(27.15) Regulation of Female Reproductive System
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
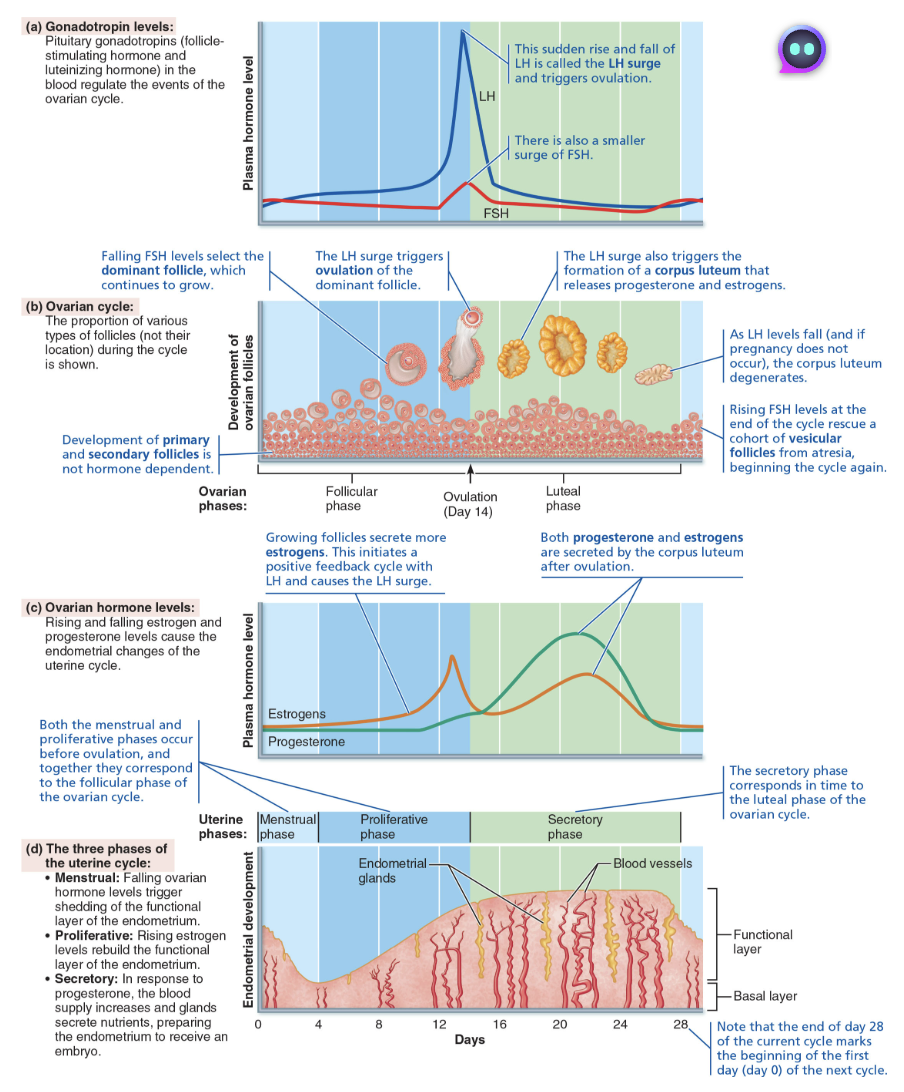
Describe Establishing the Ovarian Cycle
Before puberty, ovaries secrete small amounts of estrogen
As puberty nears GnRH is released stimulating FSH and LH release by pituitary that then acts on ovaries
Events continue until an adult cyclic pattern is achieved and menarche occurs
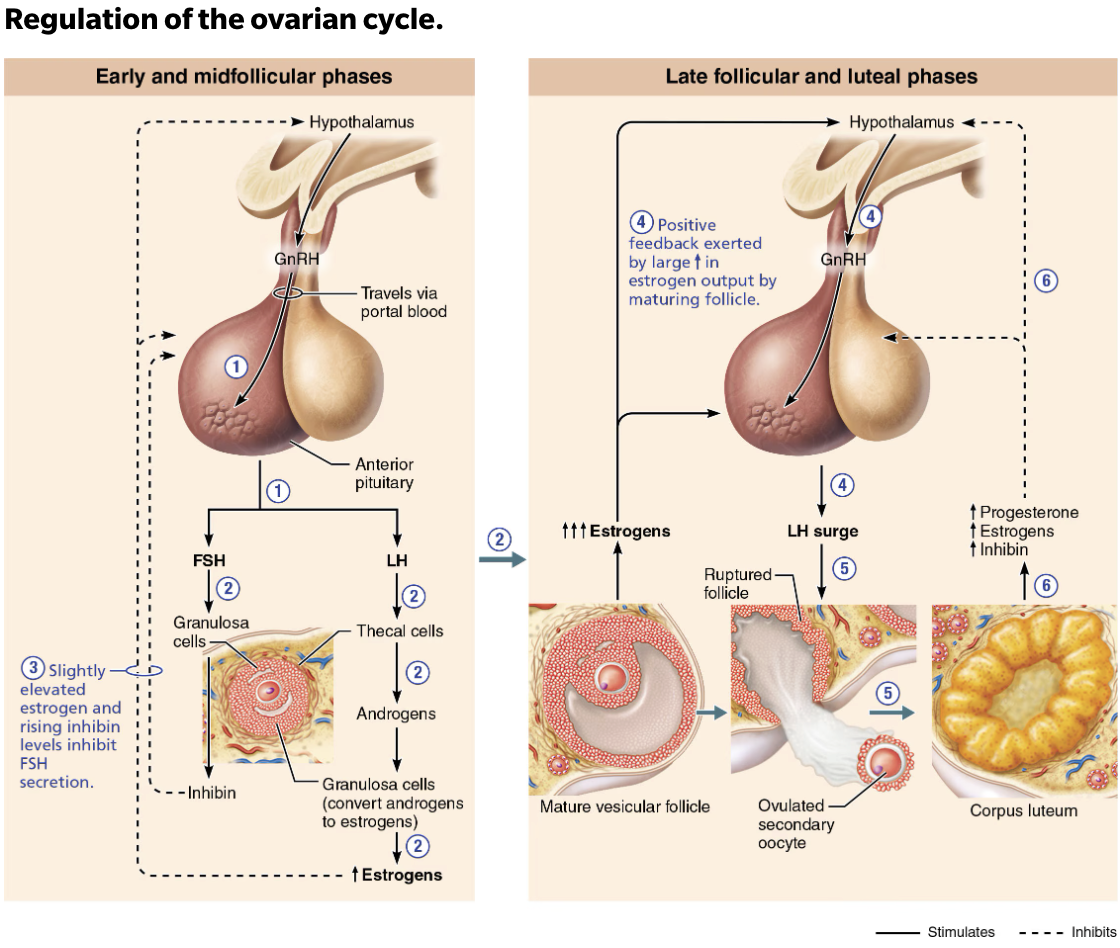
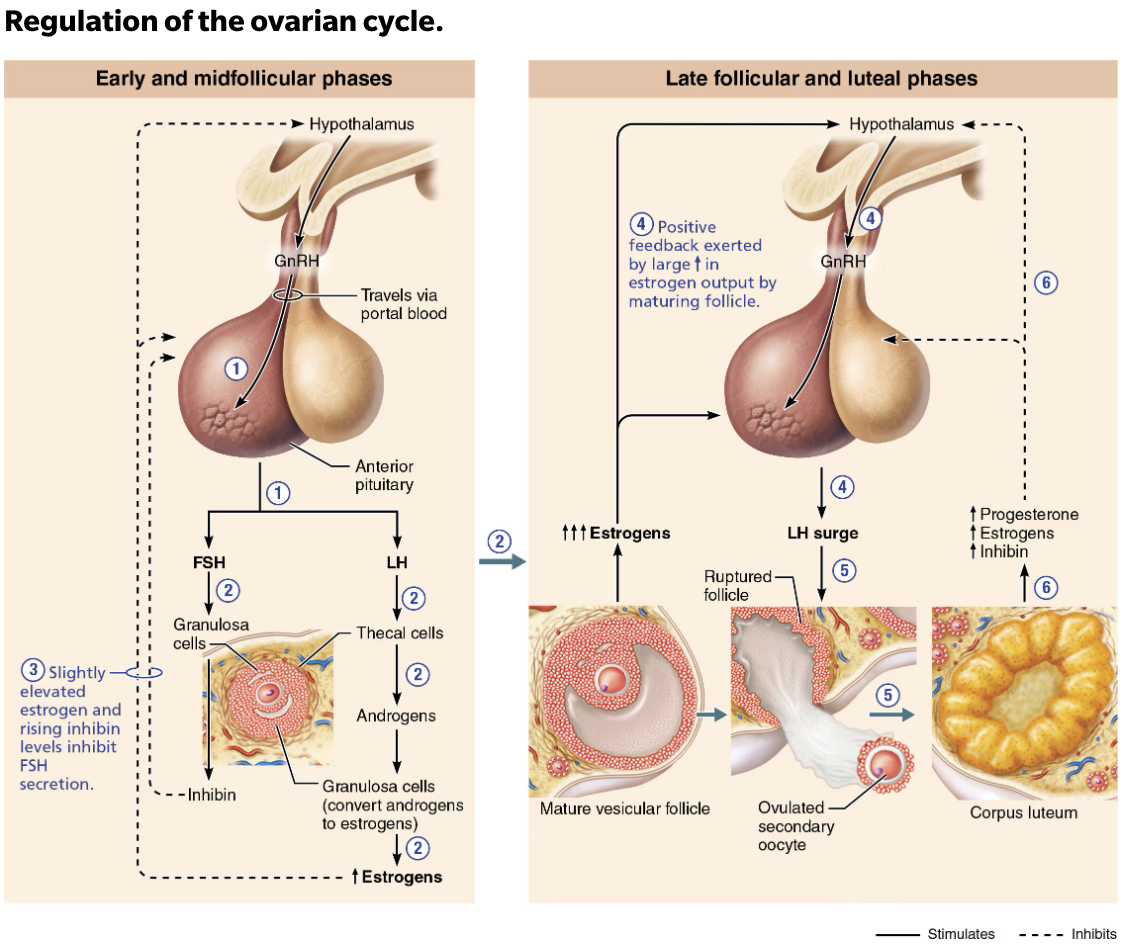
Describe the regulation of the ovarian and uterine cycles.
GnRH stimulates FSH and LH secretion
