Pulmonary Exam 1: Physiology - Perfusion and Ventilation (Dr. Leavis)
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
Define the following:
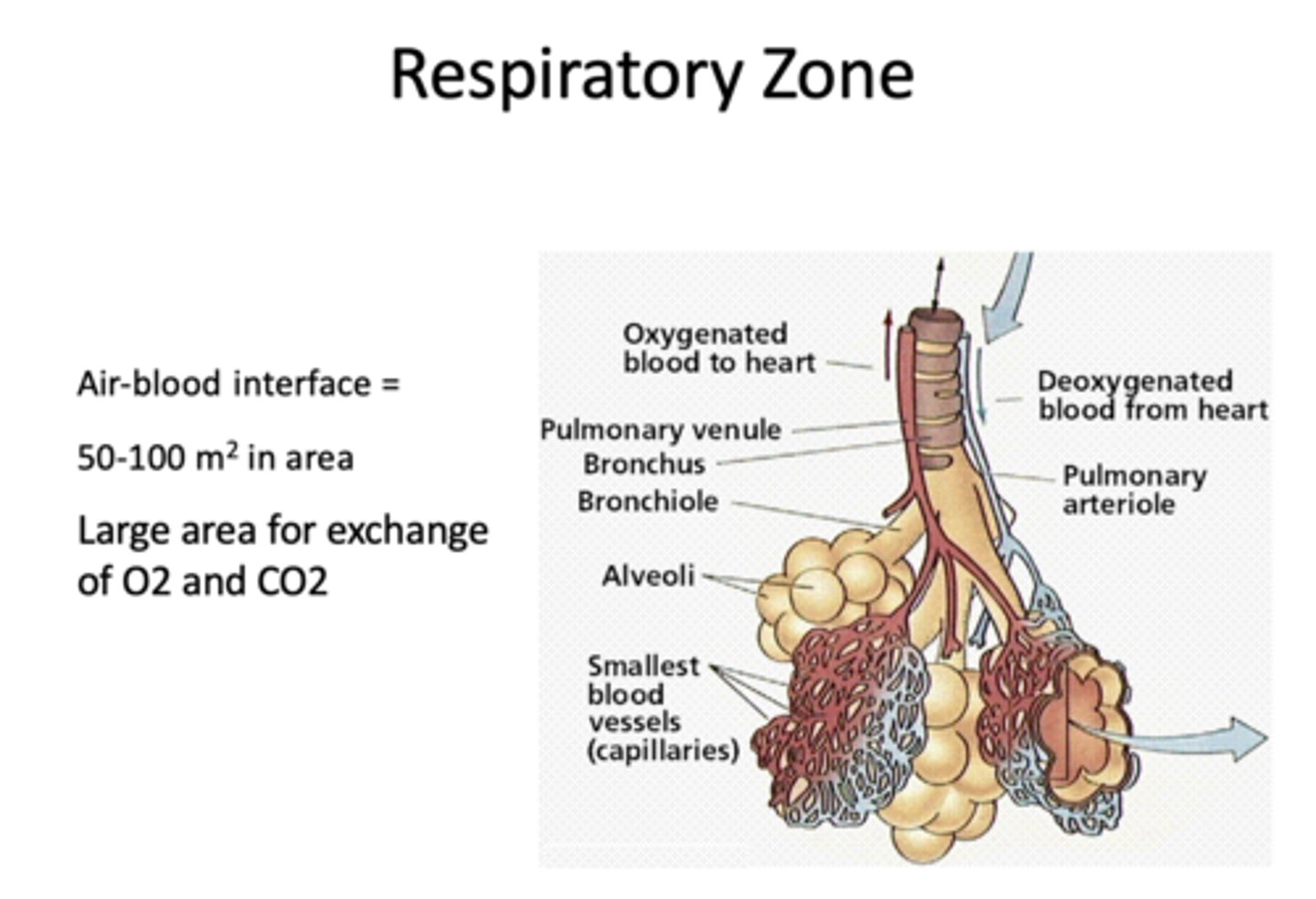
Large area for exchange of O2 and CO2
respiratory zone
Define the following:
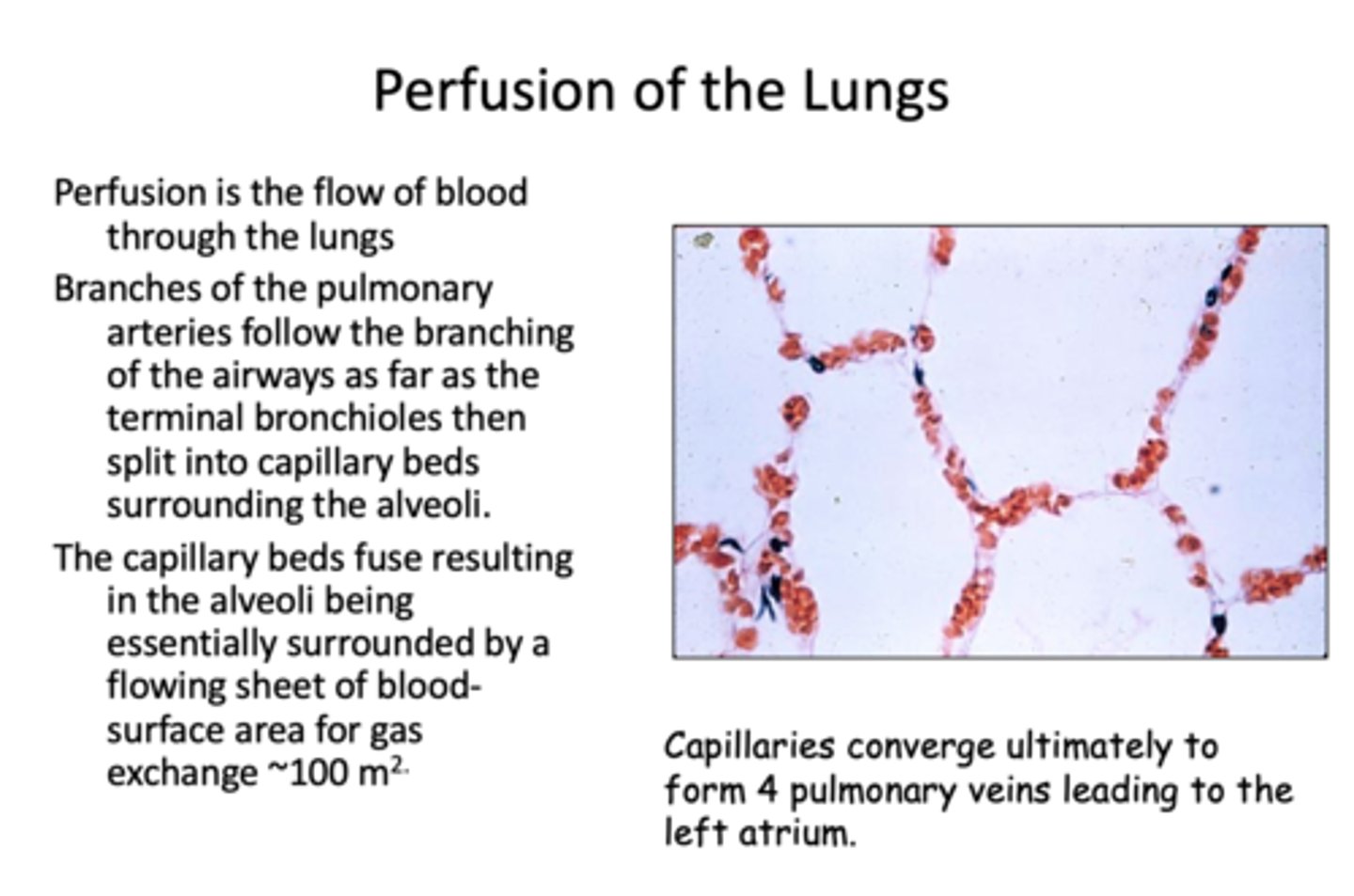
The flow of blood through the lungs
perfusion
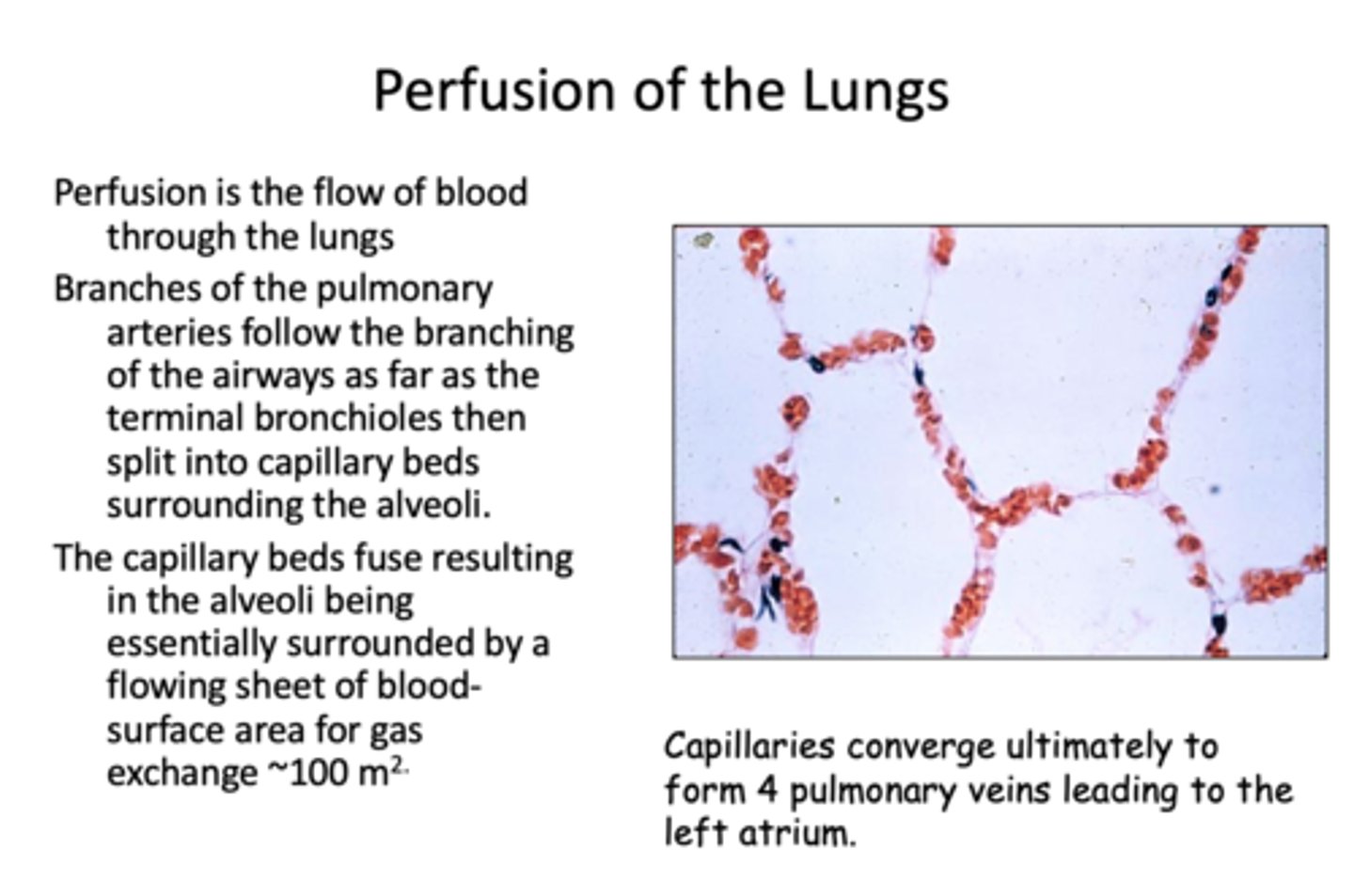
Branches of the pulmonary arteries follow the branching of the airways as far as the terminal bronchioles then split into capillary beds surrounding the __________
alveoli
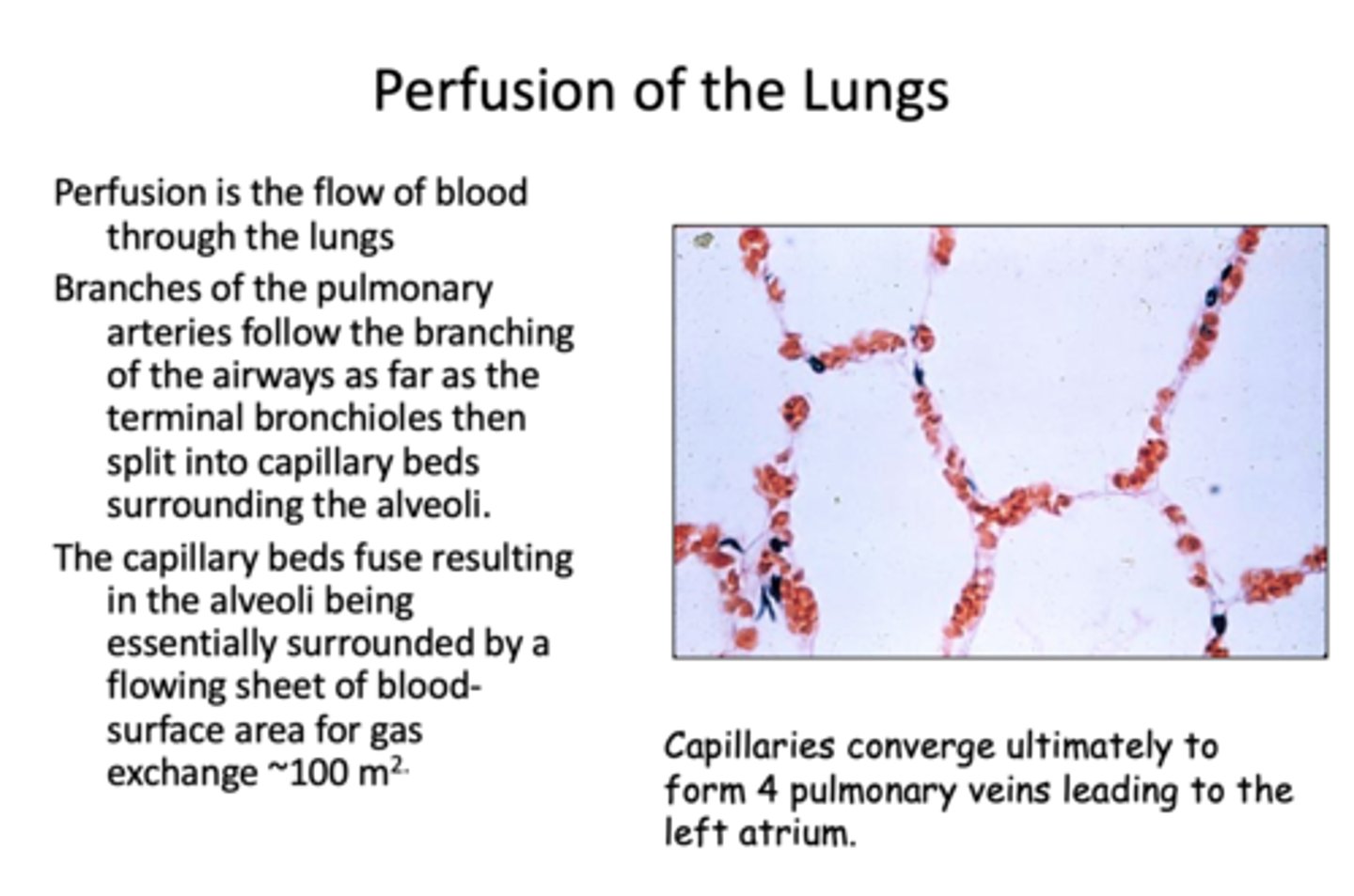
Capillaries converge ultimately to form 4 pulmonary veins leading to the __________
left atrium
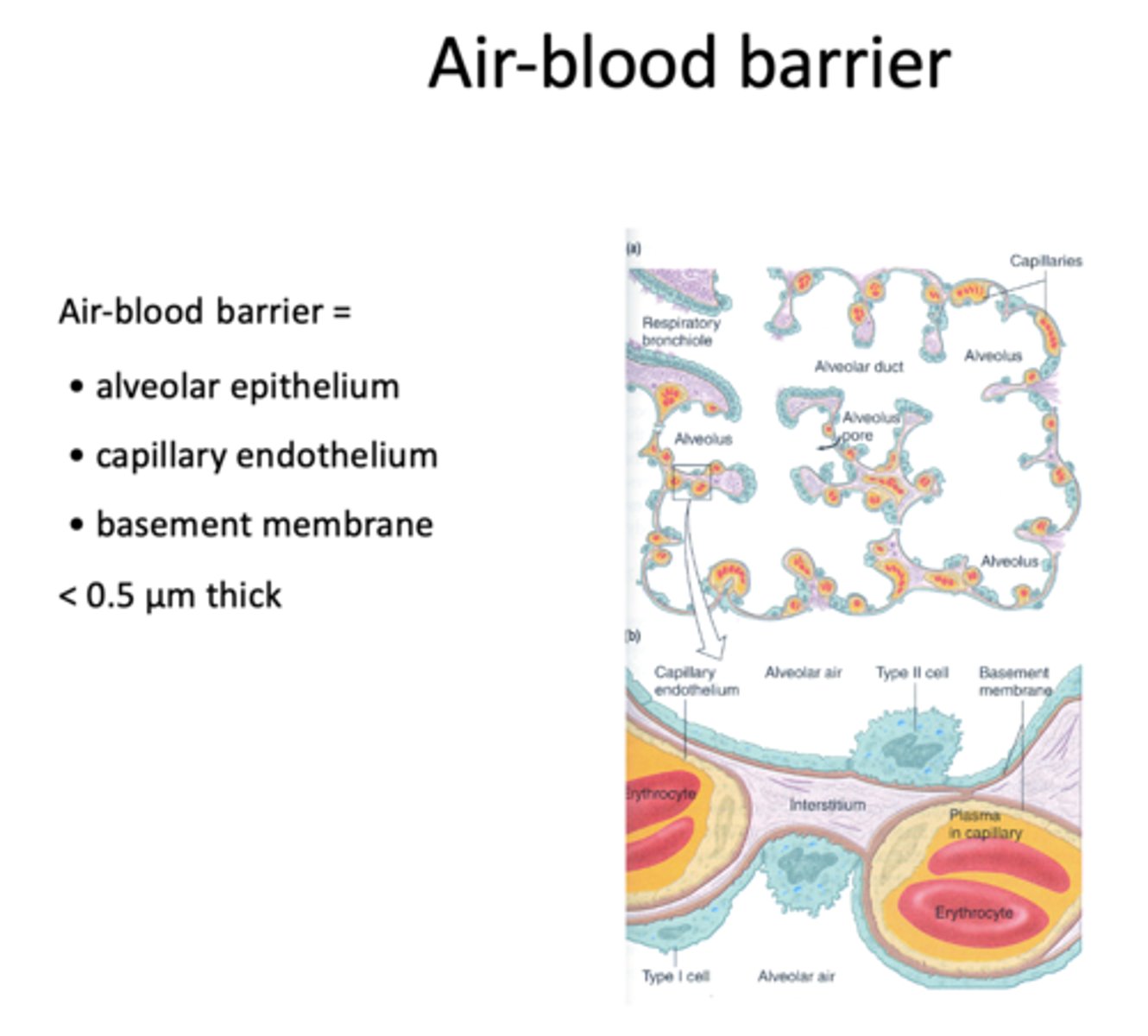
what 3 components make up the air-blood barrier?
- Alveolar epithelium
- Capillary endothelium
- Basement membrane/interstitium
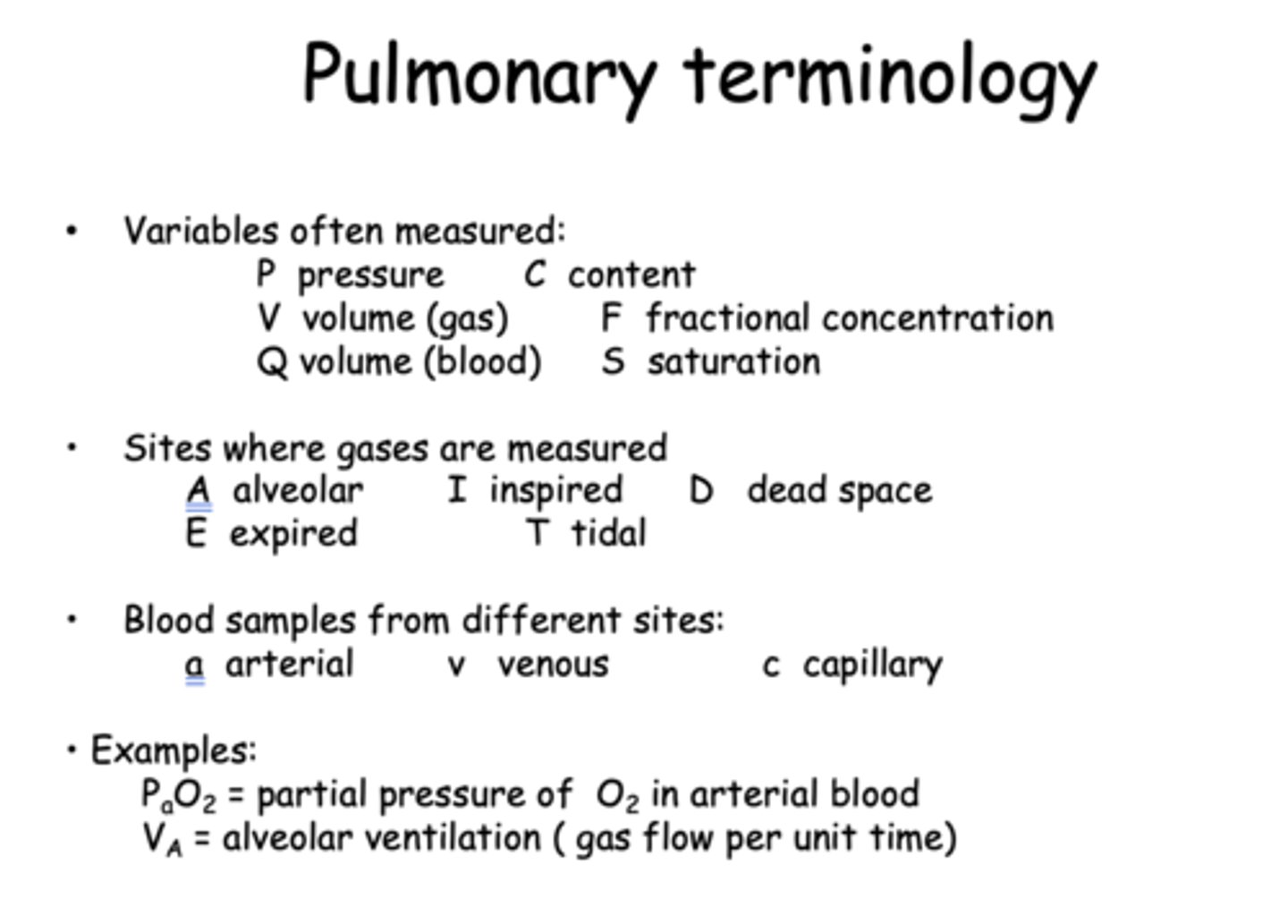
What does Q stand for in pulmonary terminology?
Volume of blood
What does V stand for in pulmonary terminology?
Volume of gas
What does PaO2 stand for?
Partial pressure of O2 in arterial blood
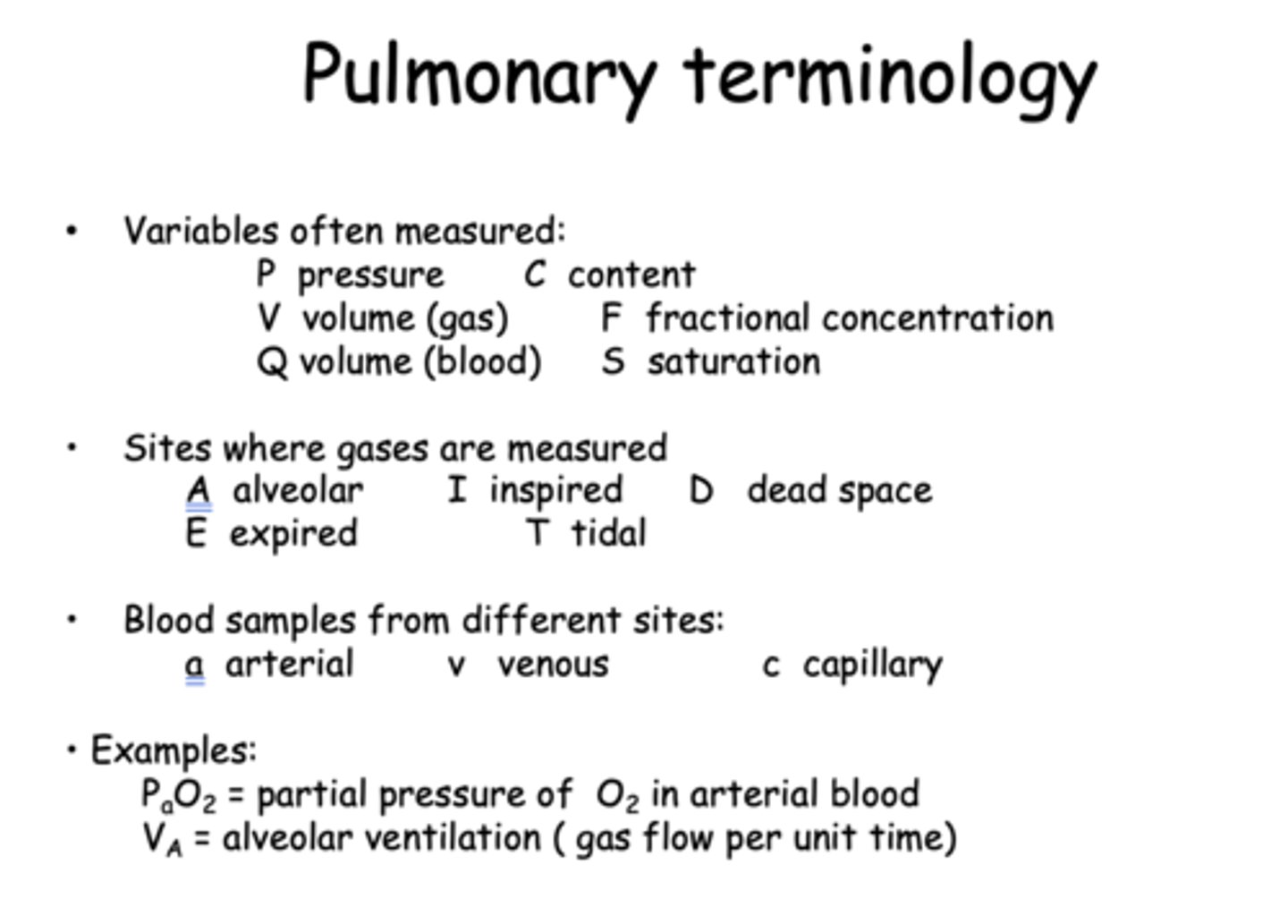
What does VA stand for?
Alveolar ventilation ( gas flow per unit time)
The pulmonary circulation handles the same blood flow as does the systemic circulation; about ___ liters/minute
5 (or 83 ml/sec)
At rest, the total circulation time through the pulmonary system is 4-5 seconds. The pulmonary capillary bed contains about _________ml blood in an upright person and the average erythrocyte takes about ________ seconds to pass through the alveolar capillary bed.
