Nutrition for the critically ill and GI ALTERATIONS
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
34 Terms
Differentiate between enteral and parenteral nutrition, including nursing/medical interventions with each.
look at ipad- notes . Ch 18
What is the Nutritional status of the critically ill
NPO status
The patient is in a hypermetabolic state in some disease or illness states, barriers to achieving optimal enteral nutrition, and the need for parenteral nutrition.
What are the patient goals
•Adequate nutrition to promote resolution of illness, wound healing, and physical strength. laying in bed will make you weaker
• Maintenance of baseline body weight.
• Nitrogen state is balanced or positive.
WHat interventions do we do
•Baseline Height, Weight, and BMI upon admission ot the critical care area.
•Daily Weights
•Consult with dietitian, clinical pharmacist, and other team members to generate a nutrition care plan.- for ex. if tube keeps getting clogged
•Assess bowel sounds, abdominal distension- measure girth and intake/output on a regular basis.
What is Parenteral and Enteral Nutrition
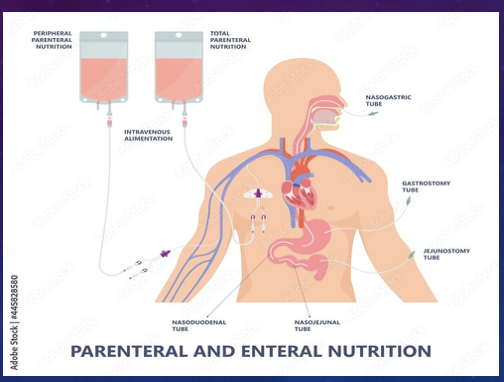
parenteral- into large bore vein
Enteral- through gut
what is enteral nutrition
•Tubes: main reason is to decompress the gut so that it does not interfere w heart or resp system. removes air, bile, fluids from the stomach. prevents N/V, dissension. , used post op for bowel obstructions- so gut can rest , can give meds to start up gut. ER-put tube for overdose - pump stomach and suck it out.
Always document color of the stuff in the tube, label canister at bedside,
Enteral
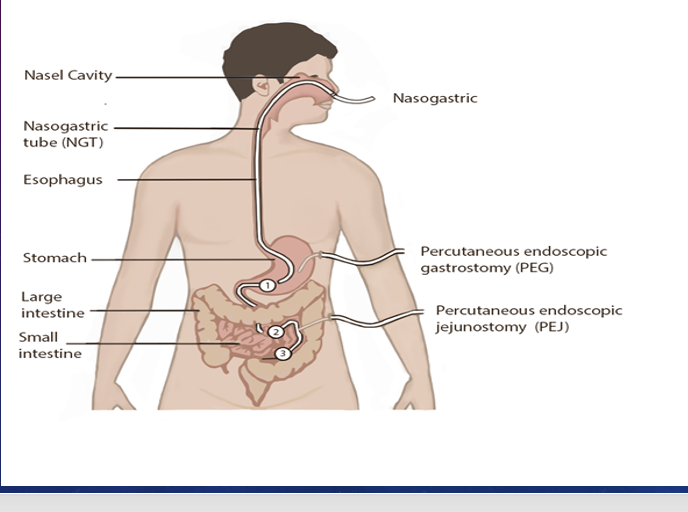
•OGT- best choice if intubated compared NGT. Mouth
•NGT- germs are in nose- can put germs down - increases likely hood of ventil acquired pneumonia. Hard to get it down with ETT. Measure tube nose to ear, gut, ask pt to swallow, short term use less than 3/4 wks . nose toute, short term, not for intubation sinusitis
to know in right place- x ray- gold stanadrd, ph test, aspiration
Small Bowel Feeding Tubes
jejunal feeding tube- when at risk for aspiration- bypass stomach and go directly to small intestine- good for neuro pts, had strokes, brain injury, delayed gastric empty, severe GERD, gastropersis, GI tumors. cool tac- helps guide tube into right spot. ( maybe dont have to know), magnetic one- accurate. used for high aspiration risk, require advanced training
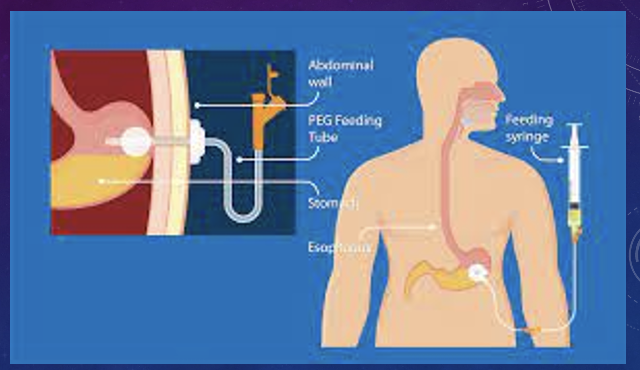
PEG- by Dr Stomach through abd wall, , as long normally fx GI tract > 4wks.