FSH and LH stimulate follicles to grow, mature, and secrete sex hormones
FSH stimulates granulosa cells to release estrogen and LH prods thecal cells to produce androgens, which granulosa converts to estrogens
LH surge triggers ovulation and formation of the corpus luteum
Surge triggers ovulation:
LH surge triggers
primary oocyteto complete meiosis I to become secondary oocyteSecondary oocytethen enters meiosis II, continuing on to metaphase II
Shortly after ovulation:
Estrogen levels decline
LH transforms ruptured follicle into corpus luteum
LH stimulates corpus luteum to secrete progesterone and some estrogen almost immediately
Negative feedback inhibits LH and FSH release
Negative feedback from rising plasma progesterone and estrogen levels inhibits LH and FSH release
Inhibin, from corpus luteum and granulosa cells, enhances inhibitory effect
Declining LH ends luteal activity and inhibits follicle development
Describe if no fertilization occurs
Corpus luteum degenerates when LH levels start to fall
Causes a sharp decrease in estrogen and progesterone, which in turn ends blockage of FSH and LH secretion → causing to start all over again
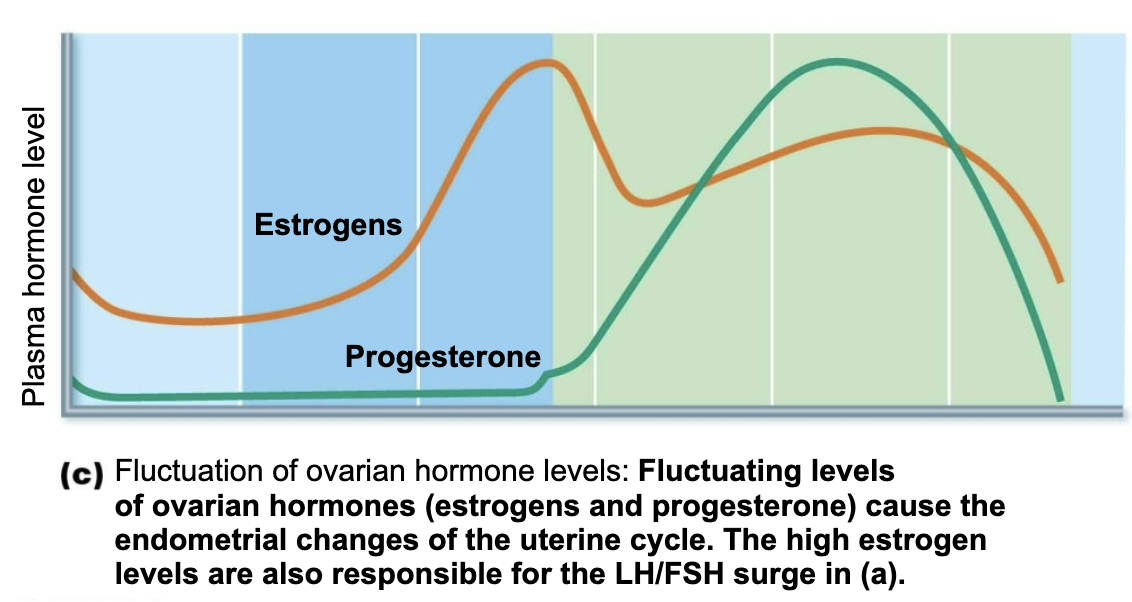
Discuss the physiological effects of estrogens and progesterone.