75 ml, 0.75 seconds
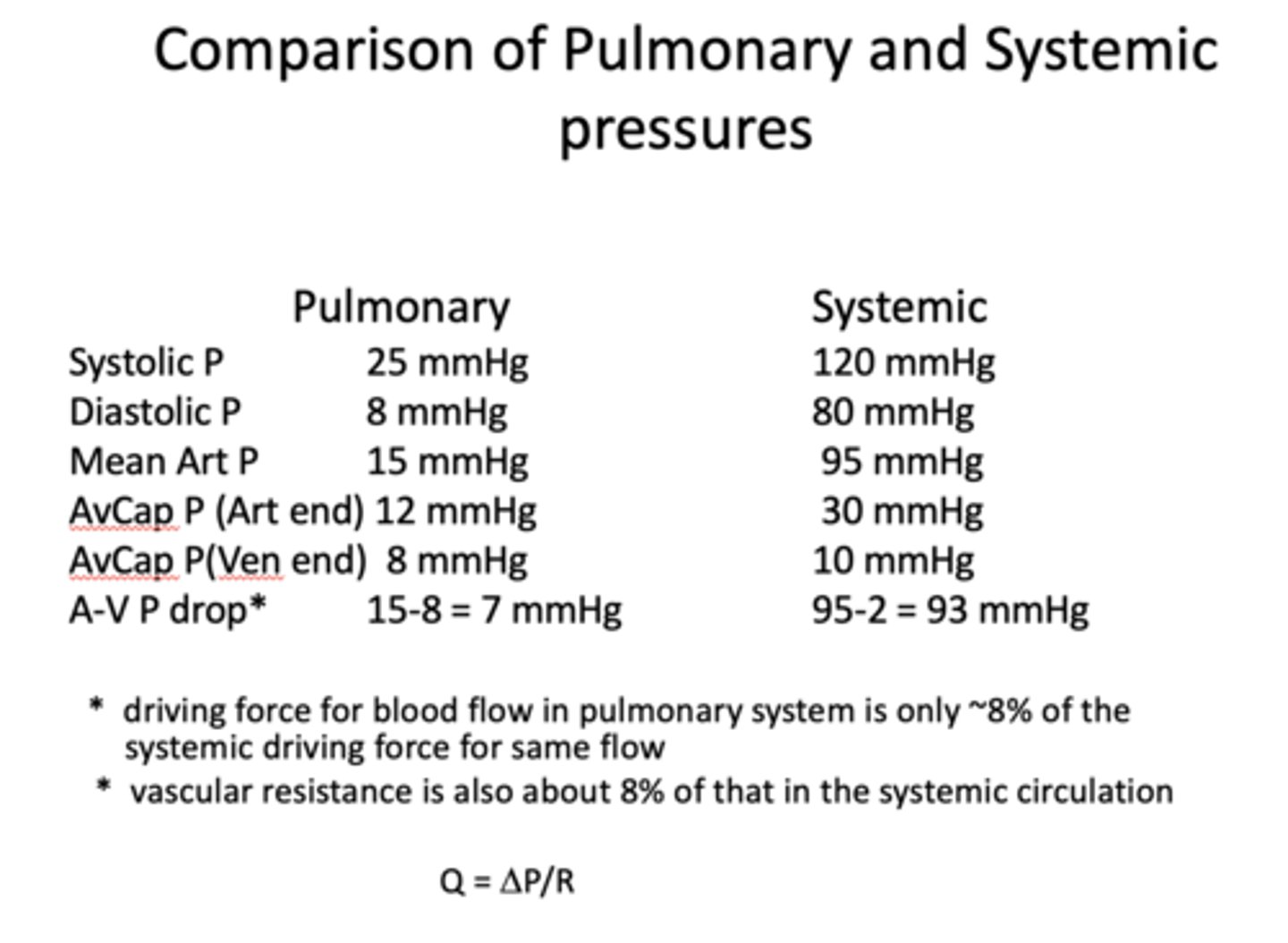
the pulmonary system is _____ pressure
low
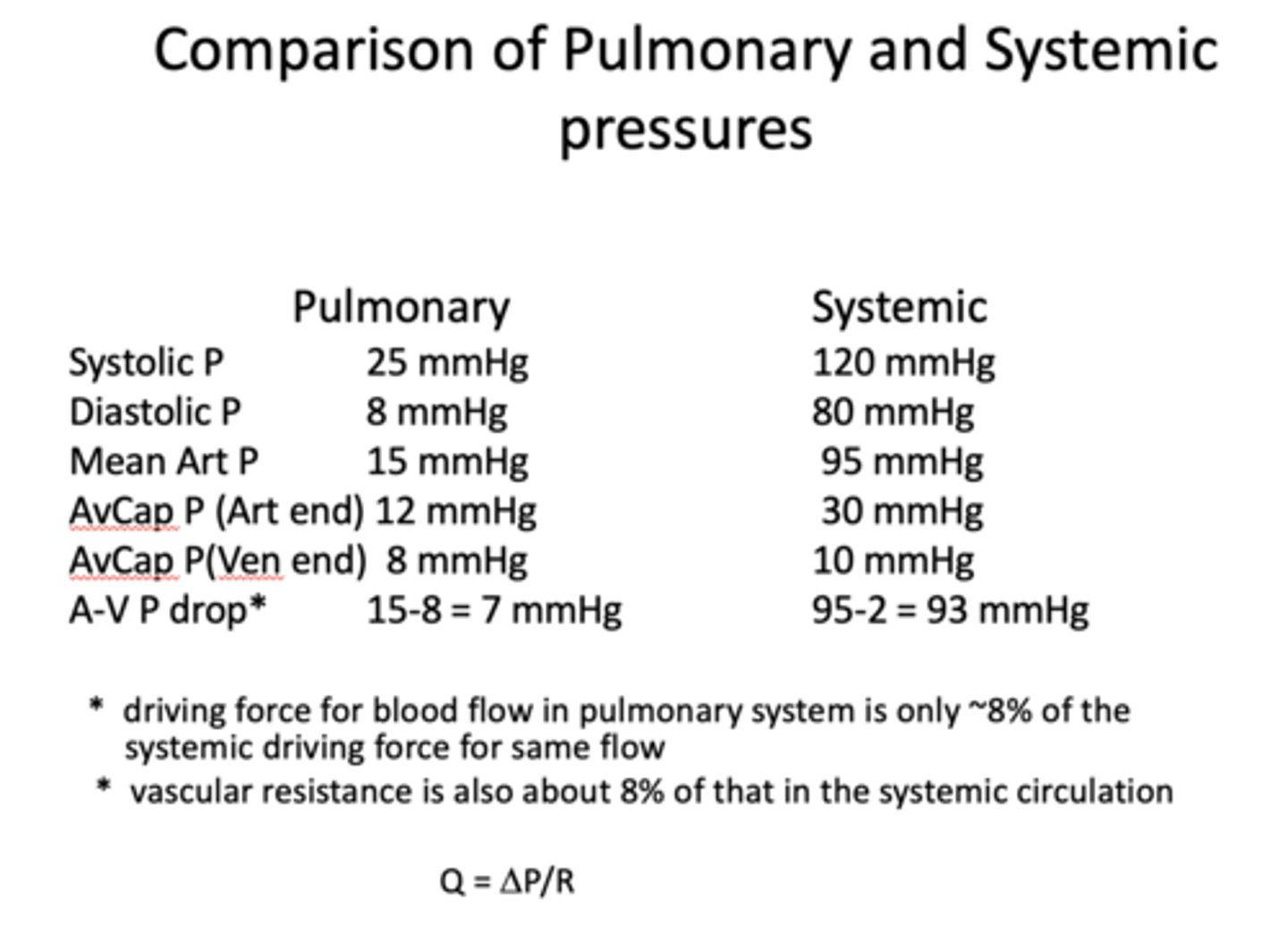
the systemic/circulatory is a _______ pressure system
high
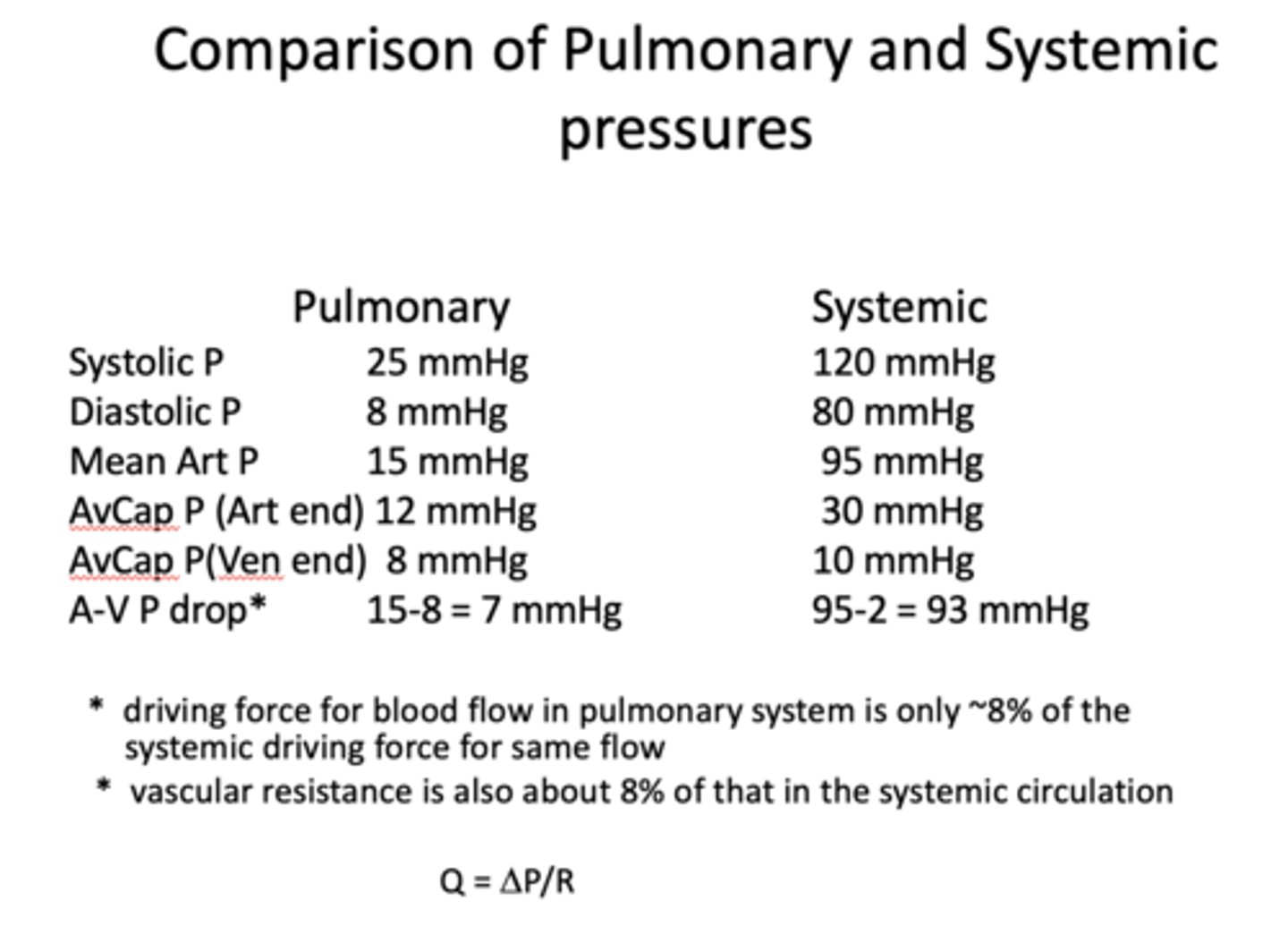
driving force for blood flow in pulmonary system is only __% of the systemic driving force for same flow
8%
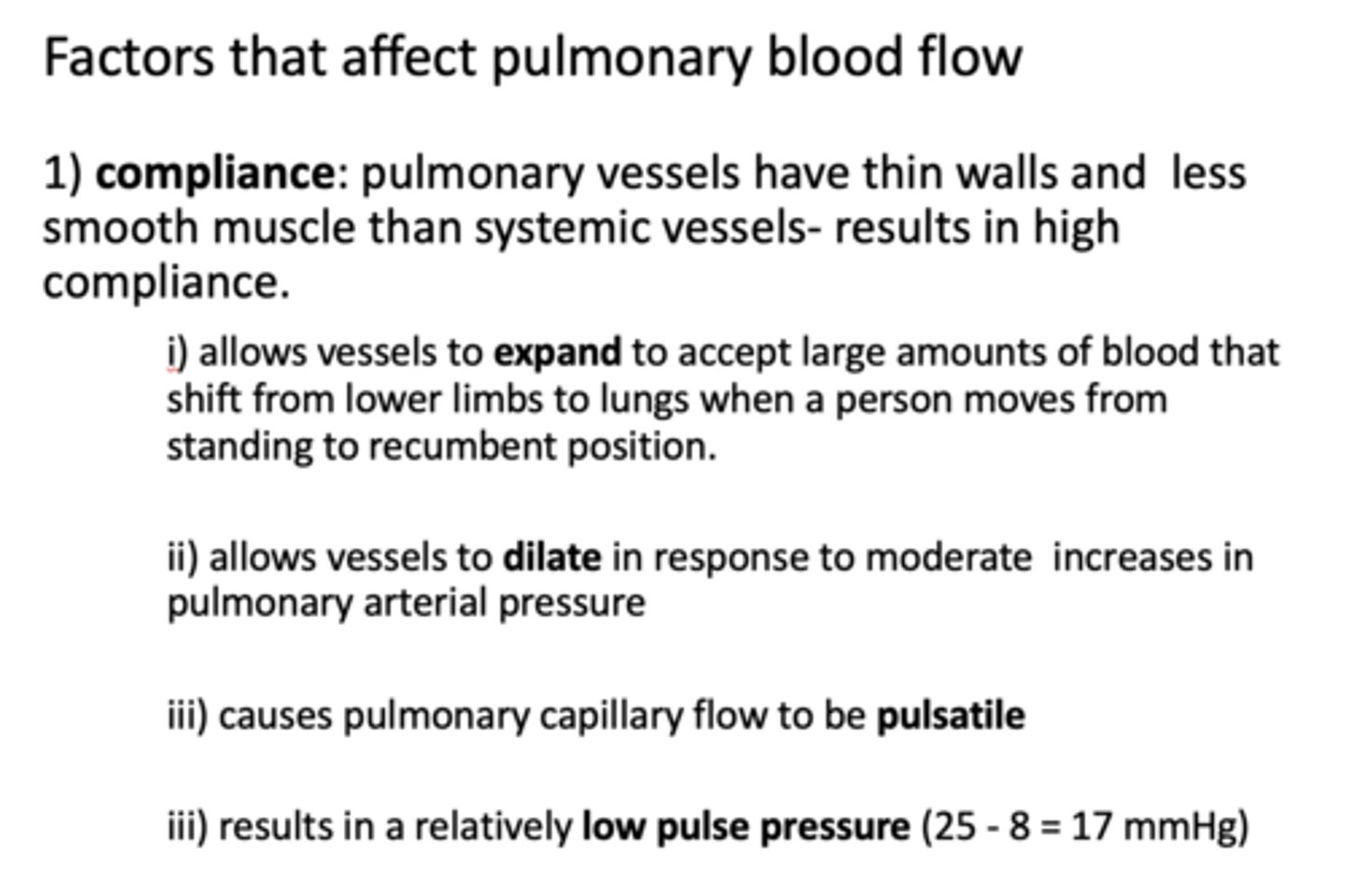
pulmonary vessels have thin walls and less smooth muscle than systemic vessels, which results in high _______
compliance
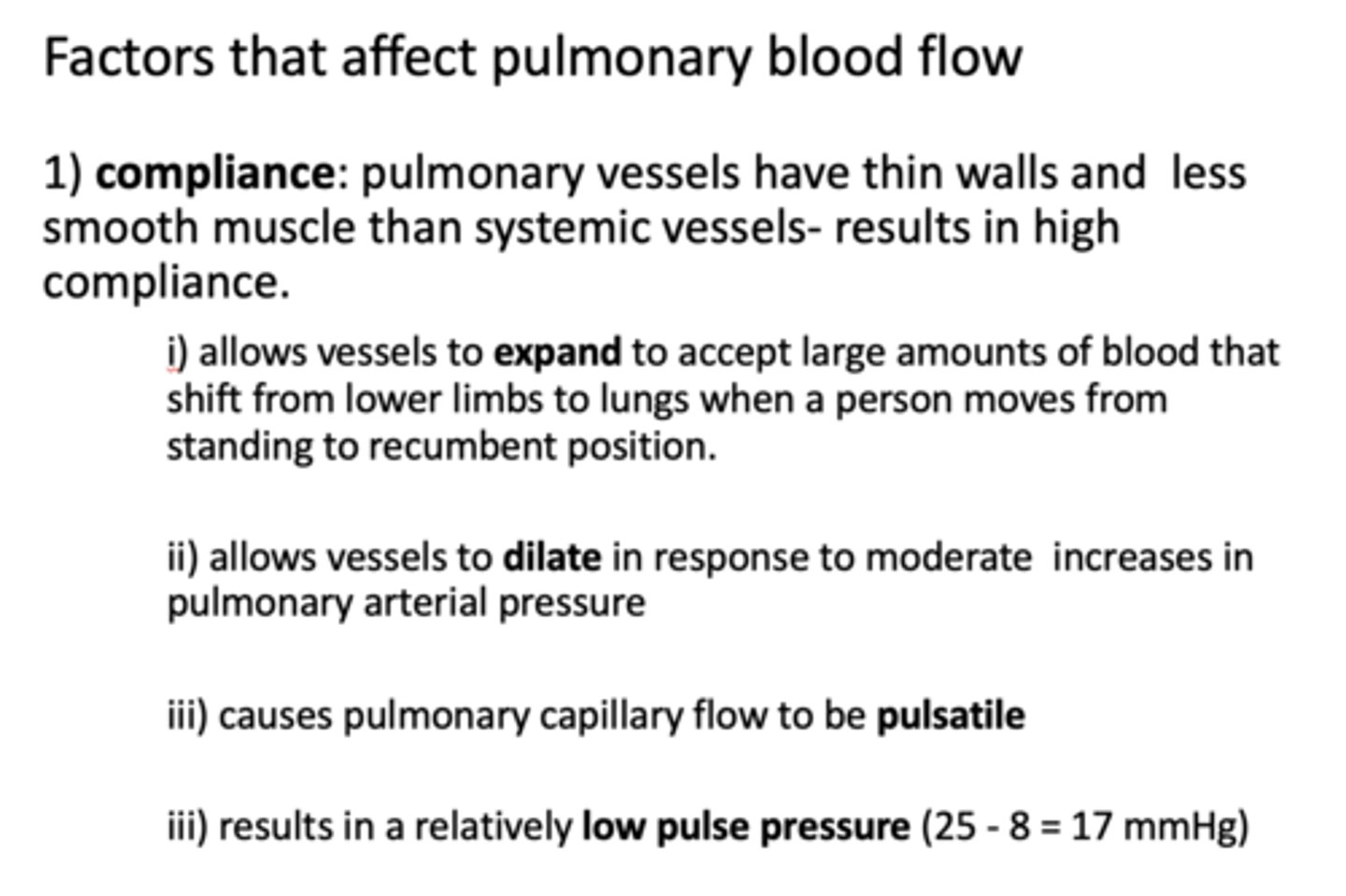
allows vessels to expand, dilate and flow to be pulsatile
compliance
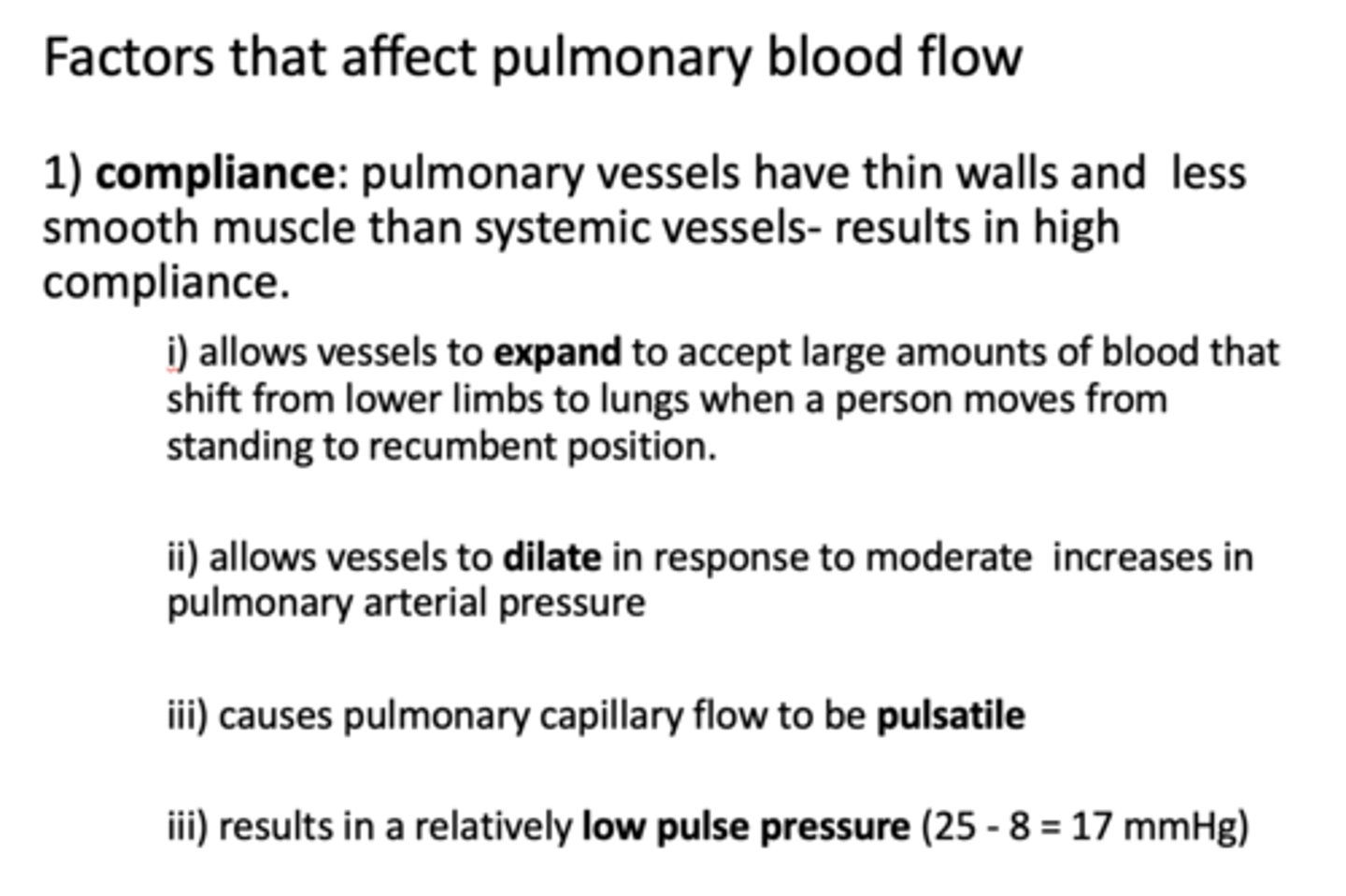
t/f: pulmonary capillary flow is pulsatile
true
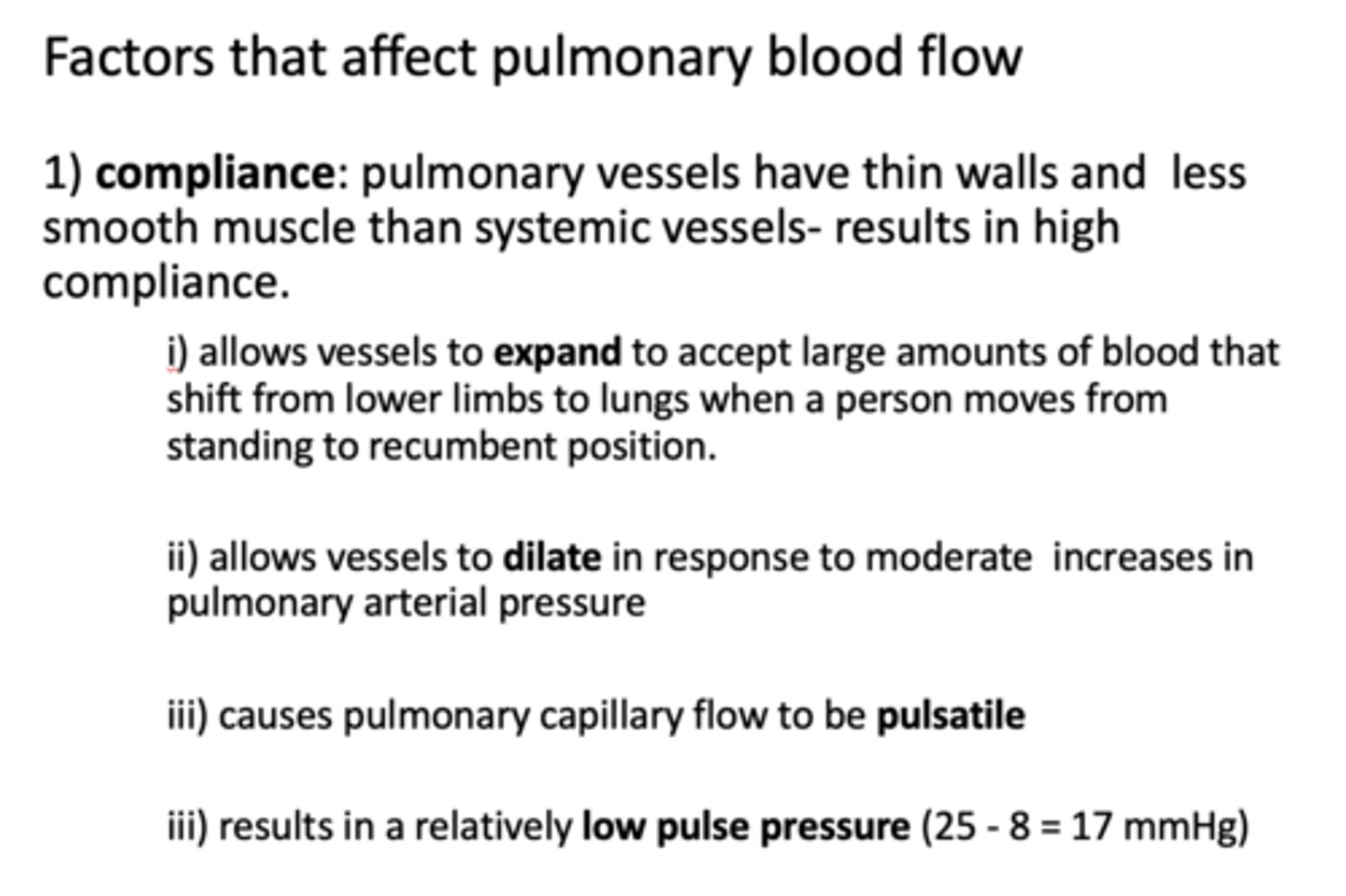
compliance results in a relatively ______ pulse pressure
low
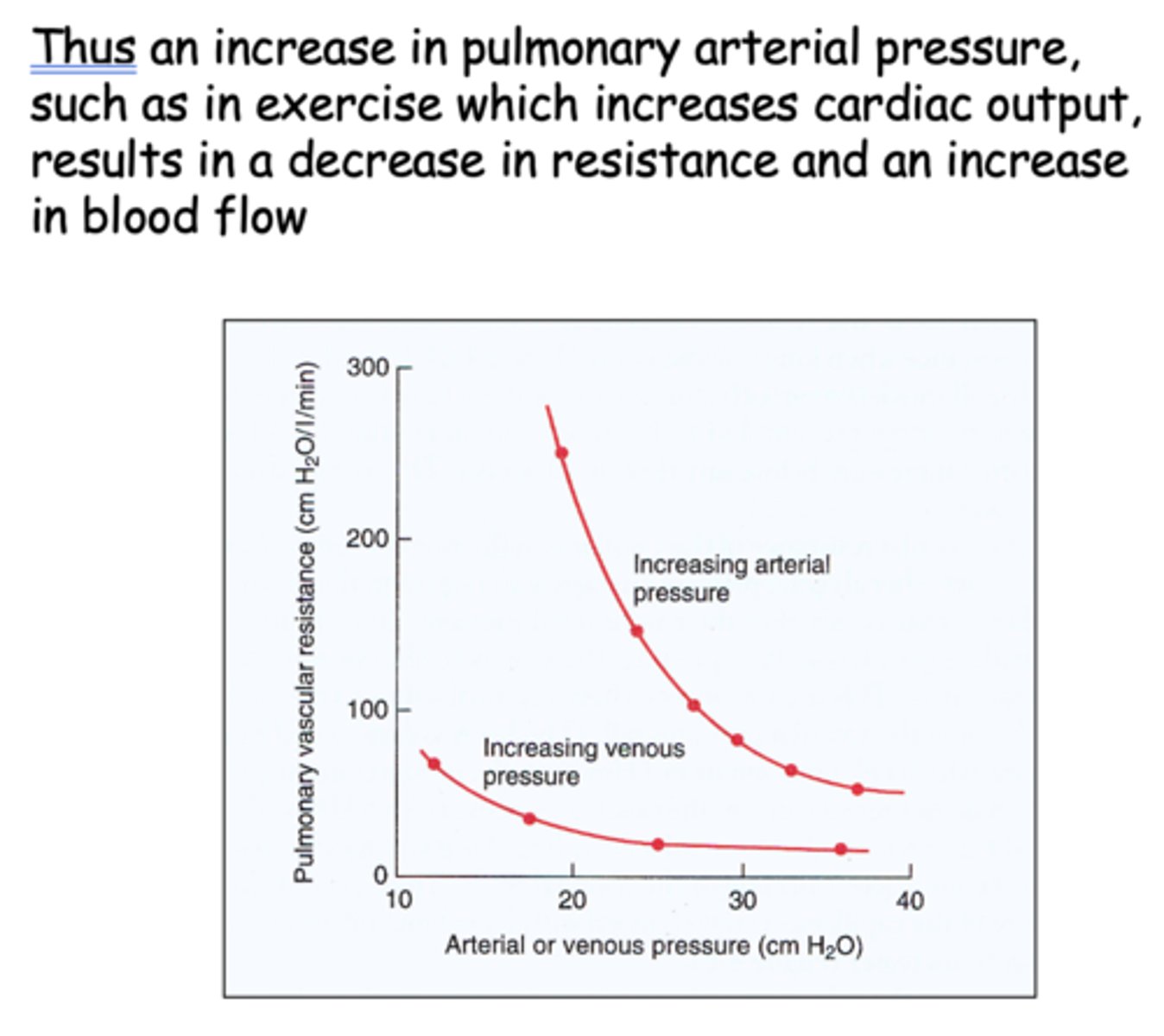
an increase in pulmonary arterial pressure results in a ________ in resistance
decrease
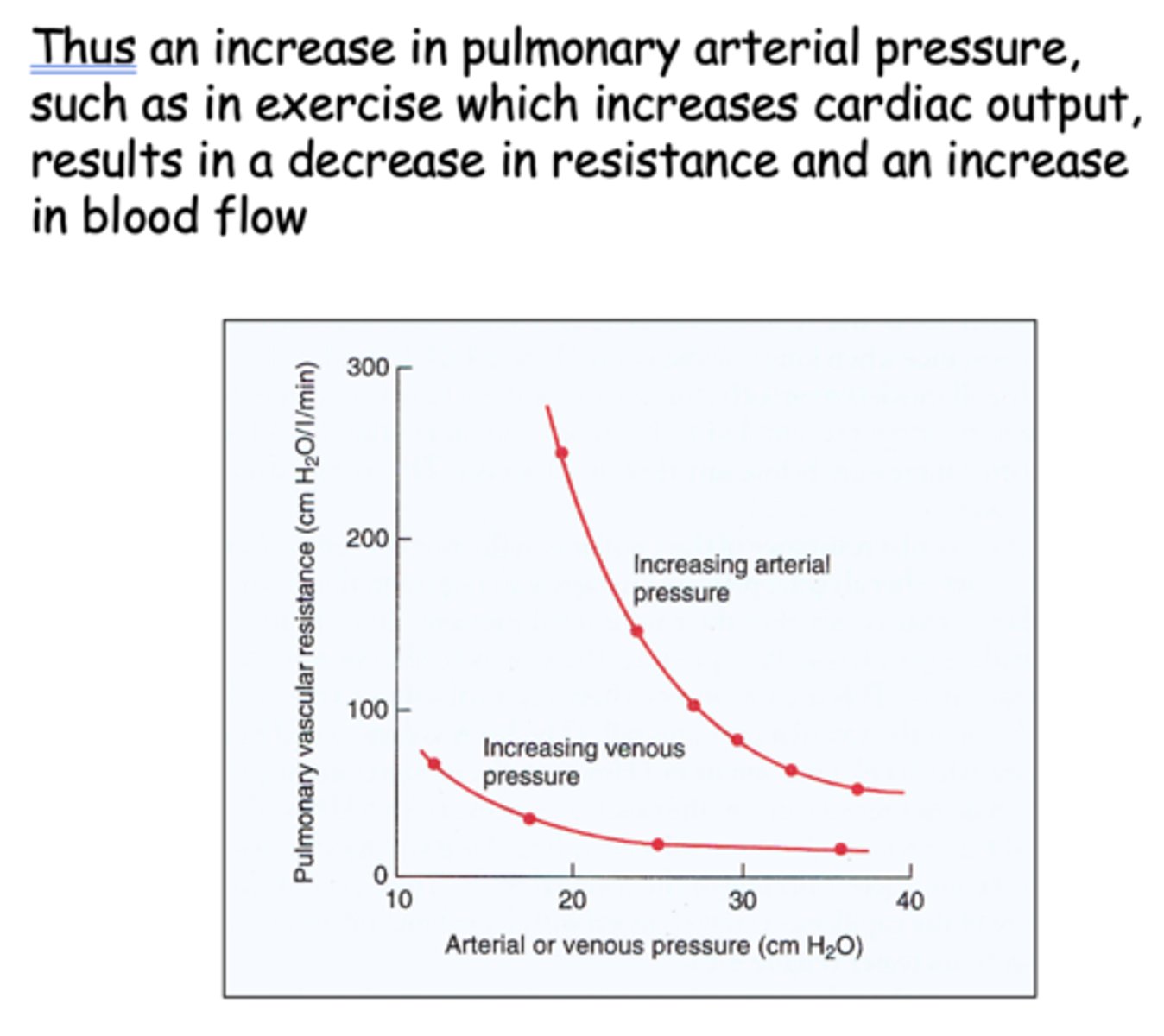
an increase in pulmonary arterial pressure results in a __________ in blood flow
increase
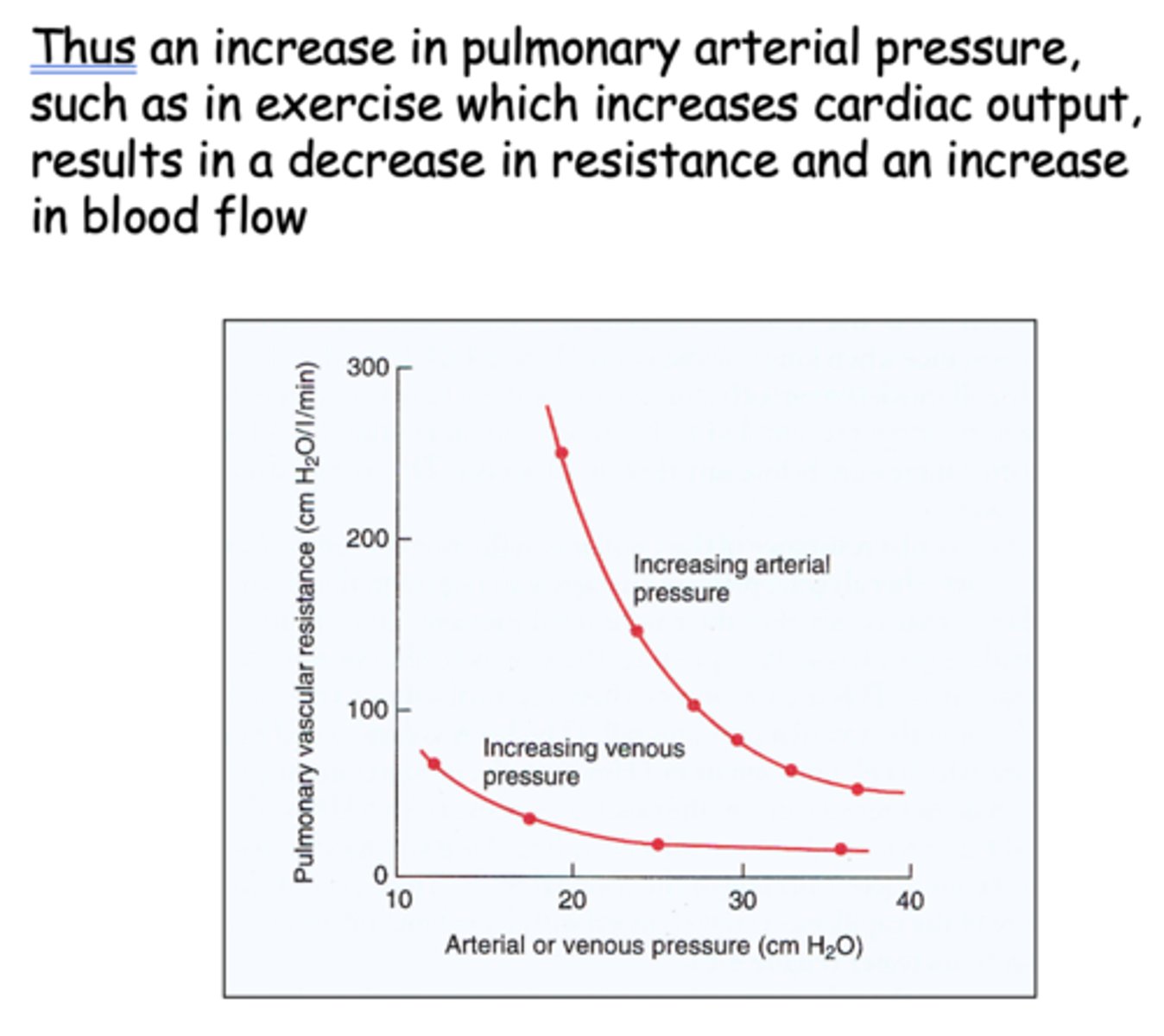
an increase in pulmonary arterial pressure results in a __________ in cardiac output
increase
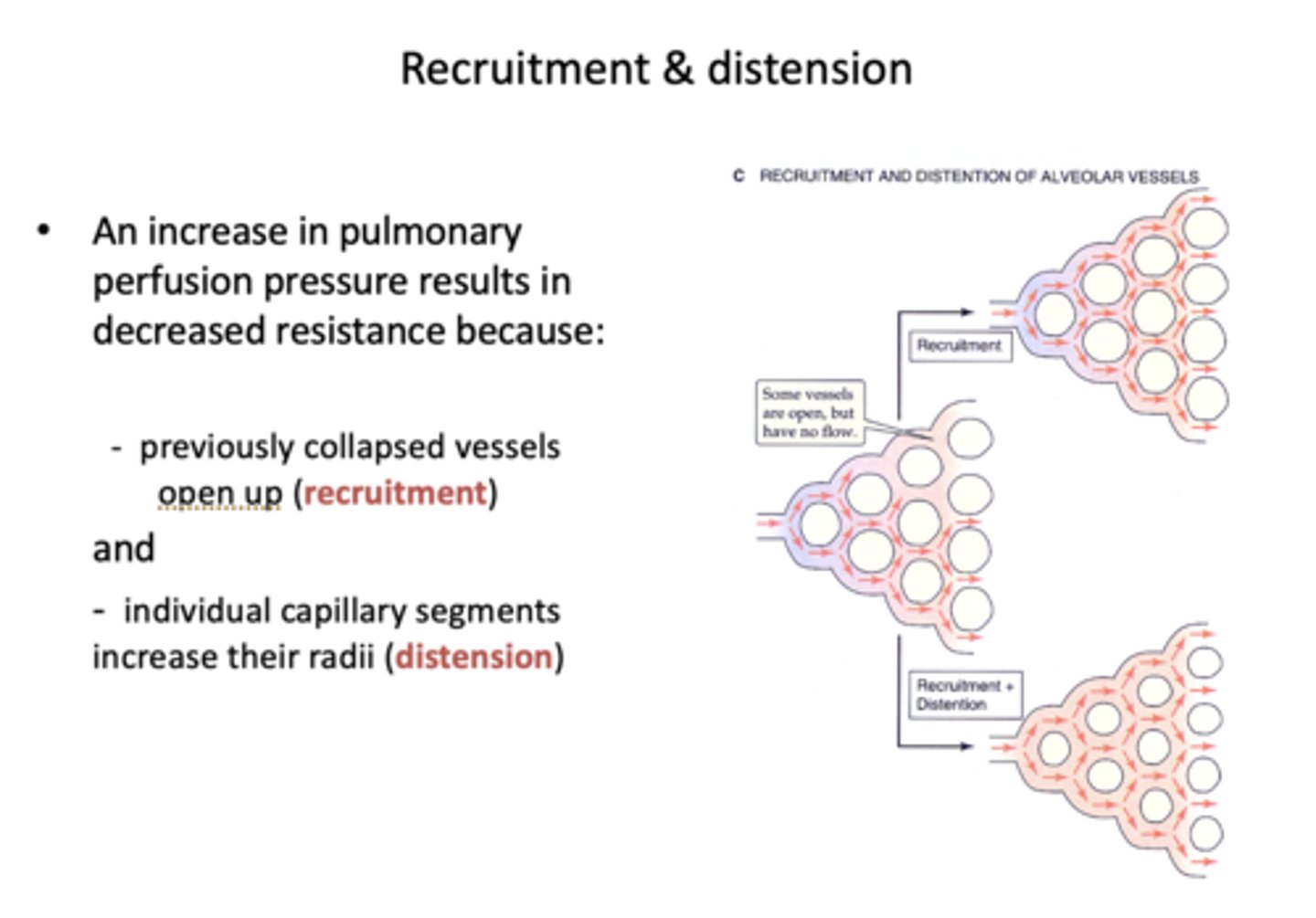
An increase in pulmonary perfusion pressure results in decreased resistance because of what factors?