always doc placement, drainage, tube length, pt tolerance.
Nutrtion is a therapeutic intervention - lowers risk pnuemonia , reduces mortaltiy, keeps intergrity of gut stronger and normal flora, decreases hospital stays , we are the advocates of nutrition. may sure monitored for malnutrition, and not being kept NPO for too long.
if they dont get nutriton- msucle wasting and weakness,, wound wont heal, prone to pressure ulcers and higher incidence of infection.
Enteral feeding- Tube/ gavage feedings- directly into stomach using a tube
best option for any critical care pt. Keeps gut healthy, helps protect the gut from infection- dt healthy flora- bacteria feed on the food we eat, lowers risk for infection, reduces mortality, keeps perestalisis going- nutrition being absorbed and stool is being elimintated, toxins is being eleminated.
Dont do enteral nutrition if have bowel obstruction, severe GI bleeding, paralytic ileus, non functioning gut
if give it to someone who has bowel obstruction- it will back up- have suction available
Its safer, cheaper, more psyologically like feeding
tropic feeding- start a feed around 10-15 ml/hr to test if gut will accept feeding or not, its a test of tolerance. Maintains gut intergirity as it heals Ex. to keep gut awake and give them something- but not full nutrition. Can always go up on feed to make it a targeted hourly rate . Low and slow for tolerance
Targeted Hourly rate- ml/hr-set rate. as tolerated you can increase. if feeding gets paused then they have a pause in nutrition. so can lose volume and calories. Most common but doesnt account for interruptions.
Volume- more flexible, set daily volume goal. ex 1500 ml in 24 hr. if miss a time tex. go to CT for 6 hrs, then have to recalulate it ex. 18 hr divided by 1500- adjust rate to 83ml/hr so can get that volume . If pause it have to adjust rate. for Adjustable, and helps meet nutrition goals even if feedings are paused.
\
HOB at least 30, when we turn pt in ICU stop feeding. dont want residual to come back and go into lungs. gastric resdiual- can cause nutrtion problems, delay feedings. check stomach bowel sounds, vomm/ diarrhea, daily weight, i &0
all tubes- have to worry about aspiration, infection, dislodgment, not going home w NGT
if clogged st not crushed meds let sit warm water and dissolve
What do we monitor after placing enteral nutrition
Tube placement | Administration of EN & meds | Assess | Tube clotting |
X-ray is the GOLD standard initial placement |
Elevate 30-45 degrees while feeding and one hour after bolus feeding | Every 4 hours for placement with residual checks. Flush with sterile water as needed. Monitor bowel sounds. |
Prevention |
Auscultation | Flush 30 mL before and after med admin |
Every 4 hours for placement. |
Flushing PRN |
pH testing- if facility policy requires | Collaborate with pharmacist, provider, and dietitian |
Assess for toleration of feeds. | Limit checking Gastric Residual Volume (GRV) |
1st- check residual
2nd- placement
toleration- are having diarrhea- slow down feed or change in feeding, constipation
for nclex reasons- only check residual if you have probelms such as distended abdomen, vommiting. dont check routinely.
