ANES 660 exam 1
0.0(0)
Card Sorting
1/129
There's no tags or description
Looks like no tags are added yet.
Last updated 3:20 AM on 6/7/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
1
New cards
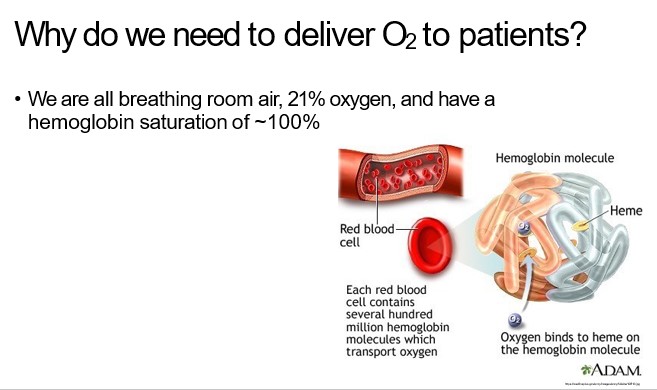
how much oxygen is in the air
21% oxygen
2
New cards
what is our hemoglobin saturation
\~100%
3
New cards
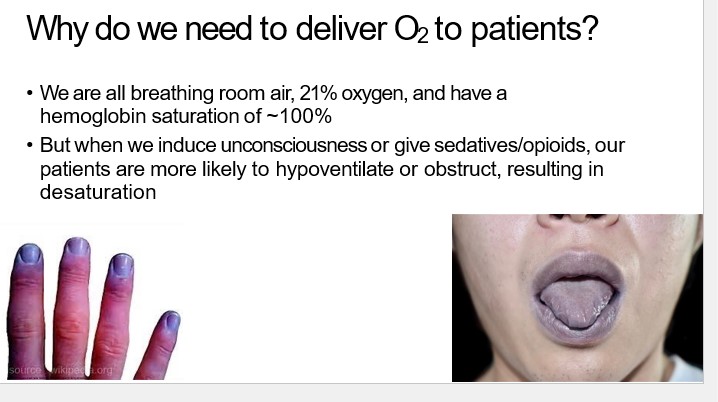
what happens when we induce unconsciousness or give sedatives/opioids
our patients are more likely to hypoventilate or obstruct, resulting in desaturation
4
New cards
what happens when we provide supplemental oxygen
•we can achieve an FiO2 >21%, and decrease the risk of desaturation
5
New cards
what is FiO2
fraction of inspired oxygen; 0.21 or 21% @ room air, up to 100% if all the “air” breathed by pt is pure oxygen \[no nitrogen or nitrous oxide\])
6
New cards
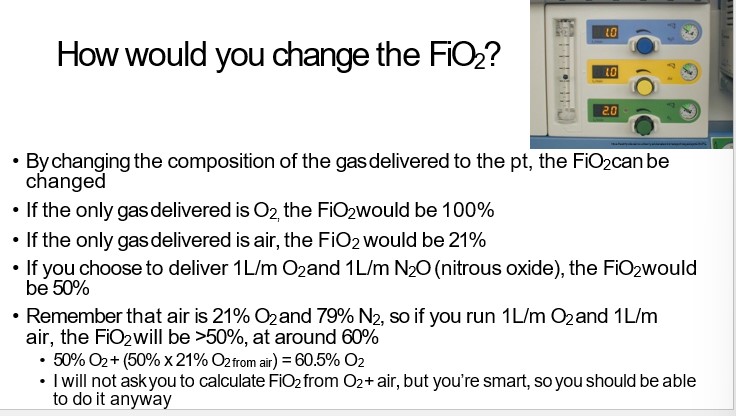
I’m giving you 50% oxygen and 50% nitrous oxide. What’s your FiO2?
To calculate the FiO2, we need to convert the percentages into decimal values and sum the fractions of oxygen. The percentage of oxygen is divided by 100 to convert it to a decimal value:
Oxygen fraction = 50% / 100 = 0.5
Since the nitrous oxide is not contributing to the FiO2 (it does not contain oxygen), we can ignore it for this calculation.
Therefore, the FiO2 in a gas mixture of 50% oxygen and 50% nitrous oxide would be 0.5 or 50%.
7
New cards
what are the two main ways we deliver oxygen in the OR
•Invasively and non-invasively
8
New cards
what devices would you use to deliver oxygen invasively
•Invasively, via an endotracheal tube or an LMA
9
New cards
when would we use an endotracheal tube or an LMA
We use these devices when a patient is under general anesthesia
10
New cards
what is general anesthesia
•**General anesthesia** is when a patient is unconscious, has a loss of protective reflexes including the ability to maintain their airway and respond purposefully to noxious stimuli or verbal commands
11
New cards
If I push 2mg/kg propofol. You have a 70kg patient. How many milligrams is that for 2 mg/kg?
140mg
To calculate the dosage of propofol for a 70kg patient at a rate of 2mg/kg, you would multiply the patient's weight by the dosage rate:
2 mg/kg \* 70 kg = 140 mg
To calculate the dosage of propofol for a 70kg patient at a rate of 2mg/kg, you would multiply the patient's weight by the dosage rate:
2 mg/kg \* 70 kg = 140 mg
12
New cards
how many CCs is that for propofol?