- Recruitment
- Distension
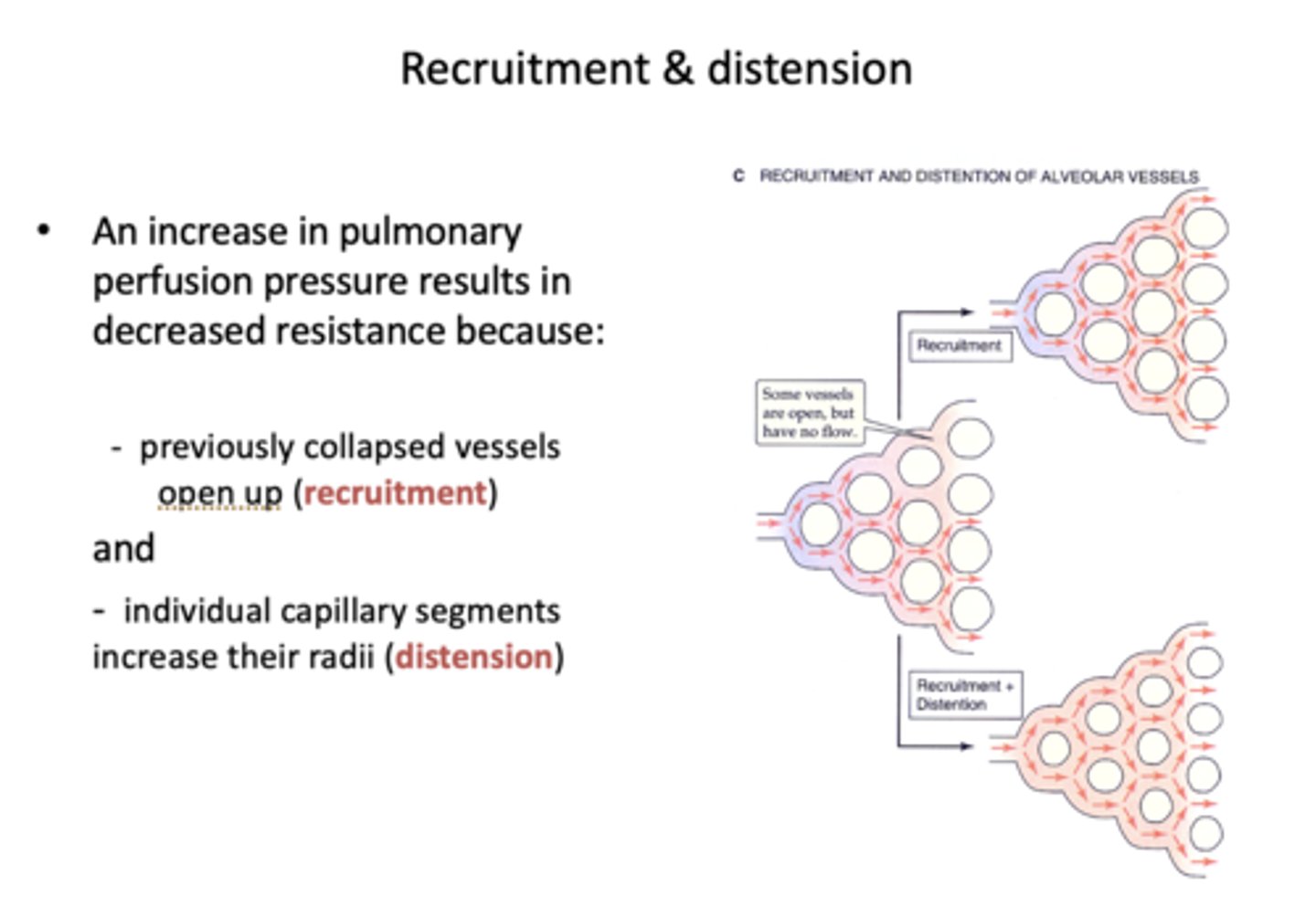
Define the following:
When previously collapsed vessels open up with an increase in pulmonary perfusion pressure:
Recruitment
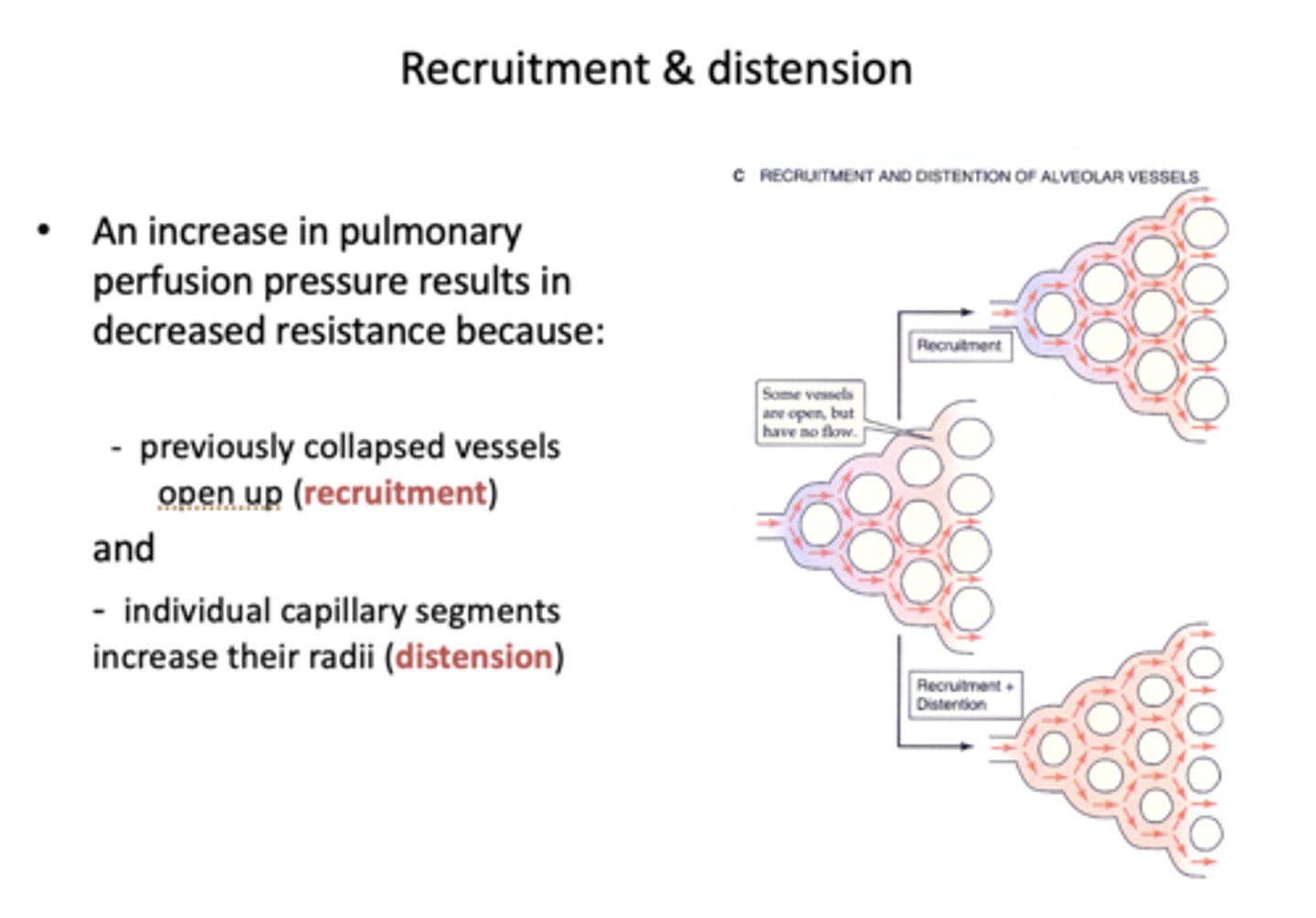
Define the following:
Individual capillary segments increase their radii
Distension
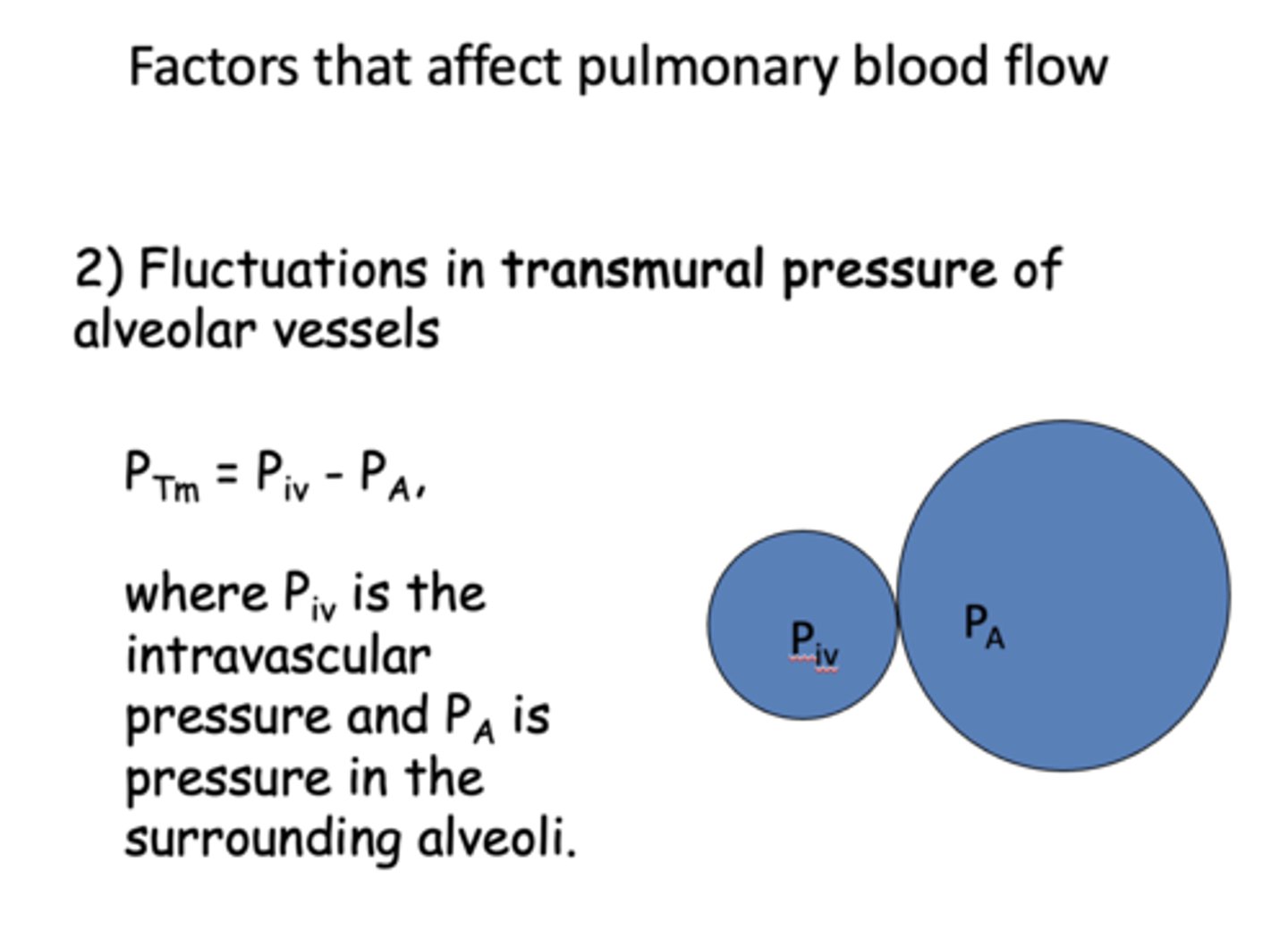
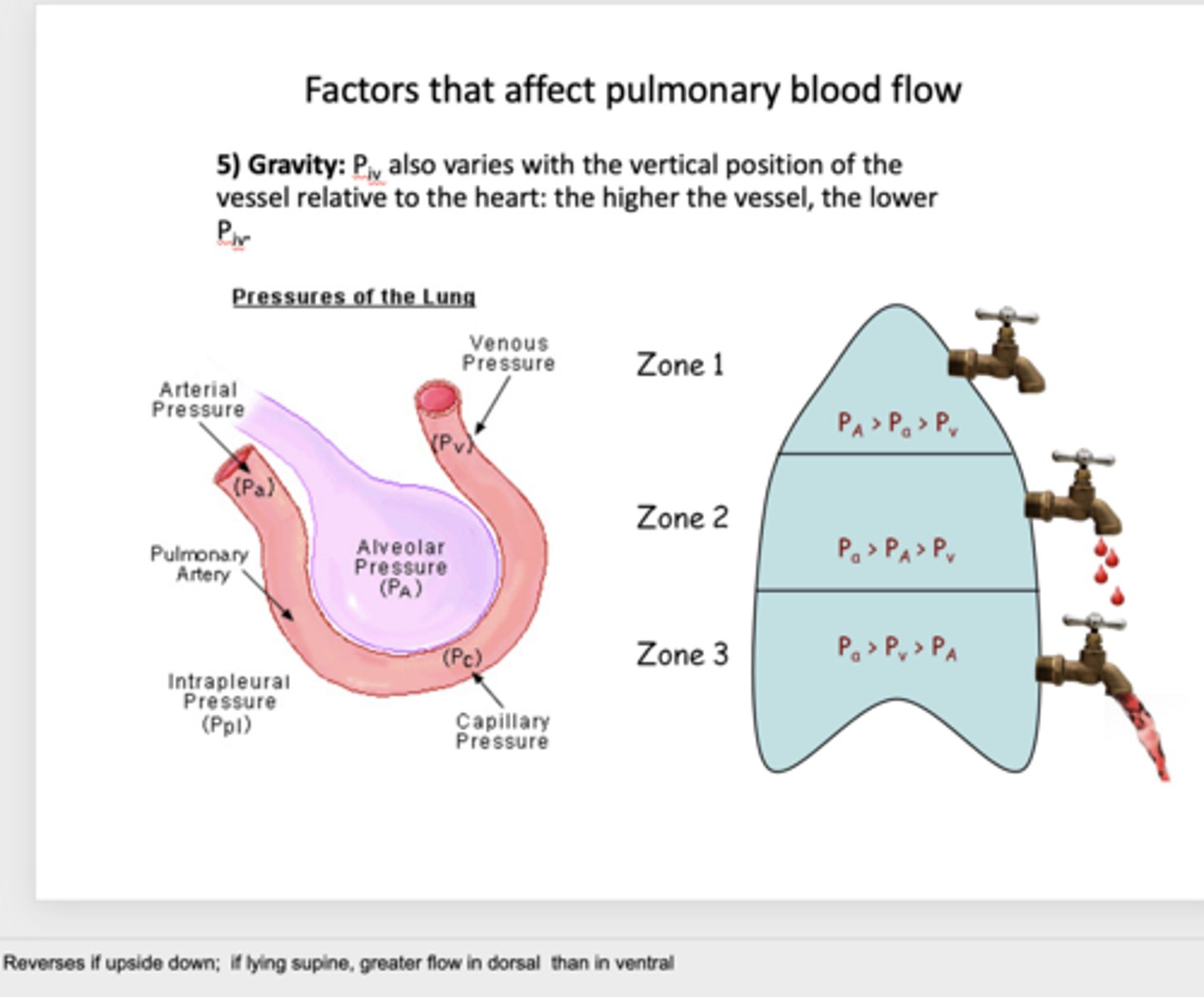
What are 5 factors that affect pulmonary blood flow:
- Compliance
- Transmural pressure
- Lung volume
- Hypoxic vasoconstriction
- Gravity
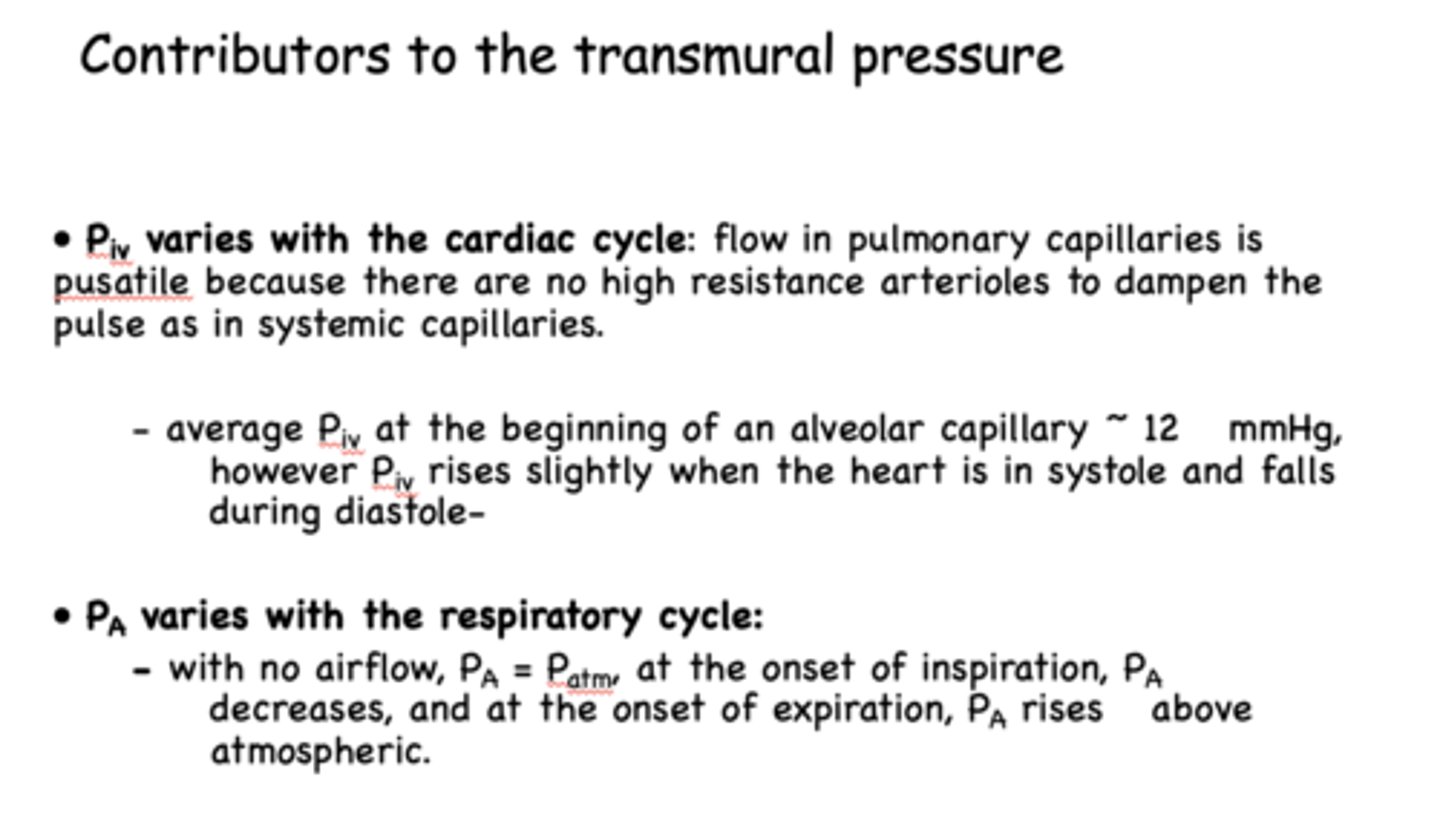
pulmonary intravascular pressure (Piv) varies with the _____ cycle
cardiac
alveolar pressure (PA) varies with the ________ cycle
respiratory

flow in __________ capillaries is pulsatile because there are no high resistance arterioles to dampen the pulse
pulmonary
with no airflow, alveolar pressure will equal _______
atmospheric pressure
t/f: cardiac and respiratory cycles are synchronous
false
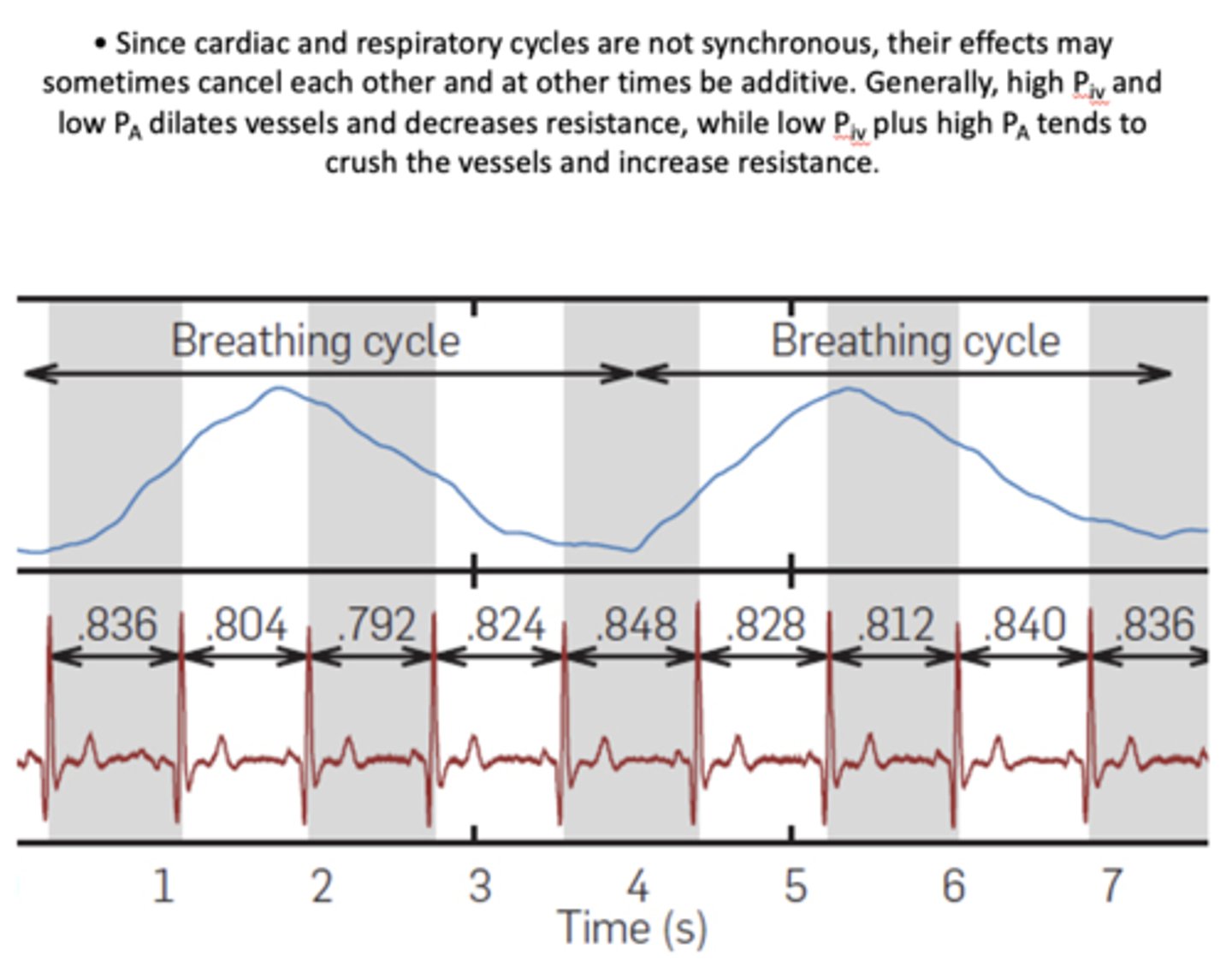
at the onset of inspiration, PA ______
decreases
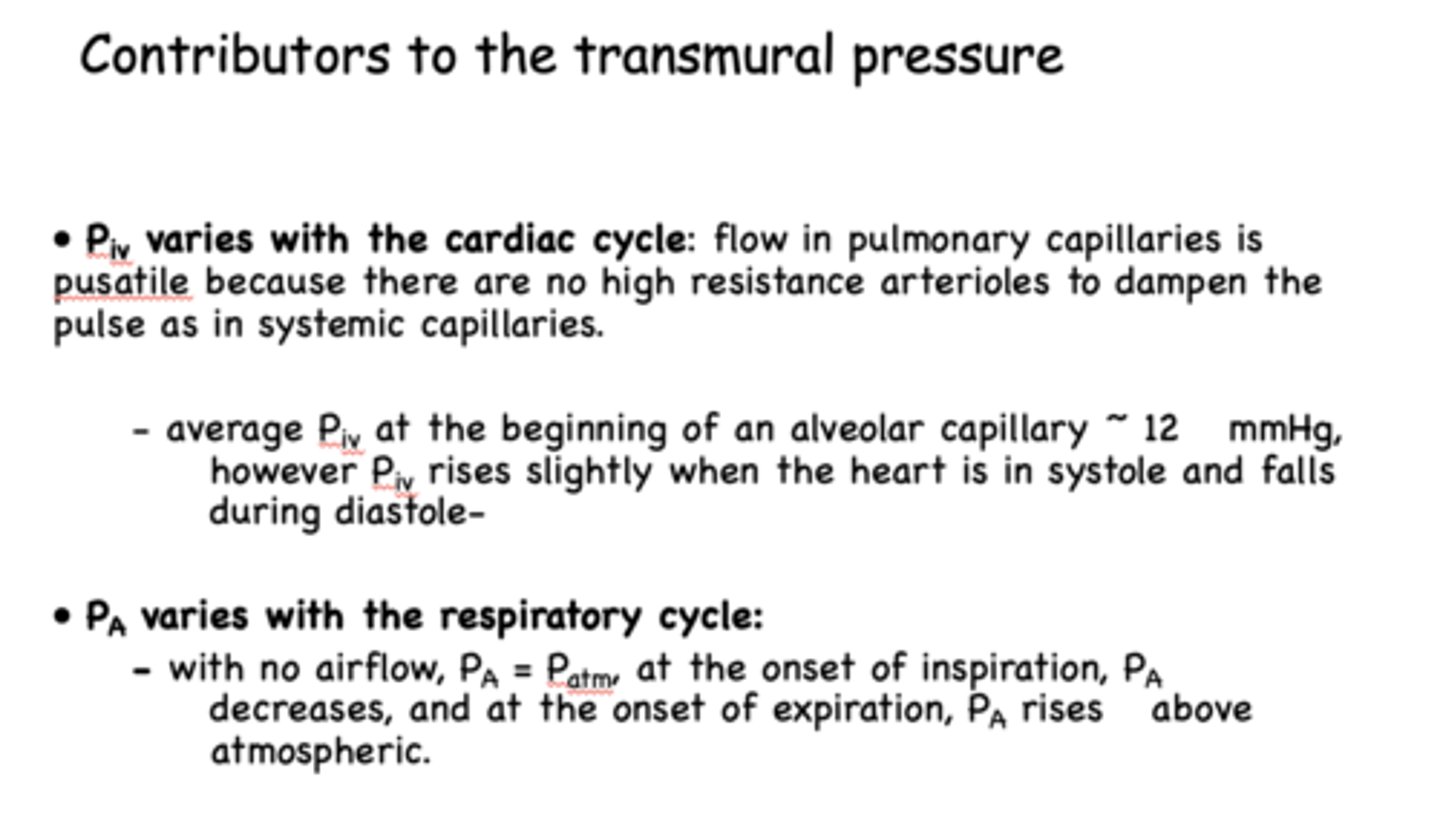
at the onset of expiration, PA ______
increases above atmospheric
high P(iv) and low Pa does what in terms of vessels and resistance?
dilate vessels, decrease resistance
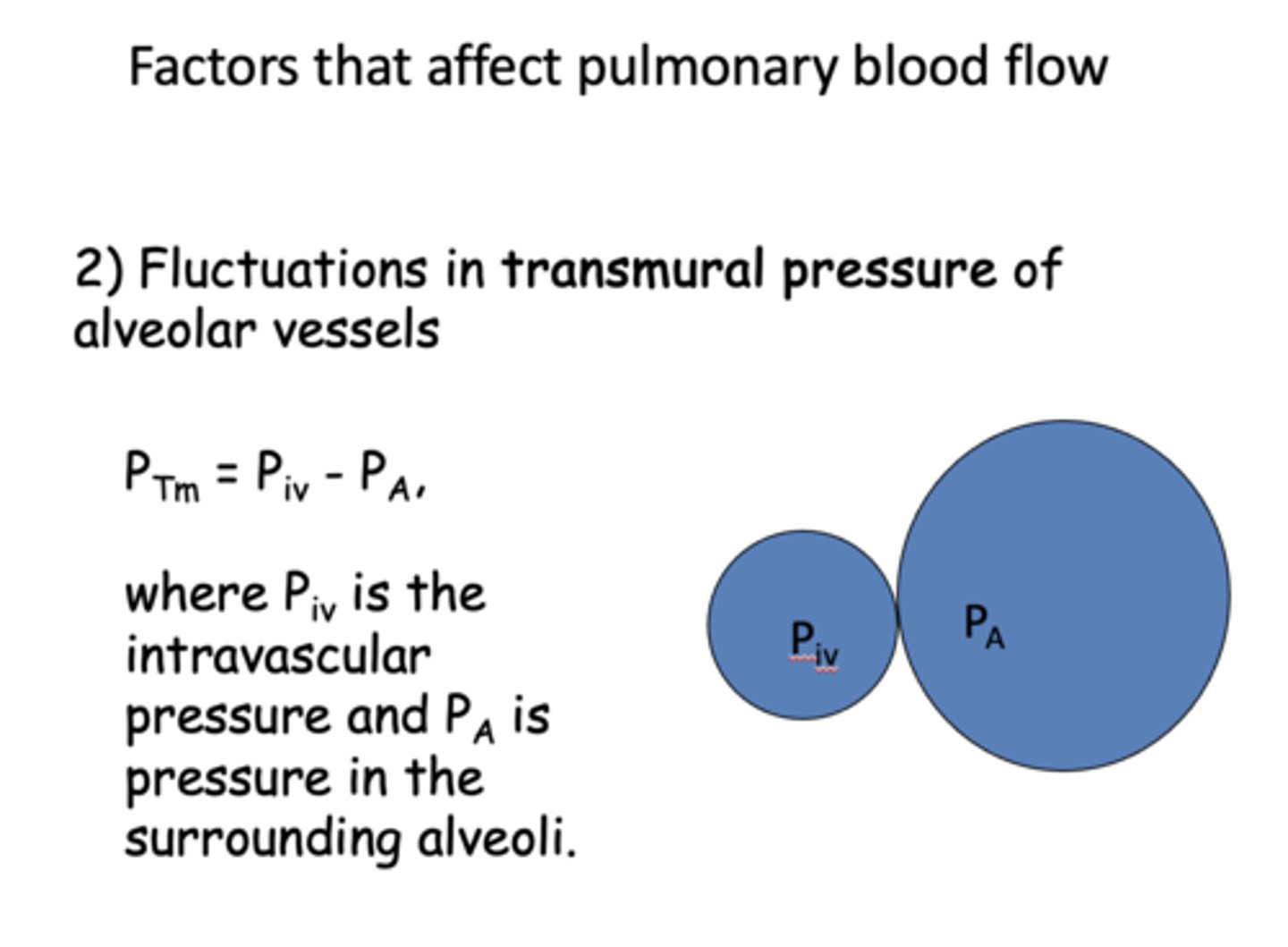
low P(iv) and high Pa does what in terms of vessels and resistance?
