Airflow and Gas Exchange
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
55 Terms
What is normal respiratory rate for domestic species?
- 20-30 brpm in most domestic species
- 10-12 brpm in horses
Define Eupnoea
normal breathing
Define Tachypnoea
increased rate of breathing
Define hyperpnoea
increased respiratory depth
Define Dysponea
Increased respiratory effort
Define apnoea
absence of breathing
What pressure changes cause inspiration, how is this achieved?
- pressure in the alveoli is less than atmospheric pressure
- active process, generated by expanding the thoracic cavity
What pressure changes cause exhilation, how is this achieved?
- pressure in the alveoli is greater than atmospheric pressure
- achieved by decreasing the size of the thoracic cavity, this is a passive process due to the elastic recoil of the lungs
What muscles are responsible for the expansion of the thoracic cavity during inspiration?
- Diaphragm contracts and flattens caudally
- External intercostal muscles contract- run caudo-ventrally so lift ribs out cranially
Under what circumstances might expiration become active?
- horses have active and passive phase to both inspiration and expiration
- in other species it may become active during exercise
What muscles are involved in active expiration and what is their action?
- abdominal muscles push abdominal contents cranially forcing the diaphragm to dome up into the thoracic cavity
- Internal intercostal muscles: run cranio-ventrally so contract to pull the ribs caudally and inwards
Define compliance in term of the lung
The degree to which a decrease in trans-pulmonary pressure (the difference between alveolar pressure and intra-pleural pressure) leads to an increase in volume of the lung
What does compliance depend on?
elasticity of lungs and surface tension of alveoli
What creates surface tension in the alveoli, and what effect does high surface tension have on compliance?
- Alveoli are lined with fluid to facilitate dissolution and diffusion of gasses
- hydrogen bonds in the water molecules create surface tension
- the surface tension reduces surface area and mean the alveoli resist expansion, therefore reducing compliance.
What substance acts to reduce surface tension of the alveoli and how does it do this?
Surfactant
- it is a mixture of phospholipids, protein and Ca2+, so have hydrophilic heads and and hydrophobic tails
- the heads dissolve in the liquid lining the alveoli and the tails remain on the inside of this liquid layer to prevent hydrogen bond formation
What does pressure inside the alveolus depend on?
radius and surface tension inside it
What would happen if a small alveolus communicated with a larger one?
There would be a higher pressure in the smaller one compared to the larger one, this would create a pressure gradient causing air to move into the larger alveolus and therefore the collapse of the smaller.
What adaptation are in place to prevent the collapse of smaller alveoli due?
The total amount of surfactant per alveoli is the same regardless of size, so the concentration of it is higher in smaller alveoli. This results in lower surfeit tension with reduces the pressure so it will equal the pressure in the larger ones.
What dos the resistance of the airway depend on?
Radius and length of the airway, and the viscosity (effectively equal to turbulence of the air)
What effect will increasing the length have on the resistance?
increase resistance
What effect will increasing the radius have on the resistance?
decrease resistance
What effect does decreasing the turbulence have on the resistance?