14cc
For a 10 mg/ml concentration: Volume (in cc) = Dosage (in mg) / Concentration (in mg/ml) = 140 mg / 10 mg/ml = 14 cc
For a 10 mg/ml concentration: Volume (in cc) = Dosage (in mg) / Concentration (in mg/ml) = 140 mg / 10 mg/ml = 14 cc
13
New cards
how do we deliver O2 to patients non-invasively
•Non-invasively - via a nasal cannula, simple face mask, or non- rebreathing facemask
14
New cards
when are non-invasive devices used
•**These devices are used when a patient is able to maintain their airway**
•Usually utilized during **MAC procedures**, after extubation of advanced (invasive) airways, or by patients with pulmonary diseases (e.g. COPD) who need higher FiO2 @ baseline
15
New cards
what is MAC
•MAC = monitored anesthesia care; colloquially known as “twilight” anesthesia; lighter sedation \*without\* complete loss of consciousness and airway
16
New cards
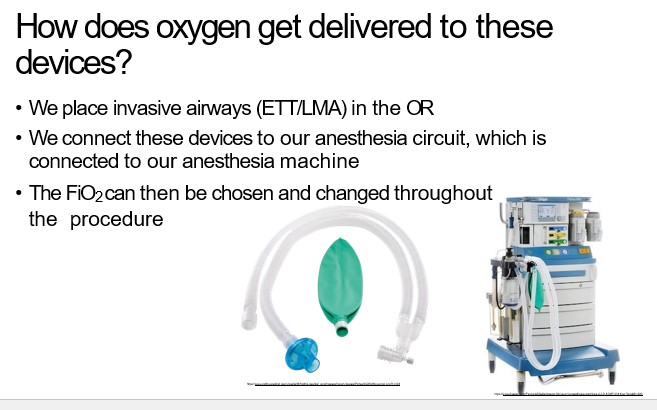
How does oxygen get delivered to these devices?
•We place invasive airways (ETT/LMA) in the OR
•We connect these devices to our anesthesia circuit, which is connected to our anesthesia machine
•The FiO2 can then be chosen and changed throughout the procedure
17
New cards
How would you change the FiO2?
18
New cards
why are we able to choose the FiO2 with LMAs and ETTs
the gas is delivered in a “closed” system
19
New cards
for non-invasive airway, is the system open or closed?
•With non-invasive airway, the system is “open” to atmosphere to varying degrees, meaning the FiO2 is more variable, depending on the device and the ”flows”
20
New cards
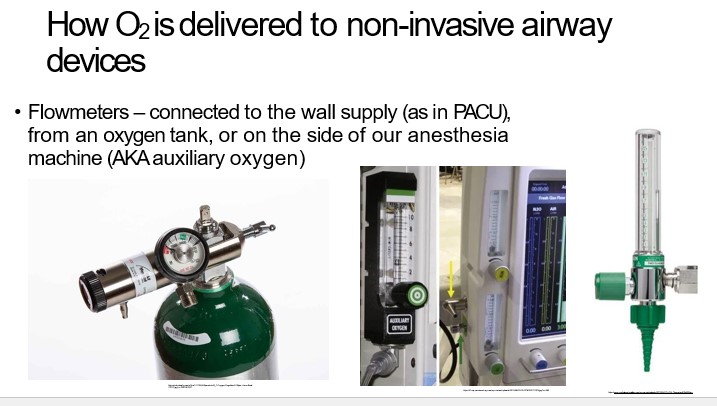
what are flowmeters
connected to the wall supply (as in PACU), from an oxygen tank, or on the side of our anesthesia machine (AKA auxiliary oxygen)
21
New cards
what is Spontaneous
•patient is breathing on their own; negative pressure ventilation
22
New cards
what is Airway obstruction
•the patient’s upper airway “collapsed” or obstructed resulting in decreased or absent ventilation, despite patient trying to breathe spontaneously
•Think snoring
23
New cards
what is Positive pressure ventilation
•breathing provided by generating positive pressure to expand the lungs
•This is how the ventilator on our anesthesia machine works
24
New cards
what is apneic
not breathing
25
New cards
what is one way to fix a patient who has gone apneic
Bag-mask-ventilation (BMV)
26
New cards
what is Bag-mask-ventilation (BMV)
•A way to provide non-invasive positive pressure ventilation
27
New cards
when do you use Bag-mask-ventilation (BMV)
When to use it?
•It’s most commonly used between induction and intubation
•But it can also be used if a patient is obstructing with a non-invasive airway device (e.g. during a MAC procedure)
•Also during CPRwithout a “secured airway”
•It’s most commonly used between induction and intubation
•But it can also be used if a patient is obstructing with a non-invasive airway device (e.g. during a MAC procedure)
•Also during CPRwithout a “secured airway”

28
New cards
