Reproduction thoery week 1-20
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
3 parts of pregnancy
antepartum
intrapartum
postpartum
antepartum
(before birth)
period after pregnancy before labor
from conception to labor
intrapartum
during labor and delivery
postpartum
period after baby is delivered. usually first 6 weeks sometimes till 12
phases and stages of labour
stage 1
latent
active
transition
stage 2
stage 3
stage 1 of labor
longest stage of labor
begins wiht onset of true regular contractions adn whens when cervix is fully dilated at 10cm
devided into three phases
latent, active, transition
latent phase
cervix dilates from 0 to ~3-4 dm
contractions: mild to moderate, irregular at first then become more regular
mom can still usually talk
active phase
cervix dilates from 4 to 7cm
Contractions: stronger and longer (40-60 seconds), and mroe frequent (every3-5 minutes)
mom usually needs to focus through contractions
Transition phase
cervix dilates from 8 to 10 cm
Contractions: very strong, every 2 ot 3 minutes lasting 60 to 90 seconds
shortest phase but most painful. mom may feel pressure shaking, nausea irritablity or urge to push
stage 2:
expulsion of baby
from full cervical dilation (10cm) to the delivery of baby
contractions are strong and frequent
mothers actively push wiht contractions
ends with brith of baby
stage 3
expulsion of placenta
from delivery of baby to delivery of placenta
usally 5-30 min
contractions conitnue but less intense
placenta and membranes are delivered, uterus contracts to control bleeding
stage 4
first 1-2 hours after placenta delivery
period of maternal stabilization - uterus contracts to prevent hemmorhage
GTPAL & G/P
Gravida, Term, Preterm, Abortion, Living
Gravida/ Para
Gravida
G – Gravida
Total number of pregnancies, regardless of outcome.
Includes current pregnancy, if applicable.
Term
T – Term births
Number of pregnancies delivered at term (≥37 weeks gestation).
Preterm
P – Preterm births
Number of pregnancies delivered preterm (≥20 weeks but <37 weeks).
Abortion
A – Abortions
Number of pregnancies ending before 20 weeks, either spontaneous (miscarriage) or induced.
Living
L – Living children
Number of children currently living.
Para
P – Para: Number of pregnancies that reached viable gestational age (≥20 weeks), regardless of whether the child is living.
GA
Gestational age
acceleration
temporary increase in FHR from baseline, seen during a FHT or NST
Individualized Care
one on one appointments with provider throughout pregnancy, scheduled
these are usualy only 15-30 min. quick. on. a schedule
Group Care
groups of pregnant women in similar GA meet regularly
every 2 to 4 weeks over 6 months
usually 90 to 120 min
there is one provider there, measure fundal heights or BP, weight
some form of education or group discusion. nutrition, stress, mental health, breastfeeding
group sessions can replace individualized care
what are the weeks for each trimester of antepartum/ oregnancy
1st trimester: 0-14 weeks
2nd trimester: 15-27
3rd trimester: 28 until delivery. usually 37 weeks
Fundal height
measurement from pubic symphysis to top of uterus
at 24 weeks and beyond fundal height cm = GA + or - 2weeks
this tracks fetus development adn alerts if fetus is too small or too big
typical care/ schedule for first Trimester of pregnancy
blood panel
initial ultrasound at 12-14 weeks
optional genetic testing
appointments every 4 weels
health and pregnancy history
surgical, ob/gyn histroy, family, medical history
what is included in the blood panel fro 1st trimester
Blood type & Rh factor
CBC (complete blood count)
HIV, Hepatitis B, Syphilis, Rubella immunity
Urinalysis / urine culture (diabetes)
STIs (chlamydia, gonorrhea)
Optional: thyroid, vitamin D, other labs depending on risk
normal values for (Hgb, Hct, PLTs, WBCs)
Lab | Normal Range (Pregnancy) | Physiological Change |
|---|---|---|
Hemoglobin (Hgb) | ≥11 g/dL (1st & 3rd trimesters) ≥10.5 g/dL (2nd trimester) | Mild hemodilution → “physiologic anemia” |
Hematocrit (Hct) | ~32–42% | Decreases due to plasma expansion |
Platelets (PLTs) | 150,000–400,000 /mm³ (may fall slightly but >100,000) | Mild decrease possible; <100,000 = concern (gestational thrombocytopenia or preeclampsia) |
White Blood Cells (WBCs) | 5,000–15,000 /mm³ (can rise to 25,000 during labor/postpartum) | Leukocytosis due to stress, hormones |
In a non pregnant adults (not needed to know)
Lab | Normal Range (Female) | Notes |
|---|---|---|
Hemoglobin (Hgb) | 12–16 g/dL | Measures oxygen-carrying capacity |
Hematocrit (Hct) | 36–48% | % of blood volume that is RBCs |
Platelets (PLTs) | 150,000–400,000 /mm³ | Clotting function |