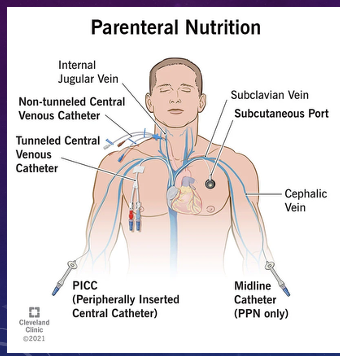
Where does parenteral nutrtion go
Through vein
Total parenteral nutrition (TPN)
Peripherally inserted central catheter (PICC)-
Port
Central venous access
Subclavian, jugular, or femoral
Longer term
10% dextrose- has lot of glucose, high protein helps w healing, vitamin, minerals, add lipids for energy and essential fats - in seperat ebag
Hyperosmolor- thick and concentrated liquid- have to have central line. If do peripher- cause thrombophelbitits . full nutrion, monitor blood sugar closely q 6 hrs, lipids count toward totoal calories
Peripheral parenteral nutrition (PPN)
Midline catheter
Large-bore PIV
Short term partial solution
Lower sugar and osmolality- not as thick, doesnt provide enough nutrition for really sick pts. Physician call.
Given to pt not ventilated, no major heart or lung issues, septic, end stages of heart attack. Sick but not far end.
Lipids
PIV – limited days avoid phlebitis
Central venous catheter- always given bc thicker solution
Watch triglycerides – hold if elevated
Propofol
given q day
What are some nursing considerations with Parenteral Nutrition
•Use dedicated port- dont give meds in TPN line.
•Refeeding syndrome- life threatening electrolyte imbalance cause by reintroducing food too fast in a malnourished pt.
•Monitor electrolytes- when maulnorished get TPN get a lot of glucose pured into body- causes release of insulin . causes cells to reuptake magnesium and K , electrolytes are low. msucle weak dt low k and poshhate, arryhtmias bc low k, and magneisum, cardiac dysfunction bc low phosphate, seizure acitivty dt low mg, dehydation bc high sugar and low fluid content
•Monitor blood sugar- hyperglycemia, hypoglycemia can occur if tpn discontinued immediately - always taper it.
•Document intake
•Weights
•Assess hydration status
•Tubing changes- TPN q 24 hr, even if it isnt completely done
Can get into fluid overload- s/s- hypertnesion, crackles, sob, buld neck veins, edema
A nurse is orienting a new graduate nurse caring for an intubated client in the ICU that has orders to start enteral nutrition (EN). Which statement by the new graduate nurse demonstrates understanding?
a. “I will ensure the client has an x-ray before starting EN.”
b. “I can only use central venous access to administer feed.”
c. “I will hold EN if client starts to have loose bowel movement.”
d. “I will initiate EN if the patient has absent bowel sounds.”
A
•Analyze the pathophysiology, assessment, outcomes, and medical and nursing interventions for gastrointestinal alterations.
•Relate assessment findings to nursing/medical interventions for gastrointestinal bleeds.
WHat are upper and lower bleeds
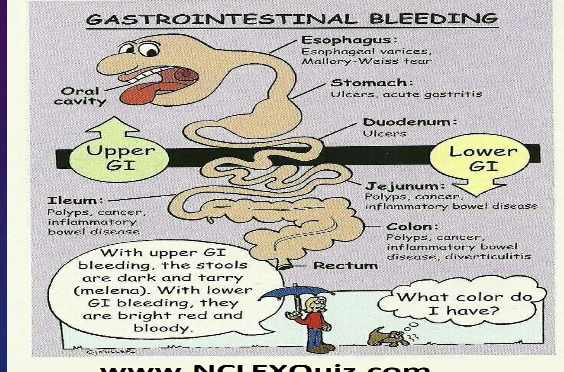
upper- oral cavity, espohagus, dudoenum, stomach. can be from a duodenal ulcer, esoph/gastric varices, gastric ulcer, mallory weiss tear
lower- jejuneum, colon, rectum
cancer, diverticultities, hemmorhoids, chrons, inflamm diseases
What is Peptic Ulcer Disease
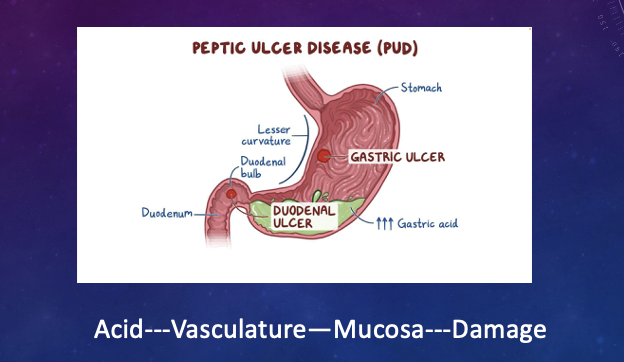
overactive acidic enviornment that damages muscualr layer- erodes muscoa and bleeds- can lead to GI perforation, bleeding into abdominal cavity. can go through muscualr layer. acid being over produced.