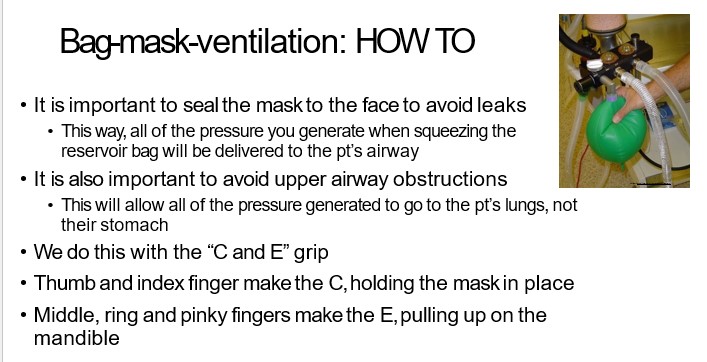
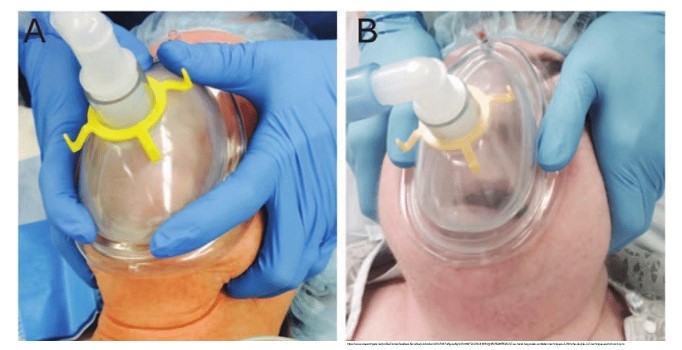
how do you do a Bag-mask-ventilation
•It is important to seal the mask to the face to avoid leaks
•This way, all of the pressure you generate when squeezing the reservoir bag will be delivered to the pt’s airway
•It is also important to avoid upper airway obstructions
•This will allow all of the pressure generated to go to the pt’s lungs, not their stomach
•We do this with the “C and E” grip
•Thumb and index finger make the C, holding the mask in place
•Middle, ring and pinky fingers make the E, pulling up on the mandible
29
New cards
Bag-masking technique
•Rest the top of the mask over the bridge of the nose
•The bottom of the mask should sit below the lower lip but above the chin – if not, you may need a different sized mask
•Especially important in peds

30
New cards
proper finger placement during BVM ventilation
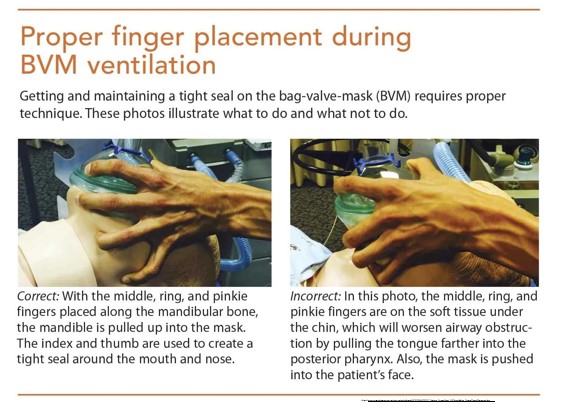
31
New cards

is this the proper technique?
This is incorrect. The 3 fingers are on the soft tissue
32
New cards
true or false
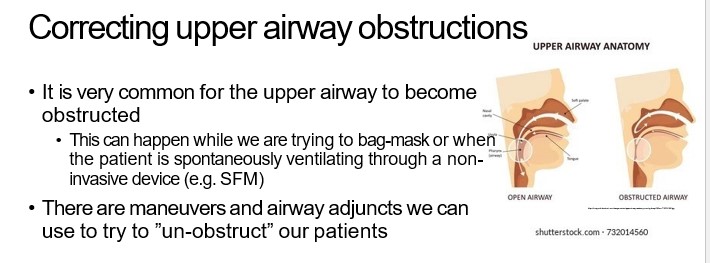
it is uncommon for the upper airway to become obstructed
it is uncommon for the upper airway to become obstructed
false.
•It is very common for the upper airway to become obstructed
•It is very common for the upper airway to become obstructed
33
New cards
when can the upper airway become obstructed
•This can happen while we are trying to bag-mask or when the patient is spontaneously ventilating through a non- invasive device (e.g. SFM)
34
New cards
true or false
•There are maneuvers and airway adjuncts we can use to try to ”un-obstruct” our patients
•There are maneuvers and airway adjuncts we can use to try to ”un-obstruct” our patients
true
35
New cards
what are some ways to correct upper airway obstructions
Chin-lift / Head-tilt
Jaw Thrust
Two-hand bag-mask technique
Sit the patient up
Sniffing position
Jaw Thrust
Two-hand bag-mask technique
Sit the patient up
Sniffing position
36
New cards
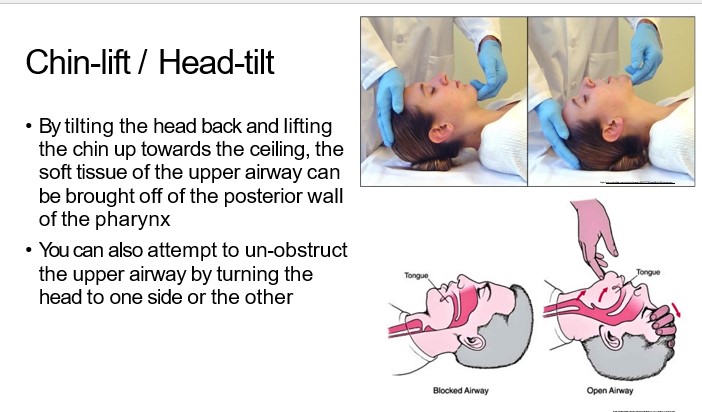
describe Chin-lift /Head-tilt
•By tilting the head back and lifting the chin up towards the ceiling, the soft tissue of the upper airway can be brought off of the posterior wall of the pharynx
•You can also attempt to un-obstruct the upper airway by turning the head to one side or the other
37
New cards
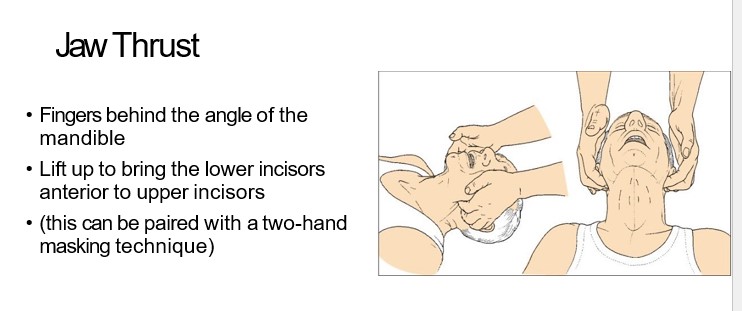
describe jaw thrust
•Fingers behind the angle of the mandible
•Lift up to bring the lower incisors anterior to upper incisors
•(this can be paired with a two-hand masking technique)
38
New cards
describe Two-hand bag-mask technique
•One practitioner holds the mask/face with both hands while a second provider squeezes the bag
•Two techniques for holding the mask:
•Double C/E hold
Thumbs/heels of hand on mask, 4 fingers pulling up on the mandible
39
New cards
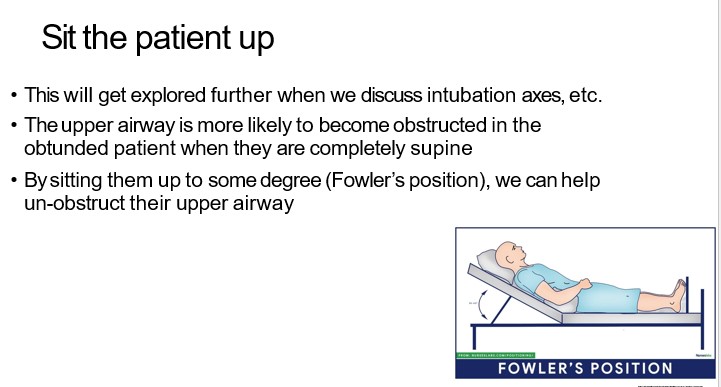
describe sit the patient up
•This will get explored further when we discuss intubation axes, etc.