decrease resistance (due to friction of air molecules)
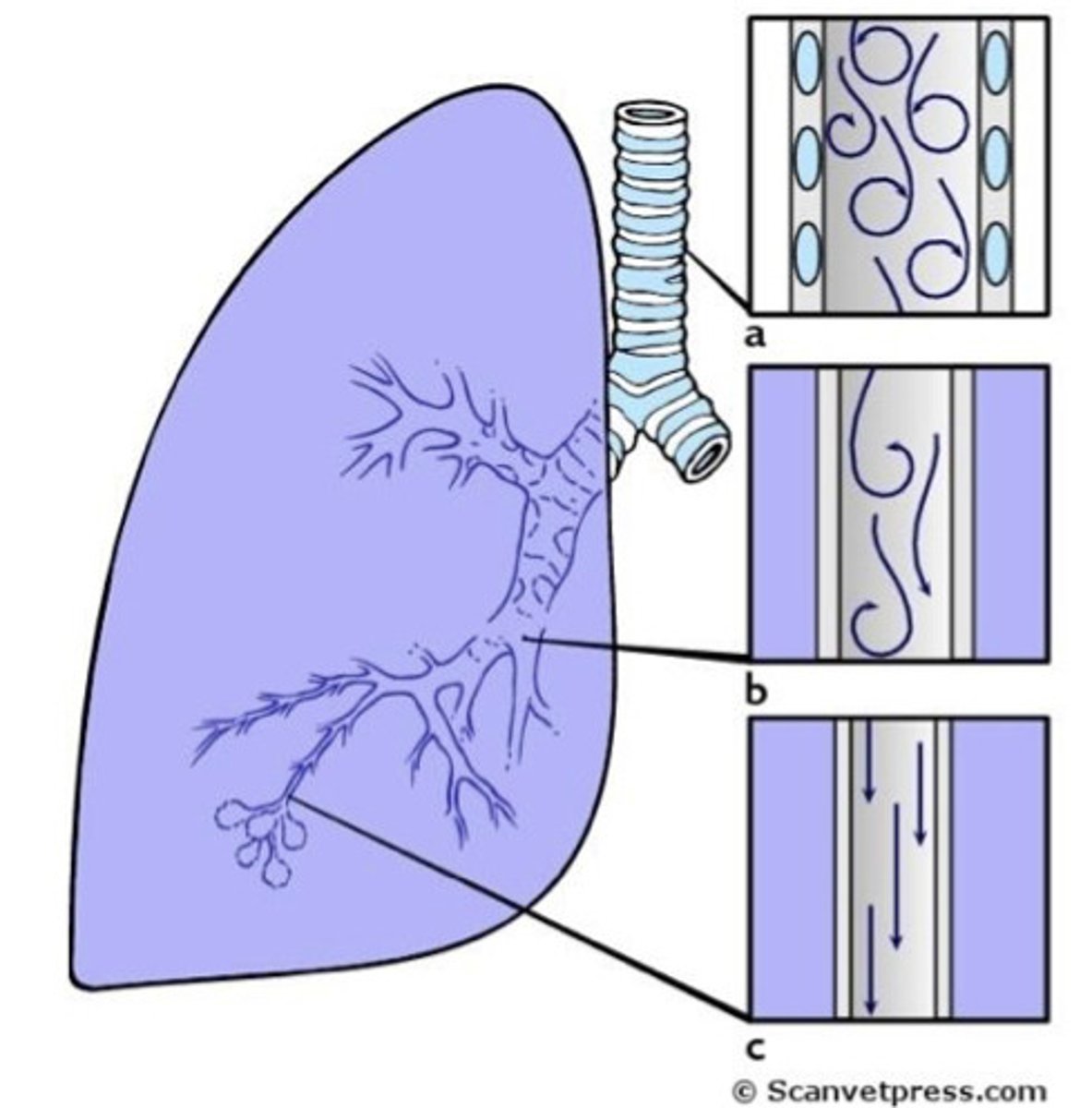
Will larger airways have higher or lower turbulence than smaller ones? Why?
higher as turbulence increases with speed of flow- which is greater in the larger airways.
Which of the factors effecting resistance to flow is easiest to change clinically?
Radius- there are drugs that can be given to increase this (e.g. inhalers)
Is the resistance lower during expiration or inspiration in the lower airways? why?
Lower airways are always distended during inspiration therefore there will be a lower resistance during inspiration
When is the resistance highest in the upper airways?
During inspiration, due to turbulence
How is the radius of the airways altered by the animal?
Smooth muscle in walls of the airways that are innervated by the ANS so can relax or contract to alter the radius
What effect does the sympathetic nervous system have on the airways?
Activation of the sympathetic system causes the smooth muscle to relax due to stimulation of β2-andrenoreceptors.
