Basic principles of immunity
1/26
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
INNATE IMMUNE SYSTEM
Foreign bodies such as bacteria, viruses, parasites, and fungi first encounter barriers of the innate immune system. These barriers include the skin; the physical and biochemical components in the nasopharynx, gut, lungs, and genitourinary tract; and the populations of commensal bacteria that compete with invading pathogens and the body's inflammatory response. Each of these is related to physiologic mechanisms taking place during the inflammatory process. Inflammation is a protective mechanism of the innate immune system, but it can overreact and actually cause tissue damage itself.
Monocytes
also follow neutrophils to inflammatory sites. Here, like neutrophils, they ingest and destroy inert particles, viruses, bacteria, and cellular debris by phagocytosis. In the blood, they are called monocytes, but when they migrate to various tissues and organs and interact with specific cytokines, become macrophages. Macrophages may also be derived from other tissues. They are located in the connective tissue, liver, brain, lung, spleen, bone marrow, and lymph nodes, and together they make up the mononuclear phagocytic system.

Natural Killer cells
not T or B lymphocytes, but rather, they are a small subset of lymphocytes found in the blood and the peripheral lymphoid organs. NK cells recognize and destroy host cells that are infected with microbes, such as viruses. They also activate phagocytes by releasing interferon-Y. Interferons are cytokines (soluble proseins secreted by cells to mediate immune responses) that elicit other cellular reactions, such as the prevention of viral replication, and they influence the actions of NK cells. They are also active in the adaptive immune response.
The complement system
consists of a group of proteins found in the blood. Collectively they are referred to as complement, and they are integral in both the innate and adaptive systems. When activated, a series of chemical reactions known as the complement cascade occurs. The system can be activated through one of three pathways, but the later steps are the same for all pathways. The components of the complement system are numbered C1 through C9, with some having several subunits designated by letters.
The classical pathway
which is a mechanism of the adaptive immune system, is activated when C1 is bound to an antigen-antibody complex. The other pathways of complement activation are part of the innate immune system, and they are triggered by microbial surfaces and plasma lectins that bind to microbes (Fig. 49.1). All three initial pathways catalyze a series of reactions of other complement molecules that have numerous physiologic effects. These include opsonization of the microbes to promote phagocytosis. Opsonization refers to the binding of complement to the antigen. Complement activation can also result in the stimulation of inflammation and cell lysis by the formation of a membrane attack complex on the surface of the antigen.
Adaptive Immune System
more sophisticated. The adaptive immune system is divided into two components: The humeral immune system and the cell-mediated immune system. The adaptive immune system has the ability to respond specifically to foreign substances. The substances called antigens may be bacterial, viral, parasitic or fungal or altered endogenesis cells of the host body. Their presence initiates humeral and cellular responses that neutralize, detoxify, and eliminate these foreign materials from the host.
Lymphocytes and their progeny
the cell types largely responsible for the adaptive immune system. However, this line of defense is not divorced from the innate immune system. Macrophages process antigens and present them to antigen committed lymphocytes. In other words, they act as antigen presenting cells.
Lymphoid stem cells
develop first in the yolk sac and then in the fetal liver. The bone marrow assumes this responsibility near parturition and serves as the source of these cells throughout postnatal life. The lymphoid stem cells are destined to further mature in one of two places: the bone marrow or the thymus. B lymphocytes mature in the bone marrow, whereas T lymphocytes mature in the thymus
Humoral Immune System
Lymphocytes that mature in the bone marrow (B cells) are concerned chiefly with the production and secretion of immunoglobulin (Ig) molecules, which are also known as antibodies. This is referred to as humoral immunity, because the antibodies are secreted into the body's fluids or "humors." Their maturation process consists of three stages: the lymphoblast, the prolymphocyte, and the mature lymphocyte. The mature cells leave the bone marrow to seed secondary lymphoid organs (chiefly the spleen and lymph nodes), where they encounter antigens. The humoral immune system can recognize billions of different antigens because, as B cells mature, each B cell develops a specific receptor molecule to a specific antigen
mature B cell
as they mature they develops a specific receptor molecule to a specific antigen. cell that is committed to that particular antigen will react with it. The stimulation of that B cell to produce antibodies is a complex process that requires the help of specialized T lymphocytes called helper T cells.