•The upper airway is more likely to become obstructed in the obtunded patient when they are completely supine
•By sitting them up to some degree (Fowler’s position), we can help un-obstruct their upper airway
40
New cards
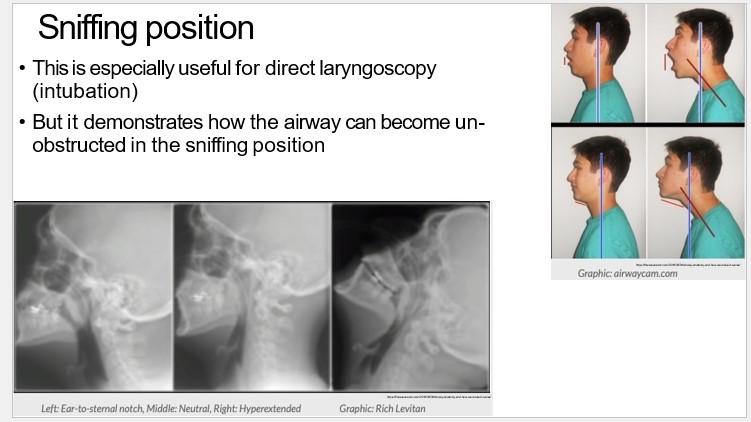
describe the sniffing position
•This is especially useful for direct laryngoscopy (intubation)
•But it demonstrates how the airway can become un- obstructed in the sniffing position
41
New cards
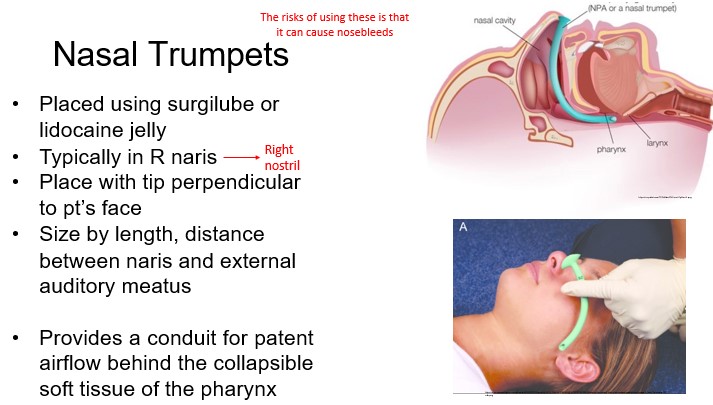
how are nasal trumpets placed
•Placed using surgilube or lidocaine jelly
42
New cards
which nostril are nasal trumpets places
•Typically in R naris
43
New cards
how would you put in a nasal trumpet
•Place with tip perpendicular to pt’s face
44
New cards
how would you determine the right size of a nasal trumpet
•Size by length, distance between naris and external auditory meatus
45
New cards
what is the function of a nasal trumpet
•Provides a conduit for patent airflow behind the collapsible soft tissue of the pharynx
46
New cards
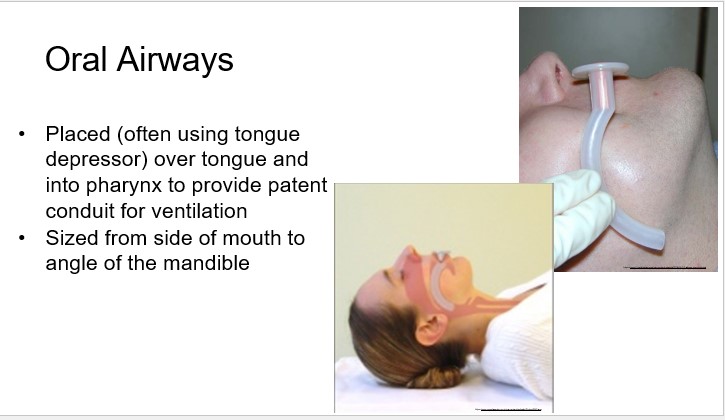
what is the function of oral airways
•Placed (often using tongue depressor) over tongue and into pharynx to provide patent conduit for ventilation
47
New cards
how would you determine the right size of an oral airway
•Sized from side of mouth to angle of the mandible
48
New cards
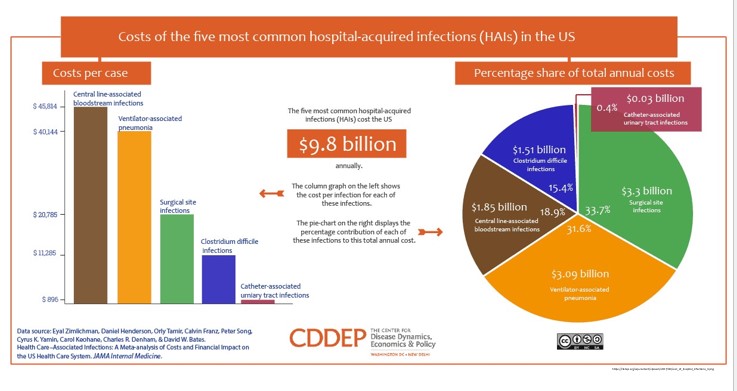
how much does the five most common hospital-acquired infections (HAIs) cost the US
$9.8 billion annually
49
New cards
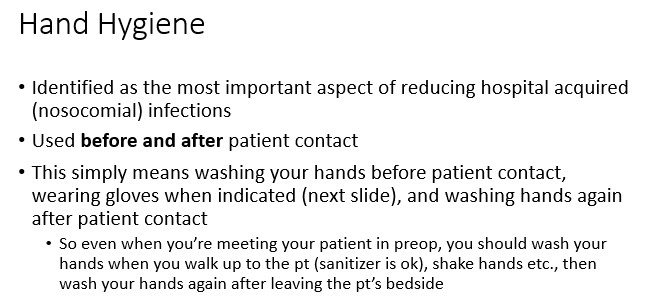
what is the most important aspect of reducing hospital acquired (nosocomial) infections
hand hygiene
50
New cards
when should you practice hand hygiene
**before and after** patient contact
51
New cards
elaborate on the last slide
•This simply means washing your hands before patient contact, wearing gloves when indicated (next slide), and washing hands again after patient contact
•So even when you’re meeting your patient in preop, you should wash your hands when you walk up to the pt (sanitizer is ok), shake hands etc., then wash your hands again after leaving the pt’s bedside
52
New cards
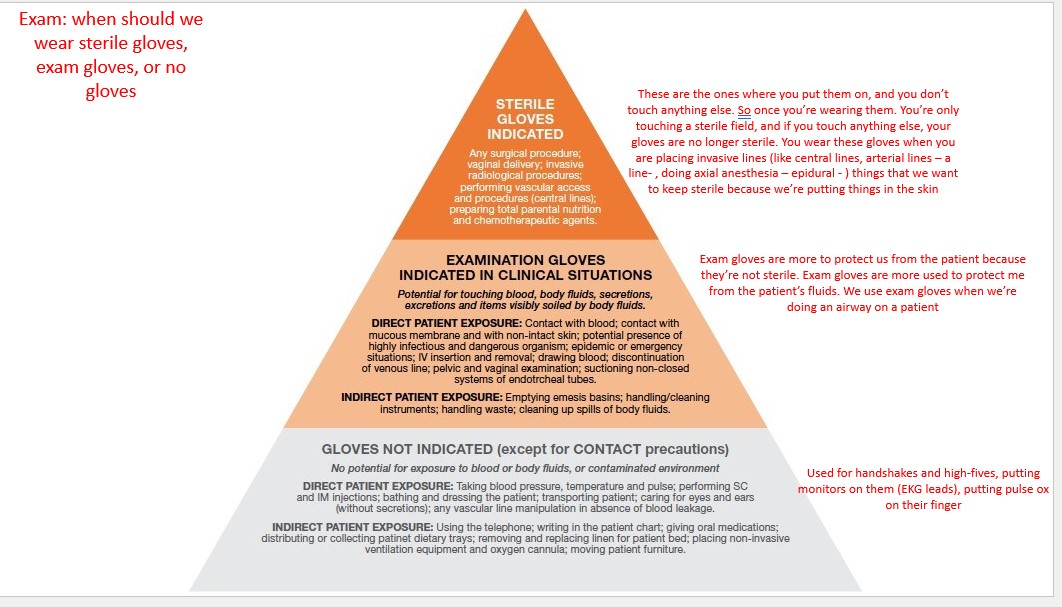
when should we wear sterile gloves
any surgical procedure; vaginal delivery; invasive radiological procedures; performing vascular access and procedures (central lines); preparing total parental nutrition and chemotherapeutic agent
53
New cards
when should we wear examination gloves