caused- secretion acetocholine, gastrin, secretin
reasons- stress, overuse NSAIDS, smoking, drugs like achohol, H pylori- flies carry it.
s/s- abrupt onset abdominal pain, board like rigid abdomen, absent bowel sounds, vommit blood last 2 hrs- would be emergent
What are stress ulcers
•go into flight or flight- steroids make membrance permeable, glucose has inflamm response on muscoa of gut. chronic stress. causes ichemia, ersoion, causes acid
Ischemia related ulcers: causes
•Hemorrhage
•Trauma- physical/mental/emotional
•Burns (Curling’s ulcer)- stress ulcer
•Heart Failure
•Sepsis
Cushing's Ulcers:
•Head trauma
•Brain surgery
ex. have head injury- have a risk for cushing ulcer
What are Esophageal Bleeds
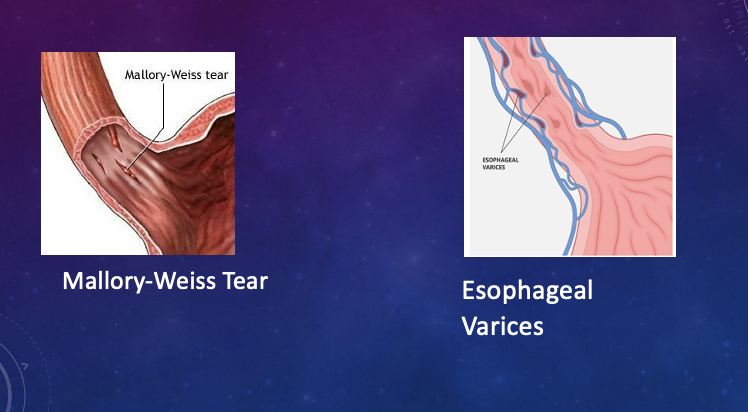
another reason for GI bleeding
upper GI - mallory weiss tear- causes by forecful or prologned vommiting/ wrenching.
bleeding resolves without intervention- on its own
if lacerations ocur at espophageal gastric junction where they connect- can have massive GI bleed- would have to do surgey, or endoscopic type therapy.
What is esophageal varicies
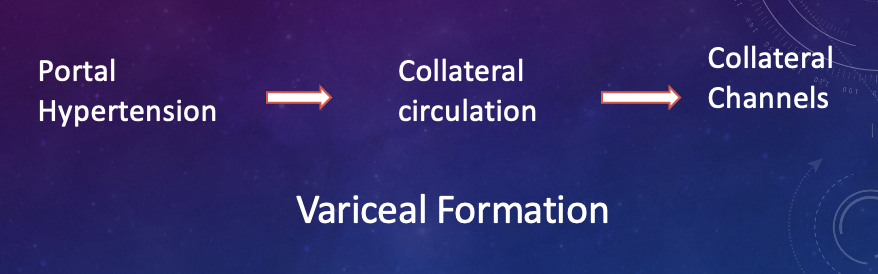
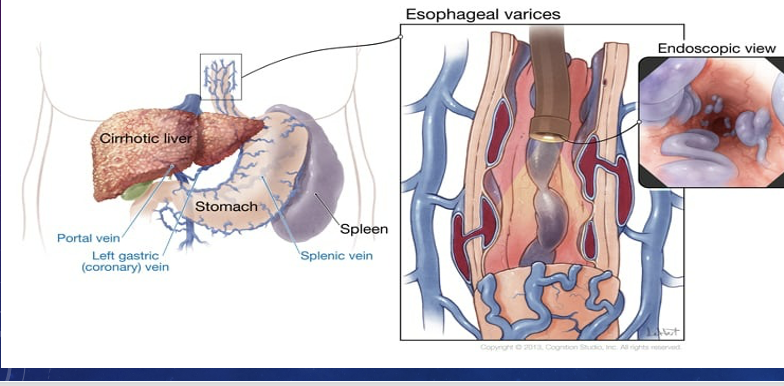
Esophargeal varicies- vein buldging in esophagus. rt liver disease, portal hypertesnion causes blood to shunt, backs up and creates large veins in esophagus to buldge. Blood goes from liver to system cirul to relieve pressue.
veins have increase pressure, enlarge- when portal hypertension > 10mmhg. varicies=chronically buldging.
submucosa of esophagus and rectum - hemmorhais, antterior wall and peritieal peritineum, go to all organs abdomen. veins collterally circulating
WHat are the s/s of a GI bleed?