Increases radius, therefore decreases resistance. to allow for increased oxygen demand.
What effect does the parasympathetic nervous system have on the airways?
Contraction of smooth muscle, therefore constriction of airways
What disease states cause bronchoconstriction?
Asthma
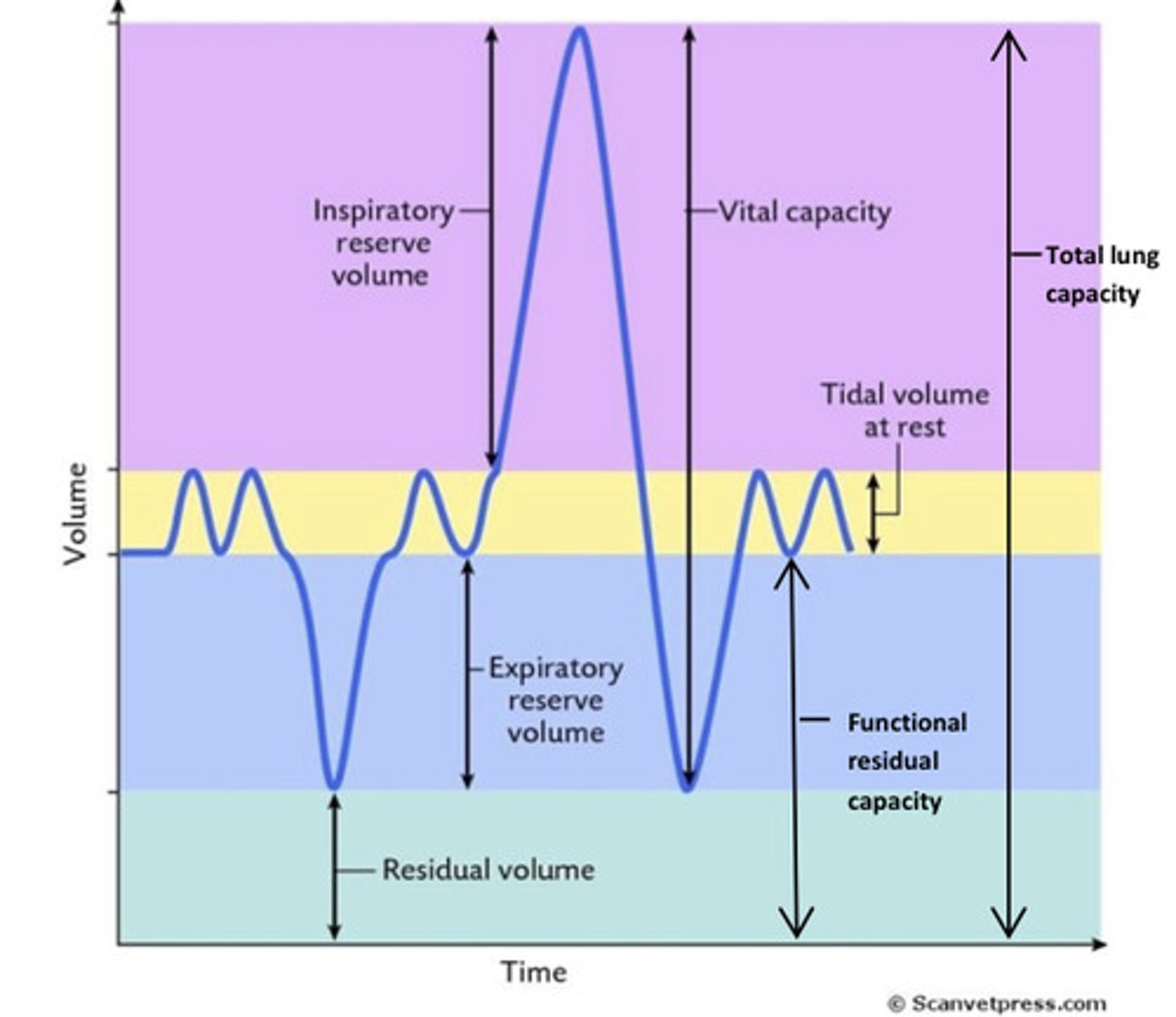
Define tidal volume
Volume of air moved in a respiratory cycle
10ml/kg in a normal dog
What is minute ventilation?
tidal volume x respiratory rate
When and how would minute volume be increased?