potential for touching blood, body fluids, secretions, excretions and items visibly soilded by body fluids
DIRECT PATIENT EXPOSURE: contact with blood; contact with mucous membrane and with non-intact skin; potential presence of highly infectious and dangerous organism; epidemic or emergency situations; IV insertion and removal; drawing blood; discontinuation of venous line; pelvic and vaginal examination; suctioning non-closed sysrems of endotrcheal tubes
INDIRECT PATIENT EXPOSURE: emptying emesis basins; handling/cleaning instruments; handling waste; cleaning up spills of body fluids
DIRECT PATIENT EXPOSURE: contact with blood; contact with mucous membrane and with non-intact skin; potential presence of highly infectious and dangerous organism; epidemic or emergency situations; IV insertion and removal; drawing blood; discontinuation of venous line; pelvic and vaginal examination; suctioning non-closed sysrems of endotrcheal tubes
INDIRECT PATIENT EXPOSURE: emptying emesis basins; handling/cleaning instruments; handling waste; cleaning up spills of body fluids
54
New cards
when do you not have to wear gloves
no potential for exposure to blood or body fluid, or contaminated environment
DIRECT PATIENT EXPOSURE: taking blood pressure, temperature and pulse; performing SC and IM injections; bathing and dressing the patient; transporting patient; caring for eyes and ears (without secretions); any vascular line manipulation in absence of blood leakage
INDIRECT PATIENT EXPOSURE: using the telephone; writing in the patient chart; giving oral medications; distributing or collecting patient dietary trays; removing and replacing linen for patient bed; placing non-invasive ventilation equipment and oxygen cannula; moving patient furniture
DIRECT PATIENT EXPOSURE: taking blood pressure, temperature and pulse; performing SC and IM injections; bathing and dressing the patient; transporting patient; caring for eyes and ears (without secretions); any vascular line manipulation in absence of blood leakage
INDIRECT PATIENT EXPOSURE: using the telephone; writing in the patient chart; giving oral medications; distributing or collecting patient dietary trays; removing and replacing linen for patient bed; placing non-invasive ventilation equipment and oxygen cannula; moving patient furniture
55
New cards
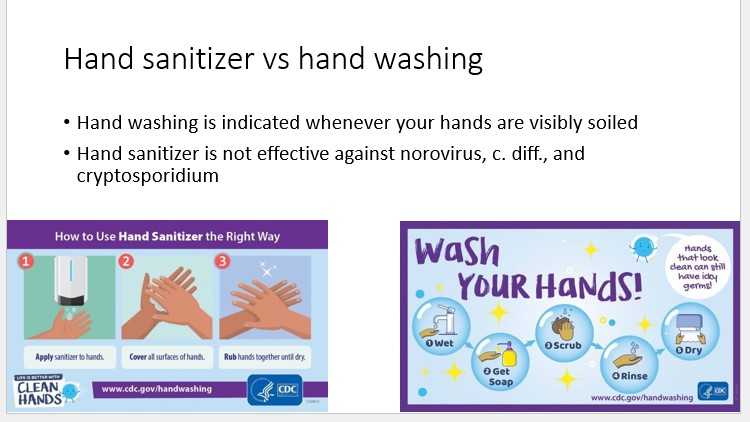
what the difference between Hand sanitizer and hand washing