crush vessels, increase resistance
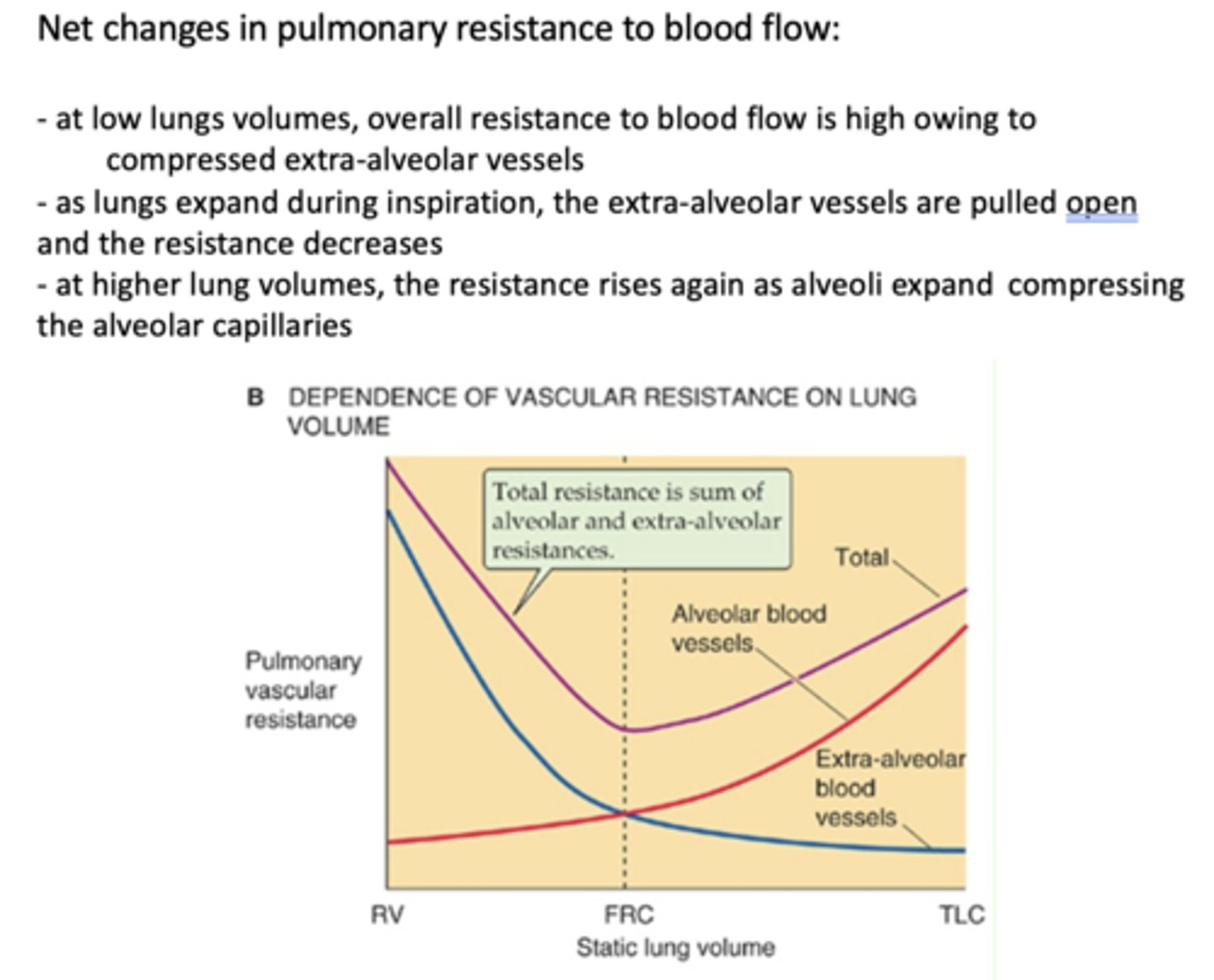
alveolar vessel resistance _____ when lung volume increases
increase
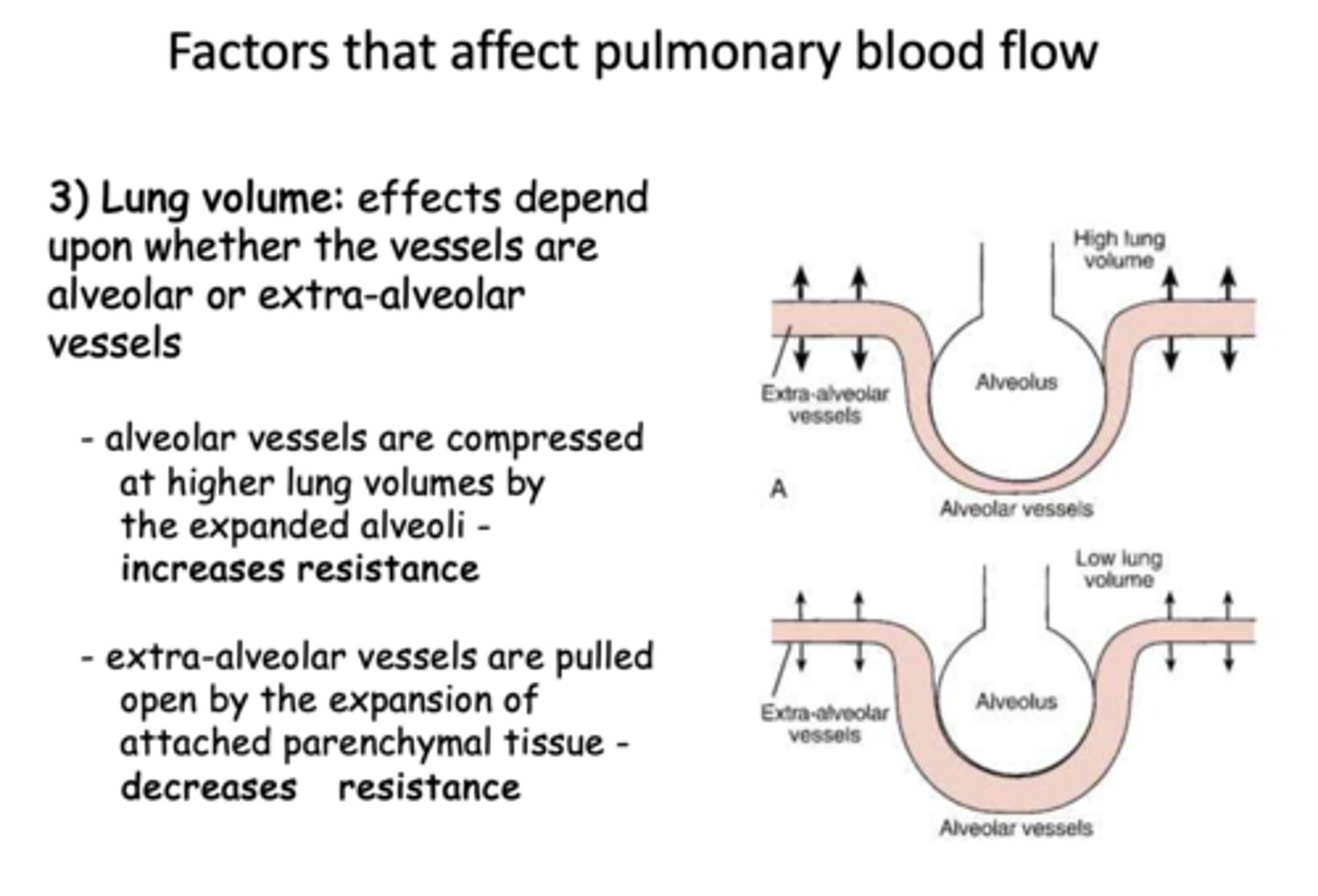
what causes alveolar vessel resistance to increase when lung volume increases?
compression by expanded alveoli
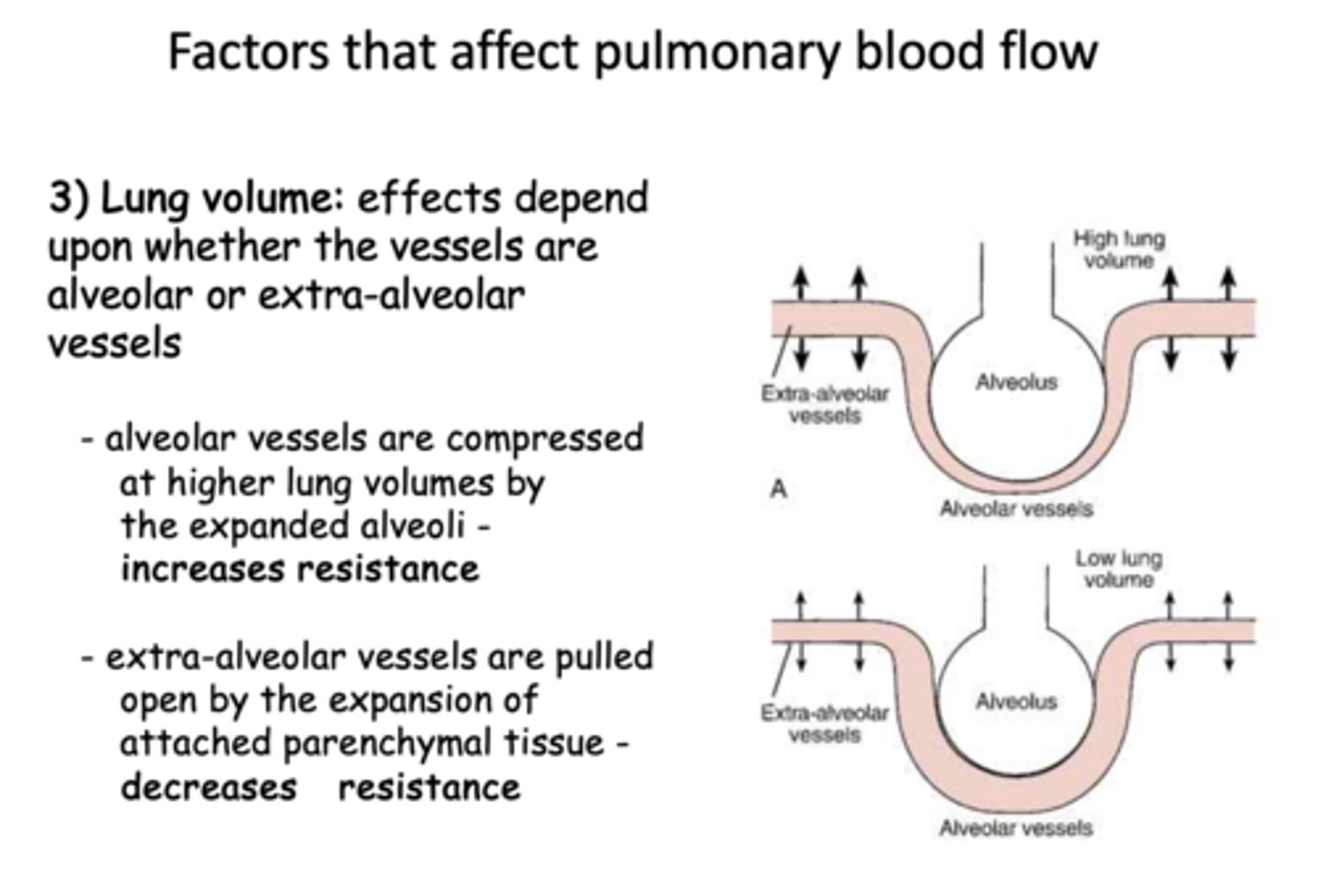
extra-alveolar vessel resistance ______ when lung volume increases
decrease
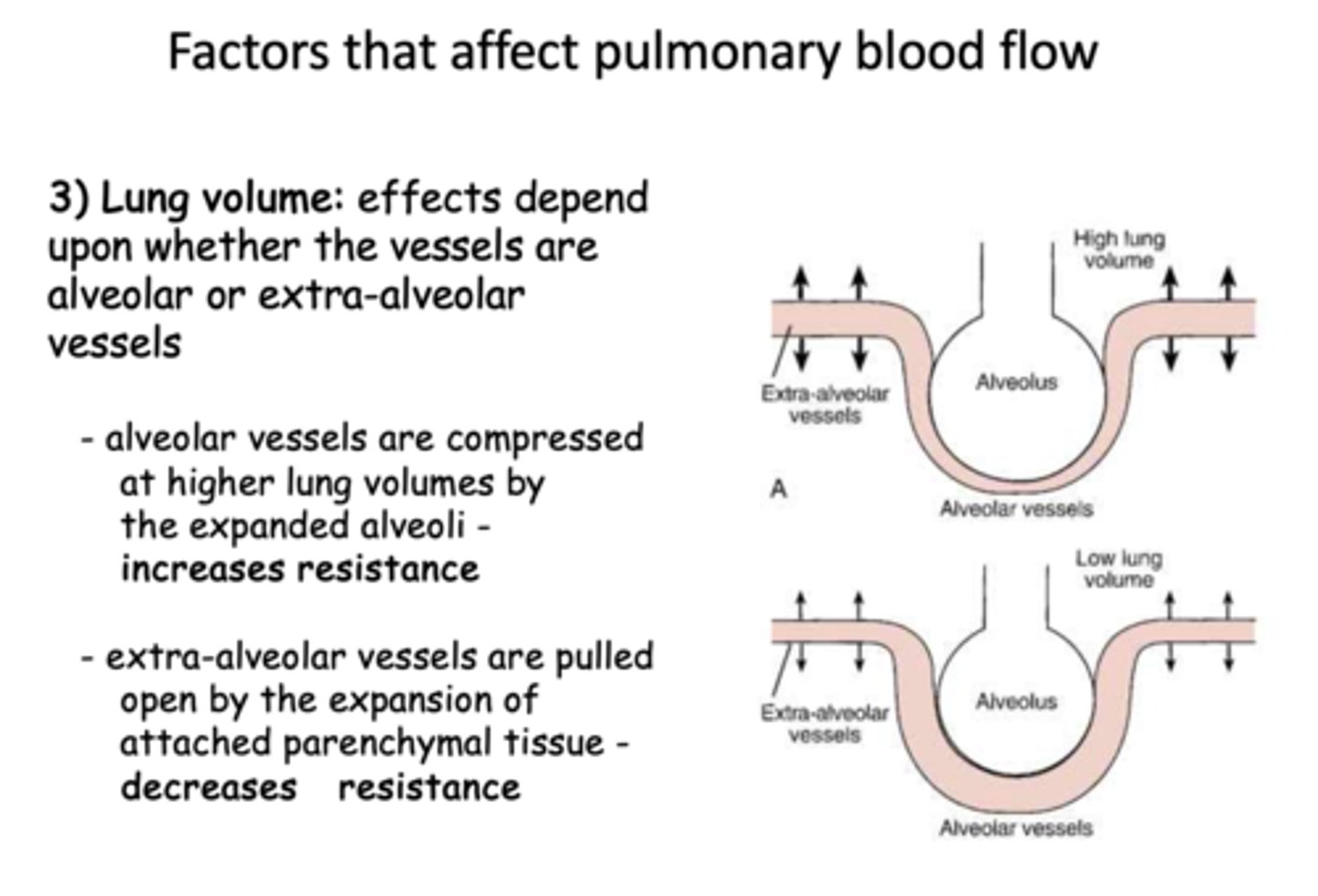
at low lung volumes, alveolar vessel resistance is
decreased
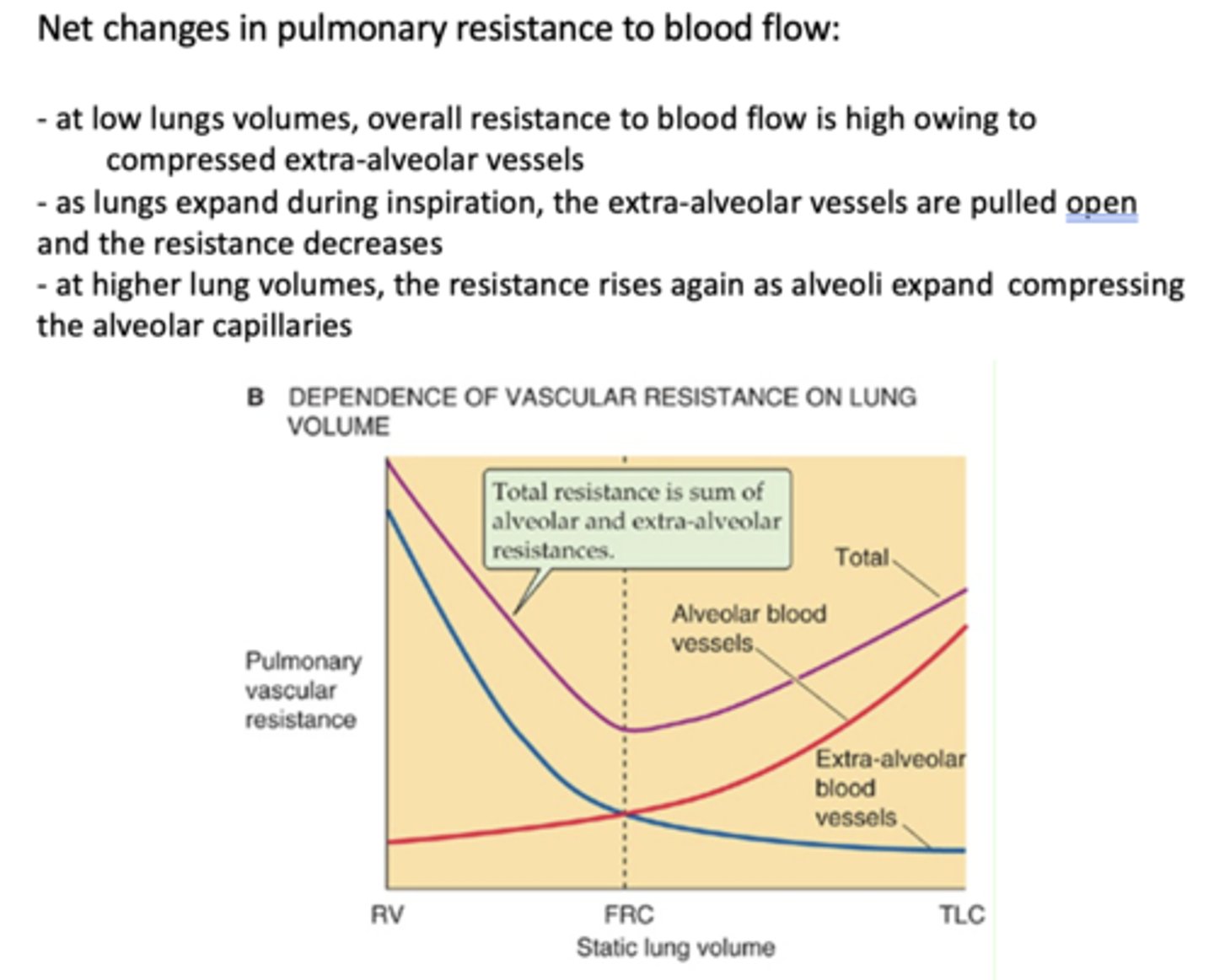
at low lung volumes, extra-alveolar resistance is
increased
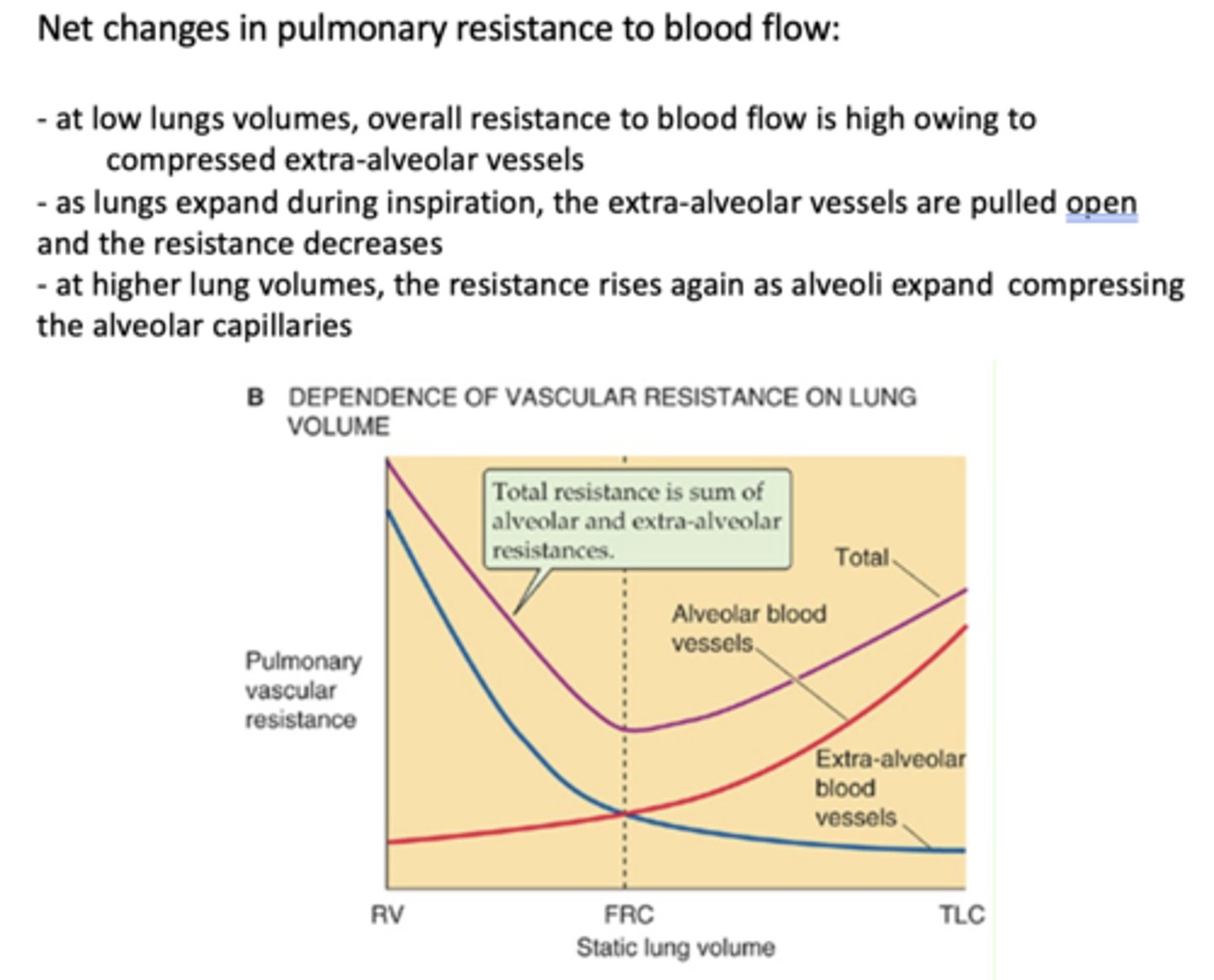
what causes extra-alveolar vessel resistance to decrease when lung volume increases?
pulling open by the expansion of attached parenchymal tissue
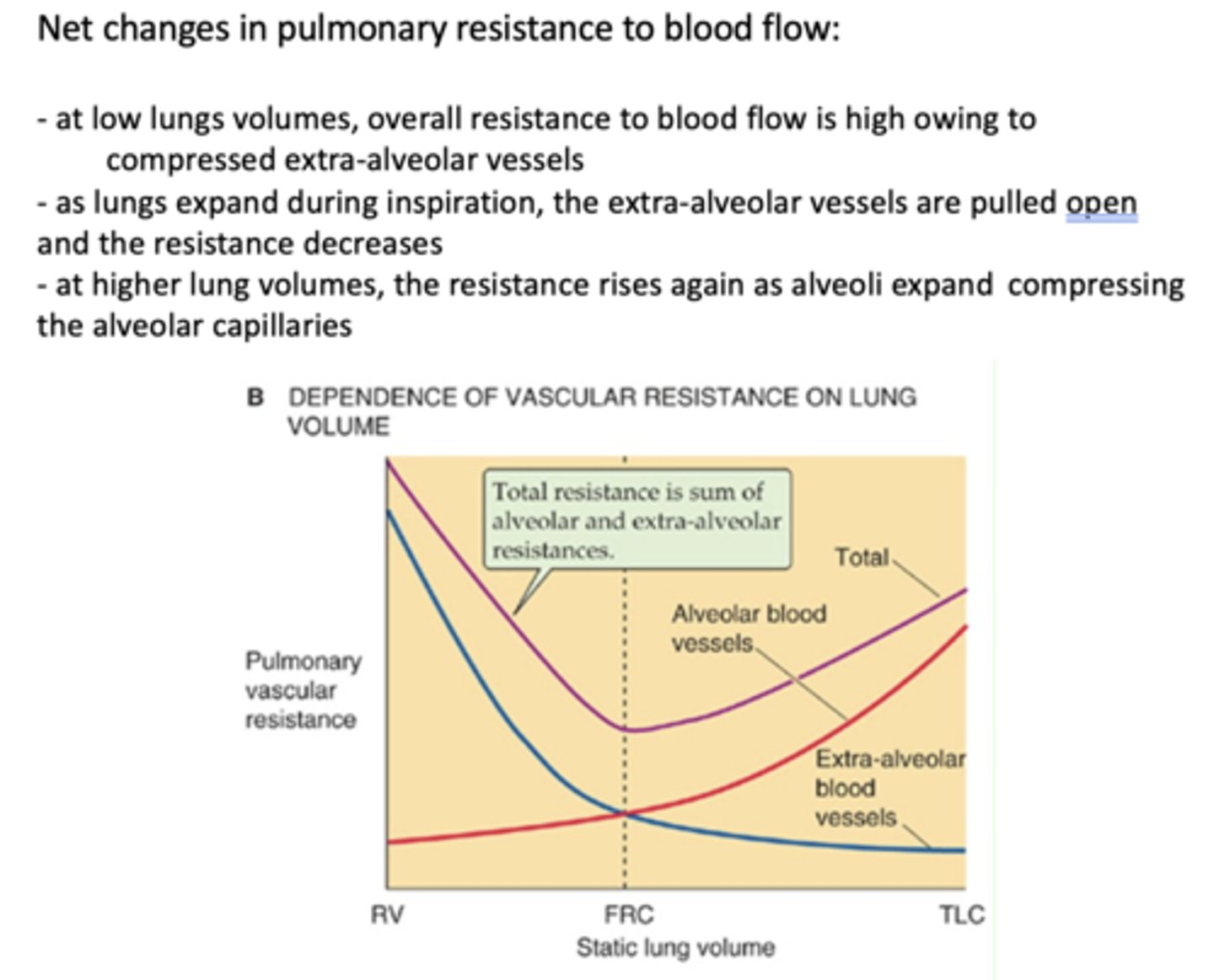
at low lungs volumes, overall resistance to blood flow is ____
high
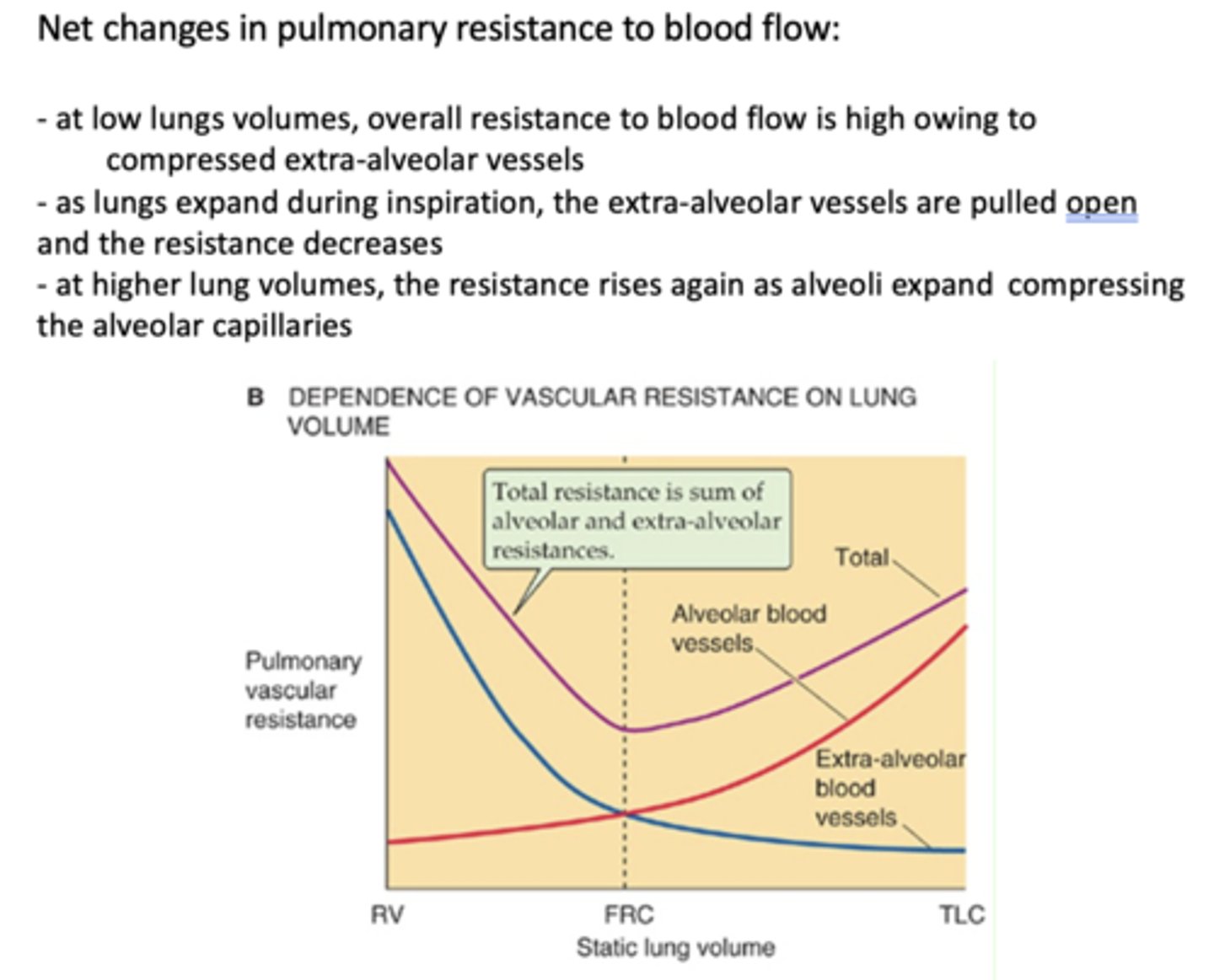
at low lungs volumes, overall resistance to blood flow is high owing to _______
compressed extra-alveolar vessels
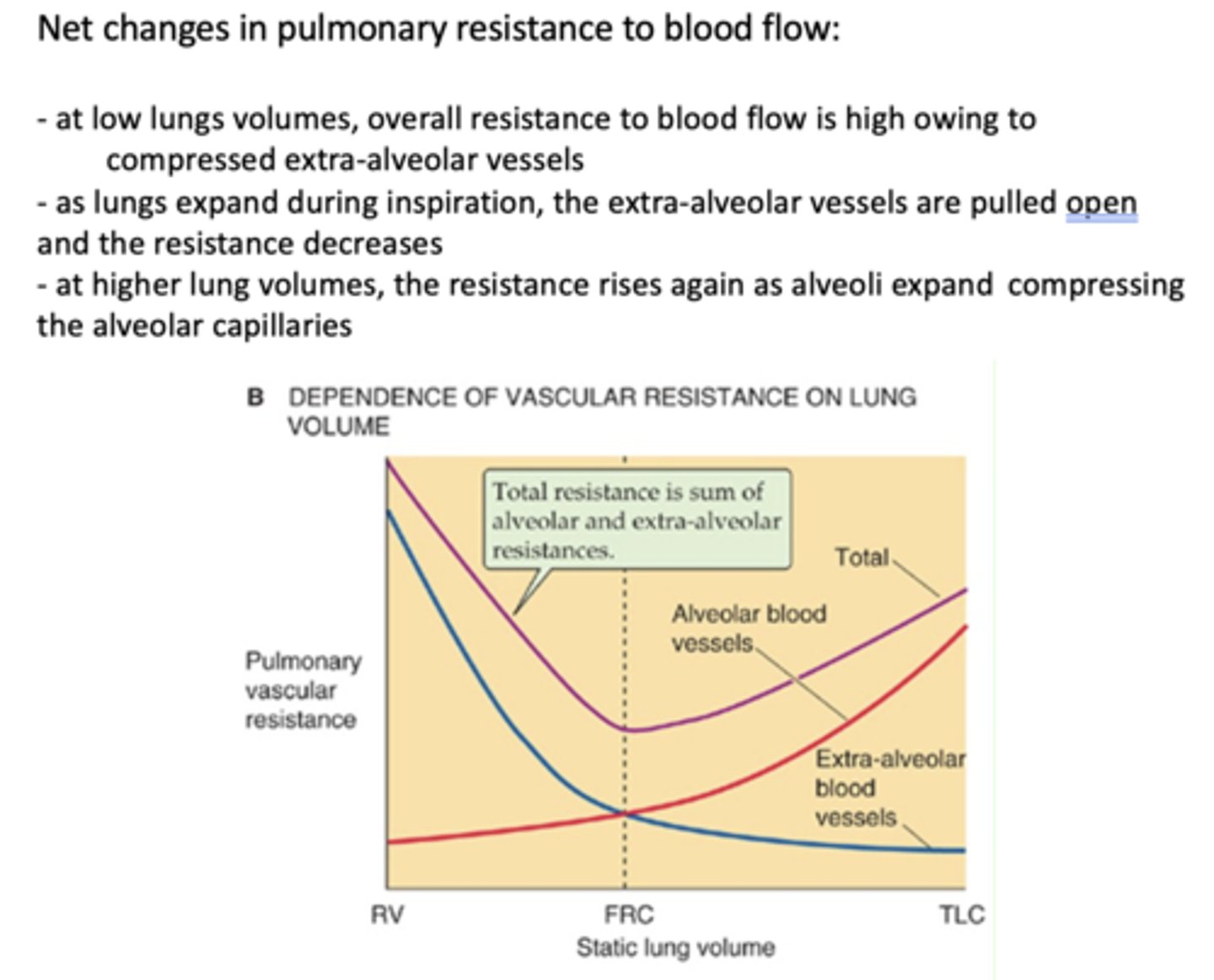
at higher lung volumes, the resistance rises again owing to ______
compression by expanded alveoli
hypoxic vasoconstriction will occur when PAO2 ( alveolar O2 pressure) drops below _____ and pulmonary vessels constrict
60 mmHG
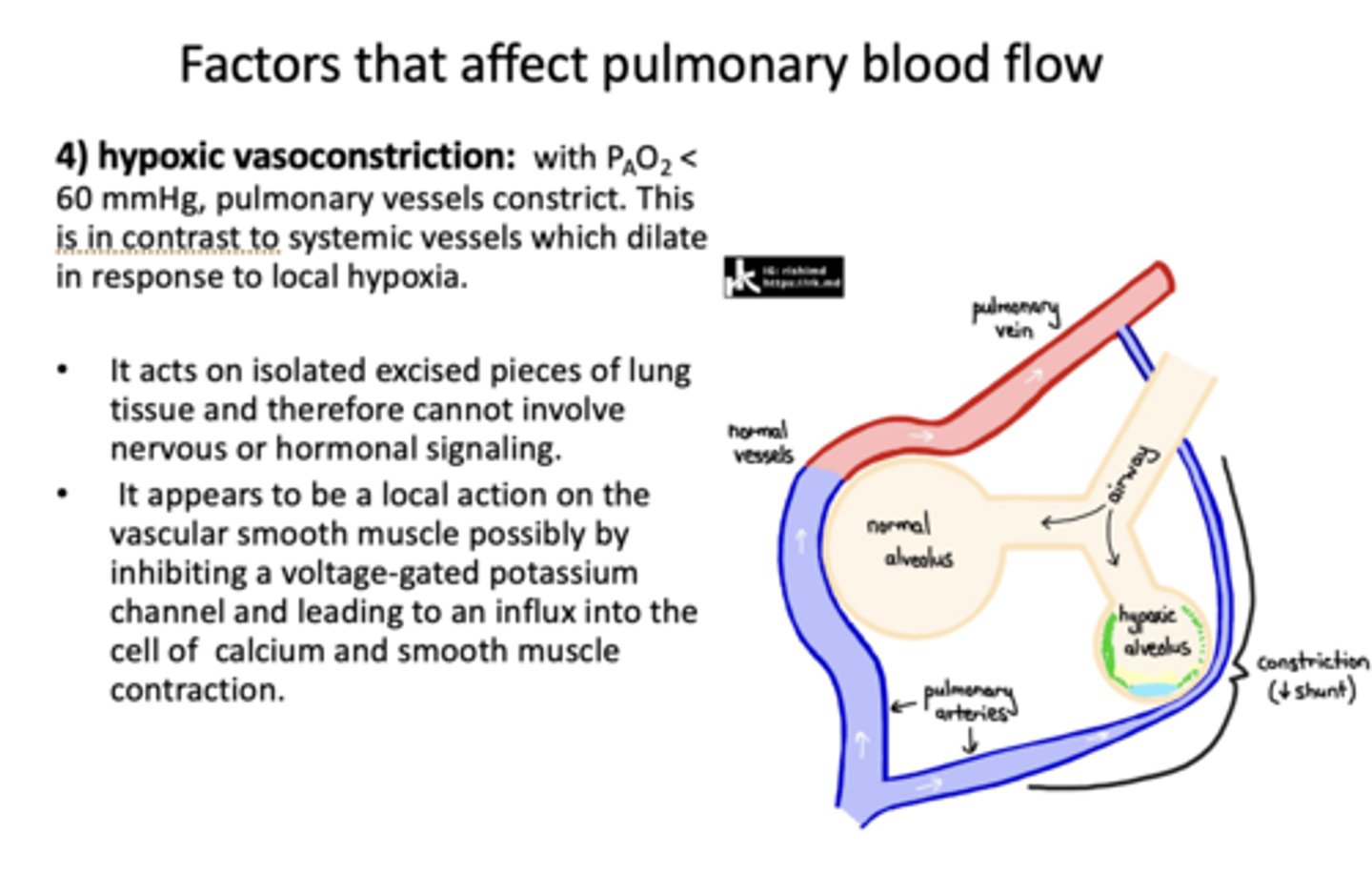
t/f: hypoxic vasoconstriction acts on isolated excised pieces of lung tissue and cannot involve nervous or hormonal signaling