White Blood Cells (WBCs) | 4,000–10,000 /mm³ | Immune defense |
typical care/ schedule for second Trimester of pregnancy
Appointments every: 4 weeks
Ultrasound at: 18–22 weeks – anatomy scan; gender reveal optional
GTT testing at: 24–28 weeks (1-hour glucose tolerance test for gestational diabetes)
Fundal Height, FHTs: measured at every visit
Maternal AFP
typical care/ schedule for third Trimester of pregnancy
appointments every 2 weeks unitl 36 weeks
after 36 weeks every week until delivery
Groub B strep 35-37 weeks
vaginal/rectal swab. if positive mom gets iv antibiotics during labor
fundal heihg
fetal heart tones each visit
cervical checks
optionacl, typicaly begin 36-38 weels. mainly if indicated or concer for labor progress. or contractions
discussion of labor / planning
FHT
Fetal Heart Monitoring tracs fetal heart rate to assess well being and fetal viability
manual listening with a doppler or fetoscope
FHS in 2nd trimester
HR: usually 120-160bpm (usually slightly higher in early second trimester, slows in late second trimester)
doppler is most common tool to measure
Fetal movements: kick counts start around 28 weeks. should feel at least 10 movements in 2 hours
NST
a non stress test is conducted if there are abnormal findings during FHT, maternal conditions such as diabtees, post term pregnancy(>40 weeks),
this is a non invasive test that monitors hetal heart rate response to fetal movements
goal: determin if babt is well oxygenated and neuroligcally intact
how its peformed
the mother reclines in chair or bed
two monitors placed on abdomen
detects contractions
detects fetal heart rate
mother may press button when she feels the baby move
usally lasts 20-40 min
how performed
reactive
2 or greater accelerations in FHR within 20 min,
(after 32 weeks)each lasting 15 seconds or geater and rising 15 bpm above baseline
(before 32 weeks) criteria are >= 10bpm for 10 seconds
GTT testing and why
Gestation glucose tolerance test
Gestiational diabetes mellitus (GDM) can develop during pregnancy
testing helps prevent complicatoins for both infant and mother
performed at 24-28 weeks
1 hour screening (50g glucose)
blood drawn 1 hour after drinking sugary solution
passing value: <140mg/dl
if equal or greater than moves to a 3 hour test
3 hour GTT (100g glucose)
blood drawn, fasting, 1 hour, 2 hour, 3 hour after drinking
diagnosis made if 2 or more values are elevated
management
diet modification
excersize
sometimes insulin or medications
what are teh three types of confirming pregnancy
presumptive
probable
positive
presumptive confirmation of pregnancy
Subjective — reported by the patient. These suggest pregnancy but are not proof (they could have other causes).
Amenorrhea (missed period)
Nausea/vomiting (“morning sickness”)
Breast changes (tenderness, enlargement, darkened areola)
Fatigue
Frequent urination
Quickening (mother feeling fetal movement, around 16–20 weeks — but gas/other movement can feel similar)
probable sings of pregnancy
Objective — observed by examiner. Stronger evidence than presumptive, but still not 100% conclusive (could be due to other conditions like tumors, hormonal changes).
Positive pregnancy test (hCG in blood or urine — false positives can occur with certain tumors or fertility meds)
Goodell’s sign (softening of cervix)
Chadwick’s sign (bluish-purple discoloration of cervix/vagina due to vascularity)
Hegar’s sign (softening of lower uterine segment)
Ballottement (fetus rebounds when examiner taps cervix/vagina)
Braxton Hicks contractions
Enlargement of abdomen/uterus
positive
absolutely confirm pregnancy. Can only be explained by a fetus.
Examples:
Ultrasound evidence of fetus (gestational sac, fetal pole, cardiac activity)
Fetal heart tones heard by Doppler (around 10–12 weeks) or fetoscope (16–20 weeks)
Fetal movement palpated by examiner (not just reported by mom)
EDD and how is it calculated
estimated due date
uses naegeles rule
takes day of last menstrual period (LMP)
subtract 3 months and add 3 days, adjust for year
OR add 9 months and 7 days
determining Gestation age
GA assessment with crown rump length (top of head to bottom) done less than 14 weeks has an accuracy of +- 5-7 days
why is determining GA important
helps in letting providers know what developmental milestones a baby should/ is hitting
should there be a HR, should there be fetal movement rn
accurate plannig and care testing
GTT, GBS, anatomy scan
safe timing of interventions and deliver
induction of labor, stopping preterm labo
viability GA
~23/24 weeks
if preterm parents have to decide if they will go through resucitation or hospice and ensure baby is given a peaceful time before death.