•Upper: Bright red blood or coffee ground consistency.- blood will digesta little in gut and throw up
•Lower: Hidden or dark/bright red or maroon colored.- vomit
can have blood loss by - vommiting, drainage from NGT, , expelling stool
upper gi- these signs may not be seen if bleeding is stoppedbc of clotting of clotting factors- andcan have expulsion in stool. still have an upper GI bleed it just stopped
comommon s/s of vommiting blood- coffeground
causes for peptic ulvers, esophageal varices, mallory weise tears,
Can have melena- shiny black foul smelling stool
50 ml of blood in stomach can turn the stool black.
occult blood- testing to see if positive or not
What would you assess in a GI bleed
•Vital signs every 15 min
•LOC
•Urine output
•Monitor for S/S of Hypovolemic shock
•Soft or distended abdomen
•Hyperactive bowel sounds bc gut like i want to get rid of it
•
What is blood loss is significant? How will I know?
>1000ML -------
SBP < 100 mmHg
Postural decrease in BP > 10 mmHg- if lay down and bp 120- and stand up it goes to 80/40
HR > 120 BPM
What labs would you look for in a GI bleed
•Lab work: CBC, PT, PTT,- prolonged BMP, Liver enzymes- elevated , Pancreatic enzymes- elevated
•ABG– metabolic acidosis or Reparatory Alkalosis
•Ammonia level- very high
•Calcium- low bc needed for clotting. constantly bleeding
•Lactic Acid- elevated bc tissue hypoxia
•Positive Guaiac/Acidic pH of gastric contents.
Diagnostic procedures
•Upper GI endoscopy
•Lower GI endoscopy
shows sights or bleeding, presence of tumor or inflammation. if inflamm- could be chrons or other diseases- take biposy and send off.
Barium study
What immedicate tx would you do for GI bleed
•Large Bore IV
•LR bolus fluids - give volume 999 ml or on pressure bag . if SBP <90mmg/hg (according to hospital protocol)
•Colloids- albumin to draw plasma into intravasular space
•Crystalloids.- LR, NS
Find the source of bleeding
What tx do we do for GI bleed
•Gastric lavage– decreases bleeding and can identifies source. cleans out stomach
•Antacids
•Histamine antagonists
•PPIs*
•Mucosal barrier enhancers
•Abx
•Surgical interventions- Biliroth 1 and 2- procedure or surgery or cant get ulcer to heal
What are Esophageal Bleeding Treatments
Somatostatin- targest blood vessels of gut. give IV continuously like 26-72 hr & Octreotide

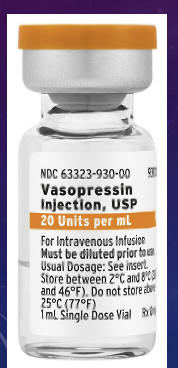
•VASOPRESSIN: synthetic antidiuretic hormone used to lower portal pressure/ hypertesnion. vasconstricts splenic blood vessels and messentary- gut blood vessels. decreases blood flow to portal vein.
What are Endoscopic interventions
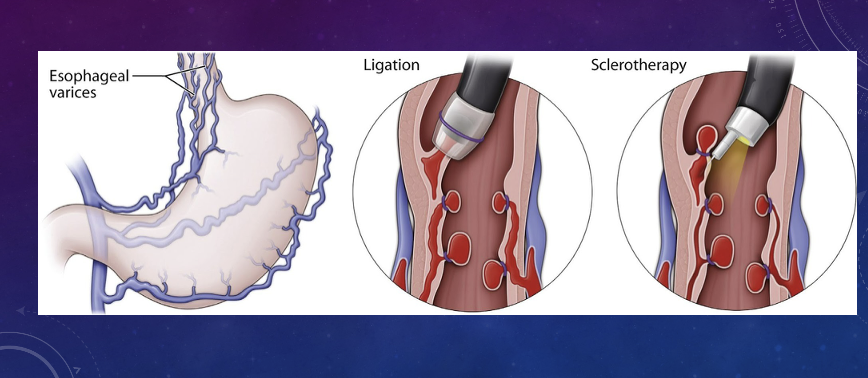
Ligation- tie it off and stops bulding and bleeding
Sclerotherapy- inject saline into veins and collaps them.
