Complete Blood Count RBC Indices
1/153
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
154 Terms
What CBC component is the following:
Erythrocytes- biconcave disc with no nucleus
RBCs
what are complete blood counts useful for?
detecting disorders (infections, anemia, autoimmunue/immune mediated, allergy, blood cancers)
monitor response and/or side effects of treatment
What CBC component is the following:
Granulocytes (granular, multilobulated)
•Neutrophils
•Eosinophils
•Basophils
Agranulocytes (agranular, single nucleus)
•Lymphocytes
•Monocytes
WBCs
What CBC component is the following:
Essential cells for clot formation
•Megakaryocytes
Platelets
Define the following:
Process where mature blood cells are produced from hematopoietic stem cells (HSCs)
Hematopoiesis
where does fetal/embryonic hematopoiesis originate?
yolk sac
Biconcave disc with no nucleus:
erythrocytes
where does fetal/embryonic hematopoiesis mature?
fetal liver & spleen
what is the major site of hematopoiesis in children & adults?
bone marrow
What are erythrocytes function?
oxygen & carbon dioxide transport
____________ binds/transports O2 from the lungs to tissues & CO2 from tissues to the lungs
hemoglobin protein
where is erythropoietin produced?
kidneys
What has the following characteristics?
- Convert Pro-erythroblasts to erythrocytes,
- Stimulates the production of RBCs when O2 saturation is low (e.g. COPD patients)
erythropoietin
What blood cells contribute to blood cancers?
White blood cells because they have a nucleus (DNA)
low RBC count:
anemia
high RBC count:
polycythimea
normal RBC count for males:
4.5-5.9 million/mL
normal RBC count for females:
4-5.2 million/mL
The average life span of the RBC is:
120 days
RBC count can be decreased by...
decreased production from bone marrow
How can patients with leukemia have anemia?
Leukemia cells rapidly divide in bone marrow, overwhelming the healthy RBCs, so they have a difficulty stopping bleeding
what are potential causes of decreased RBC count?
decreased production from bone marrow
increased destruction (hemolysis)
blood loss
sickle cell anemia causes a decrease in RBC caused from:
Increased destruction (hemolysis)
thalassemia causes a decrease in RBC caused from:
Increased destruction (hemolysis)
a chronic O2 deficiency will _____ RBC count & stimulate ______
increase; erythropoietin
increase in RBCs due to chronic O2 deficiency:
primary polycythemia vera
increase in RBCs due to dehydration, steroid use, or smoking:
secondary polycythemia
dehydration, steroid use, and smoking will ____ RBC count
increase
in Hb F, beta chains are replaced by:
gamma chains
normal hemoglobin for males:
13.0 to 17.5 gm/dL
normal hemoglobin for females:
11.5 to 15.5 gm/dL
how many ferrous molecules are on the quaternary Hb A molecule?
4
what are the components of the quaternary protein Hb A?
2 alpha chains
2 beta chains
4 ferrous molecules
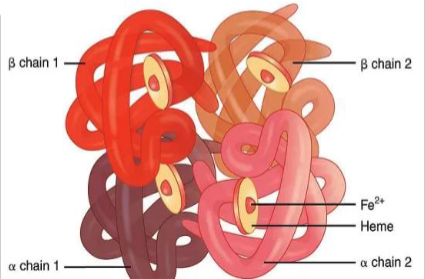
which form of hemglobin is found in fetus? following birth?
fetus → Hb F
following birth → Hb A
normal hematocrit for males:
41%-50%
normal hematocrit for females:
36%-48%
Define the following:
% by volume of RBCs in blood
hematocrit
Why does renal failure cause anemia?