Maternal afp testing 2nd tri
Maternal alpha fetoprotein
protein that devloping baby makes and passes into maternal blood
high or low levels indicate complications
blod test around 15-20 weeks (around time of NT ultrasound
GBS testing
group b streptococcus often found in vagina/rectum
many women carry harmlessly but during delivery can pass to baby and cause serious infection
routinely done at 35-37 weeks
mother given antibiotics during pregnancy to reduce infant exposrue
this is very common. more of a coincidence that anything indicitave of the mother. colinization is unpredictable and does not consider someone as sick
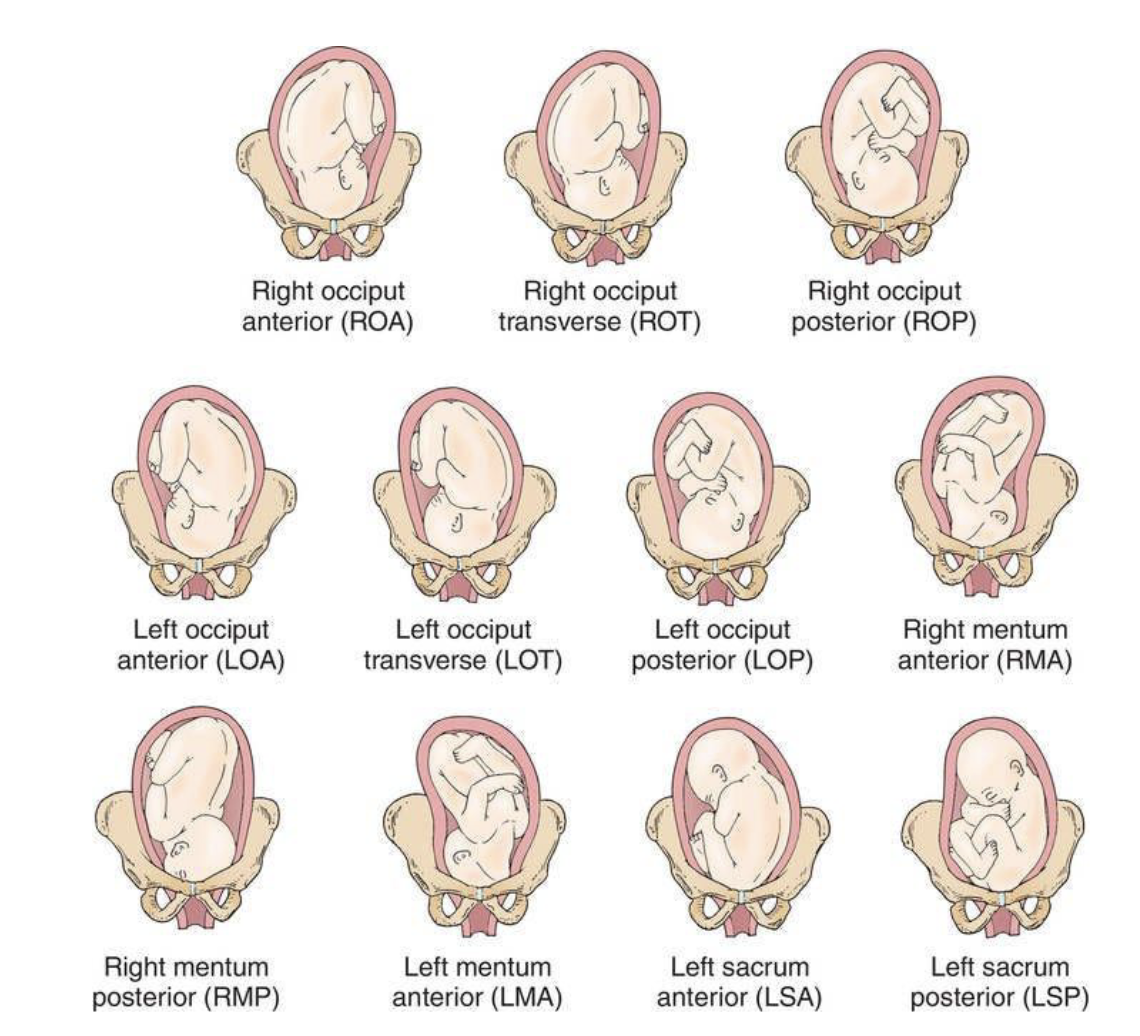
passenger position and why is it iimportant
orientation of baby as it moves through mothers pelvis
What side of the mother’s pelvis the baby’s presenting part is facing
Which part of the baby is presenting (the part that’s entering the pelvis first)
Which direction that presenting part is facing within the pelvis
seperated into three letters
Fetal position tells us how the baby is oriented in the mother’s pelvis, which affects how easily labor and birth happen.