•Hand washing is indicated whenever your hands are visibly soiled
•Hand sanitizer is not effective against norovirus, c. diff., and cryptosporidium
56
New cards
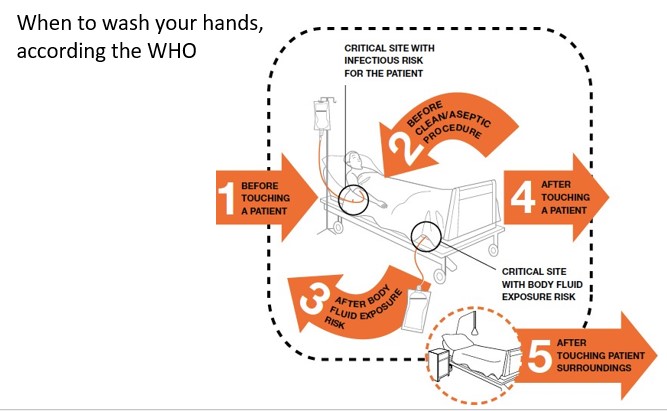
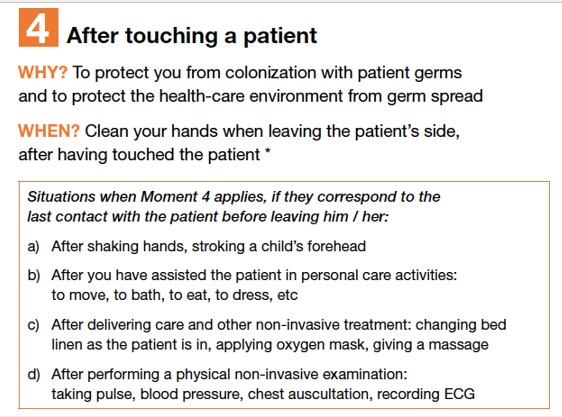
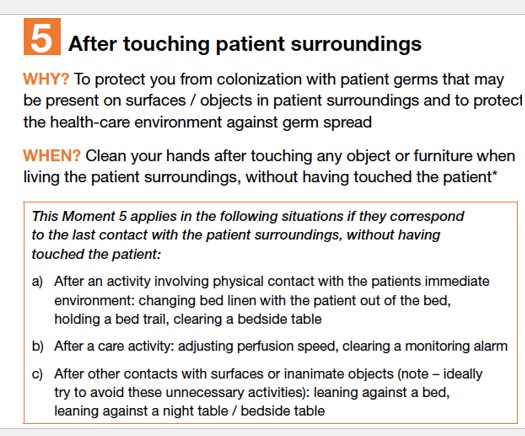
according to the WHO, when should you wash your hands
1. before touching a patient
2. before clean/aseptic procedure
3. aftern body fluid exposure risk
4. after touching a patient
5. after touching patient surroundings
57
New cards
why should you wash your hands before touching a patient
to protect the patient against colonization and, in some cases against exogenous infection, by harmful germs carried on your hands

58
New cards
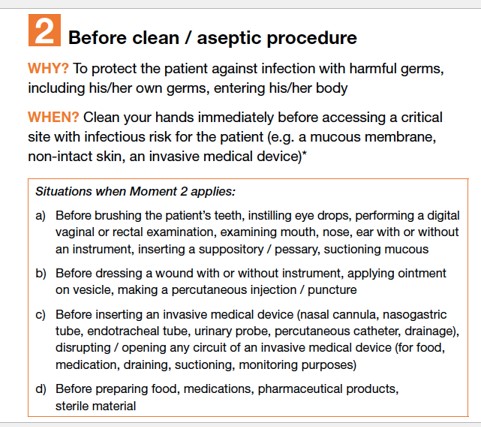
why should you wash your hands before a clean/aseptic procedure
to protect the patient against infection with harmful germs, including his/her own germs entering his/her body
59
New cards
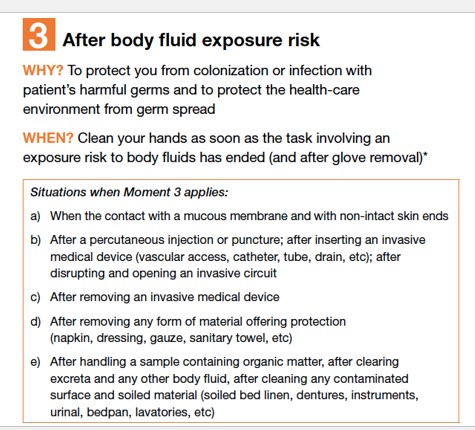
why should you wash your hands after body fluid exposure risk
to protect you from colonizationg or infection with patient’s harmful germs and to protect the health-care environment from germ spread
60
New cards
why should wash your hands after touching a patient
to protect you from colonization or infection with patient’s harmful germs and to protect the health-care environment from germ spread
61
New cards
why should you wash your hands after touching patient surroundings
to protect you from colonization with patient germs that may be present on surfaces/objects in patient surroundings and to protect the health-care environment against germ spread
62
New cards
what are standard precautions
•constitutes the primary strategy for the prevention of healthcare-associated transmission of infectious agents among patients and healthcare personnel
63
New cards
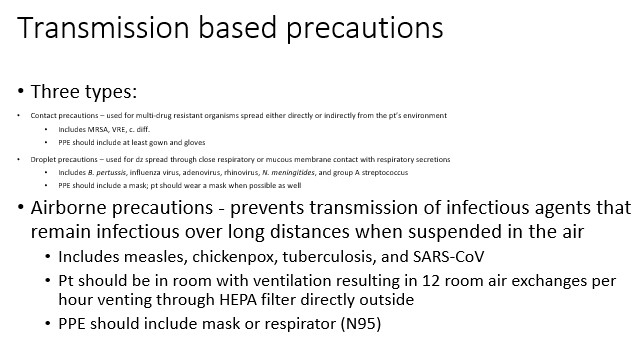
what are Transmission based precautions
used when a patient is infected with an epidemiologically significant microorganism or an uncontained and transmittable infection
64
New cards
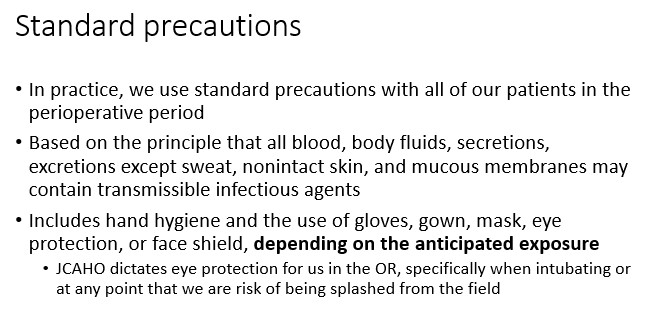
when do we use standard precautions
•In practice, we use standard precautions with all of our patients in the perioperative period
65
New cards
what contains transmissible infectious agents
•all blood, body fluids, secretions, excretions except sweat, nonintact skin, and mucous membranes may contain transmissible infectious agents
66
New cards
