Biological Factors in Osseointegration and Treatment Planning for Dental Implants
1/89
Earn XP
Description and Tags
Flashcards on the biological factors influencing osseointegration and treatment planning for dental implants.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
90 Terms
Osseointegration
An anchorage mechanism by which bone grows on the surface of a foreign body made of titanium, allowing for the support of prosthetic components
Three Components of Osseointegration
Careful planning
Meticulous surgical technique
Skillful prosthetic management
Host Response
An inflammatory (immune-mediated) process that drives successful osseointegration, involving various cells and mediators
Inflammatory Process
A key driving factor in osseointegration; involves protein adsorption that aids tissue integration with biomaterials
What happens after the foreign material is placed in the body?
Recruitment of granulocytes, mesenchymal stem cell, and monocytes / macrophages
What does the PDL do?
Highly sensitive - indicates pressure and pain; ranges in width from 0.15 to 0.38 (thinnest part is in the middle 1/3 of the root). The width decreases with age
What makes implants different than teeth?
The fibers around implants are different
Perpendicular around teeth, circular gingival fibers around implants
Lack of PDL

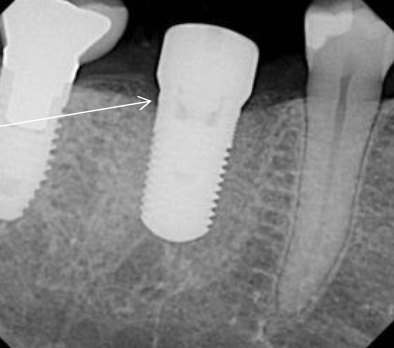
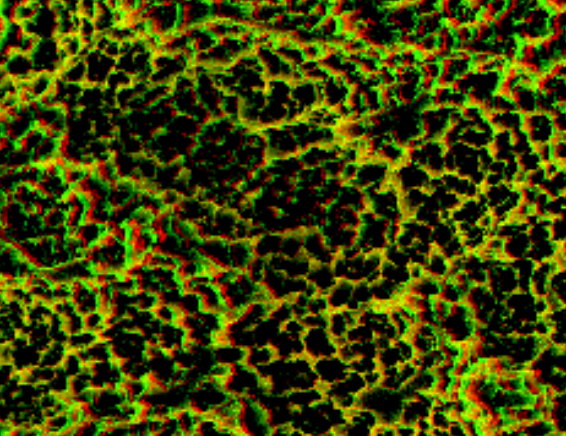
What are you measuring here?
How thick the gum tissue is above the bone
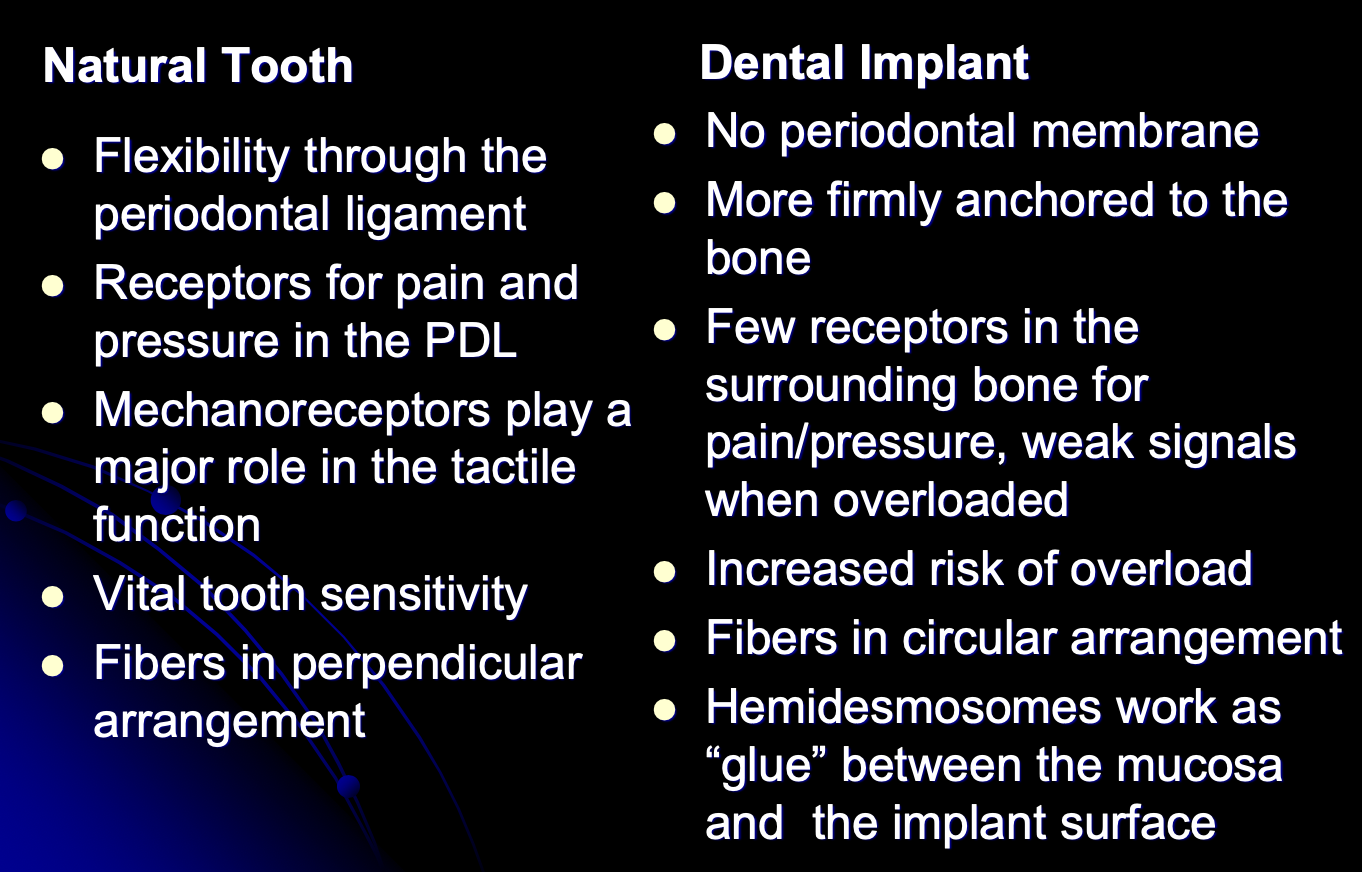
Differences between Natural Tooth and Dental Implant
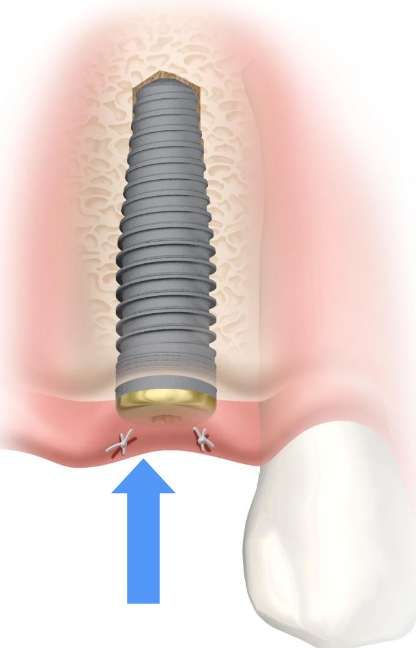
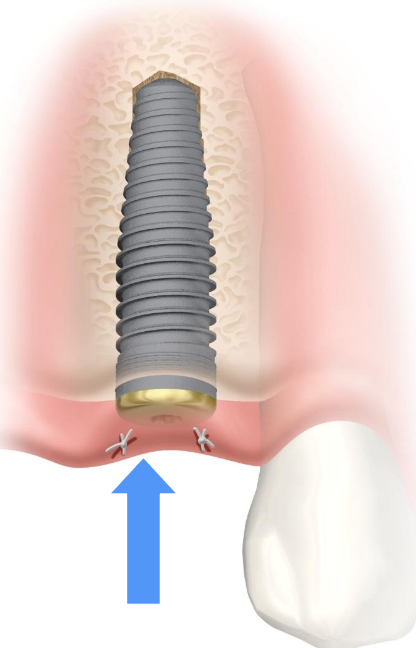
What is the surgical procedure for implants?