first letter of passenger position
First letter — Left (L) or Right (R)
This tells you which side of the maternal pelvis the fetal reference point (a landmark on the presenting part) is pointing toward.
L = toward mother’s left
R = toward mother’s right
So it’s not about which way the baby’s face points overall — it’s about which side the reference point is closer to.
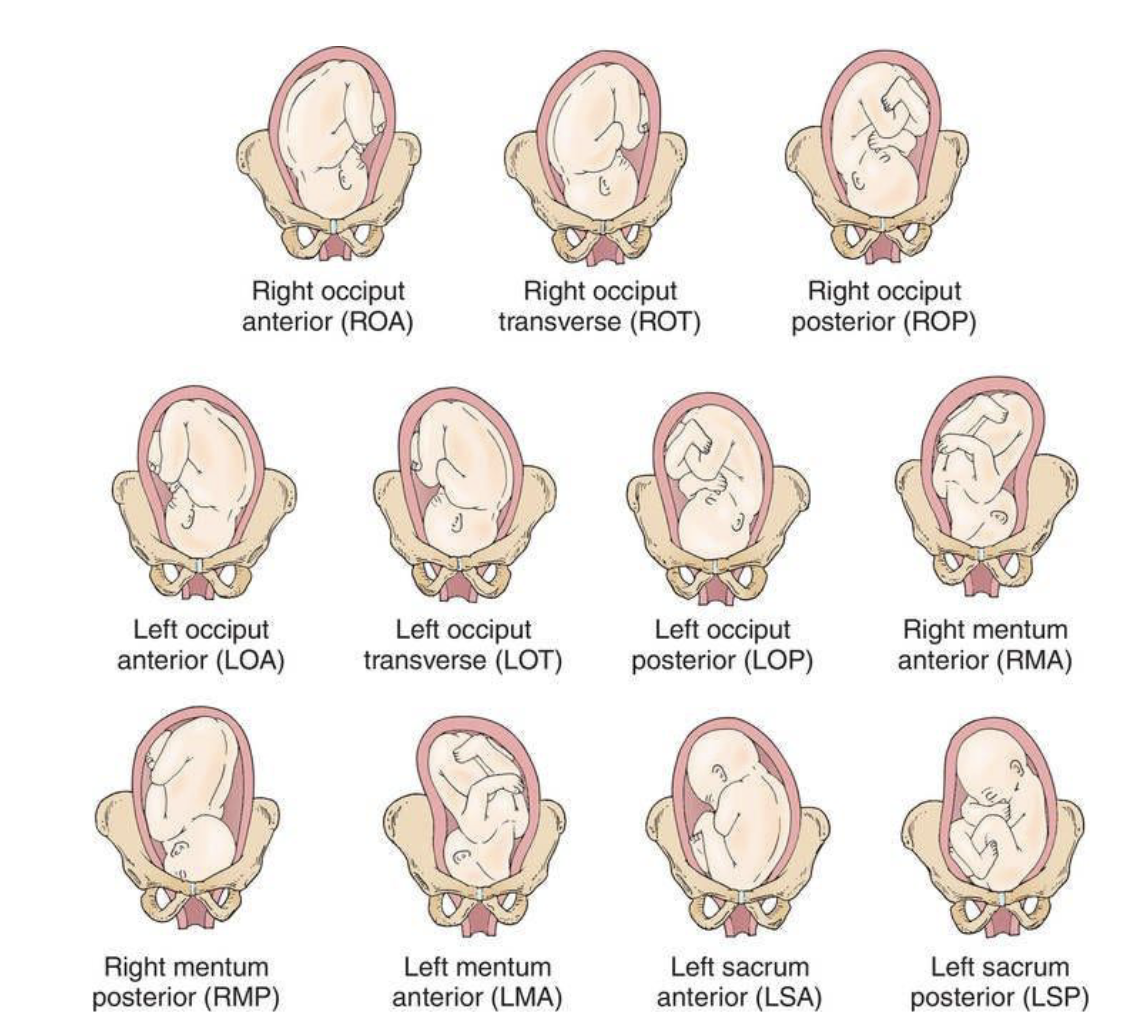
second letter of passenger position
Fetal presenting part (the landmark)
This letter shows what part of the baby is presenting — it depends on what’s coming out first.