true
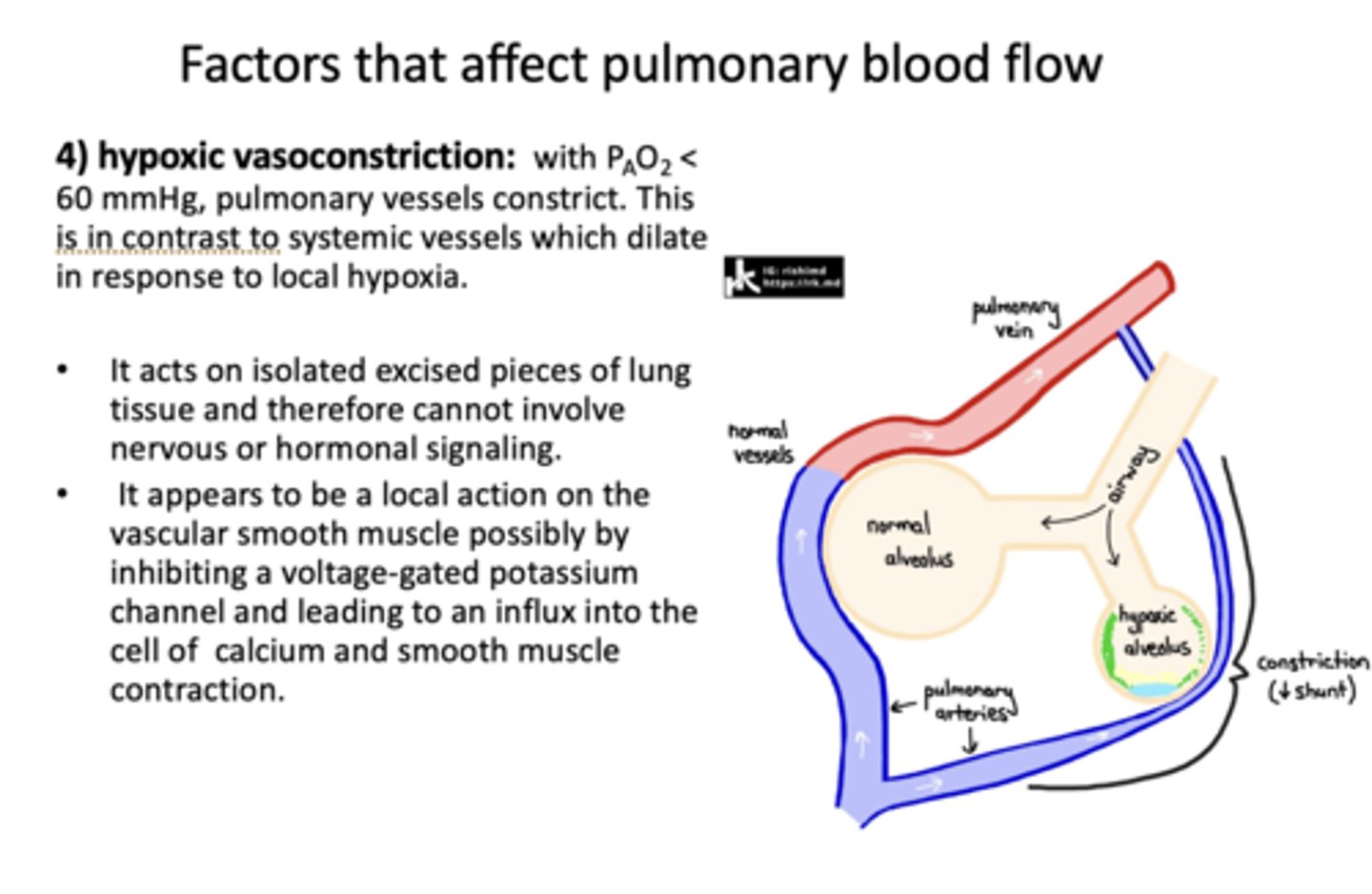
a local action on vascular smooth muscle possibly by inhibiting a voltage-gated potassium channel and leading to an influx into the cell of calcium and smooth muscle contraction
hypoxic vasoconstriction
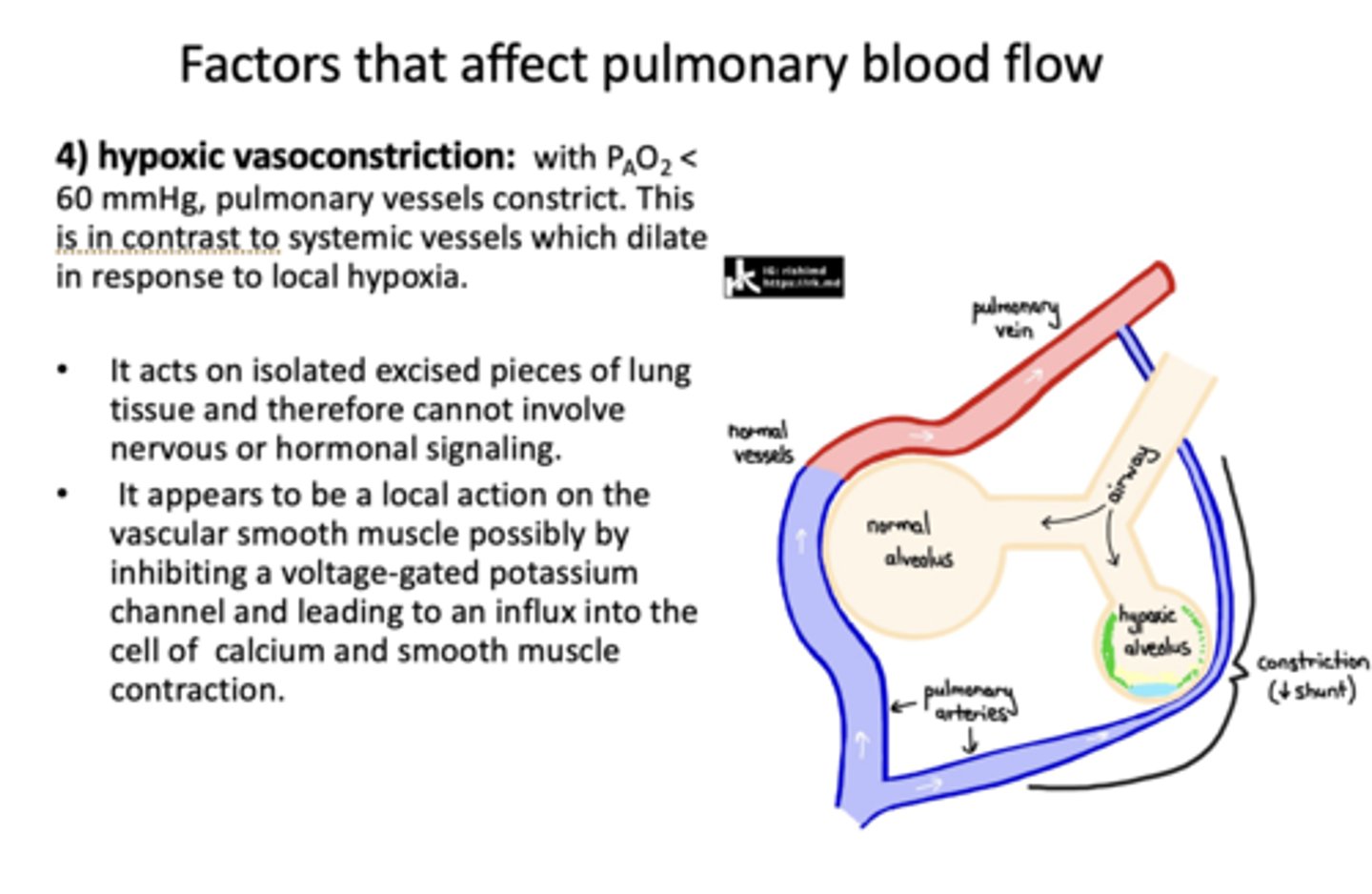
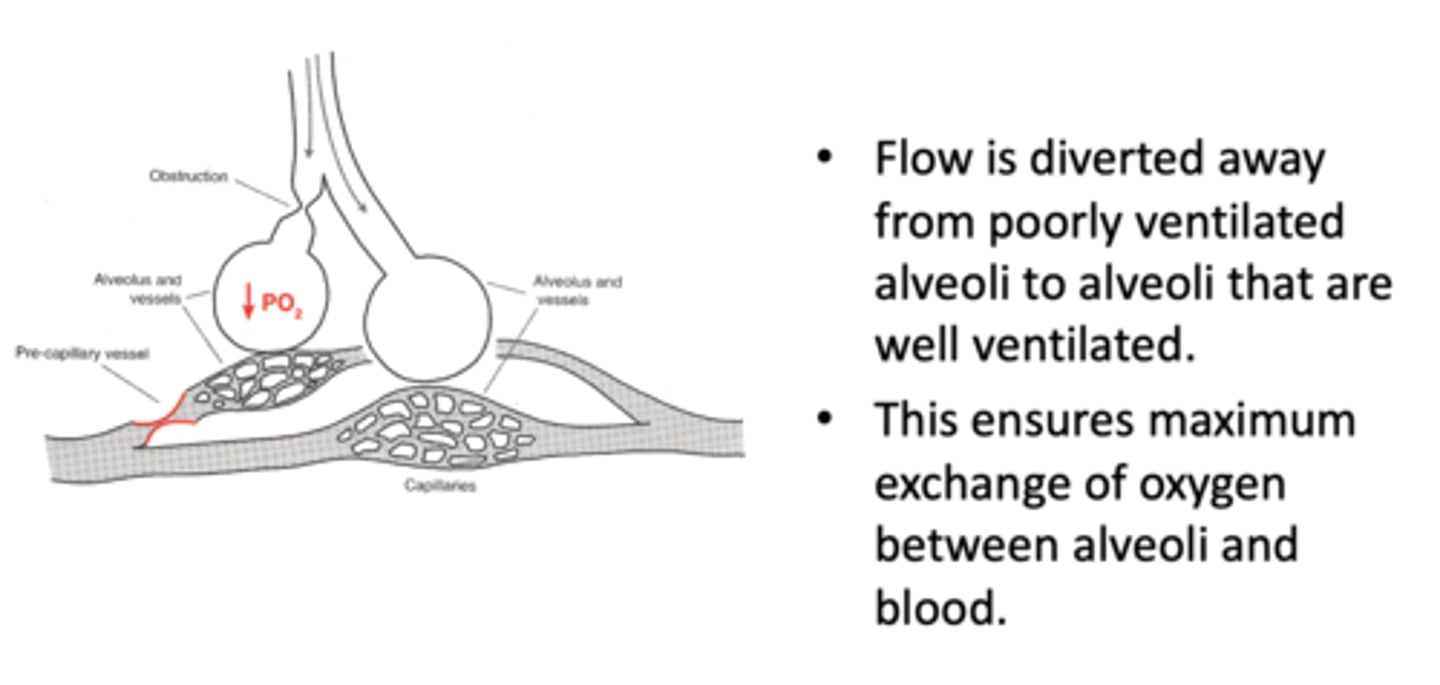
What has the following characteristics?
- When blood flow is diverted away from poorly ventilated alveoli to alveoli that are well ventilated
- This ensures maximum exchange of oxygen between alveoli and blood
hypoxic vasoconstriction
Piv also varies with the vertical position of the vessel relative to the heart: the higher the vessel, the _________ Piv.
Lower
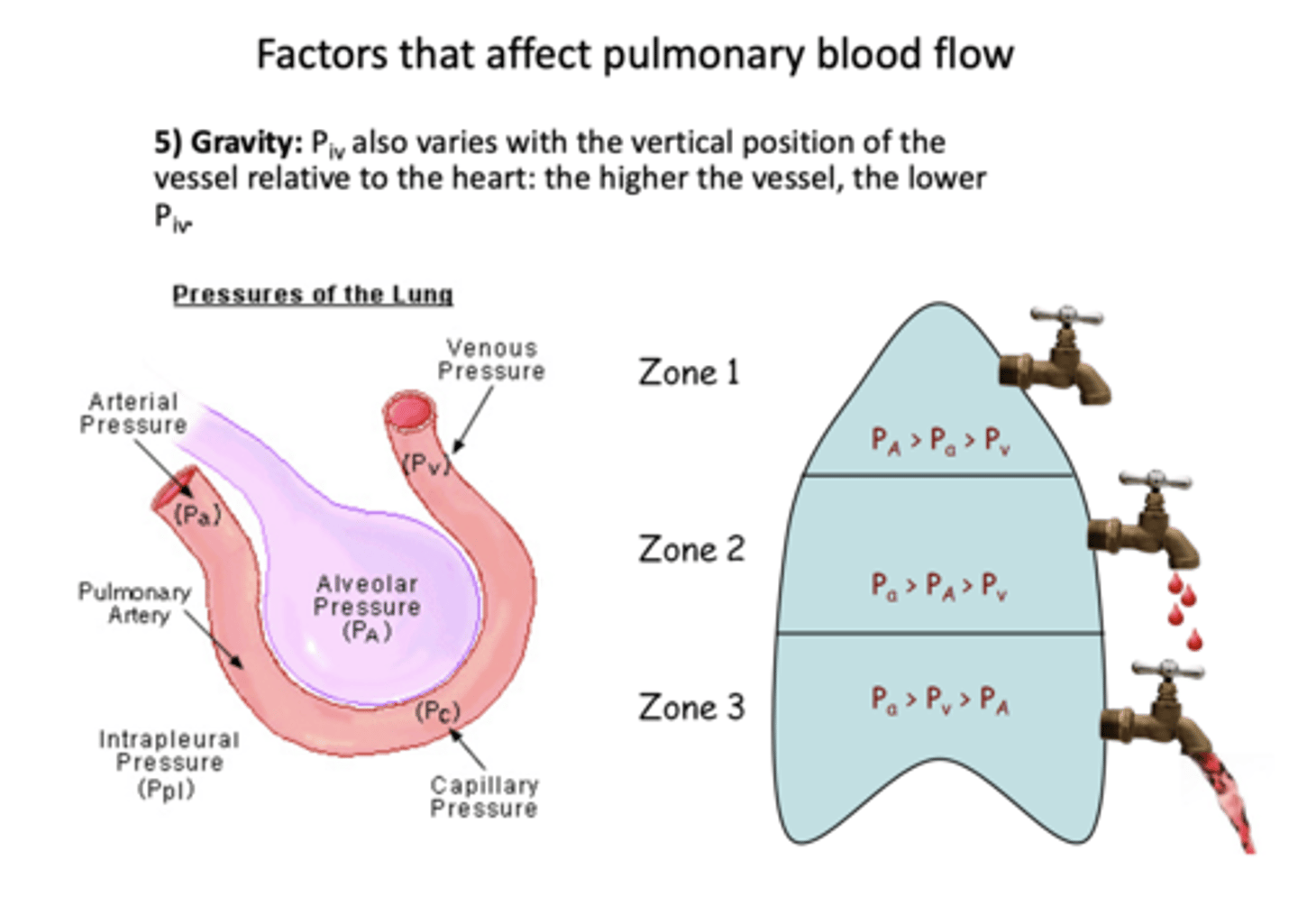
when a patient is upright in what zone is perfusion highest in the lungs?
zone 3
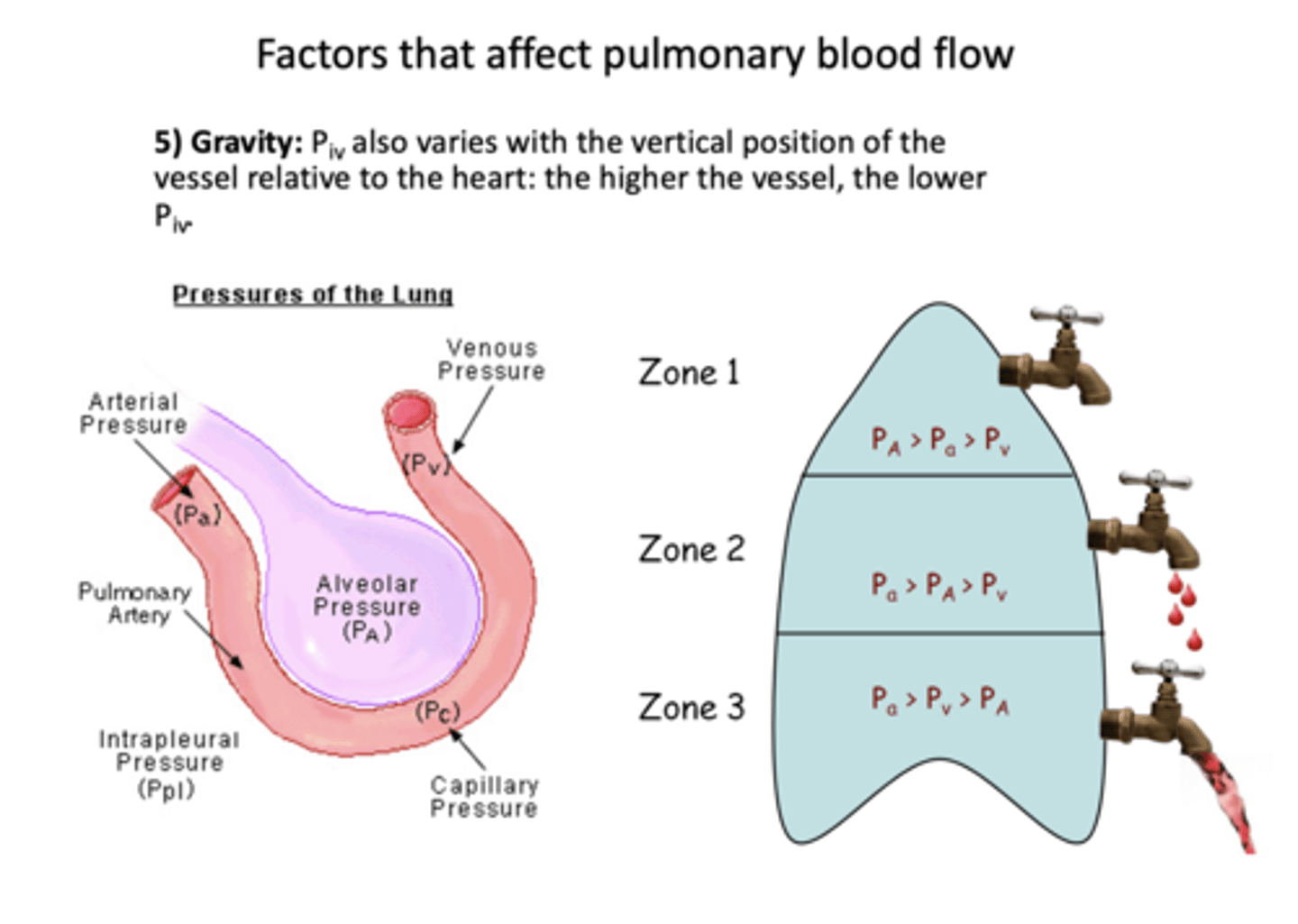
when a patient is upright in what zone is perfusion lowest in the lungs?
zone 1
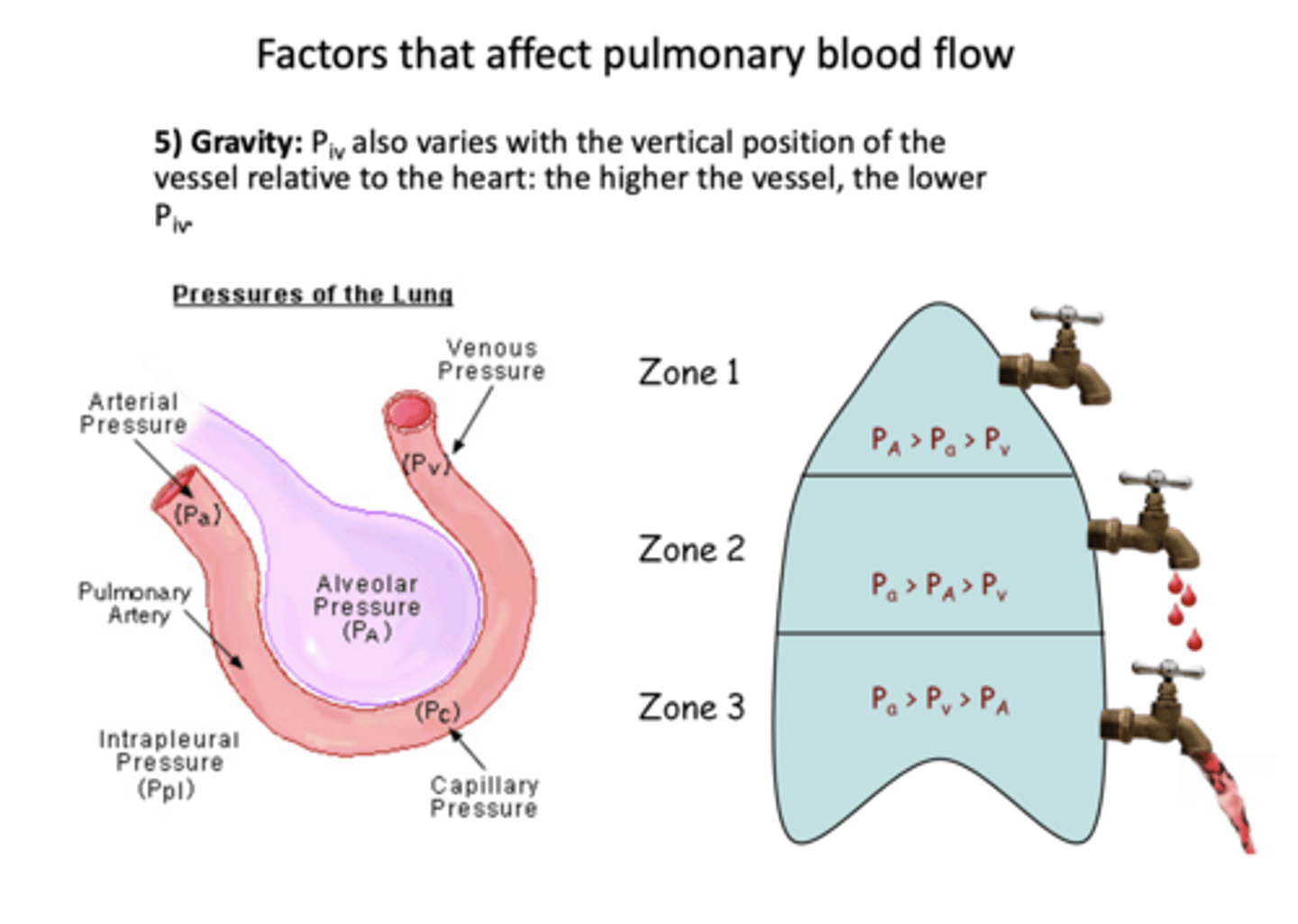
ID which zone the following perfusion pressure trend belongs to:
PA> Pa> Pv
zone 1
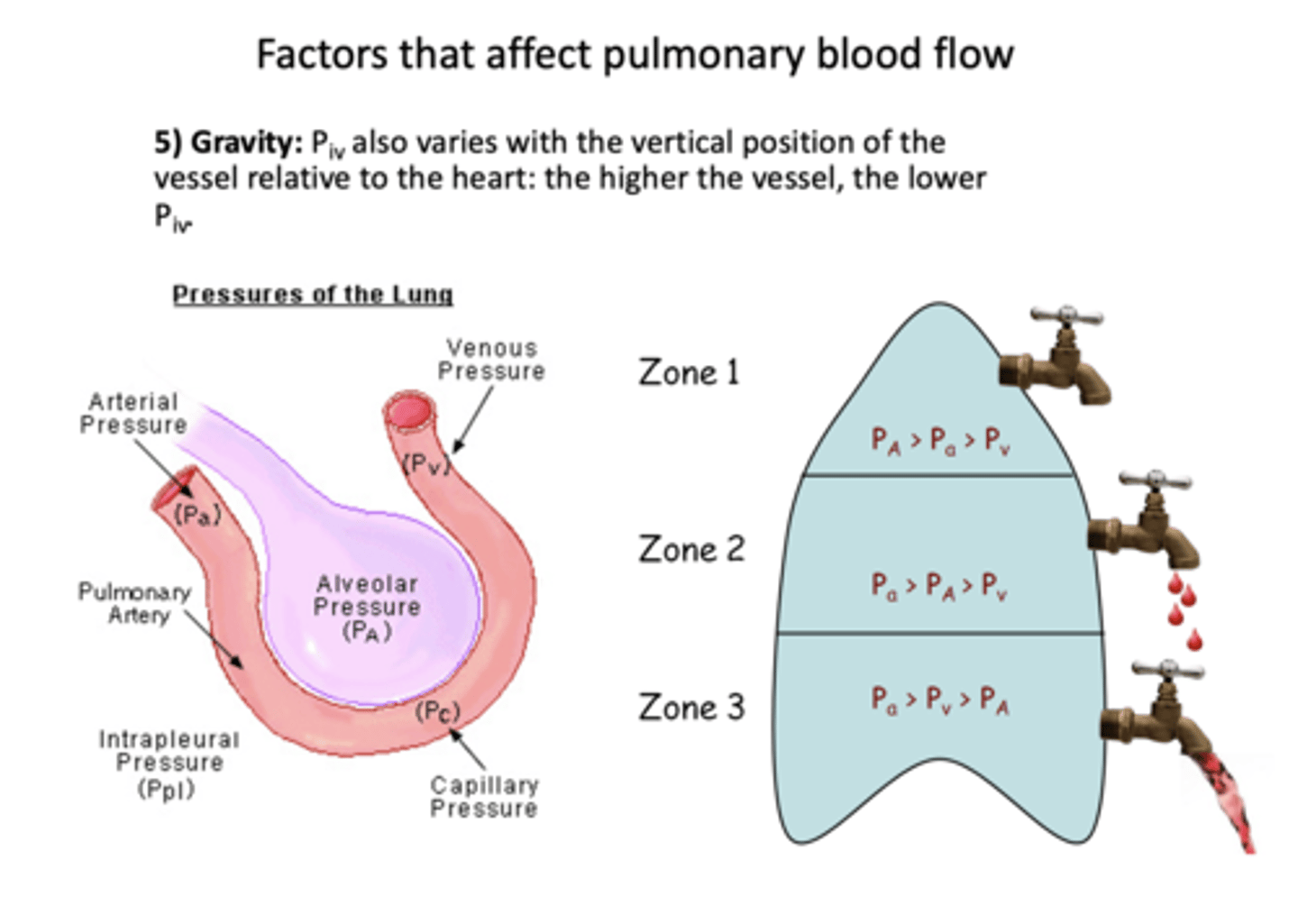
ID which zone the following perfusion pressure trend belongs to:
Pa> PA>Pv
zone 2
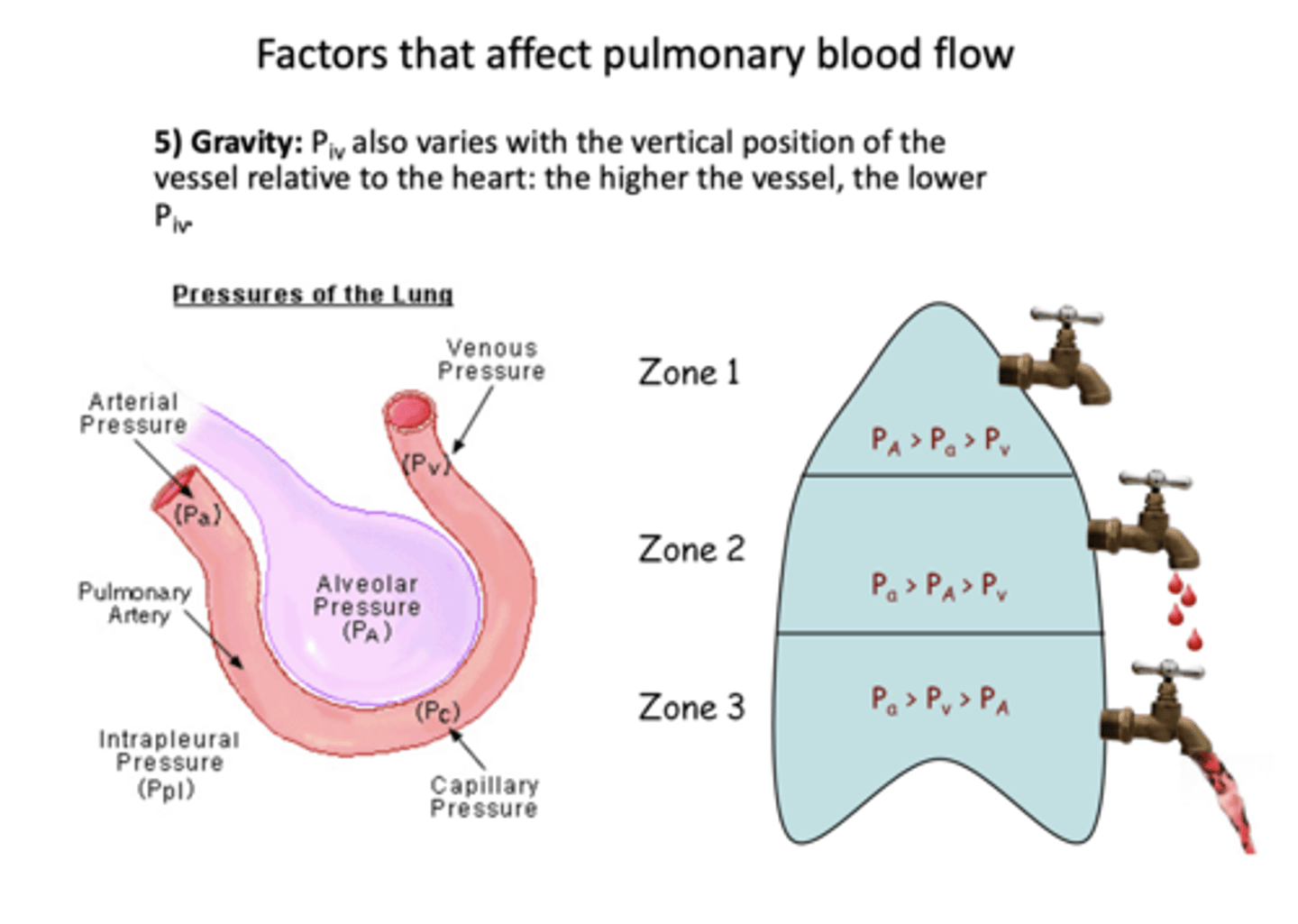
ID which zone the following perfusion pressure trend belongs to:
Pa> Pv >PA
zone 3
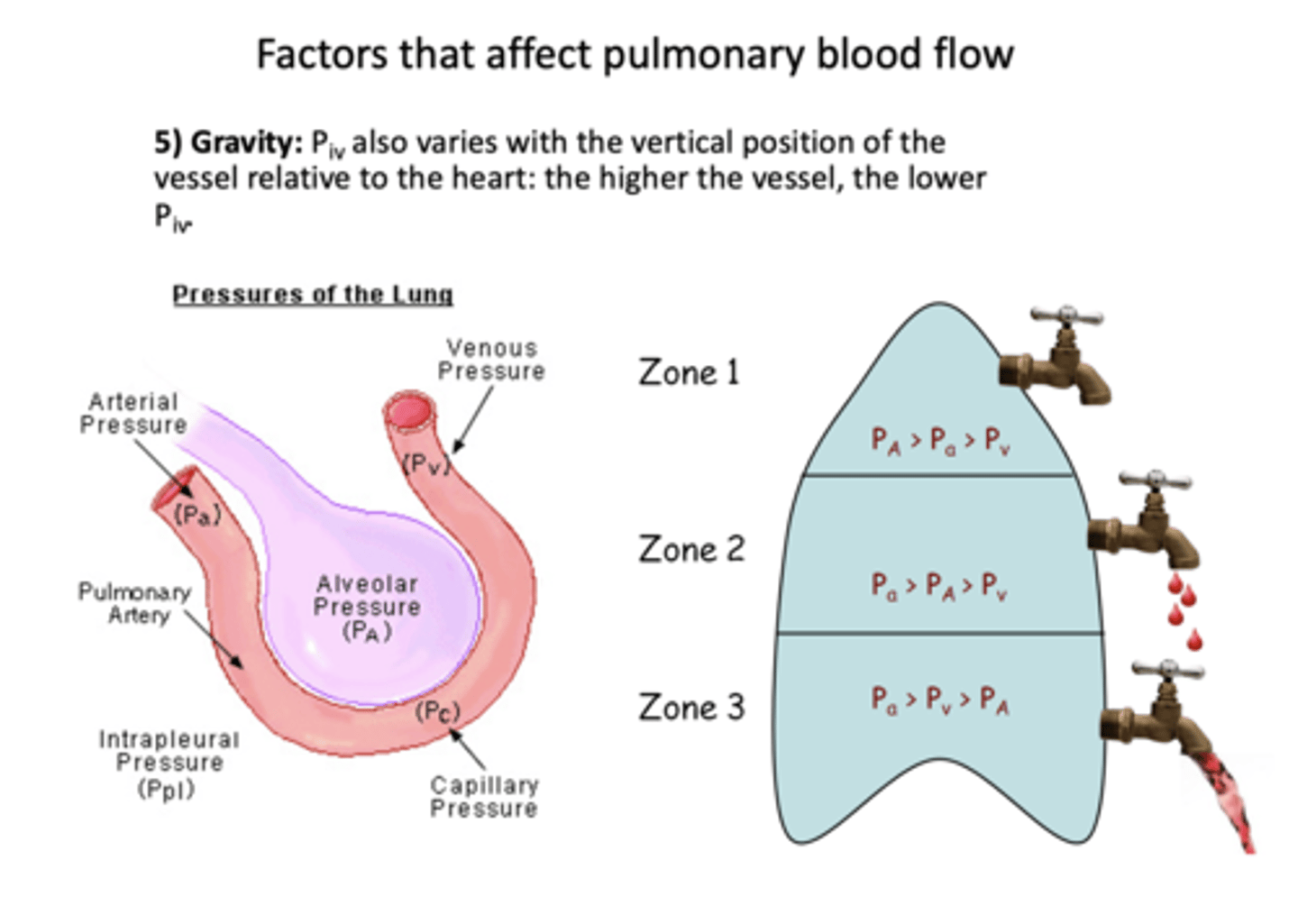
If lying supine, where is their greater flow: dorsal or ventral?