Wound creation
Heat control
Irritation
Why do you not irrigate during the finalization of the osteotomy?
Because we want blood flow; water will wash that away
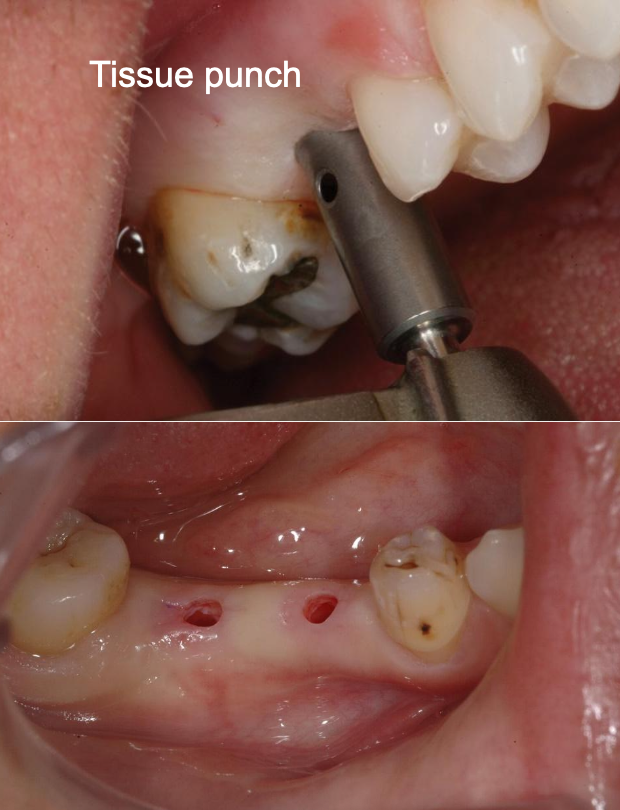
What are the advantages of a flapless surgery?
Minimally invasive surgery
Less trauma to the hard and soft tissues- reduced postoperative symptoms, reduced risks of peri-implant bone loss
Maintained blood supply to the bone: major supra-periosteum vessels, and the vessels of the alveolar bone.
Less bleeding- easier to view the surgical field
Less risk of scarring and gum tissue recession
Reduced surgical time

What are the disadvantages of a flapless surgery?
Requires advanced diagnostics- CBCT
Requires fabrication of precision surgical guide
Requires meticulous planning using expensive computer software
Requires special drills and surgical equipment-sleeves and longer drills
More expensive $$$ compared with conventional implant surgery
Does not allow complete view of the bone surrounding the osteotomy
Risk of overheating the bone – preparation of the osteotomy requires continued use of the surgical guide
Why is local infiltration anesthetic an important surgical consideration?
Temporarily reduces blood supply
What is a surgical consideration when doing an incision and reflecting a flap (osteotomy)?
Damage can cause swelling in the tissue
What is a surgical consideration when tissue is affected by friction heat?
Provides an ideal habitat for microorganisms (spirochetes, gram anaerobes)
Some criteria to minimize surgical trauma during osteotomy
Avoid hard pressure during the osteotomy
Sharp drills- check recommendations by manufacturer
Low speed- follow recommendations by manufacturer (600-800 rpm)
Copious irrigation
“Pumping” movements during osteotomy to rinse from debris and improve cooling of the drill
What is the wound healing process after surgical implant placement?
Thermal and mechanical trauma
Hematoma
Necrotic zone
Minor inflammatory response
Primary Osseointegration
The initial mechanical stability achieved when the implant is first placed into the bone.
Secondary Osseointegration
The biological process of replacing the initial bone matrix with mature, mineralized bone around the implant.