Presentation | Landmark | Letter | Meaning |
|---|---|---|---|
Vertex (head flexed) | Occiput (back of head) | O | Occiput |
Face | Mentum (chin) | M | Mentum |
Breech | Sacrum (butt) | S | Sacrum |
Shoulder | Acromion process | A | Acromion |
So:
O = head first (normal)
S = butt first (breech)
M = face presentation
A = shoulder presentation
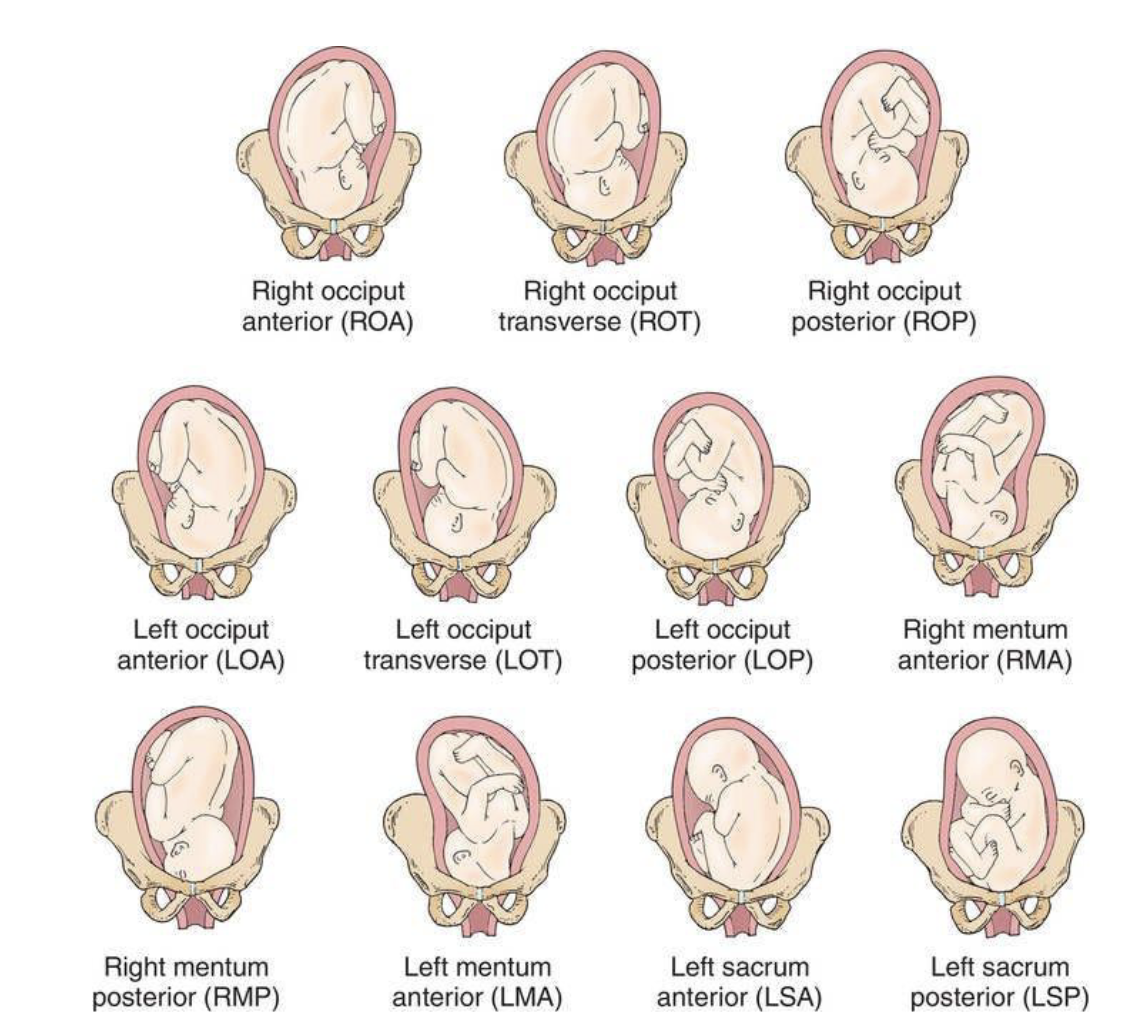
third letter of passenger position
hird letter — Anterior (A), Posterior (P), or Transverse (T)
This shows which way the fetal reference point is facing relative to the mother’s pelvis (front or back).