Dorsal (Reverses if upside down)
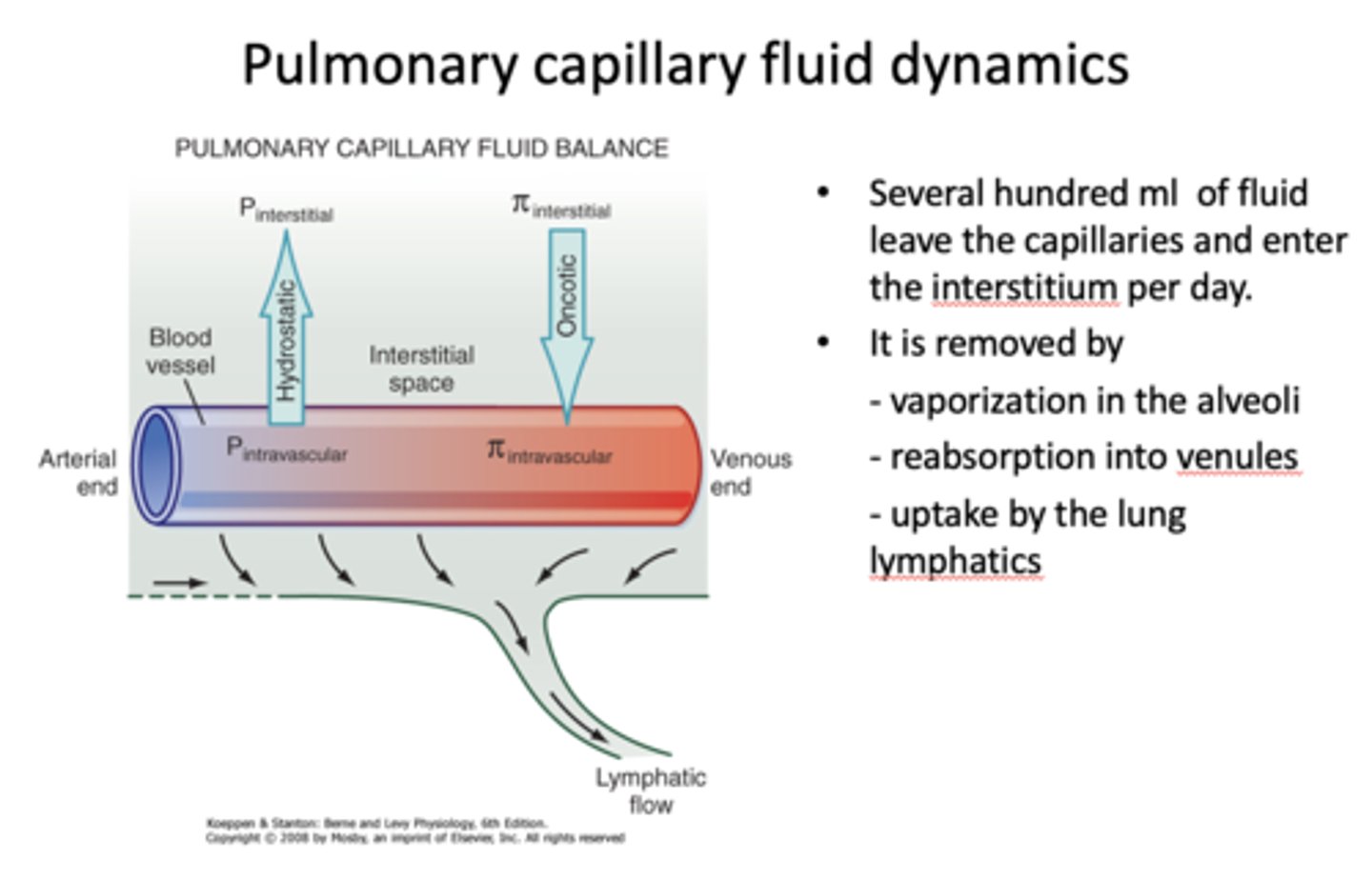
as blood flows from the arterial end (deoxygenated) to the venous end (oxygenated) of capillaries, hydrostatic pressure will _______
decrease
as blood flows from the arterial end (deoxygenated) to the venous end (oxygenated) of capillaries, oncotic pressure will _______
increase
fluid leaves the capillaries and enter the interstitium. that fluid is removed by (3):
- Vaporization in the alveoli
- Reabsorption into venules
- Uptake by the lung lymphatics
patients with mean pulmonary pressure exceeding 25mmHg at rest OR 35 mmHg during excercise have ___________
pulmonary hypertension
What has the following characteristics?
- Patients with pulmonary capillary pressure exceeding 25mmHg at rest
- Excessive fluid in the interstitial tissue or alveoli
- Fluid flux out of capillary exceeds capacity of the lymphatics to drain interstitum
pulmonary edema
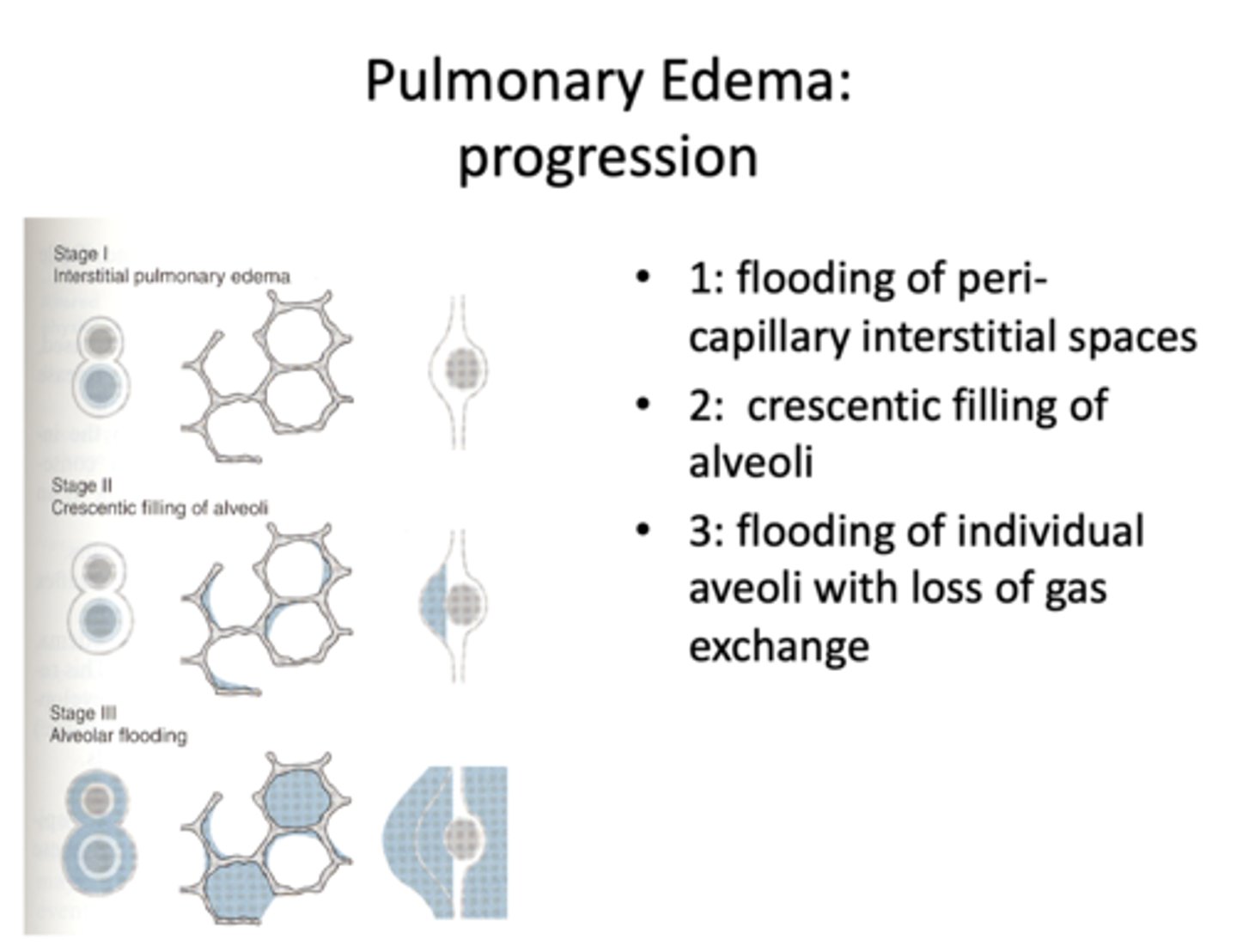
The three following progression steps result in what?
1: Flooding of peri-capillary interstitial spaces
2: Crescentic filling of alveoli
3: Flooding of individual aveoli with loss of gas exchange
Pulmonary edema
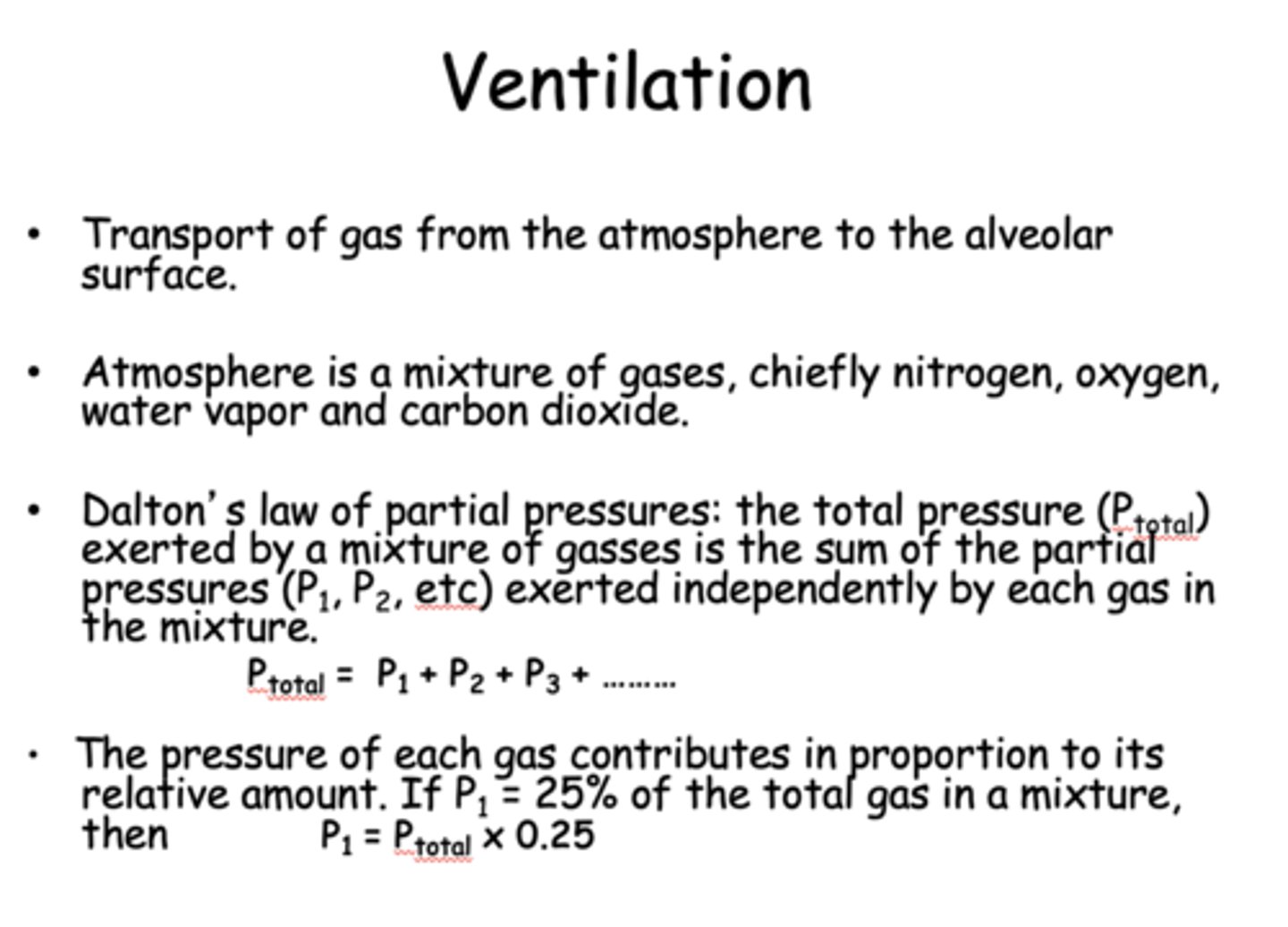
Define the following:
Transport of gas from the atmosphere to the alveolar surface
Ventilation
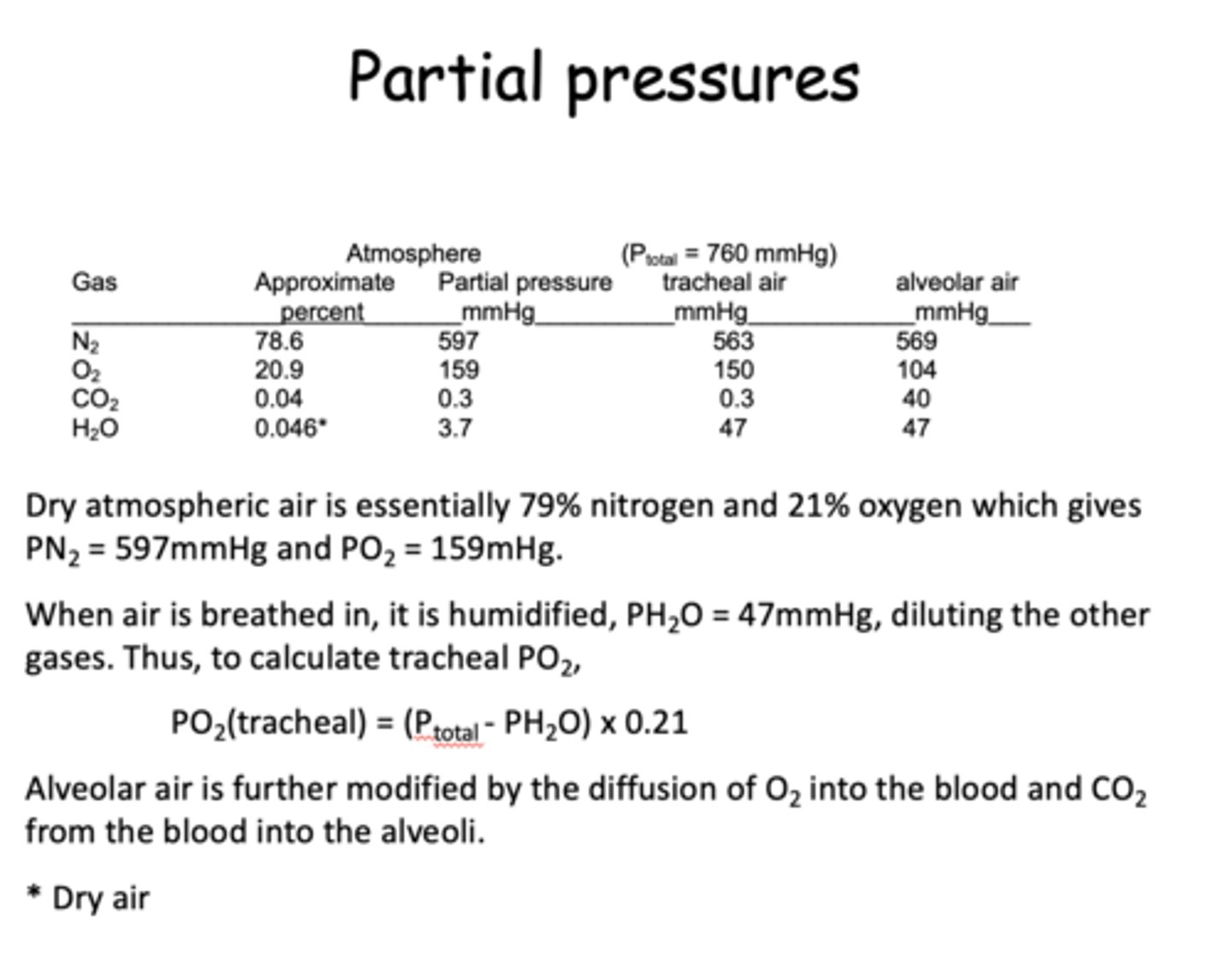
What main gases does the atmosphere compose of?
- Nitrogen
- Oxygen
- Carbon dioxide
- H2O vapor
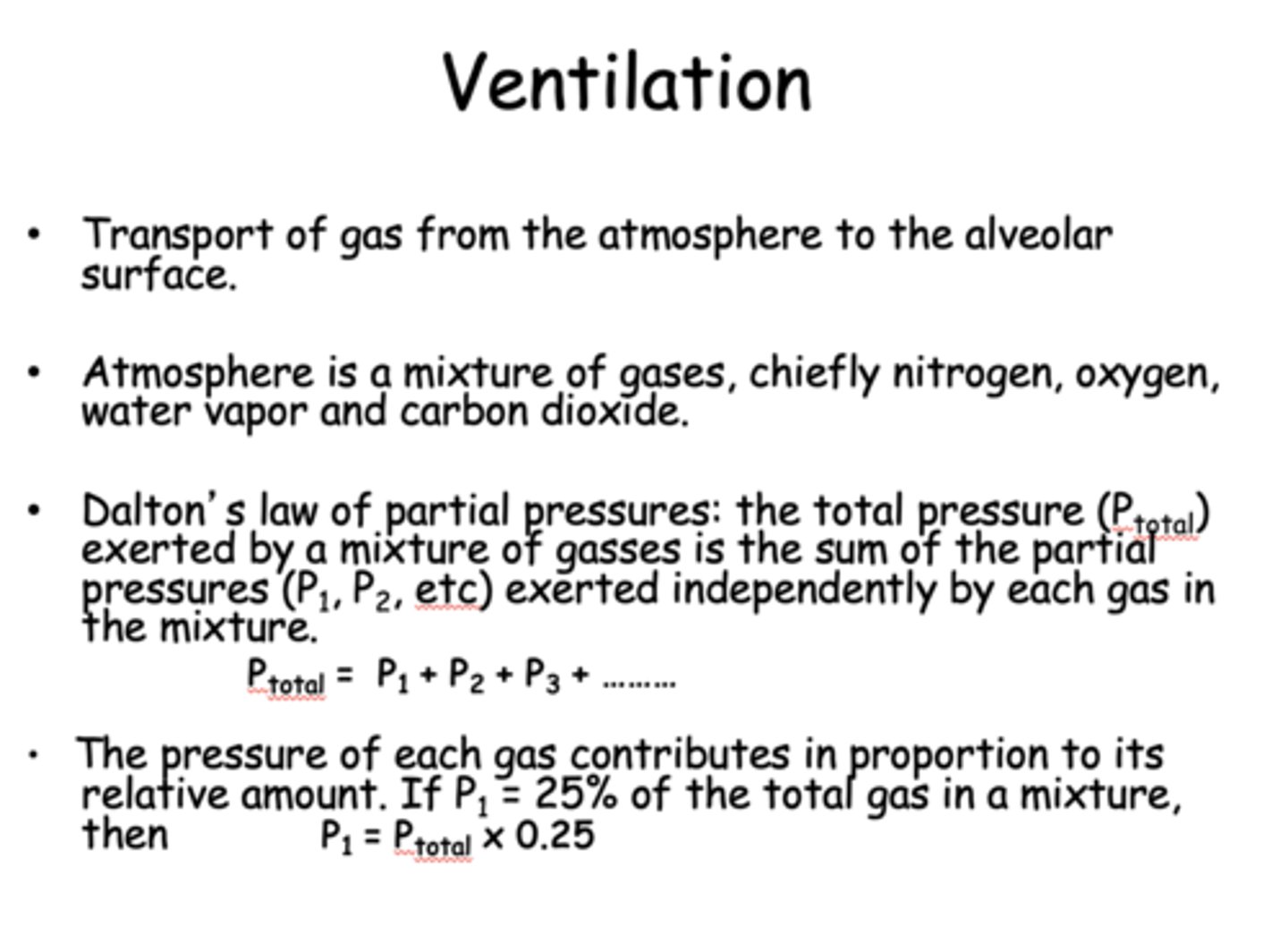
Define the following:
The total pressure (Ptotal) exerted by a mixture of gasses is the sum of the partial pressures (P1, P2, etc) exerted independently by each gas in the mixture
Dalton's law of partial pressures
what gas makes up the majority of the atmospheric air?
nitrogen
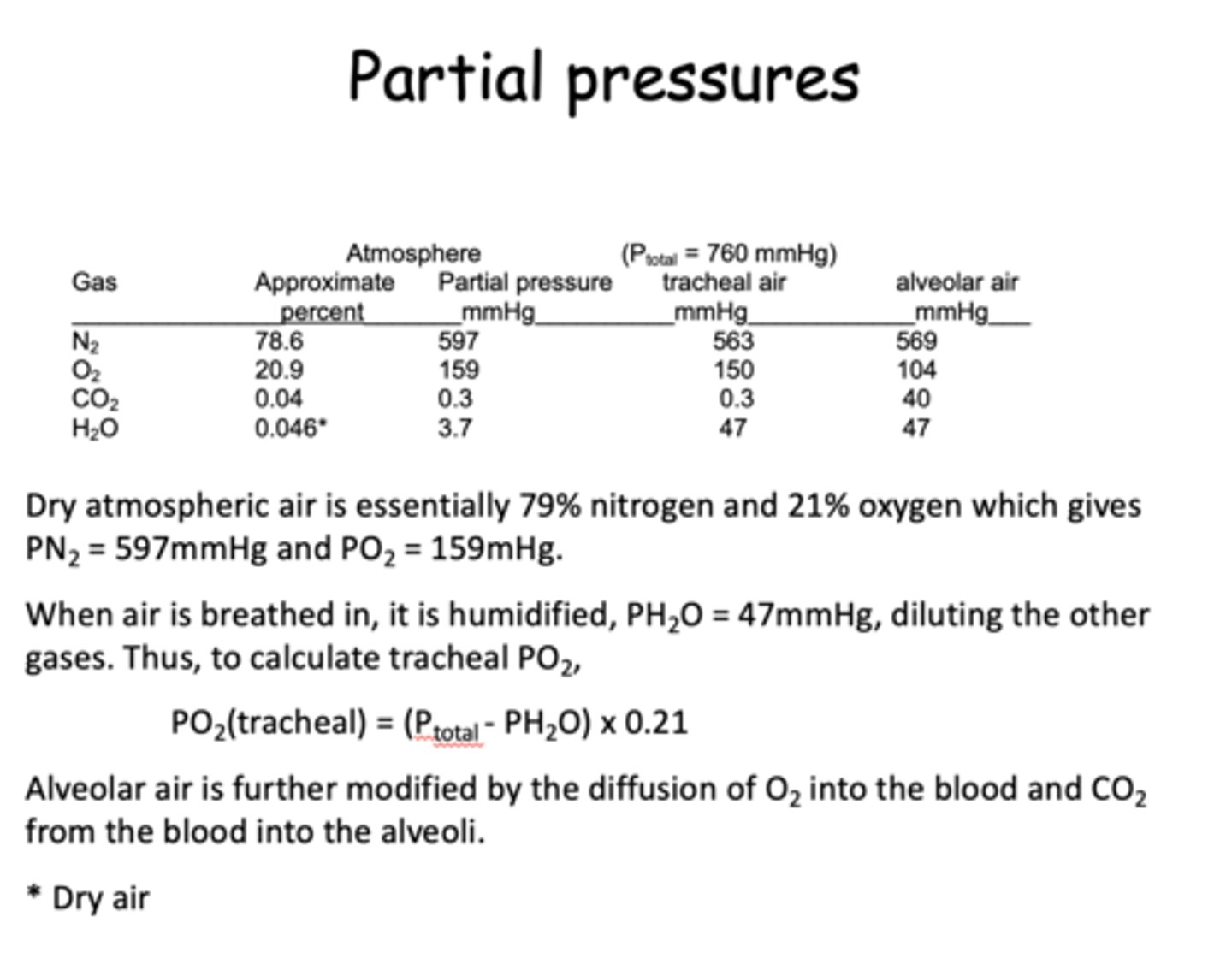
when you breath in and were to sample the air from the trachea, which gas value has a drastic increase?
H2O
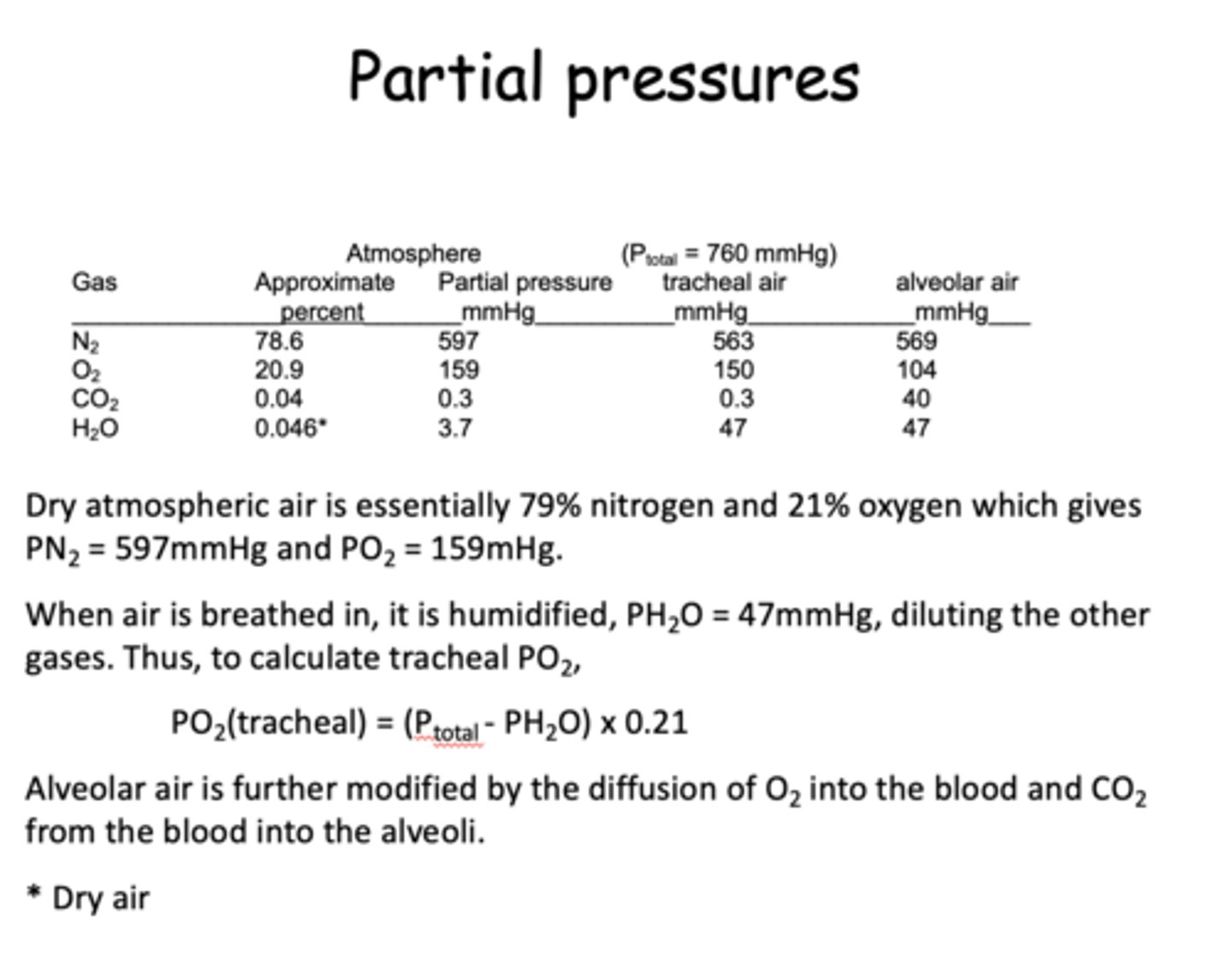
what is the steady state pressure of O2 in the alveoli?
104
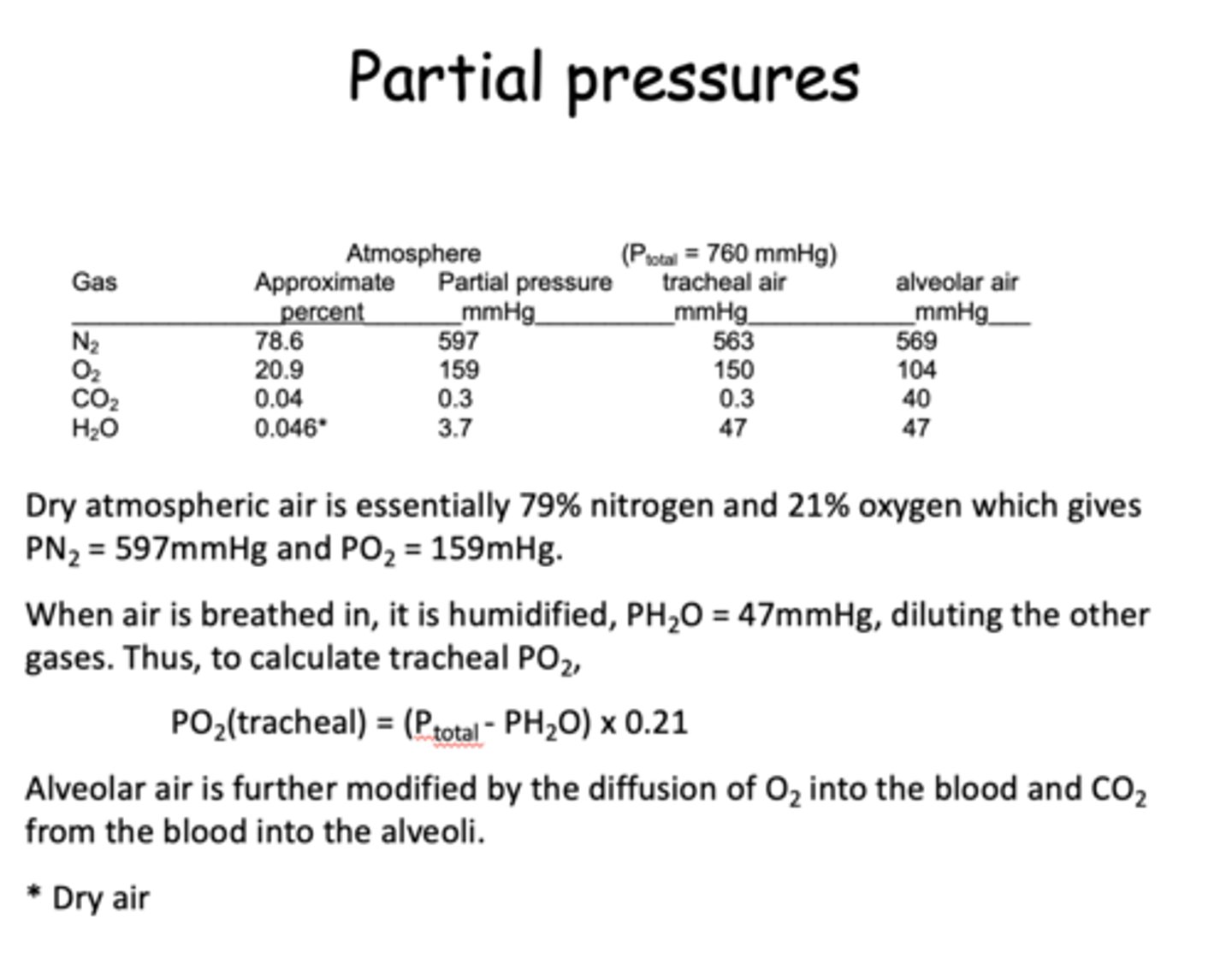
what is the steady state pressure of CO2 in the alveoli?