What are surgical interventions
•Portocaval shunt
•Splenorenal and mesocaval shunting
shunt everything around where bleeding is
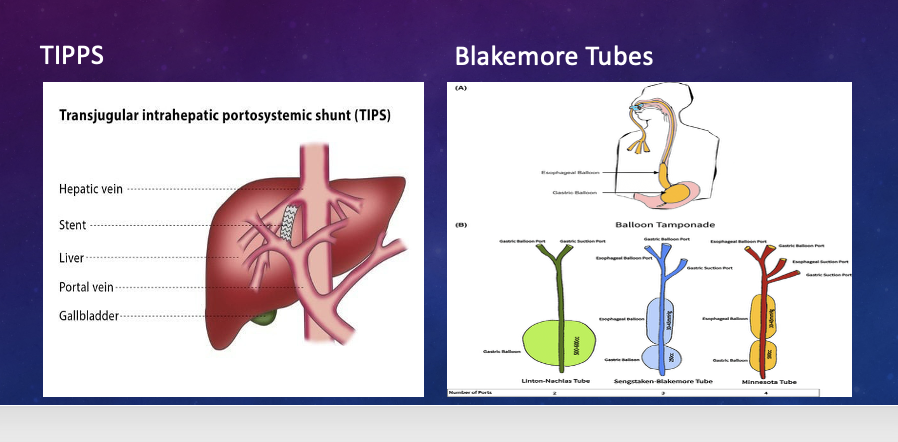
TIPSS- esophageal bleeding
chronic esophageal bleeding- put a blakemore tube- like NGT but has ballons in esophagus and anchorc past pylric valve and applies pressure to where bleeding is. defelate ballon q 8-12 hrs so theres so releif. complications- ruptured ballons- keep scciors at bedside if pts airway becomes compromised used to tx bleeding, and acities from portal hypertesnion, and a bridge to liver transplant.
Objective acute pancreatitis
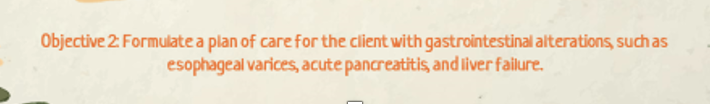
What is acute pancreatitis
enzymes go uo- digests pancreas- leads to inflamm response, release of histamin. instead of digesting food.
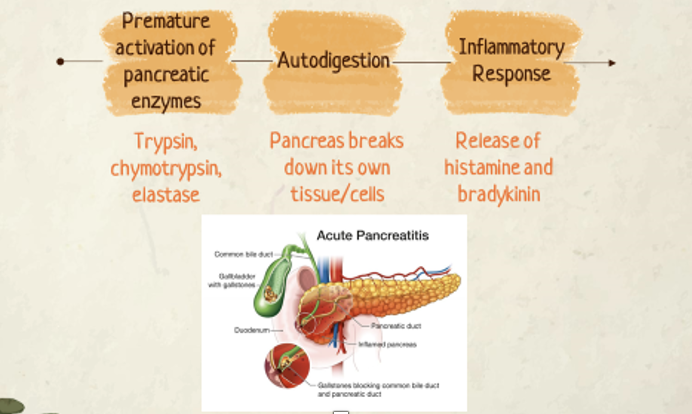
WHat are the causes of acute pancreatitis
cause- alchohol consumption chronic, biliary disease like galbladder, liver, glp1, galstones, cystic fibrosis, smoking, family hx,
What assessment do we for for acute pancreatitis
•Severe pain
• Epigastric or midabdominal
• Radiates to back
•Nausea and vomiting
•Fever
•Dehydration
•Abdominal distention and guarding
•Ascites and jaundice (severe) chronic