due to standard precautions, what should you wear
•Includes hand hygiene and the use of gloves, gown, mask, eye protection, or face shield, **depending on the anticipated exposure**
67
New cards
according to JCAHO, when should you wear eye protection
•JCAHO dictates eye protection for us in the OR, specifically when intubating or at any point that we are risk of being splashed from the field
68
New cards
what are the 3 types of transmission based precautions
contact precautions
droplet precautions
airborne precautions
droplet precautions
airborne precautions
69
New cards
what are contact precautions used for
used for multi-drug resistant organisms spread either directly or indirectly from the pt’s environment
70
New cards
what kinds of virsuses do contact precautions include
•Includes MRSA, VRE, c. diff.
71
New cards
what kind of PPE should we wear under contact precautions
•PPE should include at least gown and gloves
72
New cards
what are droplet precautions used for
used for dz spread through close respiratory or mucous membrane contact with respiratory secretions
73
New cards
what kinds of virsuses do droplet precautions include
Includes *B. pertussis*, influenza virus, adenovirus, rhinovirus, *N. meningitides*, and group A streptococcus
74
New cards
what kind of PPE should you wear under droplet precautions
•PPE should include a mask; pt should wear a mask when possible as well
75
New cards
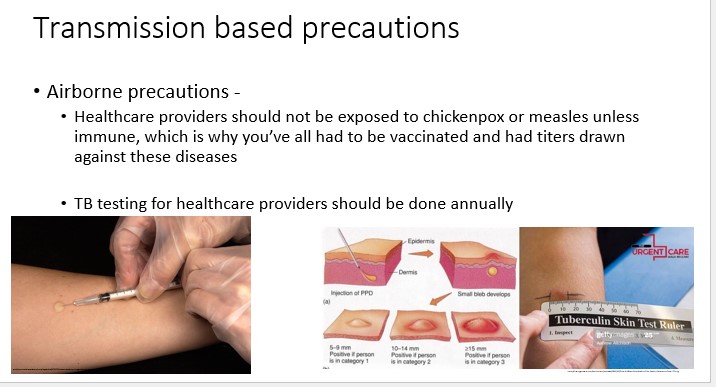
what do airborne precautions prevent
•prevents transmission of infectious agents that remain infectious over long distances when suspended in the air
76
New cards
what kinds of virsuses do airborne precautions include
•Includes measles, chickenpox, tuberculosis, and SARS-CoV
77
New cards
if a patient is under airborne precautions, what kind of environment should they be in
•Pt should be in room with ventilation resulting in 12 room air exchanges per hour venting through HEPA filter directly outside
78
New cards
what kind of PPE should you wear under airborne precautions
•PPE should include mask or respirator (N95)
79
New cards
when should healthcare provided get TB testing
annually
80
New cards
review: when should you use sterile gloves
•Arterial line placement, central line placement, neuraxial (spinal/epidural placement), floating PACs, accessing medports
81
New cards
when should you wear exam gloves
•Everything else
•Placing IVs, manipulating the airway, any contact w/ blood, mucus membranes, etc.