Helper T cells
(CD4+ cells) produce proteins called cytokines that activate the B cells. The antigen-stimulated B cell then quickly divides and differentiates, thereby producing a clone of identical B cells that all produce the same type of antigen-specific antibody. These antibody-secreting B cells are now called plasma cells, which are a type of effector cell. Helper T lymphocytes recognize antigen that has been phagocytized by an antigen-presenting cell (APC) such as a macrophage. The APC displays a portion of the antigen on its surface and presents it to the helper T lymphocyte. This stimulates the helper lymphocyte to release cytokines. These cytokines then, in turn, are the chemical signals that help the APC to further phagocytize the ingested microbe. Helper T cells, when stimulated, also release cytokines that help B cells differentiate into antibody-producing cells. Cytolytic T lymphocytes recognize antigen particles that are on the surface of infected body cells and that are able to lyse and kill the infected cells. Microbe-infected cells, tumor cells, and cells of foreign tissue graft all may be eliminated in this manner. Human immunodeficiency virus (HIV), which is the virus that causes the acquired immunodeficiency syndrome (AIDS), has a special affinity for the helper T lymphocytes
effector cell
a cell of the immune system that performs specific functions to destroy foreign antigens. Some of the antigen-stimulated B cells differentiate into memory B cells, which respond faster to a second exposure to that antigen
The inflammatory response
is a response to infection or tissue injury. Alerted by chemicals released from the infected site, blood vessels dilate and allow neutrophils to pass into tissue, where they phagocytize bacteria and kill the pathogens with chemicals stored in their cytoplasm. The classic signs of inflammation are pain, heat, redness, swelling, and loss of function.
Antibodies (immunoglobulins)
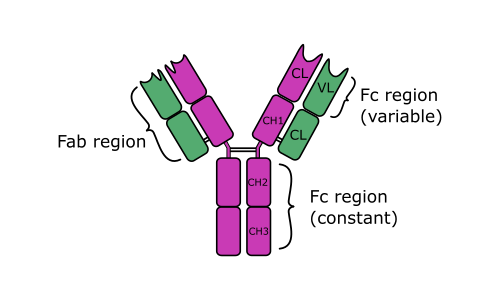
are protein molecules that consist of two pairs of polypeptide chains configured in a Y shape (Fig. 49.3). Each Ig molecule contains two variable regions and one constant region. The variable regions (Fab regions) bind to the antigen, and the constant region (Fc region) is responsible for the unique functions of the different antibody classes.
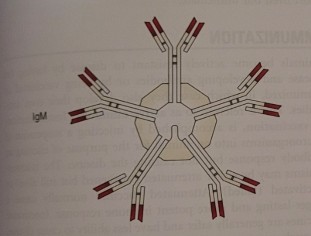
IgM
The first antibody type produced in response to an antigen. a pentameric molecule (i.e., it contains five monomers), and it comprises approximately 5% of circulating immunoglobulin. IgM is relatively large and therefore unable to enter tissue spaces. often described as a high-titer, low-avidity antibody. It is abundant in the early stages following exposure to an antigen and then in lower amounts in later stages. Avidity refers to the strength of the binding of antigen and antibody and is partly the result of the affinity of the IgM for the specific antigen
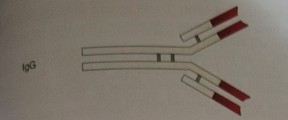
IgG
The most abundant circulating immunoglobulin. It comprises approximately 75% of circulating immunoglobulin, and it remains in the circulation for the longest time. IgG is a relatively small monomer that is capable of entering tissue spaces, and it is usually produced during a secondary immune response. IgG is a low-titer, high-avidity antibody. neutralization of microbes and toxins. opsonization of microbes for phagocytosis by macrophages and neutrophils. fetal and neonatal immunity by passive transfer across the placenta and in the colostrum
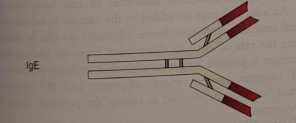
IgE
Immediate hypersensitivity reactions, such as allergy and anaphylactic shock. Coating of helminth parasites for destruction by eosinophils. is usually present in very small amounts, and it is similar in structure to IgG called a monomer
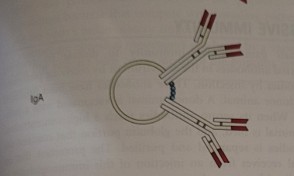
IgA
comprises approximately 20% of circulating antibody. mucosal immunity. protection of respiratory, intestinal and urogential tracts. there structure is called a dimer
IgD
a monomer that, when present, is in very low abundance. B lymphocyte surface antigen receptor in some species. especially important in defending your mouth, nose and respiratory tract. monomer
neutralization antibody reaction
occurs when antibody binds directly with the antigen. For example, if a foreign microbe or a microbial toxin is bound by antibody, it cannot infect or damage body cells. This essentially neutralizes the potential effect of the antigen. Sometimes antibodies coat microbes. The Fab region of the antibody attaches to receptors on the microbial surface. The Fc region of the antibody then binds to macrophages or neutrophils, and the microbe is phagocytized. Il the antigenic material is a helminth parasite, IgE antibodies opsonize the worms; however, instead of phagocytosis, which would be ineffectual against the large worms, eosinophils bind to and destroy the parasites. When complement is activated by some antibodies, the end result is antigenic cell lysis.