•Retroperitoneal hemorrhage- if have bleeding along w it
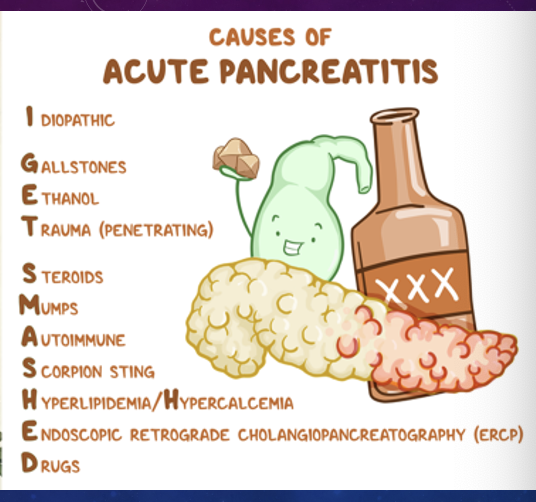
tuner sign- discolation flank
cullen- around umbilic discolartion
brusies from bleeding
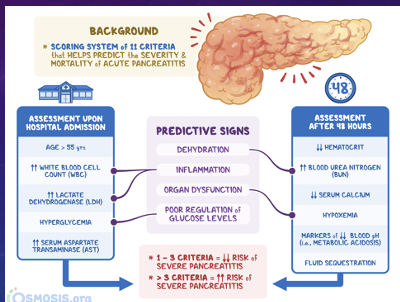
Ranson Criteria Box 18.12
Measure and record abdominal grith q 4 hrs.
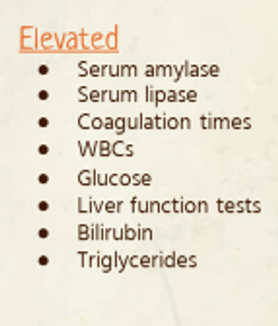
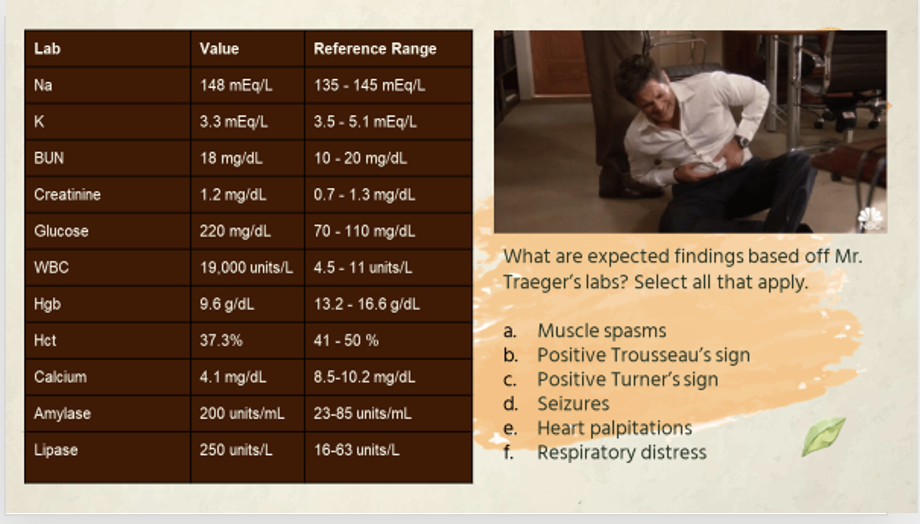
What labs do we see in acute pancreatitis
glucose bc insulin cant get out of pancrease
hypokalemic bc vommiting, hypocalcemic - when pancrease has become fatty and necrosed
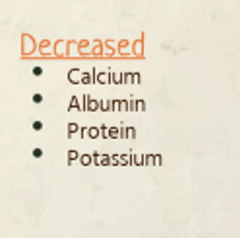
What diagnostic tests do we do
contrast of CT- sees if pancrea has nercrosed. gold standard- diagnosing
endoscopic retograde- procedure where combine x ray w endoscopy- to see what pancreas looks like. can diagnose liver, galbaldder, and bile ducts.
What interventions do we do
Manage respiratory dysfunction- •High priority
Nutrition Support-
•NPO
•NGT placement
Replace fluids & electrolytes
•Maintain & replenish vascular volume and electrolyte balance
Comfort management
•Analgesics for pain control
•NGT
incident of hypocalcemia- rt high mortality in severe pancreatitis- prolonged QT interval, tetany, seizures, resp distress. replace Calcium.
