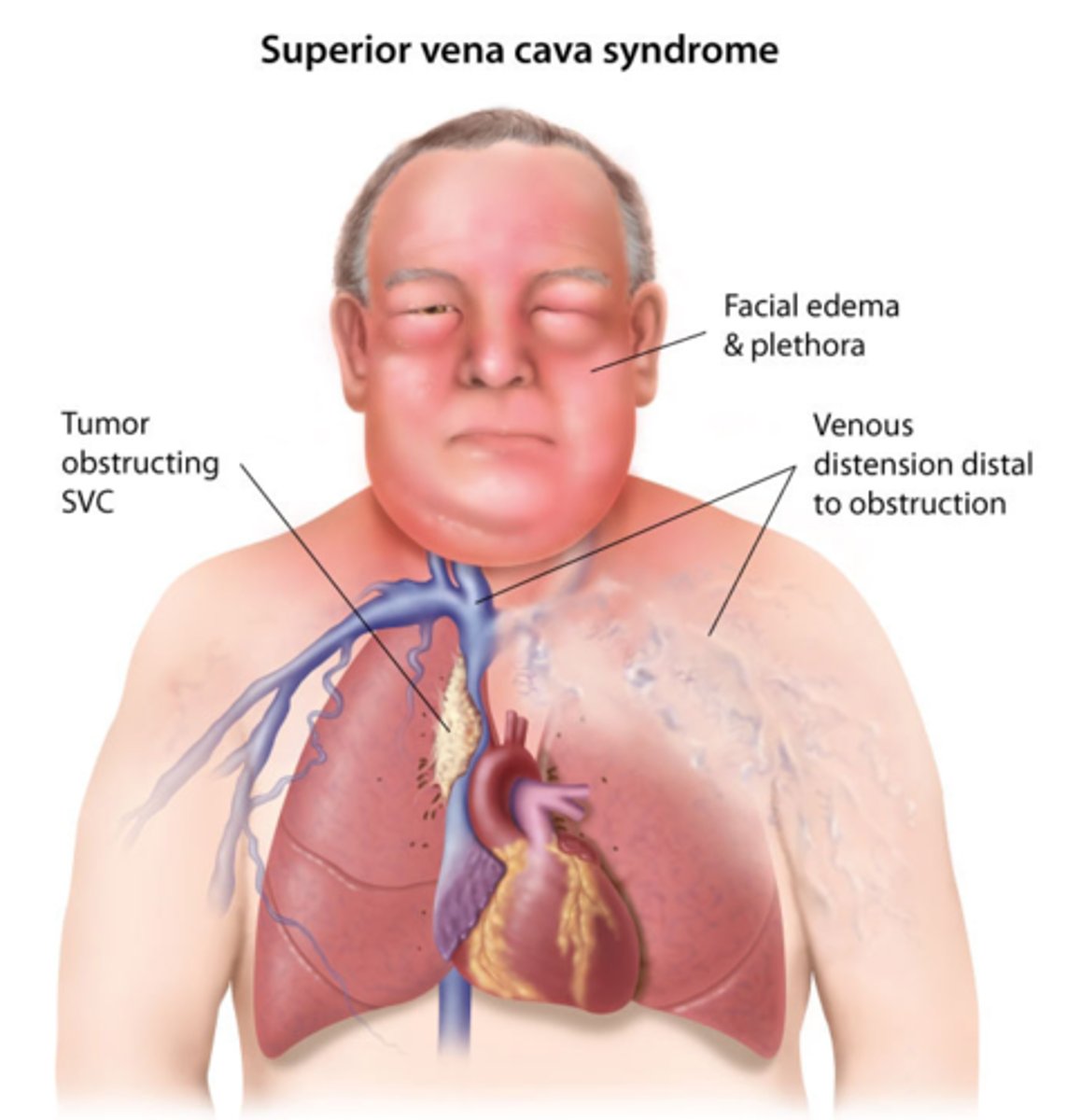
leading causes of SVC syndrome
non-small cell lung cancer, small cell lung cancer, and lymphoma
clinical manifestations of SVC syndrome
- edema
- venous distention of face, neck, trunk, upper extremities
- cyanosis
- dyspnea, dysphagia, hoarseness, stridor, cough, and chest pain
- CNS changes (i.e., headache, vertigo)
- respiratory distress
hypertension
- consistent elevation of systemic arterial blood pressure
- ≥130mmHg systolic or ≥80 mmHg diastolic
isolated systolic hypertension
elevated systolic blood pressure accompanied by normal diastolic blood pressure
primary (essential) hypertension
no identifiable cause; develops over years and most likely attributed to genetic and environmental factors
secondary hypertension
caused by altered hemodynamics from an underlying primary disease or drugs
general characteristics of hypertension
- affects the entire cardiovascular system
- increases the risk for MI, kidney disease, and stroke
risk factors for hypertension
- positive family history
- advancing age
- female >70 y/o and male > 55 y/o
- African American race
- increased sodium intake
- glucose intolerance (DM)/insulin resistance
- heavy alcohol use
- obesity
- cigarettes
patho of hypertension
- increases in cardiac output (i.e., increased HR, SV, blood volume, etc.)