Precipitation reactions
occur when antigens bind with antibodies and form an insoluble complex. This precipitate forms on surfaces, and the precipitant itself may cause pathology. For example, the precipitation of bacterial fragments in the glomerular membrane can result in glomerular nephritis, which is described in Chapter 54 as a type III hypersensitivity reaction.
Cell-Mediated Immune System
Lymphoid stem cells that mature in the thymus develop into T-cell lymphocytes. Like B cells, their maturation process consists of three morphologically distinct stages: lymphoblast, prolymphocyte, and lymphocyte. As these cells mature, they also develop receptors to specific antigens and become immuno-competent or antigen-committed T lymphocytes. Some references refer to T and B cells at this stage as naive lymphocytes. Then, after contact with their specific antigens, these cells proliferate and differentiate into either clones of memory cells or clones of effector cells against those antigens. Memory cells recognize antigens to which they have previously been exposed. On a subsequent encounter, they elicit a more rapid immune response. Different types of T-effector cells exist, such as helper T cells (CD4+ cells) and cytolytic/cytotoxic T cells (CD8+ cells). The terms CD4+ and CD8+ refer to surface molecules or markers that are found on helper T and cytolytic T lymphocytes, respectively. Cytolytic T lymphocytes are also called cytotoxic T lymphocytes. Human immunodeficiency virus (HIV), which is the virus that causes the acquired immunodeficiency syndrome (AIDS), has a special affinity for the helper T lymphocytes. Helper T lymphocytes recognize antigen that has been phagocytized by an antigen-presenting cell (APC) such as a macrophage. The APC displays a portion of the antigen on its surface and presents it to the helper T lymphocyte. This stimulates the helper lymphocyte to release cytokines. These cytokines then, in turn, are the chemical signals that help the APC to further phagocytize the ingested microbe. Helper T cells, when stimulated, also release cytokines that help B cells differentiate into antibody-producing cells. Cytolytic T lymphocytes recognize antigen particles that are on the surface of infected body cells and that are able to lyse and kill the infected cells. Microbe-infected cells, tumor cells, and cells of foreign tissue graft all may be eliminated in this manner.
Immunologic Tolerance
One of the most important features of an animal's immune system is that it does not destroy its own cells. This may seem obvious, but it can actually happen. Maturing lymphocytes develop antigen receptors for foreign antigens but also for the animal's antigens on its own cells. Therefore, these self-reactive lymphocytes could attack the self-antigens. However, in a healthy animal, mechanisms normally are in place that prevent this self-destruction. The immune system can discriminate between self and non-self, which results in immunologic tolerance.
self antigens
Invading microbes are typically immunogenic; they will interact with their specific naive lymphocytes, which then proliferate and differentiate into effector cells that destroy the foreign microbes. However, to tolerate self-antigens, the animal relies on mechanisms such as antigenic tolerance and ignorance. Self-antigens are normally tolerogenic; the lymphocytes are either unable to respond when they encounter self-antigens (anergy), or they die when they encounter self-antigens (apoptosis). Self-antigens may also be ignored by naive lymphocytes, in which case the self-antigens are called nonimmunogenic. These mechanisms are elaborate. When naive lymphocytes are destroyed by apoptosis, the immune system is in effect selecting for the beneficial lymphocytes that have receptors for foreign antigens and eliminating the self-lymphocytes that would cause self-destruction. This is called negative selection, and it takes place in the bone marrow, thymus, and peripheral lymphoid tissues.

regulatory lymphocytes
mechanism of immunologic tolerance. some T lymphocytes, formerly called suppressor T cells, become regulatory lymphocytes. Regulatory T cells prevent self-reactive lymphocytes from differentiating into effector cells. They are unable to destroy self-antigens. This is an oversimplification of the intricacies involved in the maintenance of immunologic tolerance. When these mechanisms fail, autoimmune disease results, and the animal's immune system is directed against itself.
PASSIVE IMMUNITY
Animals gain passive immunity to disease by receiving maternal antibodies in the colostrum or by receiving preformed antibodies by injection. These antibodies have been produced in a donor animal. A donor animal is vaccinated with a pathogen. When its serum antibodies reach a high concentration, the animal is bled, and the globulin portion that contains the antibodies is separated and purified. The protection that an animal receives from an injection of this immunoglobulin is short lived but immediate.
active immunity
Immunization, or vaccination, is accomplished by injecting a suspension of microorganisms into an animal for the purpose of eliciting an antibody response but not causing the disease. The microorganisms may be either attenuated (weakened but still alive) or inactivated (killed). Attenuated vaccines normally cause a longer-lasting and more potent immune response. Inactivated vaccines are generally safer and have less ability to cause disease, although vaccine-associated sarcomas in cats have been an issue. An adjuvant may be added to the vaccine to enhance the normal immune response. Some adjuvants do this by simply slowing the rate of antigen elimination from the body so that the antigen is present longer to stimulate antibody production. Killed vaccines require more adjuvant, and the increased adjuvant has been implicated as one of the potential causes of the sarcomas.