•I wear gloves almost any time I have any physical contact with patients
82
New cards
when should you wear no gloves
•Handshakes and high fives

83
New cards
what kind of containers do we use in the OR
•**Purple bin**
•**Red sharps bin**
•**Rx Destroyer**
•**Trash**
* red bio-hazard bag
84
New cards
what should you put in the red bio-hazard bag
you put things that are really bloody or soaked in urine/feces in the red bio-hazard bag
85
New cards
what do we put in purple-top bins
non-regulated waste ***ONLY***
86
New cards
where are purple-top bins located
•These bins are located on anesthesia carts or trollies for vials & containers that are **full, partially full, or contain residual non-hazardous drugs/waste.**
87
New cards
what are some examples of Non Hazardous Drugs/Waste
•Local Anesthetics
•Non-controlled Drugs/Medications (Things like atropine or metoprolol)

88
New cards
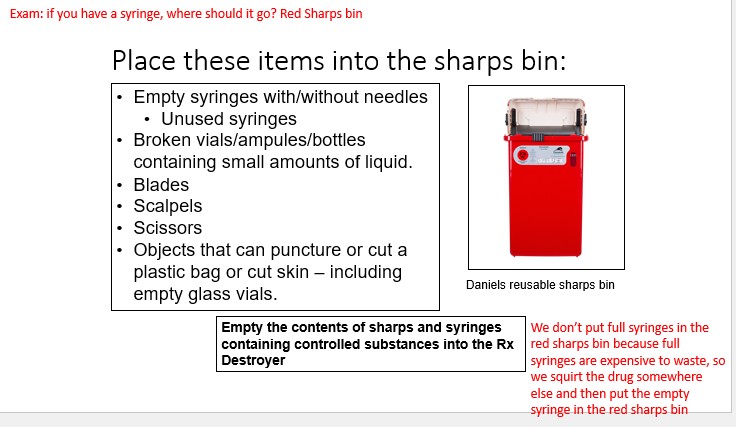
what kinds of things should you put in the sharps bin
•Empty syringes with/without needles
•Unused syringes
•Broken vials/ampules/bottles containing small amounts of liquid.
•Blades
•Scalpels
•Scissors
•Objects that can puncture or cut a plastic bag or cut skin – including empty glass vials.
89
New cards
true or false
you can put full syringes into the sharps bin
you can put full syringes into the sharps bin
false.
We don’t put full syringes in the red sharps bin because full syringes are expensive to waste, so we squirt the drug somewhere else and then put the empty syringe in the red sharps bin
**Empty the contents of sharps and syringes containing controlled substances into the Rx Destroyer**
We don’t put full syringes in the red sharps bin because full syringes are expensive to waste, so we squirt the drug somewhere else and then put the empty syringe in the red sharps bin
**Empty the contents of sharps and syringes containing controlled substances into the Rx Destroyer**
90
New cards
what should you put in the Rx destroyer
•Disposal of controlled substances
•Disposal of drugs that are at risk for diversion
•Pills, tablets, injections, solutions, patches, creams, lozenges
91
New cards
what are some examples of controlled substances
Fentanyl, propofol, morphine, ketamine
92
New cards
what should NOT go in the Rx destroyer
__**Do not**__ **put syringes, vials, packaging, or solids in these containers.**
93
New cards
where should you put empty IV bogs and tubing
These items can be defaced of patient information and disposed of in the normal trash!
__DO NOT__ place empty IV bags and tubing into the purple top or sharps bins.
94
New cards
what can go in the trash
•Empty pharmaceutical IV bags & tubing (defaced PHI).
•PPE (gloves, gowns & masks) used to administer non-hazardous pharmaceuticals.
•Disposable items that are not grossly contaminated with blood:
•Flecked, spotted, or smeared with blood
•Non broken glass bottles
95
New cards
what should you put int the blus soiled linen bags
•Throw all linen from the OR into these bags
•If it is completely saturated with blood, throw away into the red biohazard bag
96
New cards
true or false
you can eat in patient contact areas
you can eat in patient contact areas
false
•No eating or drinking in these areas
•For your own protection against contamination
•To prevent spills attracting pests
97
New cards
true or false
to cap a needle stick, you should use both hands
to cap a needle stick, you should use both hands
false. Do not use both hands to cap a needle
98
New cards
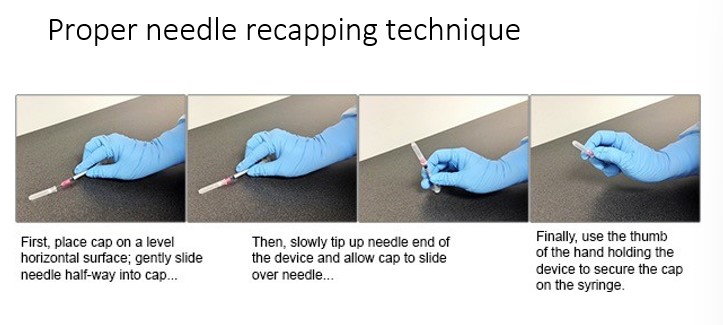
what is the proper needle recapping technique
99
New cards
what is the seroconversion rate for Hep C
\~0.5-1.8%
100
New cards
what is the seroconversion rate for Hep B if non-immunized
\~30%