- increase in total peripheral resistance (i.e., increased blood viscosity, reduced vessel diameter, etc.)
patho of primary hypertension
- extremely complicated interactions of genetics and the environment mediated by neurohumoral effects (genetics interact with diet, smoking, age, and other risk factors to cause chronic changes in vasomotor tone and blood volume)
- overactivity of sympathetic nervous system and RAAS, as well as alterations in natriuretic peptides
- inflammation, endothelial dysfunction, obesity-related hormones, and insulin resistance
overactivity of RAAS
- salt and water retention leads to increased vascular resistance
- angiotensin II enhances sympathetic neural outflow and alters the release of hormones that contribute to endothelial dysfunction, insulin resistance, dyslipidemia, and platelet aggregation
- arteriolar remodeling
- associated with end organ effects of HTN
inflammation causing hypertension
- caused by endothelial injury and tissue ischemia
- release of vasoactive cytokines result in vascular remodeling, decreased production of nitric oxide (vasodilators), and increased production of endothelin (vasoconstrictors)
obesity causing hypertension
- release of leptin and adiponectin (adipokines)
- increased activity of the SNS and RAAS
- causes inflammation, small artery remodeling, endothelial dysfunction, and insulin resistance
natriuretic peptides
ANP, BNP, CNP, and urodilantin work to decrease blood pressure
dysfunction of natriuretic peptides
- leads to shift in pressure-natriuresis relationship resulting in an increased blood volume and pressure
- linked to cardiovascular remodeling
- with inadequate function, there is a compensatory increase in levels
patho of secondary hypertension
- caused by systemic disease that raises peripheral vascular resistance and/or cardiac output
- examples include renal vascular or parenchymal disease, adrenocortical tumors, adrenomedullary tumors (pheo), and drugs (such as OCPs, corticosteroids, antihistamines)
complicated hypertension
hypertrophy and hyperplasia with associated fibrosis of the tunica intima and media in a process called vascular remodeling (essentially causing ischemia)
malignant hypertension
aka "hypertensive crisis;" rapidly progressive hypertension
clinical manifestations of malignant hypertension
- diastolic pressure is usually >140 mmHg
- can lead to encephalopathy
clinical manifestations of hypertension
aka "silent disease;" early stages of hypertension have no clinical manifestations other than elevated blood pressure
diagnosis of hypertension
measurement of blood pressure on at least two separate occasions averaging two readings at least two minutes apart with the individual seated, the arm supported at heart level, after 5 minutes of rest, with no smoking or caffeine intake in the past 30 minutes
orthostatic (postural) hypotension
decrease in the systolic and diastolic blood pressures on standing by 20 mmHg or more and by 100 mmHg or more, respectively
patho of orthostatic hypotension
lack of normal blood pressure compensatory mechanisms in response to gravitational changes on the circulation, leading to pooling and vasodilation
what might cause secondary orthostatic hypotension?
medications, starvation, dehydration, immobilization, etc.