A = toward anterior (mother’s front)
P = toward posterior (mother’s back)
T = transverse, facing sideways
dialation
measured in cm, range from 0-10
must reach 10 cm before pushing
this is to assess progress of labour, stages and phases. is the woman ready to push
effacement
how thin and short the cervix has become (cervix needs to be soft and thin for baby to be
measured in percent 0 to 100%
Measurement | Meaning |
|---|---|
0% | Thick, long cervix |
50% | Half thinned |
100% | Completely thinned out (“paper-thin”) |
must reach 100% before pushing
station
How low the baby’s presenting part (usually the head) is in relation to the ischial spines of the mother’s pelvis.
Station | Meaning |
|---|---|
–5 | High in pelvisthe |
0 | Level with ischial spines (“engaged”) |
+5 | Crowning — visible at vaginal opening |
How it’s measured:
By feeling where the baby’s head is during a vaginal exam, compared to the ischial spines.
When lowermost portion of presenting part is 1 cm below spines said to be (+1)
criteria for contraction assesment
frequency
duration
intenisty
Palpation (feeling with your hands)
The provider feels the top of the uterus (fundus) during a contraction.
They estimate how hard it feels:
Mild: feels like the tip of your nose
Moderate: feels like your chin
Strong: feels like your forehead
B. Internal monitoring (intrauterine pressure catheter — IUPC)
A thin catheter goes inside the uterus and measures pressure in mmHg.
Gives a quantitative number for intensity:
Mild: ~25 mmHg
Moderate: ~50 mmHg
Strong: 50–100 mmHg or more
criteria for fetal heart rate
baseline
variability
accelerations
decelerations
baseline
The average fetal heart rate over 10 minutes when the baby is not experiencing contractions or accelerations/decelerations.
Normal range:
110–160 beats per minute (bpm)
Why it matters:
Shows the baby’s overall oxygenation and well-being.
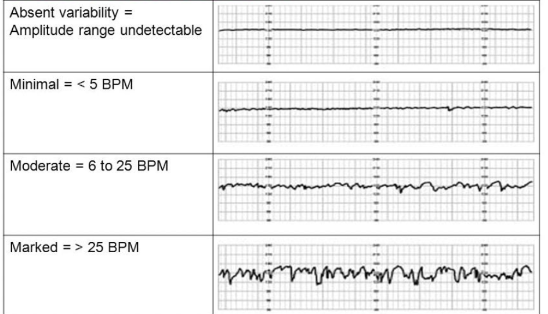
variability
What it is:
The fluctuations in the FHR around the baseline,(not random troughs beat-to-beat changes.
Types:
Absent: undetectable
Minimal: <5 bpm
Moderate: 6–25 bpm (normal, reassuring)
Marked: >25 bpm
Why it matters:
Reflects the baby’s autonomic nervous system and oxygenation.
Moderate variability = good, baby is healthy.
accelerations
What it is:
Temporary increases in FHR above baseline.
Definition:
≥15 bpm above baseline for ≥15 seconds (≥32 weeks gestation)
Shorter/milder for <32 weeks
Why it matters:
Usually a reassuring sign that the baby is doing well.
decellerations
What it is:
Temporary decreases in FHR below baseline.
Types:
Early decelerations – mirror contractions, caused by head compression, usually benign.
Variable decelerations – abrupt drops, caused by cord compression. May need intervention if severe.
Late decelerations – start after contraction begins, caused by uteroplacental insufficiency, concerning.
Prolonged Decelerations
What it is:
A drop in fetal heart rate below the baseline that lasts longer than 2 minutes but less than 10 minutes.
If it lasts 10 minutes or more, it’s considered a baseline change, not just a deceleration.
Why it matters:
Helps detect fetal distress or potential oxygen problems.