Biocompatibility
The capability of an implanted prosthesis to exist in harmony with tissue without causing detrimental changes.
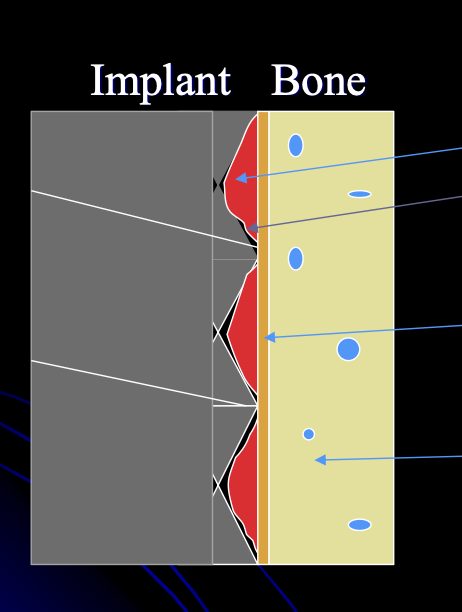
Necrotic Zone
A region of injured tissue between the bone and implant characterized by a mix of healthy and damaged cells.
Frictional Heat
High temperatures generated during drilling and cutting in jaw bone that can lead to protein coagulation and necrosis.
Ridge Preservation
A technique to maintain bone architecture following tooth extraction to support future implant placement.
Osteoblasts
Cells responsible for the formation of new bone
Mesenchymal Stem Cells
Undifferentiated cells that can be stimulated to become osteoblasts.
Osteoclasts
Cells that dissolve bone
Osteocytes
Cells in the living bone (lacunas) that participate in the remodeling process (osteocytic osteolysis)
What are the criteria for the bone healing process?
Presence of adequate cells
Presence of proper nutrition to these cells
Presence of proper stimulus for bone repair
What is re-vascularization?
The process where new blood vessels grow into necrotic (dead) bone
What must happen for blood vessels to invade necrotic bone?
Osteoclasts must resorb the necrotic bone
Osteoblasts must produce new bone
What happens when blood supply is poor?
Proliferation (growth) of fibrous tissue instead of healthy bone.
Why is re-vascularization important in bone healing?
It allows removal of dead bone and formation of new, healthy bone
What is the rate of vascular penetration in cortical bone?
~0.05 mm per day
When does bone remodeling begin at the implant surface?
About 10 days after implant placement
What is the size of the necrotic zone around an implant?
Approximately 0.5 mm
How long does it take for all necrotic bone to be replaced?
Several months
What eventually replaces the necrotic bone?
New, fully mineralized bone
What are the criteria for proper implant-bone healting?
Presence of healthy adequate cells
Proper nutrition
Adequate stimulus (triggered by the inflammatory response)
Proper implant-bone stability (= initial implant stability)

Osseoshaper Drill
A drill used to finalize the osteotomy with a slow speed to minimize traumatic impact on surrounding bone (do not exceed 800 RPM- no irrigation).
Why is slow-speed site preparation used?
It minimizes surgical trauma to the surrounding bone
What beneficial material is preserved with slow-speed drilling?
Bone chips and osseous coagulum
What is osseous coagulum made of?
A blend of blood, osteocytes, osteoclasts, and growth factors
Why is it important that bone chips and coagulum are not washed away?
They help promote healing and bone formation
How does Osseoshape preparation improve implant outcomes?
It creates very tight implant–bone contact
What is the result of tight implant–bone contact?
Increased implant stability
Mucointegration
The stabilization of mucosal tissue surrounding an abutment, important for protecting the underlying bone.
Surgical Guide
A template used to assist in precise positioning during surgical procedures, particularly in implant placement.
Wound Healing Process
The body's response to surgical implantation involving hematoma formation and inflammatory response
What is the difference between the Osseodirector and Osseoshaper?
Osseodirection is parallel sided that cuts at the tip, osseoshaper is tapered and can cut both at tip and side of drill
What is the potential benefit of an aggressive thread?