- During exercise when oxygen requirements increase
- achieved by increasing respiratory rate and/or tidal volume
What is vital capacity?
the greatest volume of air that can be expelled from the lungs after taking the deepest possible breath.
How is tidal volume maximised during peak exercise?
Additional muscles like neck and locomotion muscles can be engaged so the lungs can be further expanded to utilise inspiratory reserve volume. As well as abdominal and internal intercostal muscles
Why does the lung have a residual capacity of air?
a small amount of air remains after full expiration so the alveoli don't fully collapse causing the walls to stick together.
What is functional residual capacity?
expiratory reserve volume + residual volume
Define fraction of a gas (F)
- what proportion of a gas mixture is made up of the gas of interest
- e.g. FO2 in normal room air = 21% = 0.21
Define partial pressure of a gas (P)
- pressure exerted by an individual gas within a gas mixture
- calculated by fraction of gas x the pressure of the 'container' it's in
- e.g. PO2 in normal room air = FO2 x atmospheric pressure = 0.21 x 760 = ~160mmHg
How does a gas exert pressure?
collisions of the gas particles with surfaces
What causes movement of a gas?
Gas particles will move down their pressure gradients- other gas molecules in the gas mixture are irrelevant to that gradient.
Which is more soluble CO2 or O2?
CO2
What increases solubility of gas molecules?
increases partial pressure
What is dynamic equilibrium?
When the number of molecules of gas entering and leaving a solution during given unit of time are equal
Air that is inhaled is humidified in the airways before entering the lung, how does this effect the partial pressure of O2?
- It makes the PO2 proportionally less, but does not effect the total pressure exerted by the gas mixture.
- In order to calculate PO2 in the airways, PH2O needs to be subtracted from atmospheric pressure.
How does the partial pressure of O2 and CO2 differ in the alveoli compared to in the airways?
PAO2 will always be lower than PO2 in the airways
PACO2 will always be higher than PCO2 in the airways
What is gas exchange dependent on?
The Ventilation:Perfusion ratio
What does a low Va:Q ratio mean in the alveoli?
alveoli would be relatively overperfused and underventilated
What does a high Va:Q ratio mean in the alveoli?
alveoli would be relatively underperfused and overventillated
What would cause a change in systemic arterial gas tension?
only occur if a significant proportion of alveoli have abnormal Va:Q ratios.
What are the effects of abnormal ventilation?
- Hyperventilation causes excess loss in CO2, leading to a drop in PaCO2 = hypocapnia
- Hypoventilation causes drop in PAO2 and increased PACO2, leading to reduced PaO2 and PaCO2 (hypoxia and hypercapnia)
(risk during general anaesthesia)
What is 'dead space' in the respiratory system?
regions of the circulatory system that are ventilated but do not participate in gas exchange
Which structures are anatomical dead space and which are funtional dead space?
- conducting passageways of the respiratory tract are anatomical dead space
- alveoli that are ventilated but not perfused are functional dead space
What occurs when a dog is panting? (relating to dead space air)
- during inspiration alveoli are first filled by air from the dead space, which is higher in CO2 and lower in O2 than normal air as it is partially made up of exhaled air.
- if a dog is breathing shallowly a lower volume of air is inspired to displace the dad space gas- can lead to an insufficient amount of oxygen being taken into the blood stream, so respiration will not be as efficient
How does the ventilation equipment used during general anaesthesia alter dead space?
it can increase the amount of dead space