different deceleration types physiological cuase and nursing intervention
DECELERATION TYPE | PHYSIOLOGIC CAUSE | NURSING INTERVENTION |
|---|---|---|
Early | Fetal head compression (often benign and occurs with contractions) | Continue to monitor; no intervention usually needed; assess labor progress |
Variable | Umbilical cord compression | Reposition mother (side to side, knee-chest); administer oxygen; discontinue oxytocin if infusing; consider amnioinfusion; notify provider |
Late | Uteroplacental insufficiency (decreased oxygen transfer to fetus) | Reposition to left side; stop oxytocin; administer oxygen via face mask; increase IV fluids; notify provider; prepare for possible delivery |
Prolonged | Cord prolapse, maternal hypotension, uterine tachysystole, or prolonged cord compression | Reposition mother; administer oxygen; stop oxytocin; IV fluid bolus; assess for cord prolapse; notify provider immediately; prepare for emergency intervention if unresolved |
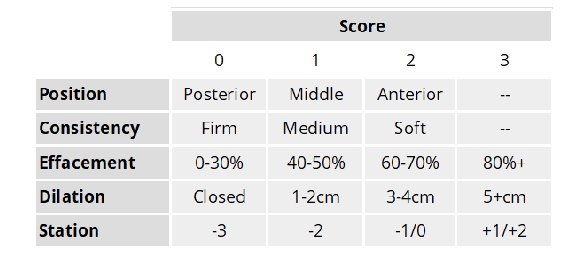
Bishops score
Low Score (< 5) = “unfavorable” =
• High Score (>8) = “favorable” =
regional anesthesia (epidural)
Combination of local anesthetic (bupivacaine),
opioid analgesic (fentanyl) or BOTH
• Time of Action ~ 15-20 minutes for full relief
• Duration ~ entirety of labor/ deliver
Nursing Considerations
• IV fluid bolus before procedure
• Assist with patient positioning
• Continuous pulse oximeter
• Frequent VS (q 5 mins, q15 mins, q 30 mins)
• Assess pain and sensory levels
• Foley catheter or I/O cathete
Nitrous oxide
laughing gas,” reduces perception of pain
• 50:50 mix of nitrous + oxygen using blender device and mask
• Rapid onset and quick clearance with exhalation
• Side Effects: nausea, dizziness
• Nursing Considerations:
• Teach woman how to self-administer
• Apply mask during start of contraction, breath slowly, remove in between
contractions
• NO ONE ELSE except the patient can use/ administer it
• Cannot use in combination with IV/ IM narcotics
Image Credit
induction of labor
Medical Indications vs Elective (Non-medically Indicated) Delivery
Medical:
Condition makes it safer or better for mother or baby to deliver
Examples: preeclampsia, fetal growth restriction, maternal diabetes, placental issues, prolonged rupture of membranes, fetal compromise
Elective (non-medically indicated):
Labor or delivery is chosen without a medical reason
Must wait until ≥39 weeks gestation (full-term) to reduce risks of neonatal complications
Brief Summary: Induced Labor
Induction of labor = starting labor artificially instead of waiting for spontaneous contractions.
Methods:
Medications
Prostaglandins (gel or insert) → soften cervix (ripening)
Oxytocin (Pitocin) → stimulate contractions
Mechanical
Foley balloon → stretches cervix to trigger labor
Other
Amniotomy → breaking the water to start contractions
Reasons for induction:
Medical indications (see above)
Post-term pregnancy (>41–42 weeks)
Maternal conditions that make waiting risky
Goal:
Achieve effective contractions and progressive cervical changes for safe vaginal delivery.
involution
process of uterus returning to pre pregnancy size shape and position after birth
cervical ripening agents
Agent | Type | Route | Key Points | Adverse Effects |
|---|---|---|---|---|
Dinoprostone (Cervidil, Prepidil) | Prostaglandin E₂ | Vaginal insert or gel | Most commonly used; Cervidil can be easily removed if uterine hyperstimulation occurs | Uterine tachysystole, fetal distress, nausea, vomiting |
Misoprostol (Cytotec) | Prostaglandin E₁ | Vaginal, oral, or sublingual tablet | Inexpensive and effective; also used for postpartum hemorrhage | Higher risk of uterine tachysystole; contraindicated in previous cesarean (risk of rupture) |
Method | Description | Advantages | Disadvantages |
|---|---|---|---|
Foley balloon catheter | A balloon inserted into cervix and inflated with saline to exert pressure | Low cost, less risk of hyperstimulation | Discomfort, infection risk |
oxytocin in labor
. It stimulates uterine contractions
Oxytocin acts directly on uterine smooth muscle receptors.
It causes rhythmic contractions that push the baby down toward the cervix and eventually through the birth canal.
These contractions help dilate and efface the cervix, moving labor along.
Postpartum
After the baby and placenta are delivered, the uterus needs to firmly contract to clamp down on the open blood vessels where the placenta was attached.
If it doesn’t, the vessels stay open → postpartum hemorrhage (excessive bleeding).
Oxytocin stimulates strong, rhythmic uterine contractions to:
Compress uterine blood vessels → ↓ bleeding
Promote uterine involution → uterus shrinks back to pre-pregnancy size
Expel any remaining clots or tissue
in almost all births, oxytocin is routinely given postpartum.