Creating superior implant-bone contact and minimizing the necrotic zone
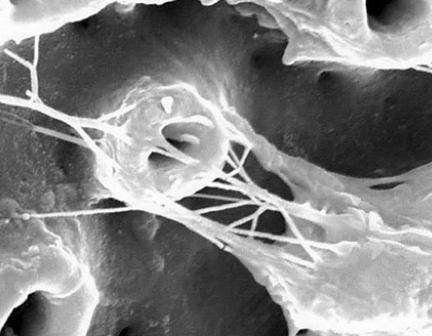
This is an example of failing implant-bone healing
Fibrous granulation tissue
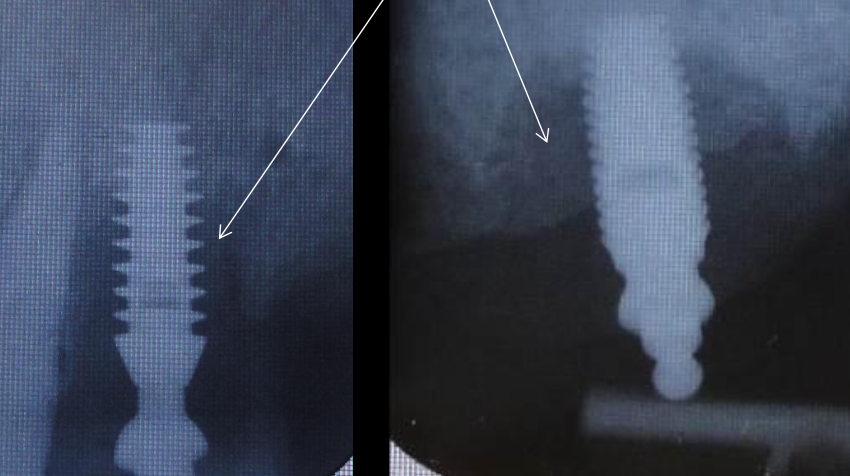
What is the bone tissue response?
Fibrous tissue formation may occur ):
Non-vital bone may remain without revascularization ):
Bone healing will ensue :)
What is the success criteria for dental implants?
No implant mobility (No periodontal ligament)
No peri-implant radiolucency
Marginal bone loss not exceeding 0.2 mm after the first year
Absence of pain, infections, paresthesia or neuropathies
What are the critical factors of bone-implant interface?
Biomaterial- Biocompatibility
Titanium has low corrosion due to tenacious surface oxide layer (5-10 micrometers)
Surface chemistry and cleaning
Bone volume and quality
Implant length
Implant design (threaded-non threaded, cylindrical- tapered)
Implant surface texture
Initial implant stability
What does biocompatibility mean?
The ability of an implanted prosthesis to exist in harmony with tissue without causing harmful changes
Why doesn’t the body reject a biocompatible implant?
The immune system recognizes it as “part of the body.”
What is key for a strong bone–implant interface?
A stable oxide layer on the implant surface
Why is the oxide layer important?
It allows mineralized bone to be deposited onto the implant
What happens when metals corrode in the body?
Metal ions are released into surrounding tissues
What is the result of metal ion release?
Inflammatory responses
How common is allergy to titanium implants?
Very rare—if it exists at all
What does the literature show about titanium allergy?
Only two papers provide strong evidence of allergy to CP (commercially pure) titanium
Why is diagnosing titanium allergy difficult?
There are no universally accepted or reliable patch tests
How does CP titanium behave when placed in living tissue?
It acts as a foreign body
What may contribute to marginal bone loss around implants?
Possible immunological reactions
Why is marginal bone loss around implants hard to define?