40
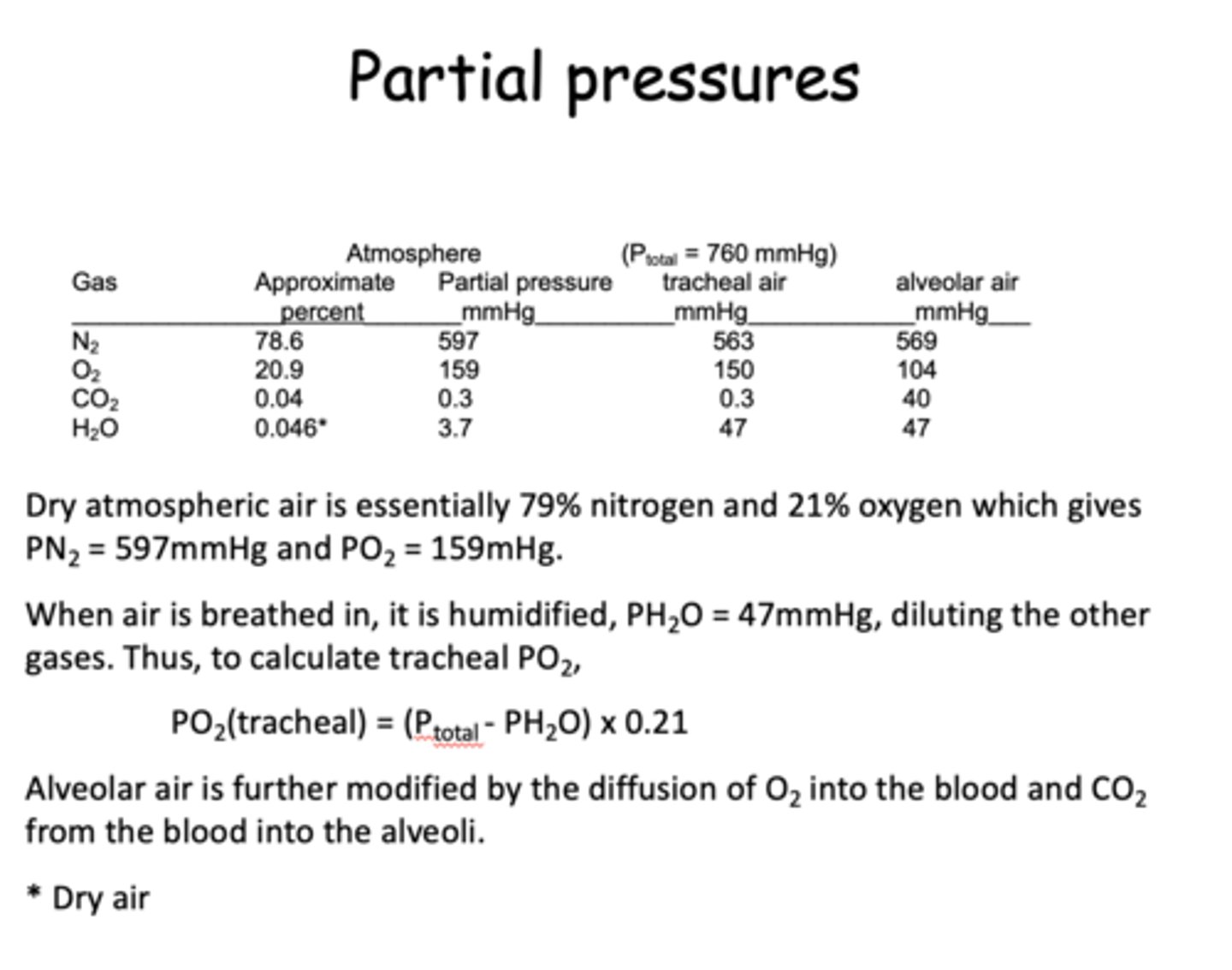
what is the steady state pressure of N2 in the trachea?
563
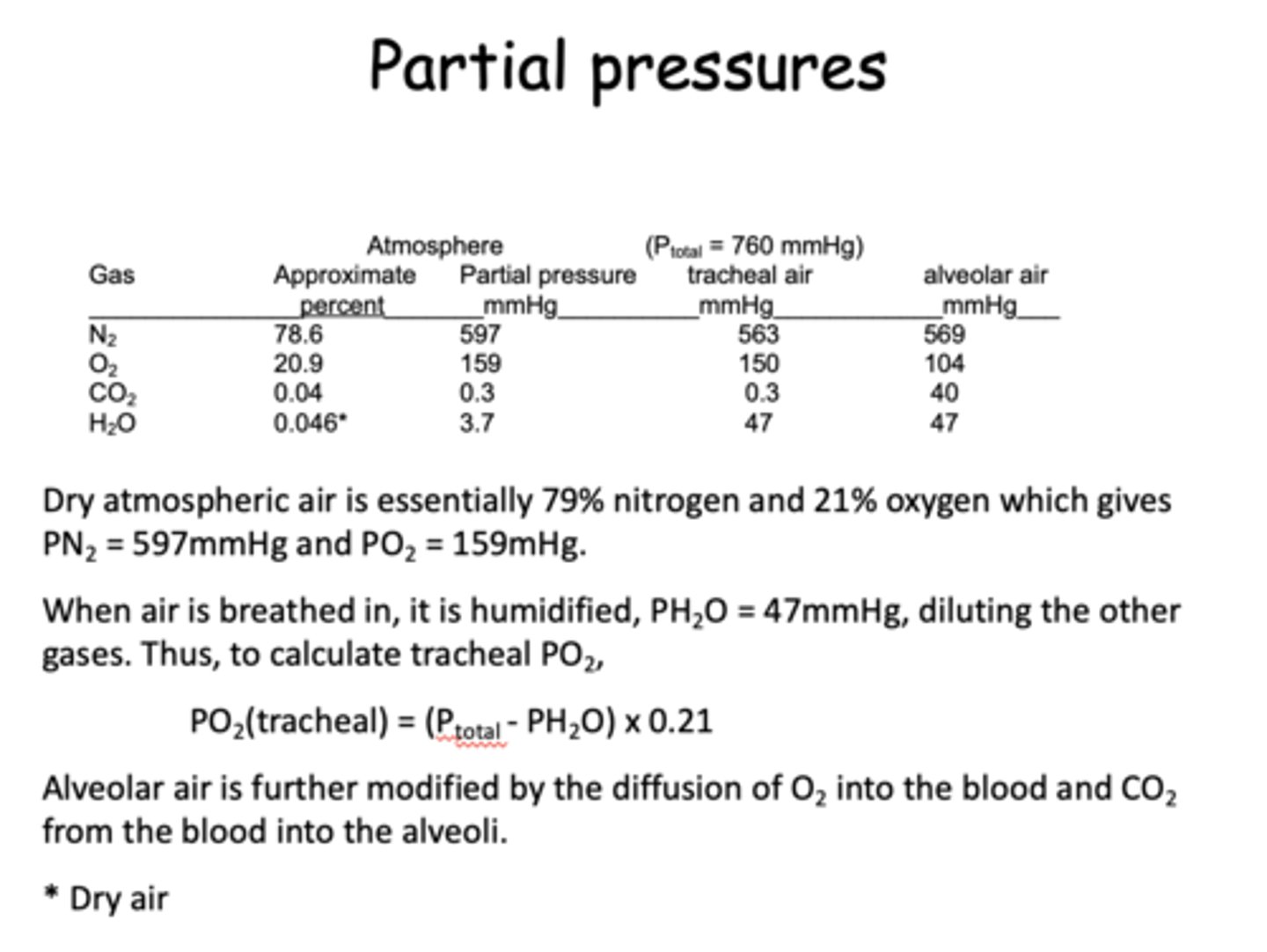
what is the steady state pressure of O2 in the trachea?
150
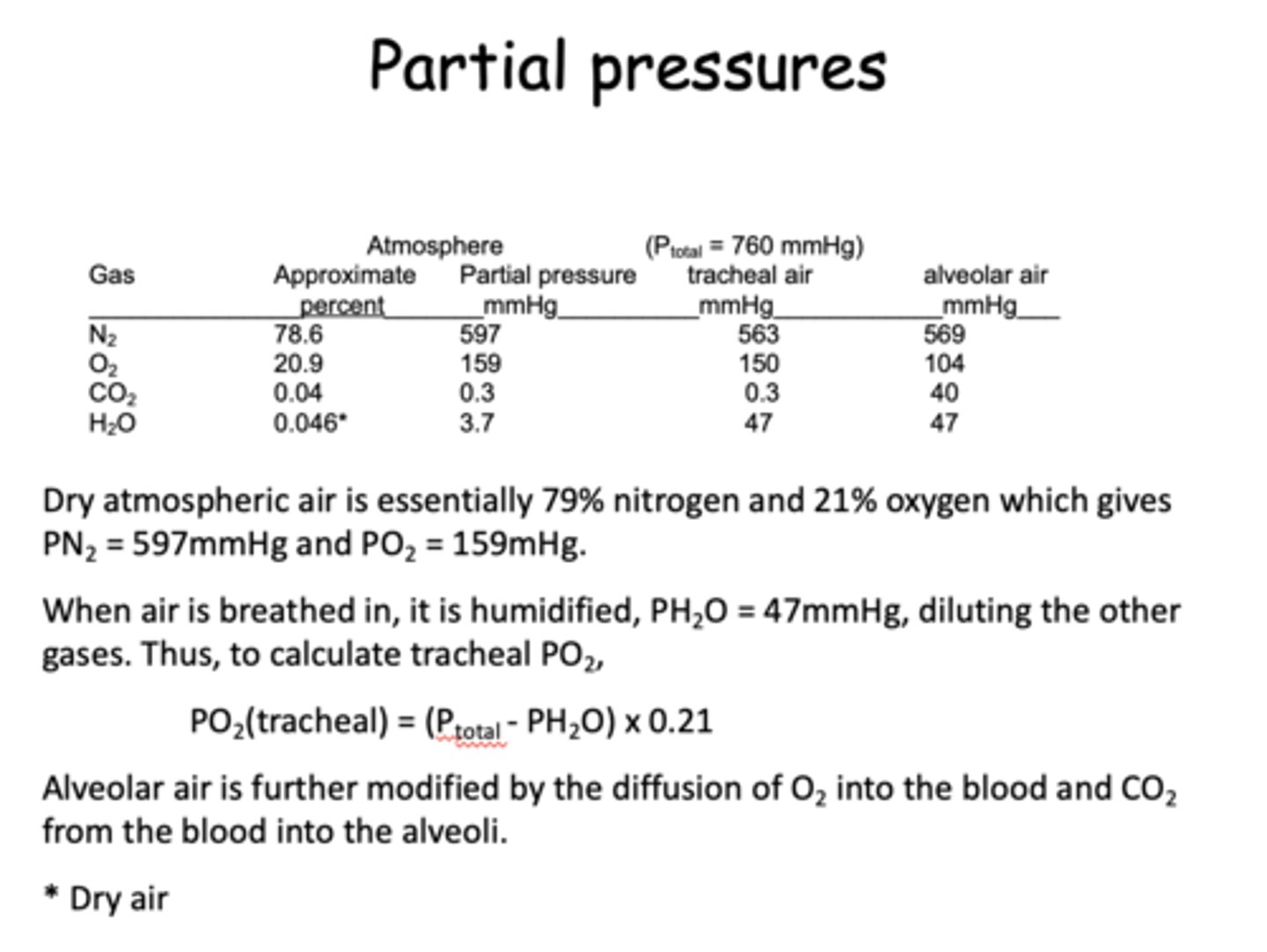
what is the steady state pressure of CO2 in the trachea?
0.3
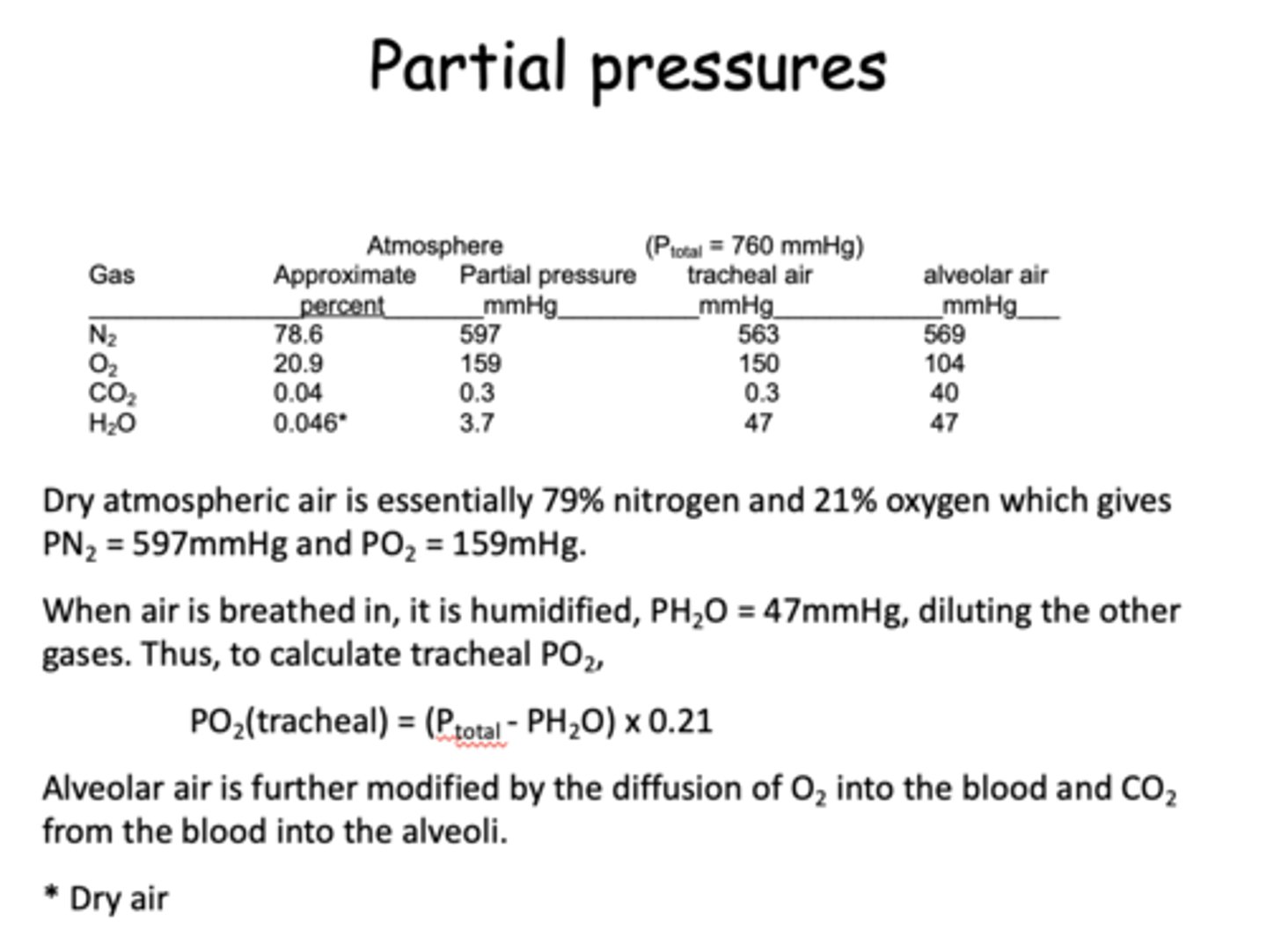
what is the steady state pressure of H2O in the trachea?
47
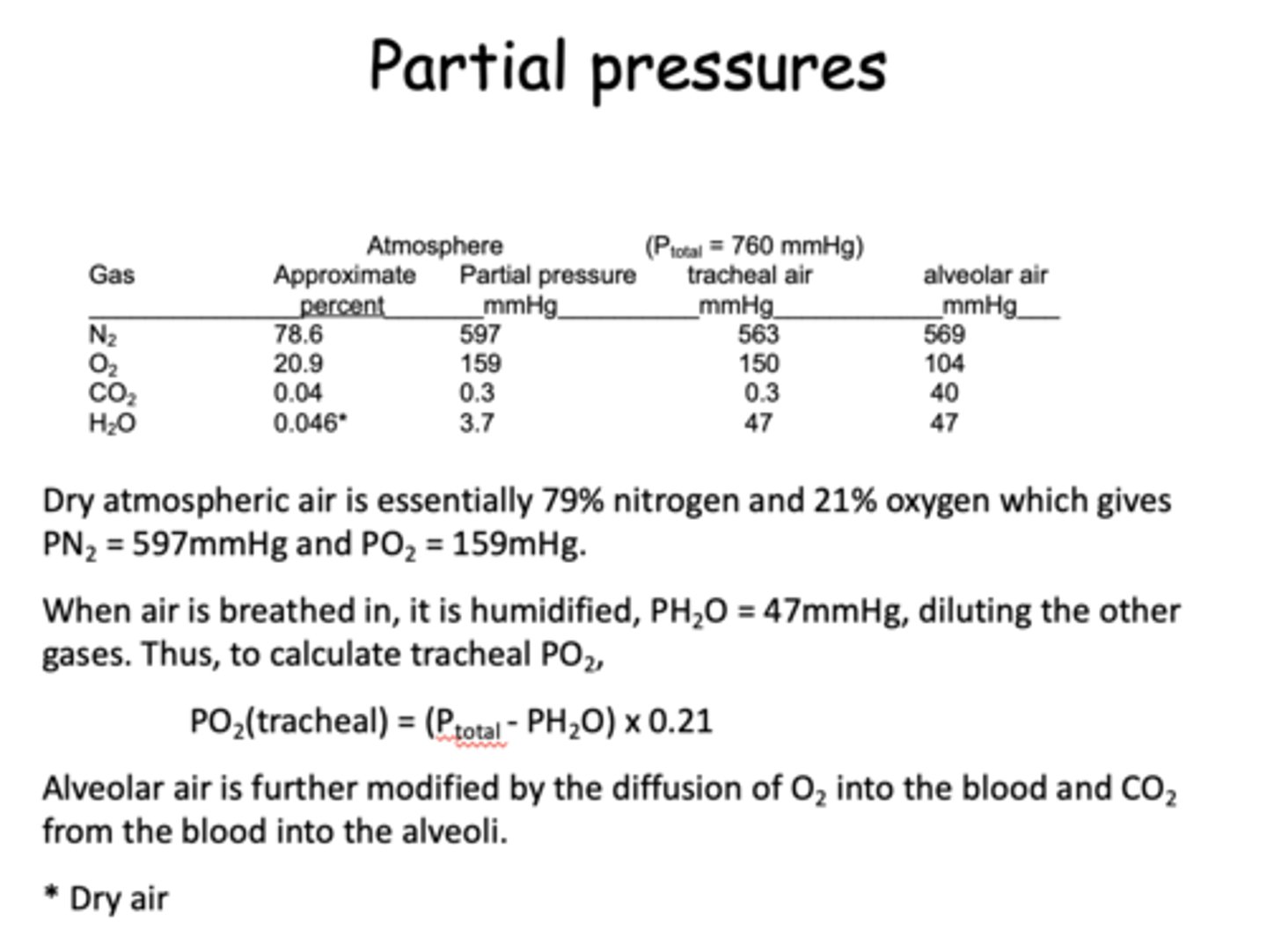
if you want to calculate the PO2 in the trachea, which gas pressure value must be subtracted from the total pressure?
H2O
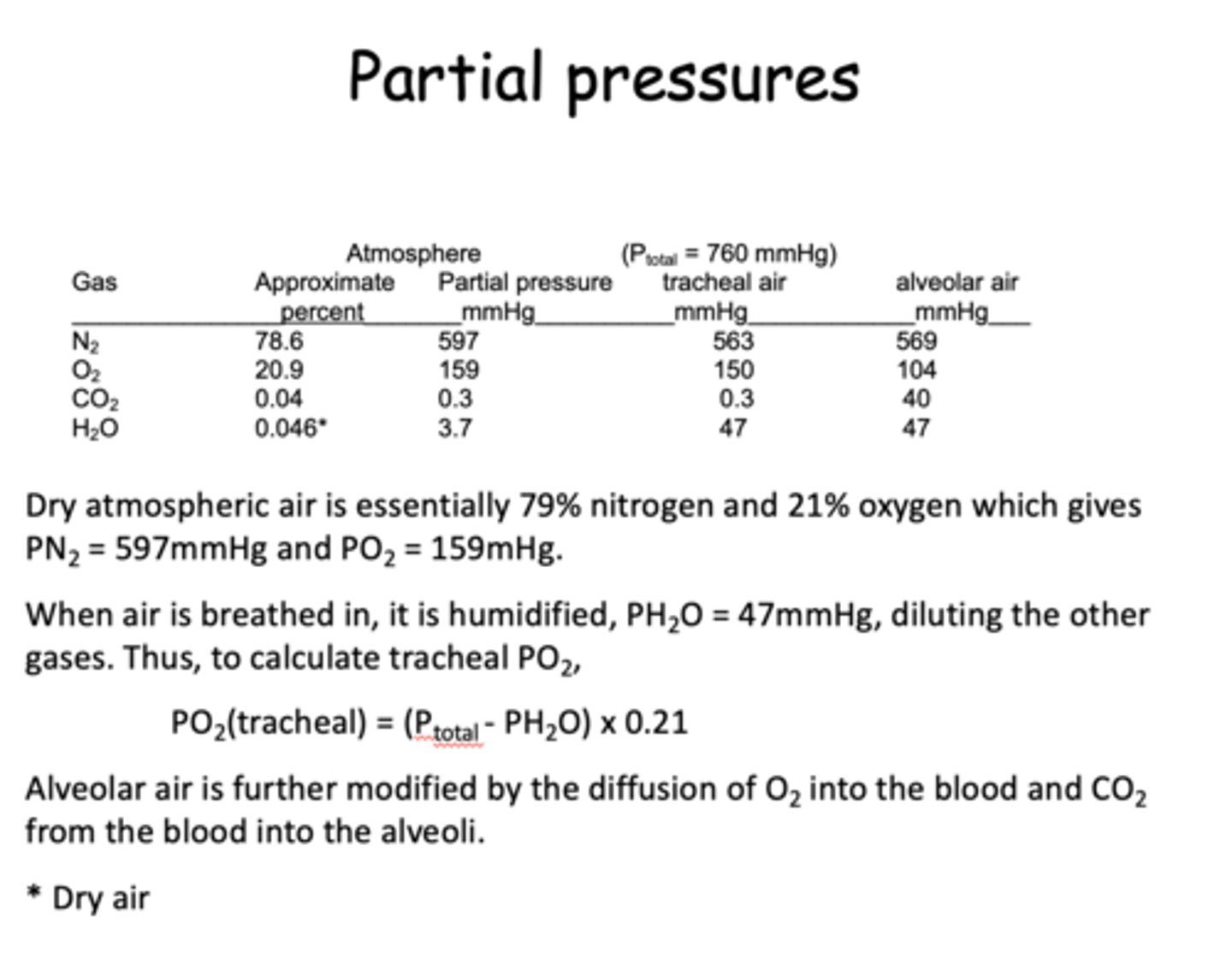
Dry atmospheric air is essentially 79% _______
nitrogen
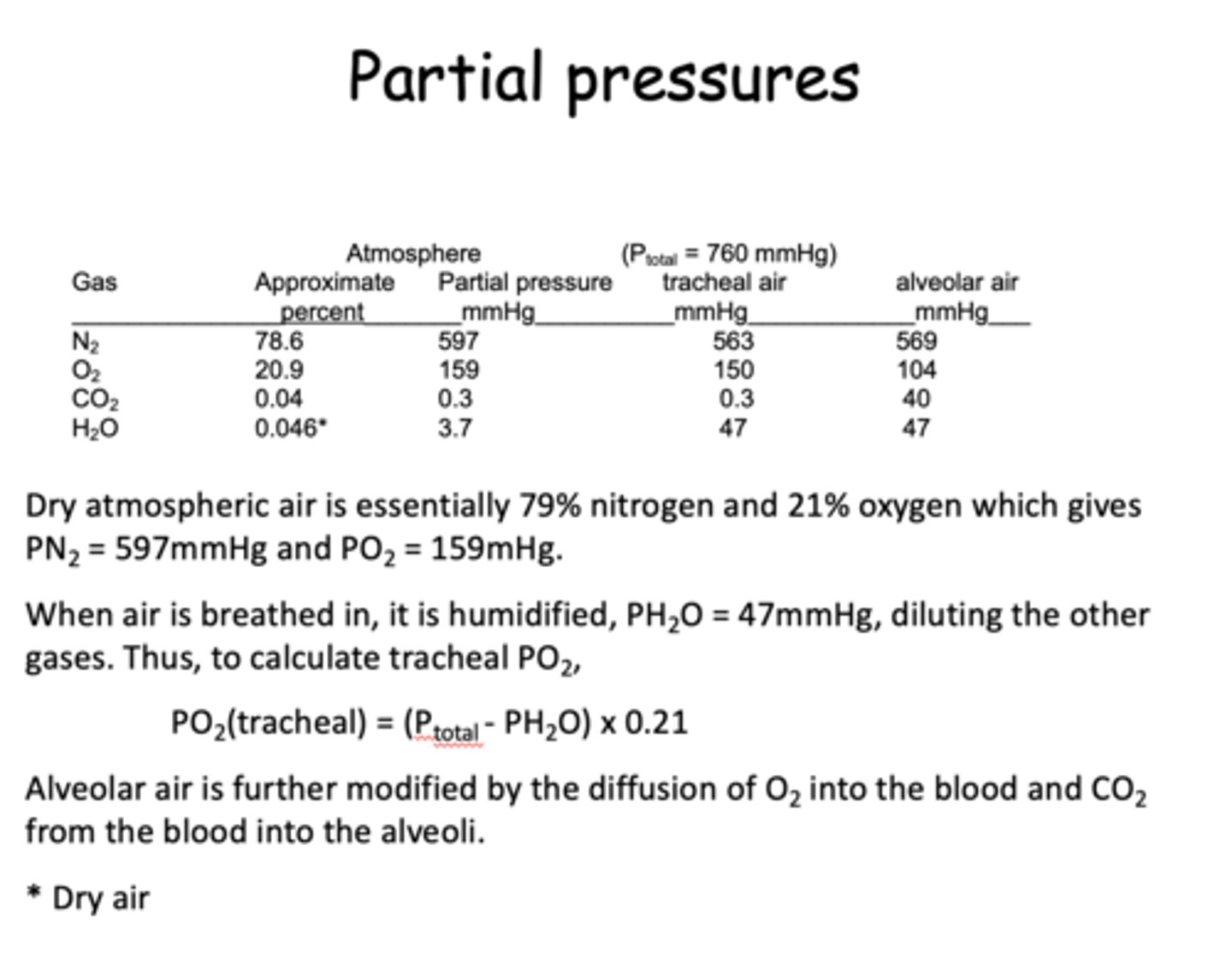
Dry atmospheric air is essentially 21% _______
oxygen
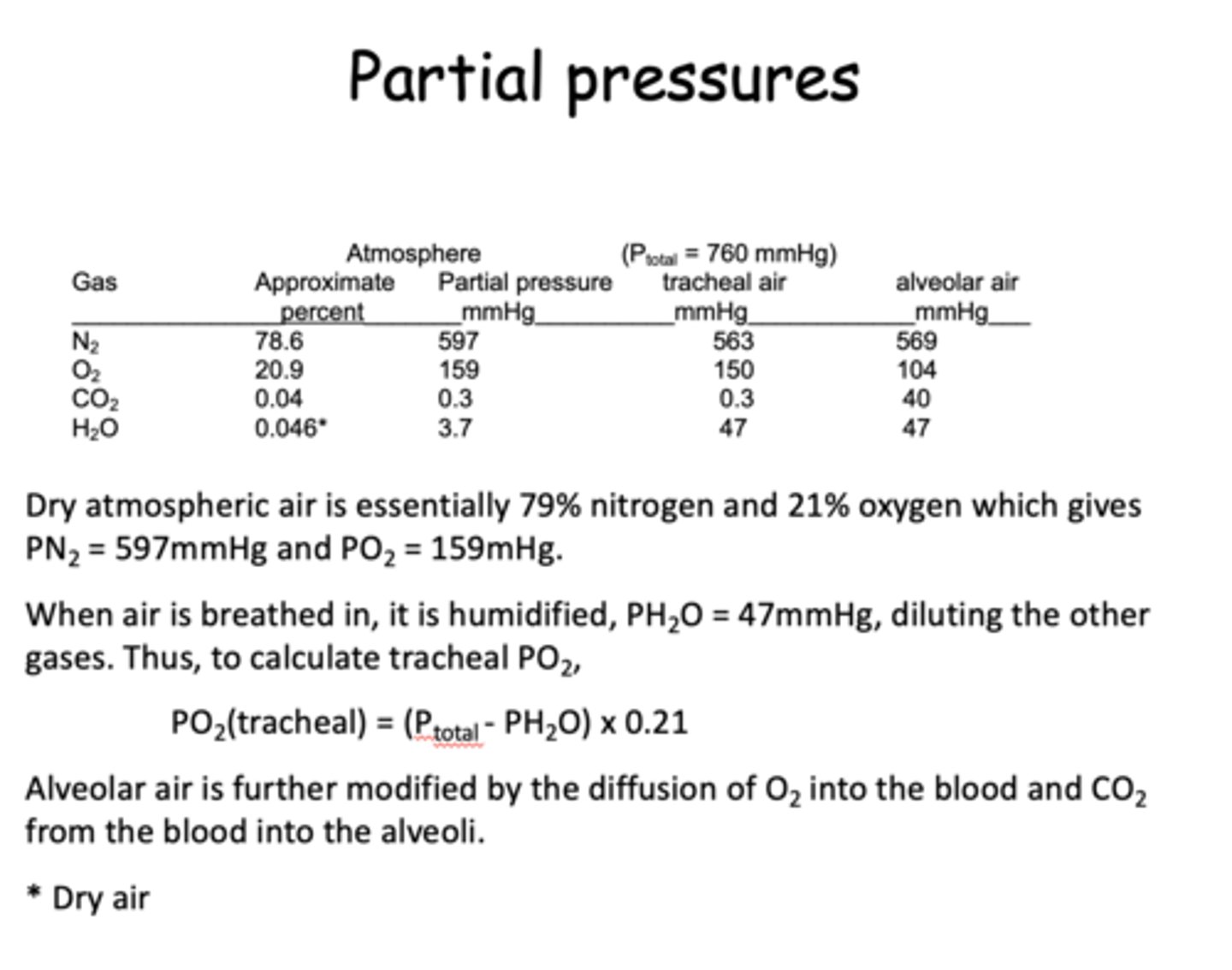
how do you calculate trachael PO2?