EPO production in kidney compromised
Low hemoglobin & hematocrit etiologies include:
anemia via dietary, blood loss, chronic disease
Reduction in Hb & HCT indicates:
tissue hypoxia & poor wound healing
what is mean corpuscular volume (MCV)>
the size of a mature RBC:
mean corpuscular volume (MCV) is calculated by:
HCT/RBC count
normal mean corpuscular volume (MCV) range is:
80-100 fL
a mean corpuscular volume (MCV) less than 80fL is:
microcytic
a mean corpuscular volume (MCV) greater than 100 fL is:
macrocytic
a mean corpuscular volume (MCV) between 80-100 fL is:
normocytic
Amount of Hb per Red blood cell:
mean corpuscular hemoglobin (MCH)
normal mean corpuscular hemoglobin (MCH) range is:
27-34 pg
a mean corpuscular hemoglobin (MCH) less than 27 pg is:
hypochromic
a mean corpuscular hemoglobin (MCH) between 27-34 pg is:
normochromic
a mean corpuscular hemoglobin (MCH) greater than 34 pg is:
hyperchromic
mean corpuscular hemoglobin (MCH) is calculated by:
Hb/RBC count
Define the following:
Hb concentration in a given volume of packed red blood cells
mean corpuscular hemoglobin concentration (MCHC)
normal mean corpuscular hemoglobin concentration (MCHC) range is:
32- 36 gm/dl
Mean corpuscular hemoglobin concentration (MCHC) is calculated:
Hb / HCT
Define the following:
- Degree of variation in size in RBCs
- Increased RDW
anisocytosis
normal red blood cell distribution width (RDW) is:
10-15%
patients with dehydration will show a ________ HCT & MCV
increased
patients with polycythemia vera will show a ________ HCT & MCV
increased
patients with COPD will show a ________ HCT & MCV
increased
patients with anabolic steroids will show a ________ HCT & MCV
increased
patients in high altitudes will show a ________ HCT & MCV
increased
patients with anemia (--> iron deficiency) will show a ________ HCT & MCV
decreased
patients with hemolysis (sickle cell, thalassemia) will show a ________ HCT & MCV
decreased
patients with acute leukemia will show a ________ HCT & MCV
decreased
patients with pancytopenia will show a ________ HCT & MCV
decreased
patients with lead toxicity will show a ________ HCT & MCV
decreased
___________ cell --> MCV is SMALLER than 80 fl/RBC
Microcytic
what is the leading cause of microcytic cells?
iron deficiency anemia
what is the 2nd leading cause of microcytic cells?
thalassemia
Define the following:
A measure of body's iron stores
ferritin levels
Ferritin levels in low deficiency anemia are _____________
low
___________ cell --> MCV is LARGER than 100 fl/RBC
Macrocytic
what is the leading cause of megaloblastic anemia?
B12 deficiency (pernicious anemia)
what is the 2nd leading cause of megaloblastic anemia?
folic acid deficiency
During a blood work up, you observe macrocytosis, there are defects in nuclear maturation, MCV & MCH are increased, while the MCHC remains normal, there is anisocytosis, and RDW is increased. You know that this macrocytosis is due to:
foliate or B12 deficiency
during a blood work up, you observe macrocytosis, there is no defect in nuclear maturation, the cells are large due to an excess red cell membrane, these cells are round, rather than oval, and the RDW is normal. You know that this macrocytosis is due to:
liver disease
_____________ measures the average amount of hemoglobin in each mature RBC
MCH
Microcytic anemias are associated with ____ MCH
low
Macrocytic anemias are associated with ____ MCH
increased
Causes of low MCHC:
- Iron deficency anemia
- Thalassemia
Causes of high MCHC
- Autoimmune hemolytic
- Anemia
- Severe burns (burns hemolytic anemia/loss of plasma)
- Liver disease (if liver damages RBCs)
What is the normal red cell distribution width (RDW)?
11.5-14.5%
Increased RDW (anisocytosis) with a decreased RBC count indicates:
active bone marrow, body is trying to compensate
Decreased RDW with a decreased RBC count indicates:
depressed bone marrow (dysfunctional bm)
__________ RDW may be associated with:
•Iron deficiency
•Vitamin B12
•Folic acid deficiency
•Hgb deficiency
•Hemolysis
•Blood transfusion
Increased
Normal Reticulocyte Count:
0.5% to 1.5%
Define the following:
Measures erythropoietic activity & BM response to anemia
Reticulocyte Count (immature nucleated RBCs is increased)
Aplastic anemia: reticulocyte count is:
low, BM not making enough RBCs
Hemolytic anemia: reticulocyte count is:
high, RBCs are destroyed prematurely & BM works overtime
Iron deficiency anemia: reticulocyte count is:
low, body does not have enough iron to make RBCs
Pernicious anemia: reticulocyte count is:
low, the body does not get enough vitamin B12
Hemolysis can occur with any of the inherited or Hemolytic anemias. The examples of congenital/hemolytic anemia are... (4)
- Sickle cell
- Thalassemia
- Hereditary spherocytosis
- G6PD deficiency
Decreased Reticulocyte count can be associated with: (4)
• Anemia of chronic disease
• Anemia due to renal failure because of decreased erythropoietin production
• Anemia associated with bone marrow failure
• Anemia due to low iron or B12 stores
Examples of acquired anemias
- Chronic use of aspirin
- NSAIDs
- Corticosteroids (can cause GI bleeding)
Are the following microcytic, normocytic, or macrocytic anemia?
• Iron deficiency anemia
• Chronic disease- lupus, rheumatoid arthritis, etc..