clinical manifestations of orthostatic hypotension
fainting upon standing
aneurysm
local dilation or outpouching of a vessel wall or cardiac chamber
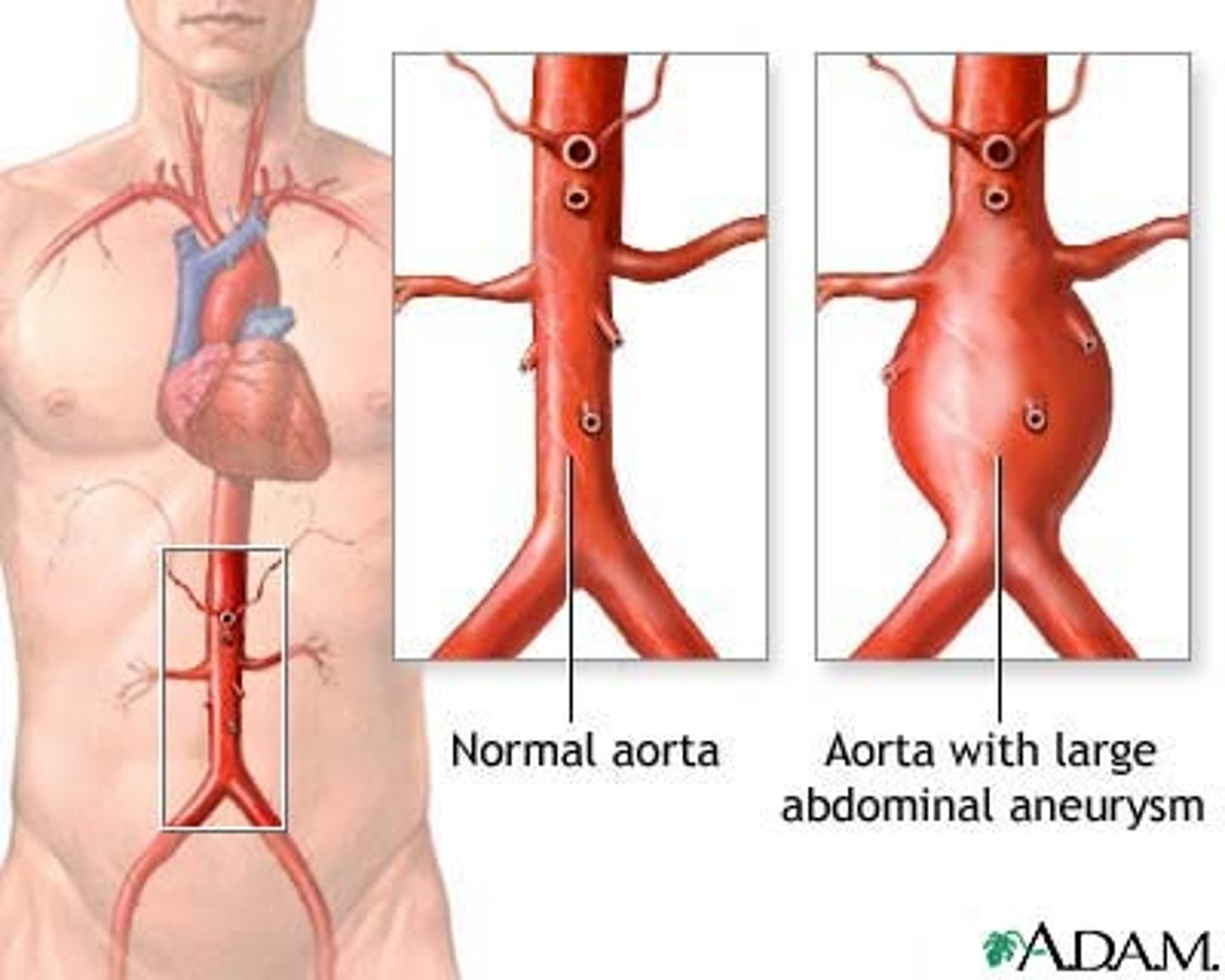
true aneurysms
- involvement of all three layers of the arterial wall
- circumferential and saccular subtypes
false aneurysms
leak between a vascular graft and a natural artery
patho of aneurysm
constant stress on the vessel wall such as
- chronic inflammation activates matrix degrading proteins and smooth muscle apoptosis, transmural infiltration of inflammatory cells
- hypertension results in mechanical and shear forces that contributes to remodeling and weakening
- atherosclerosis and plaque formation erodes the vessel wall
clinical manifestations of a heart aneurysm
includes dysrhythmias, heart failure, and embolism of clots to the brain or other vital organ
clinical manifestations of an aortic aneurysm
asymptomatic until it ruptures, then it becomes painful (often "tearing")
clinical manifestations of a thoracic aneurysm
dysphagia and dyspnea caused by the pressure
clinical manifestations of an abdominal aneurysm
flow to an extremity is impaired, causing ischemia
aortic dissection
- a devastating complication that involves the aorta (ascending, arch, or descending)
- can disrupt flow through the arterial branches
- a surgical emergency
patho of aortic dissection
when there is inflammation and release of enzymes that damage the vessel wall followed by a tear in the intima and blood enters the wall of the artery
type A aortic dissection
involves ascending aorta

type B aortic dissection
involves descending aorta

arterial thrombus formation
activation of the coagulation cascade caused by inflammation and roughening of the tunica intima by atherosclerosis
things that can cause or be caused by arterial thrombus formation
- anatomic changes of an artery
- valvular thrombi
- shock
potential threats to circulation due to arterial thrombus formation
- thrombus may grow large enough to occlude the artery causing ischemia
- thrombus may dislodge becoming a thromboembolus that travels through the vascular system until it occludes flow into a distal systemic vascular bed
embolism
bolus of matter circulates in the bloodstream and then lodges, obstructing blood flow
arterial thrombi affect which side more?
left
1 multiple choice option
what can an embolism be?
- dislodged thrombus (often a DVT)
- air bubble
- amniotic fluid
- aggregate of fat, bacteria, cancer cells
- foreign substance