There is no universally accepted definition for its causes
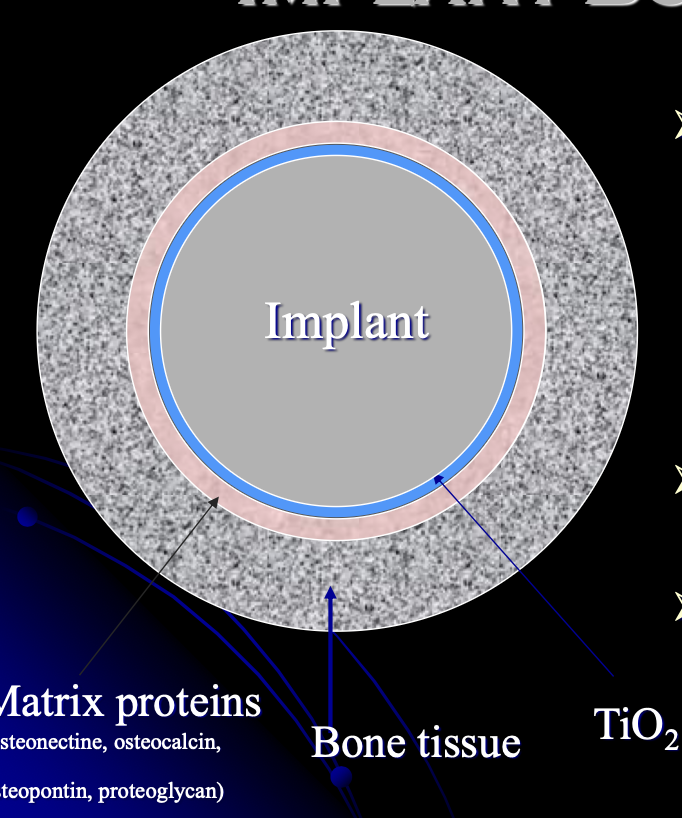
What is the implant and bone contact?
Intimate contact between extracellular matrix produced by Osteoblasts, and the Titanium oxide surface (100 Å)
1 Å = one ten-billionth of a meter
Increased oxide thickness with time (5- 200 micrometer)
What is primary integration determined by?
Implant design, shape and length
Surgical techniques and skills
Surface area and characteristics
Bone volume and quality
What are the benefits of using a threaded vs cylinder shape?
Threads provide superior initial implant stability
Threads increase implant surface area
Threaded implants show improved faster osseointegration
Less bone loss seen overtime

Which one of these is better?
No significant difference in stability. Tapered usually used for maxilla, parallel for mandibular, but studies showed no real difference in mandible
Why must an implant be protected during healing?
To prevent excessive micro-movement
What is the acceptable amount of implant micro-movement during healing?
No more than 50–100 µm
What should be avoided during implant healing?
Harmful overload (excessive force)
What happens if implant micro-movement is too high?
Increased risk of epithelial down-growth
Formation of fibrous tissue around the implant
Impaired osseointegration
What type of implant surface is preferred?
A moderately rough implant surface
Why is a moderately rough surface beneficial?
It increases the implant’s surface area
How are implant surfaces made rough?
By techniques such as sandblasting, etching, and plasma spraying
How does a rough surface affect bone cells?
It stimulates osteoblast activity and promotes new bone formation
What clinical advantage does a moderately rough implant surface allow?
Early or immediate loading of the implan
What is the ideal size of surface grooves?
Approximately 1–5 µm
On average, how much of a successful implant surface is in direct bone contact?
About 50%
What is the typical range of bone–implant contact in a stable implant?
30%–70%
Does bone contact vary between implants?
Yes, it varies depending on the position of the implant site
What does “intimate bone contact” mean in osseointegration?
Direct contact between bone and the implant surface, indicating stability and success
What are some methods to determine osseointegration?
Mobility
Clinical symptoms, pain when manipulated
Radiograph
Simple “tap” test (dull sound indicates lack of osseointegration)
Reversed torque-test using manual or electric torque device
Resonance Frequency Analysis- high frequency sonic energy (tuning fork)

What does this mean?
Why is firm soft-tissue contact with an abutment important?
It acts as a barrier that protects the underlying bone
What implant surface features promote soft-tissue attachment?
Surface chemistry (phosphate & hydroxyl groups)
Surface topography

How does keratinized mucosa affect peri-implant health?
More keratinized mucosa = fewer bacteria can penetrate