PO2(trachael)= (Ptotal-PH2O) x 0.21
how do you calculate minute ventilation (ml/min)?
respiratory rate (breaths/min) X tidal volume (ml/breath)
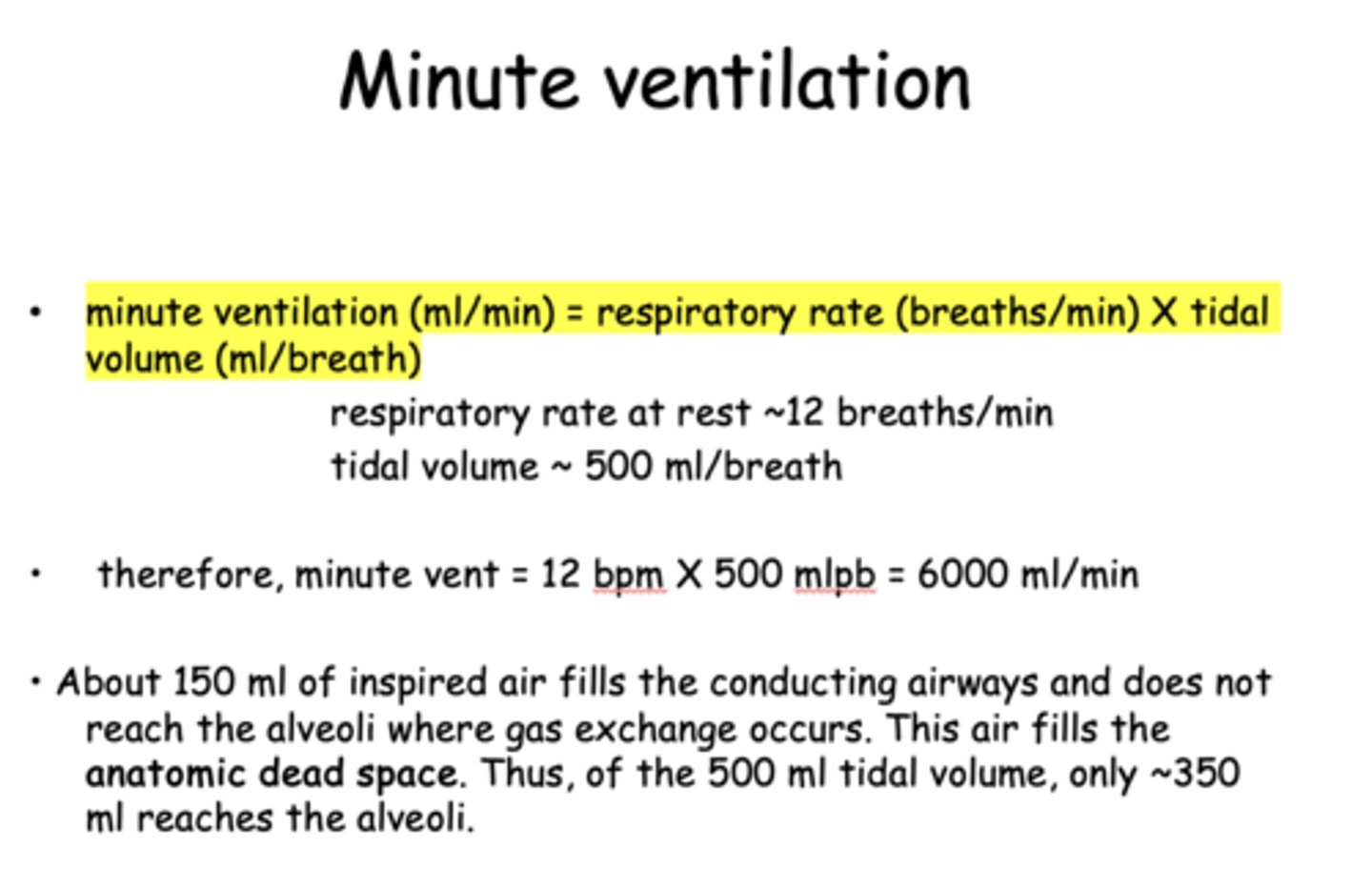
what is normal respiratory rate at rest?
12 breaths/min
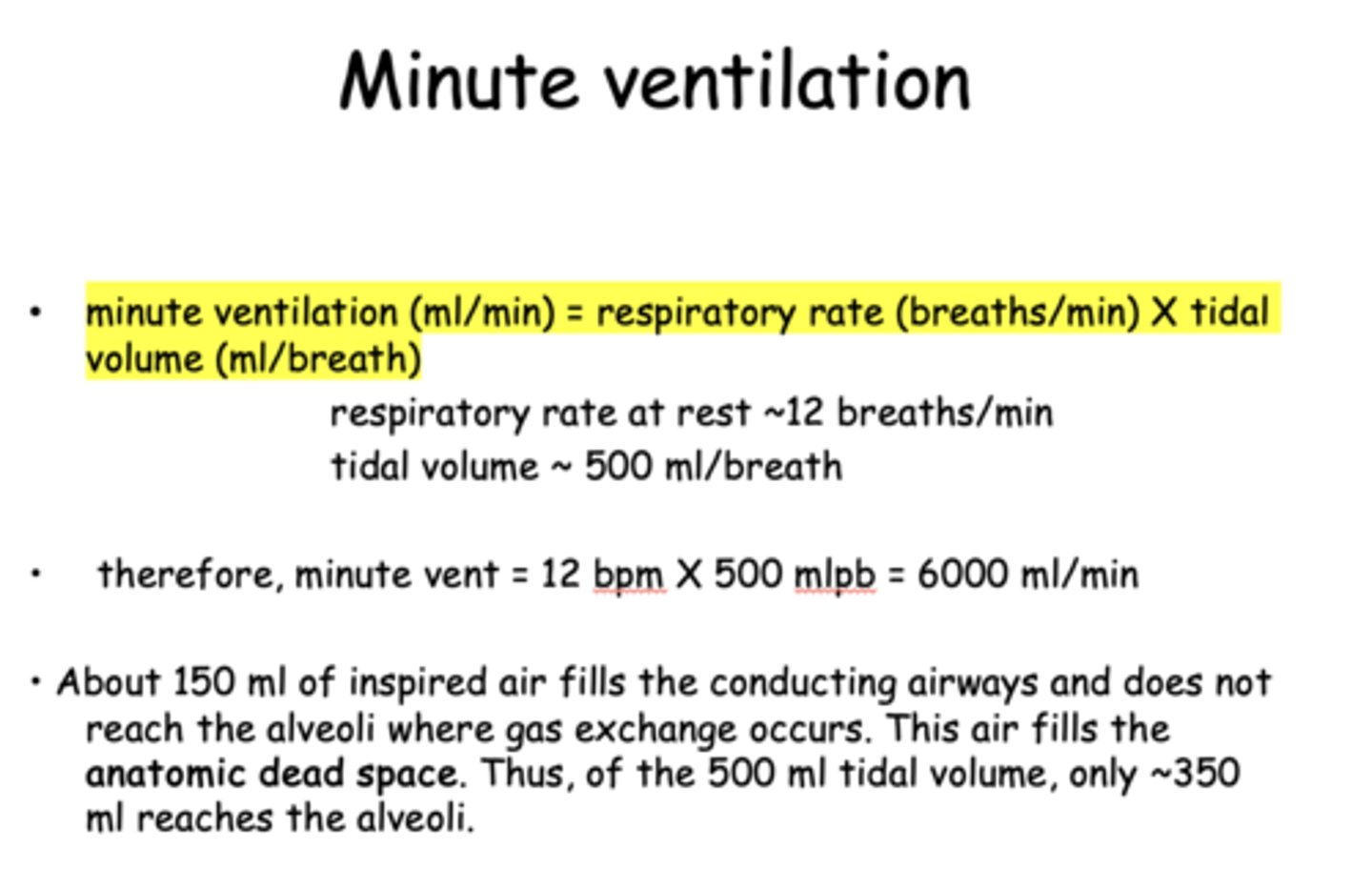
what is normal tidal volume at rest?
500 ml/breath
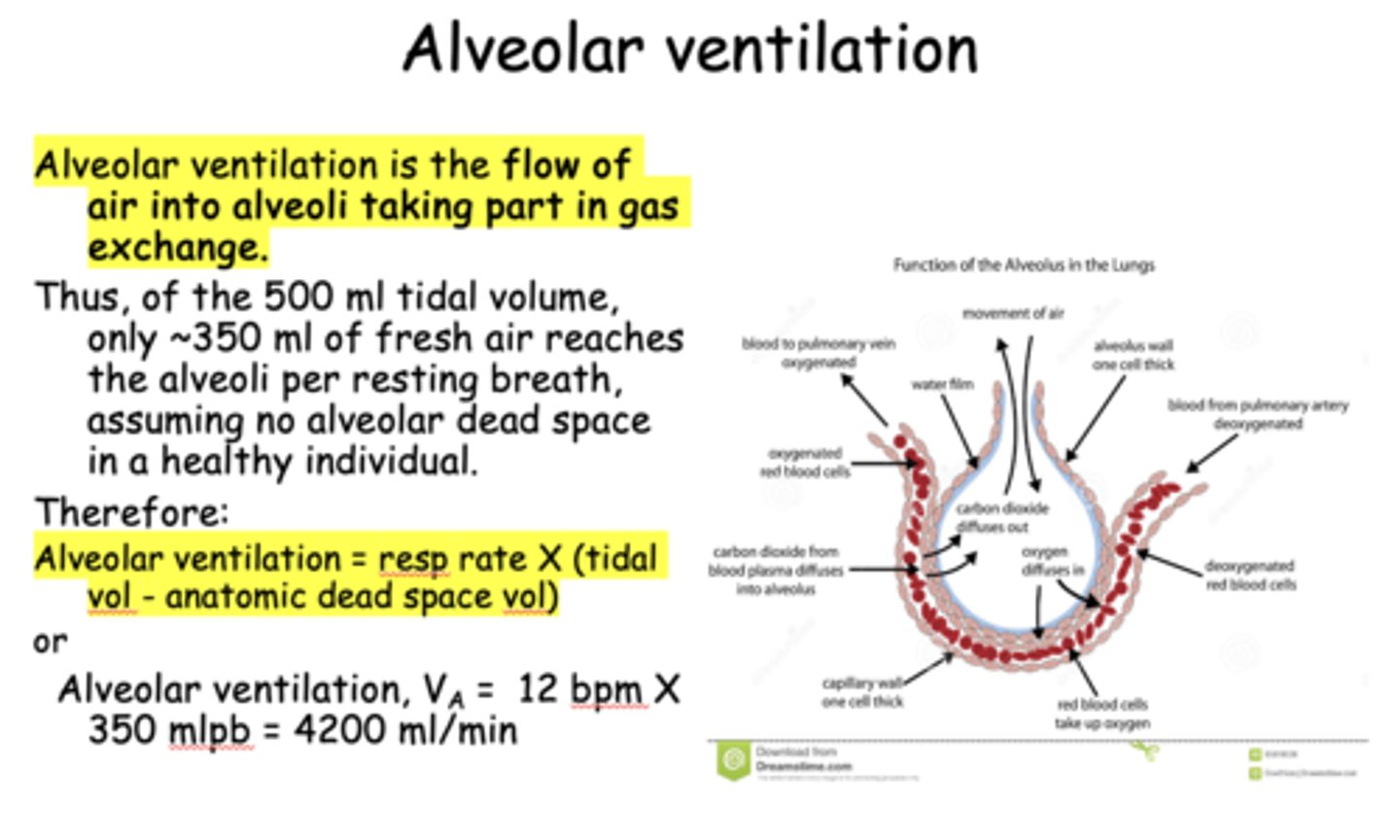
About _____ ml of inspired air fills the conducting airways and does not reach the alveoli where gas exchange occurs. This air fills the anatomic dead space
150
About 150 ml of inspired air fills the conducting airways and does not reach the alveoli where gas exchange occurs. Thus air fills the _______
anatomic dead space
The 150 ml of inspired air filling the conducting airways fills the __________ dead space
anatomic
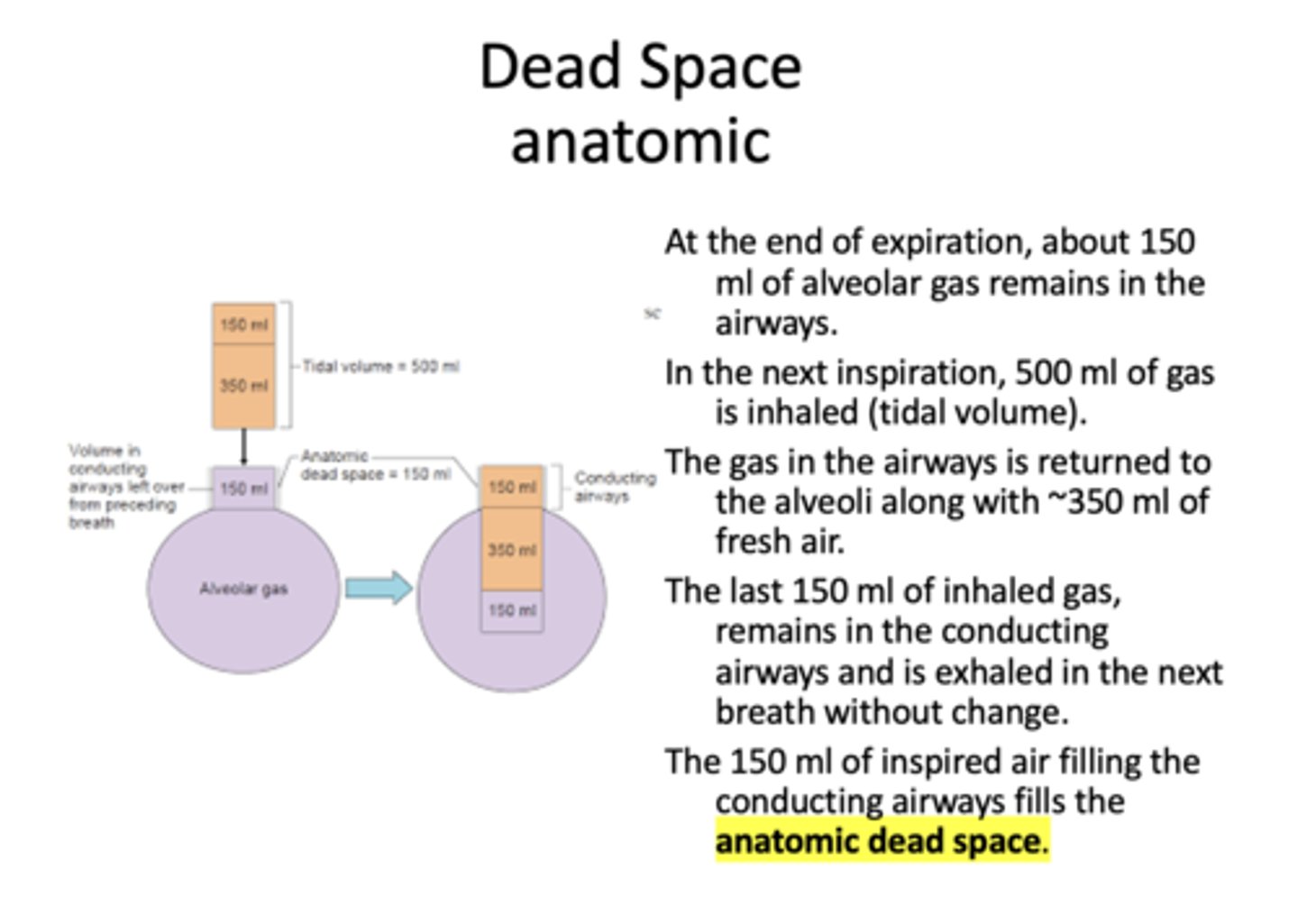
Of the 500 ml tidal volume, only ~_____ ml reaches the alveoli.
350
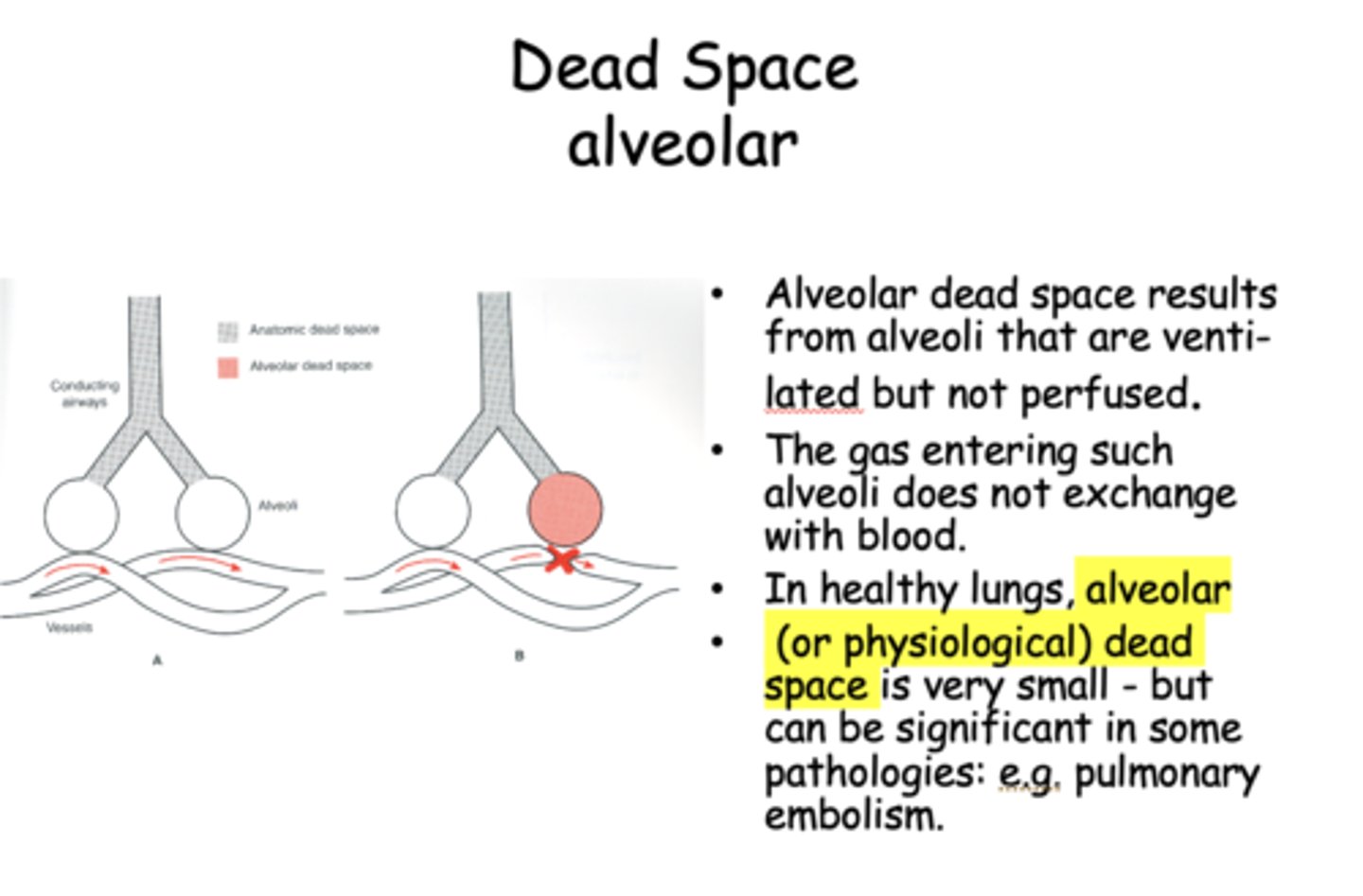
when alveoli are ventilated but not perfused (gas entering alveoli does not exchange with blood):
alveolar dead space
calculation for Alveolar ventilation:
resp. rate X (tidal vol. - anatomic dead space vol.)
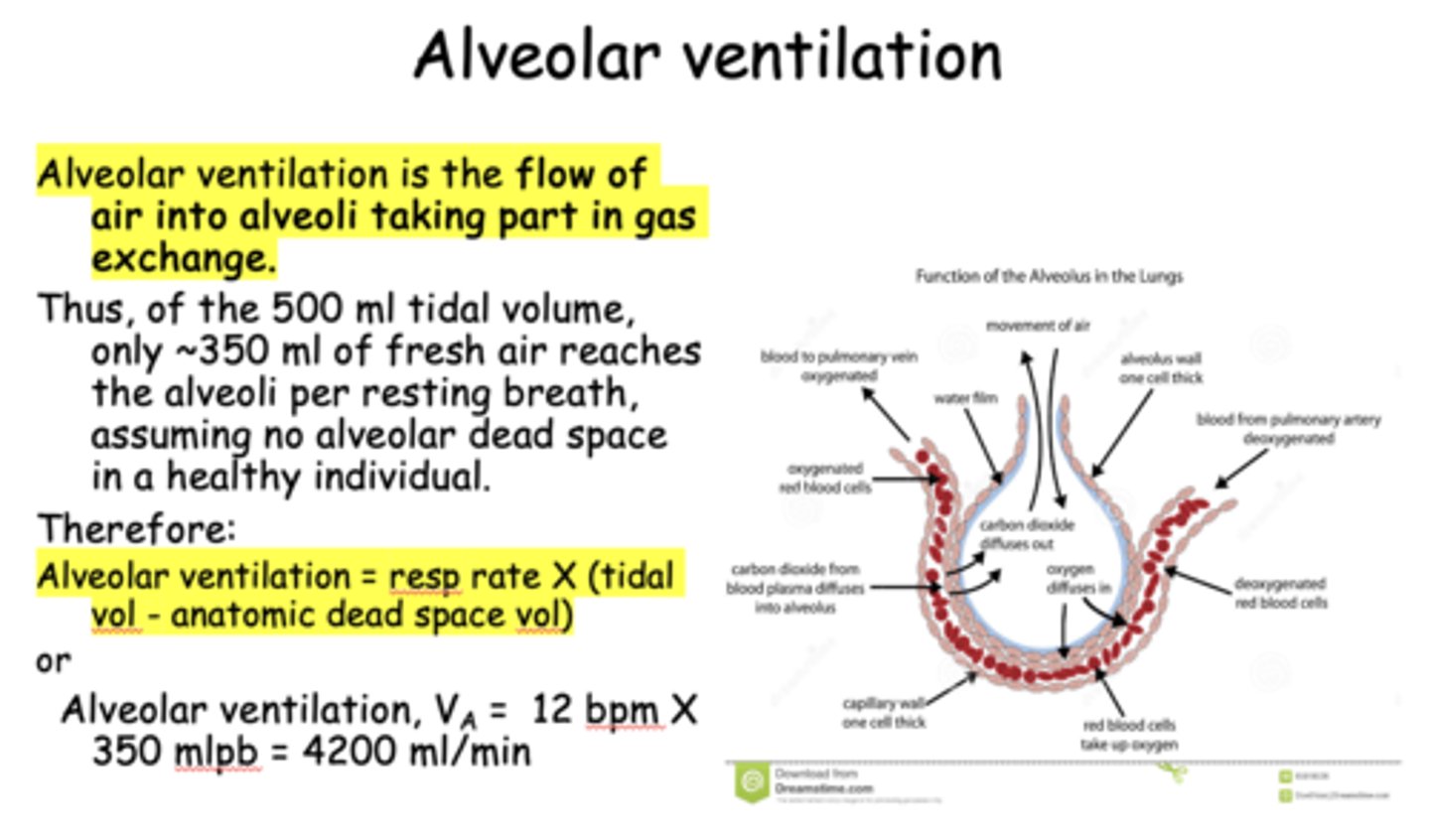
_______ is the flow of air into alveoli taking part in gas exchange
alveolar ventilation
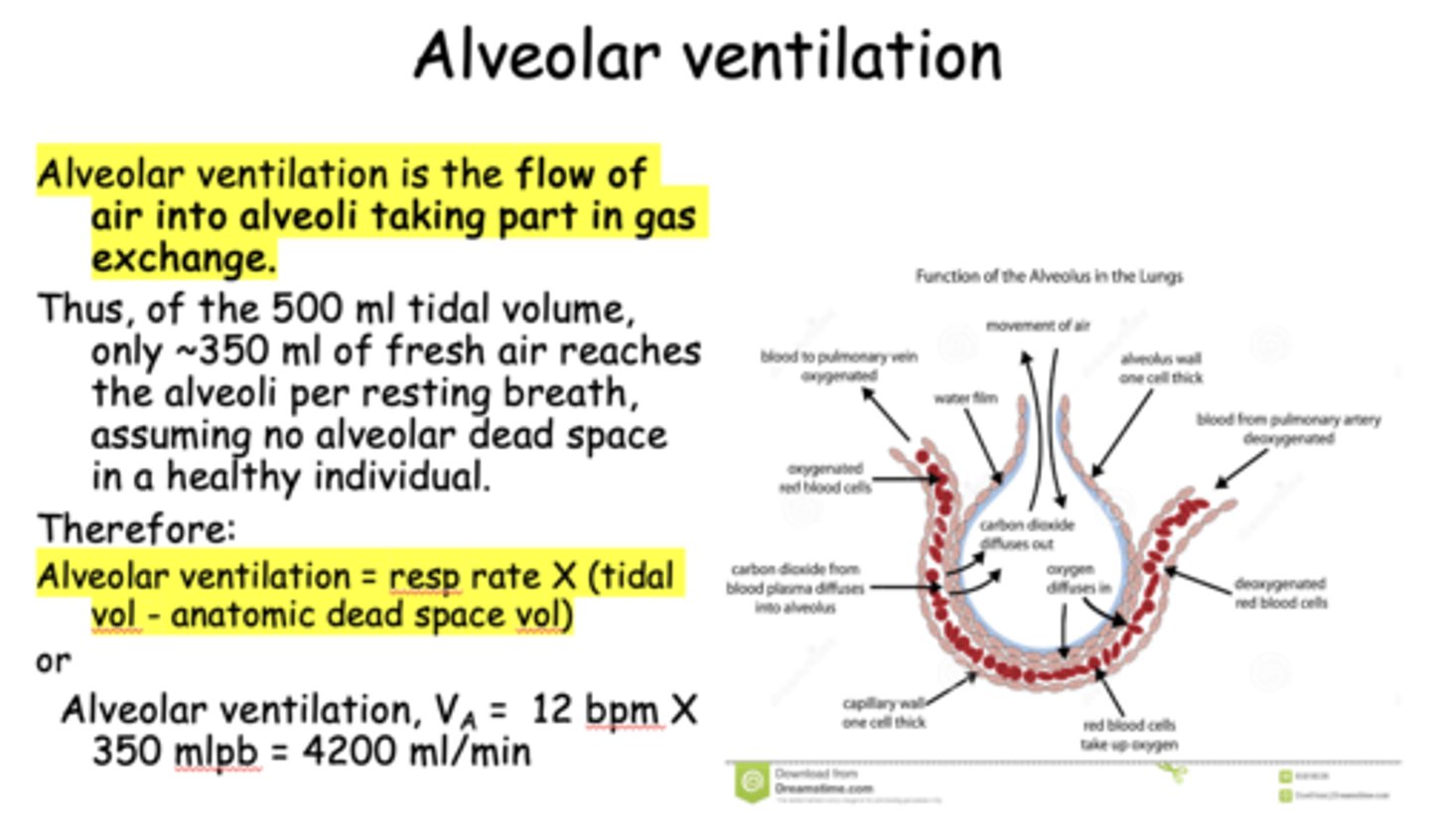
What is the typical rate of alveolar ventilation?
4200 ml/min
________ must be adequate for removal of CO2 produced by cellular metabolism
alveolar ventilation
PACO2 at any point reflects the balance between:
CO2 production and removal by ventilation
PACO2 has a direct relationship with _______
CO2 metabolic production
PACO2 has an _________ relationship with alveolar ventilation
Indirect
if alveolar ventilation decreases, PACO2 will _______
increase
if alveolar ventilation increases, PACO2 will _______
decrease
an increase in alveolar ventilation (breathing rate) that results in a decreased PACO2:
hyperventilation
a decrease in alveolar ventilation (breathing rate) that results in an increased PACO2:
hypoventilation
what is the most important factor affecting airflow?
resistance (r^4)
what 3 factors affect airflow?
- Airway resistance
- Turbulance at branch points in the airways
- Bronchial smooth muscle tone
Parasympathetic/cholinergic stimulation effect on the lungs:
bronchconstriction
Sympathetic/adrenergic stimulation effect on the lungs:
bronchodilation
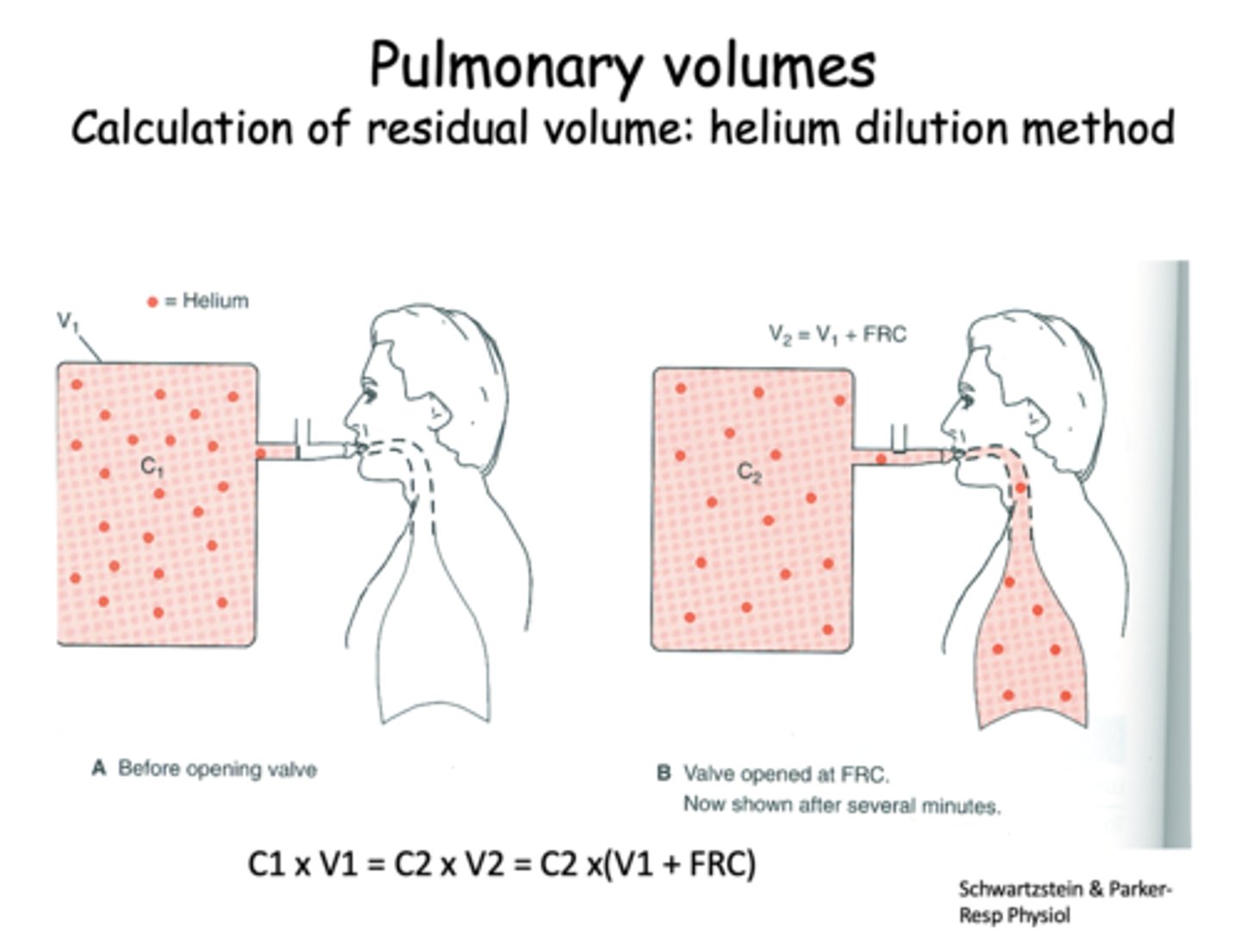
how to measure residual volume?
c1 X v1= c2 x V2 = c2 x (v1+FRC)
helium dilution method
Define the following:
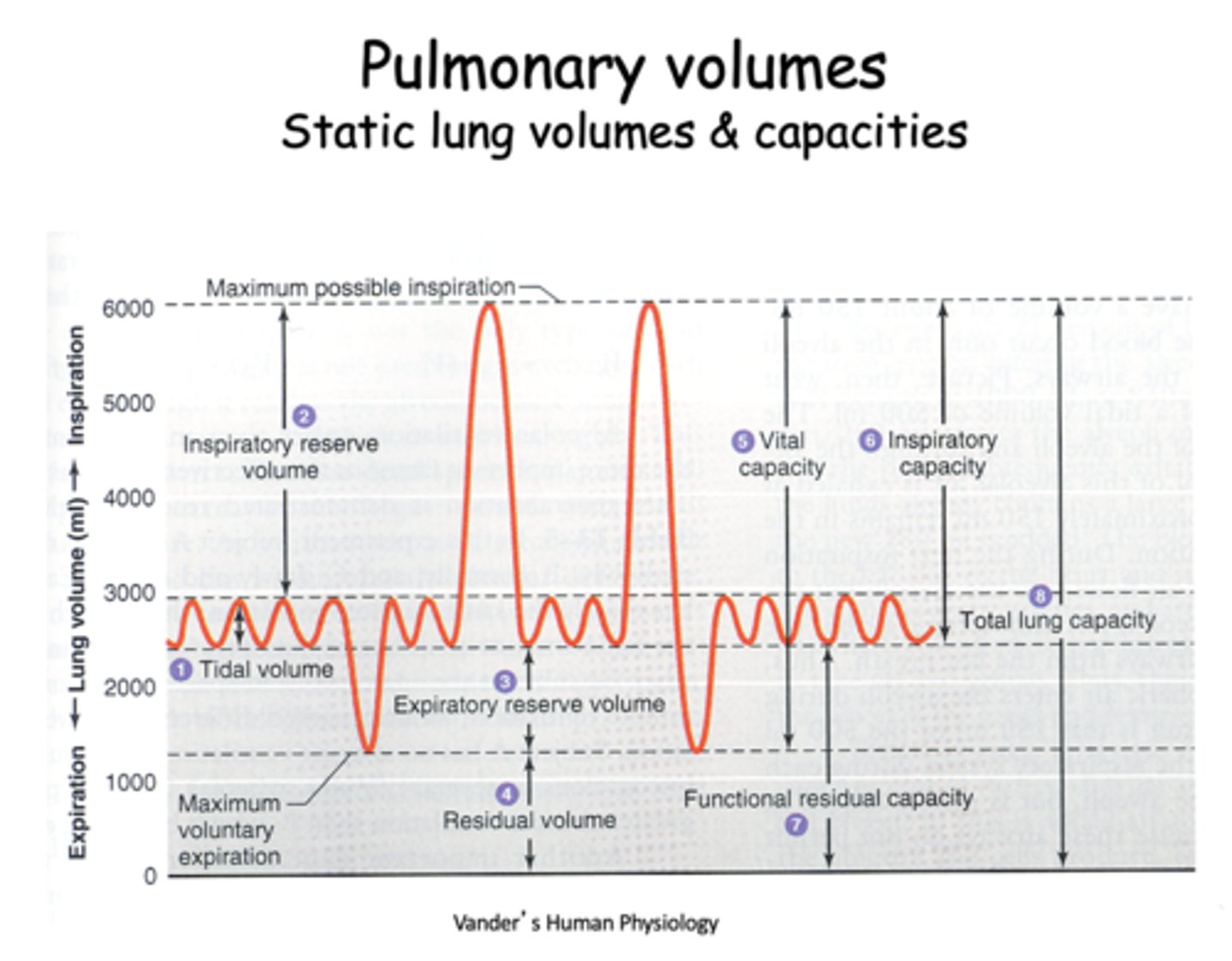
Volume of a single expired breath (500mL)
tidal volume