Helps maintain stratum functionalis
Maintains pregnancy, if it occurs
Define Uterine Cycle
Menstrual Cycle
Cyclic series of changes in endometrium that occur in response to fluctuating ovarian hormone levels
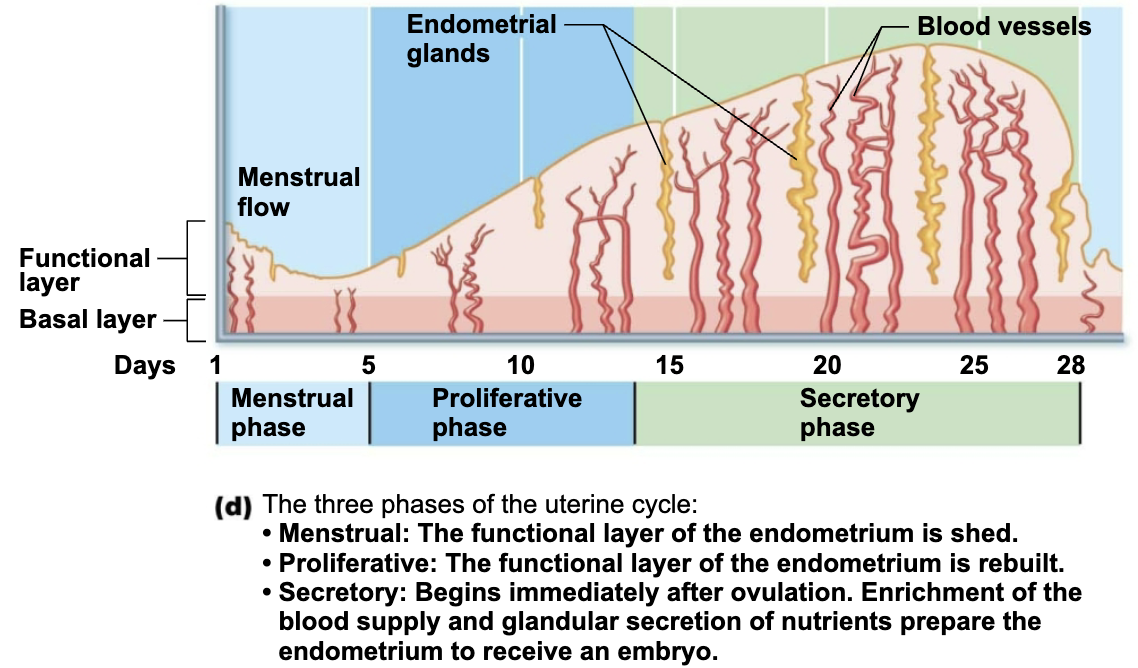
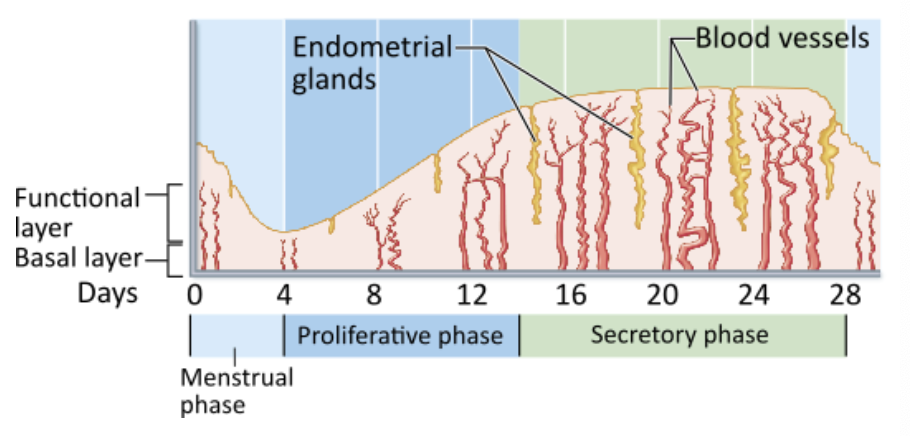
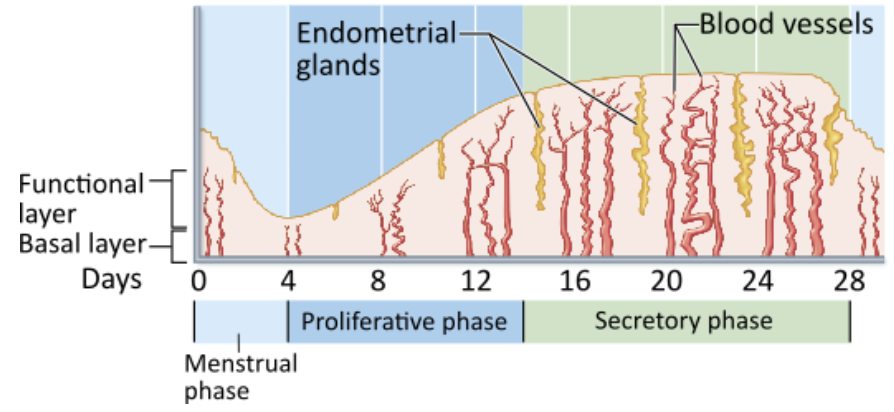
Describe the Phases of the Uterine Cycle
Days 1-5: Menstrual phase
Ovarian hormones are at lowest levels
Gonadotropin levels are beginning to rise
Stratum functionalis detaches from uterine wall and is shed
By day 5, growing ovarian follicles start to produce more estrogen
Days 6-14: Proliferative (preovulatory) phase
Rising estrogen levels prompt generation of new stratum functionalis layer
As layer thickens, glands enlarge, and arteries increase in number
Estrogen also increases synthesis of progesterone receptors in endometrium
Thins out normally normally thick, sticky cervical mucus to facilitate sperm passage
Ovulation occurs at end of proliferative phase on day 14
Days 15-28: Secretory (postovulatory) phase
Phase that is most consistent in duration
Endometrium prepares for embryo to implant
Rising progesterone levels from corpus luteum prompt:
Functional layer to become a secretory mucosa
Endometrial glands to enlarge and secrete nutrients into uterine cavity
Thickened mucus to form cervical mucus plug that blocks entry of more sperm, pathogens, or debris
If fertilization does not occur:
Corpus luteum degenerates toward end of secretory phase; progesterone levels fall
Causes arteries to kink and spasm
Endometrial cells die, and glands regress
Arteries constrict again, then relax and open wide, causing a rush of blood into weakened capillary beds
Blood vessels fragment, and functional layer sloughes off
Uterine cycle starts all over again on first day of menstruation