Choveks sign- facial twitching when tapping cheek
Trousous- hand wrist contraction w bp cuff.
tx- seizure precautions, oral airway scution at bedside, monitor EKG, replace calcium, give IV opiods for comfort, NGT to suction if not being fed to decrease pancreatic stimulation, hypokaemia, hyperglycemia- give insulin, NPO most time, give PPN.
meds- abx to decrease infection/ necrosis-
What are systemic complications of acute pancreatitis
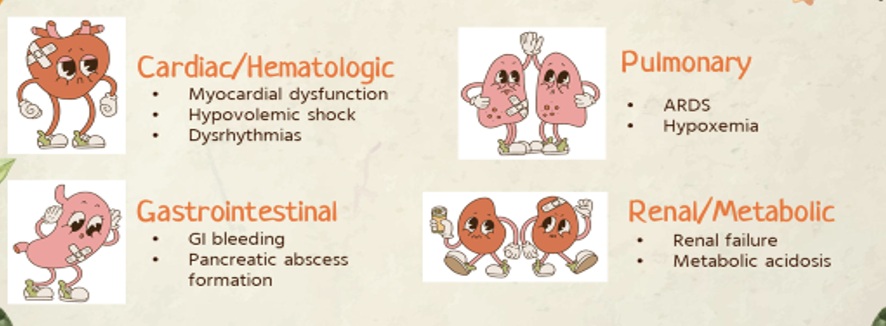
box 18.10
Case study
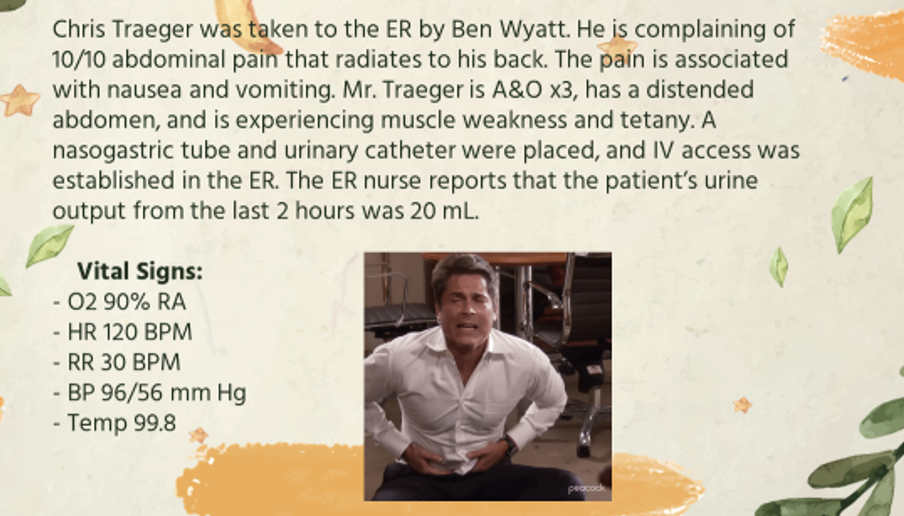
PQ
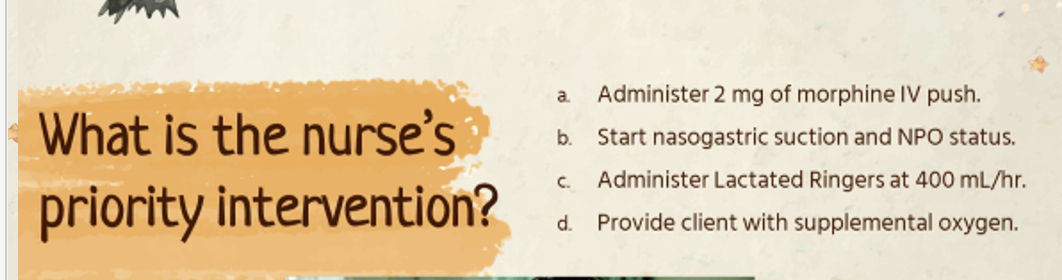
C , biggest problem pancreatitis- give LR . VS- signs hypovolemia.
A, B, C, D, F
A