• Genetic anemias --> thalassemias, sideroblastic anemia, spherocytosis
Microcytic (<80fl)
Are the following microcytic, normocytic, or macrocytic anemia?
• Chronic disease
• Sickle cell disease
• Combined deficiencies (e.g iron and B12 deficiency rogether)
• Blood loss
Normocytic (80-99 fl)
Are the following microcytic, normocytic, or macrocytic anemia?
• B12/folate deficiency
• Hemolysis
• MDS (myeloproliferative disorder)
Macrocytic (>100fl)
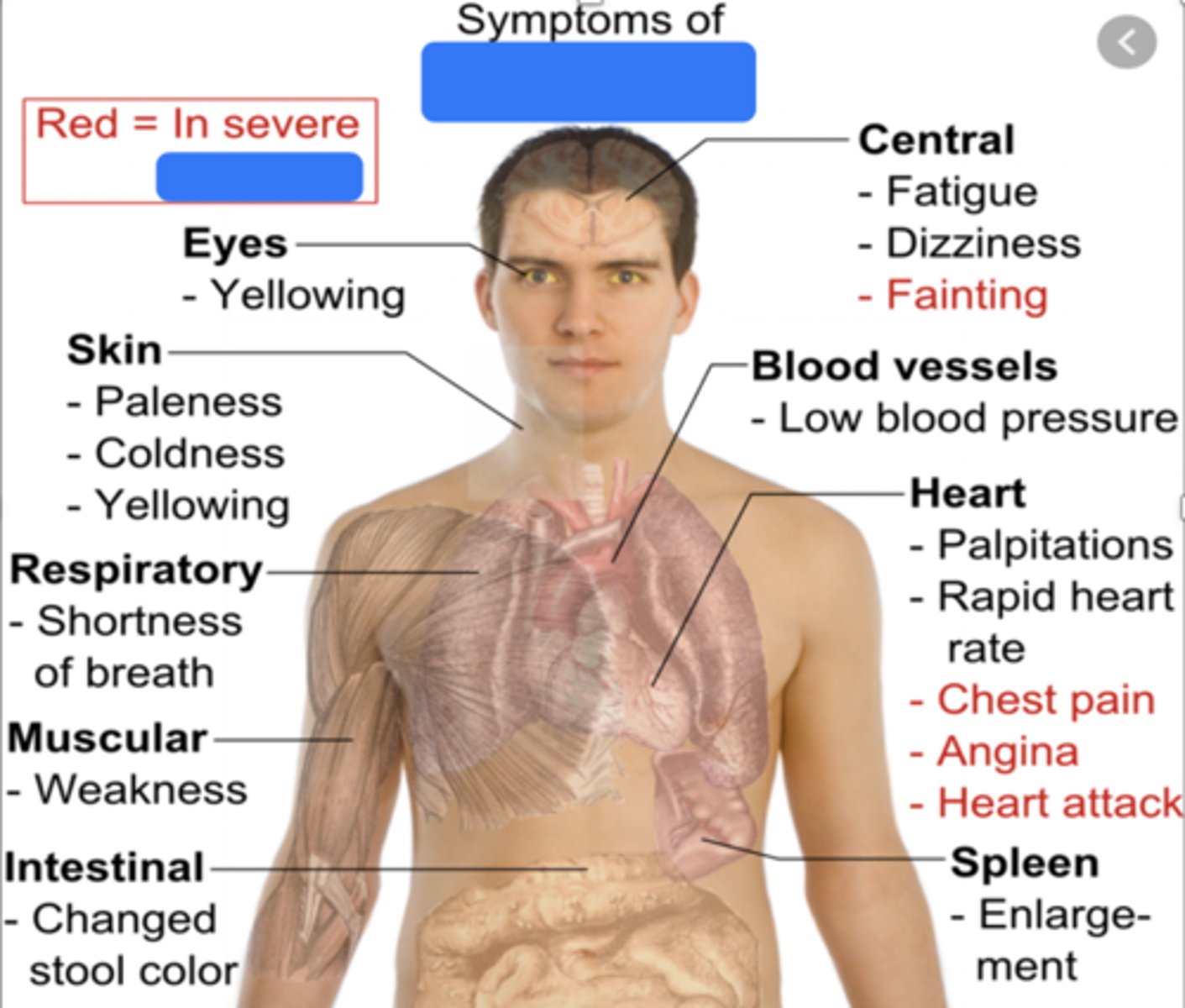
The image shows symptoms of. ____________
Anemia
what are 4 symptoms of severe anemia?
fainting
angina
chest pains
heart attack