What event coincides with the transition from the proliferative phase to the secretory phase?
→ Ovulation occurs
Ovulation of the oocyte from the ovary occurs at around day 14 of the cycle, just as the uterine proliferative phase ends and the secretory phase begins.
During what phase of the female's uterine cycle is the uterine lining shed?
→ Menstrual phase
The functional layer of the endometrium is shed during days 1 through 5 of the uterine cycle, a process called menses or menstruation
Explain Effect and Cause of Amenorrhea
EFFECT
Cessation of menstruation
CAUSE
Extremely strenuous physical activity can delay menarche in girls and disrupt normal menstrual cycle in adult women
Explain Cause and Effect of Homeostatic Imbalance of Adipose cells
CAUSE
Female athletes have little body fat; adipose cells are needed to convert adrenal androgens to estrogens
Also, leptin plays role in female puberty → informs hypothalamus if energy stores are sufficient to support reproduction
EFFECT
If they are not, reproductive cycles are shut down
Effects of Estrogens
Promote oogenesis and follicle growth in ovary
Exert anabolic effect on female reproductive tract
Support rapid short-lived growth spurts at puberty
Cause the epiphyses of the long bones to close during growth spurts in puberty
Induce secondary sex characteristics
Growth of breasts
Increased deposit of subcutaneous fat (hips and breast)
Widening and lightening of pelvis
Metabolic effects
Maintains low total blood cholesterol and high HDL levels
Facilitates calcium uptake
Effects of Progesterones
Works with estrogen to establish and regulate uterine cycle
Promotes changes in cervical mucus
Effects of placental progesterone during pregnancy
Inhibits uterine motility
Helps prepare breasts for lactation