This is part of what’s called “Active Management of the Third Stage of Labor (AMTSL)”, a globally recommended practice (by WHO, ACOG, etc.) to prevent postpartum hemorrhage (PPH) — the leading cause of maternal death worldwide.
preeclampsia and why its a concern
Preeclampsia is diagnosed when a pregnant woman has:
Blood pressure ≥ 140/90 mmHg on two occasions at least 4 hours apart after 20 weeks,
ANDEvidence of protein in the urine (proteinuria) or signs of organ dysfunction (like abnormal labs or symptoms).
poses risk for btoh mother and. baby
Abnormal placental development
The placenta doesn’t implant deeply enough into the uterine wall.
The blood vessels that feed it stay narrow and high-resistance, so the placenta doesn’t get enough oxygen (placental ischemia).
Placenta releases harmful substances
The stressed placenta releases factors into the mother’s bloodstream.
These damage blood vessel linings (endothelium) and cause vasoconstriction and inflammation throughout her body.
Widespread vascular damage and organ effects
Damaged vessels raise blood pressure, leak fluid, and form tiny clots.
This reduces blood flow to the kidneys, liver, brain, and placenta, leading to proteinuria, headaches/vision changes, and fetal growth restriction.
uterine tachyssytole
More than 5 contractions in 10 minutes, averaged over a 30-minute window.
Can occur spontaneously or due to excess uterotonic stimulation (like oxytocin or misoprostol).
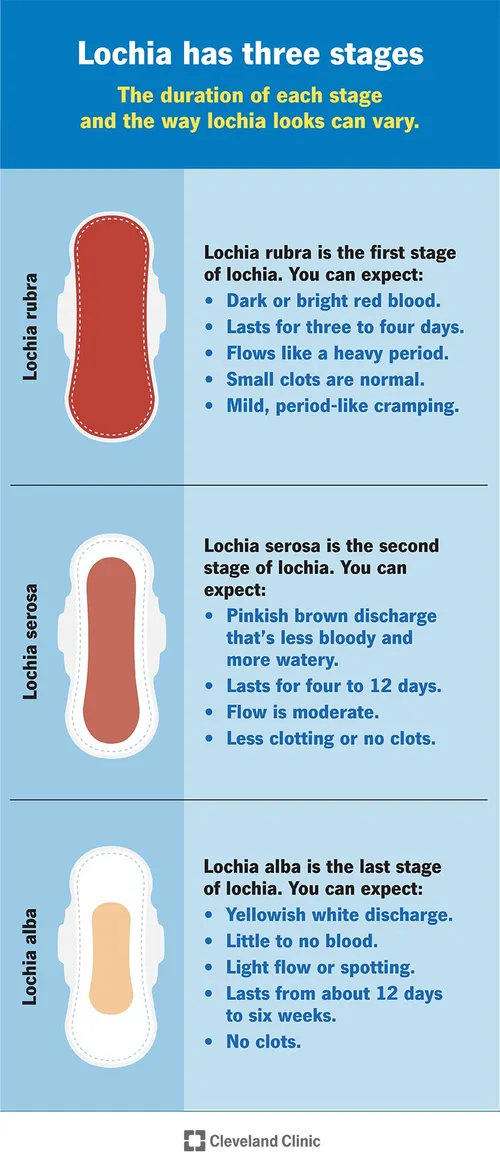
transition of lochia after birth
lochia rubra, lochia serosa, lochia silba,
lochia rubra, seros and alba
Lochia Type | Time | Normal | Abnormal |
Lochia rubra | Days 1-3 | Bright red, blood consistency; fleshy odor; temporary increase with breastfeeding and rising | Numerous large clots; foul smell; saturation of pad in half hour or less |
Lochia serosa | Usually days 4-9 (can last to 27 days) | Pinkish brown; serosanguineous consistency | Foul smell; saturation of perineal pad in 1 hour or less |
Lochia alba | Day 10 to about 6 weeks | Creamy white; fleshy odor | Foul smell; persistent lochia discharge over 3 weeks; return to pink or red discharge |
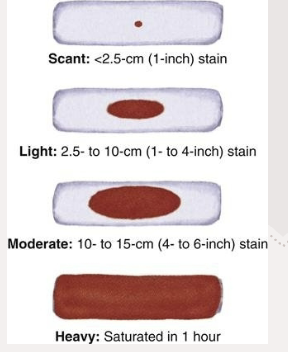
also measure amount
fundal assesmment
Tone – firm or boggy
Height – where it is relative to the umbilicus
Position – midline or deviated (often right if the bladder’s full)