Human Reproduction - ALL
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
SRY Gene - What is it’s significance
human sex is determined by the presence/absence of the SRY gene found on the Y- chromosome
if the SRY gene is present, primordial germ cells (PGC’S) migrate to the medullary region of urogenital region and become spermatogonia
in the SRY gene is absent, PGC’s migrate to the cortical region of the urogenital region and become oogonia
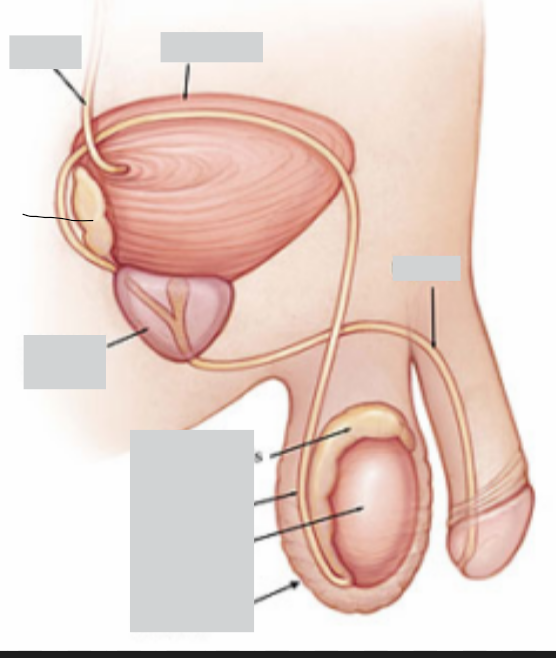
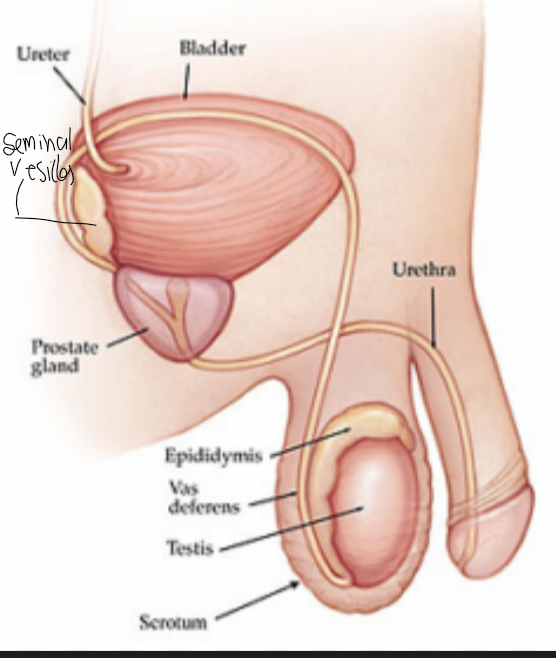
Male Primary and Secondary Sexual Organs
Primary Sexual Organs - testes (produce gamete)
Secondary Sexual Organs - penis, sperm ducts and glands (help gametes to fuse)
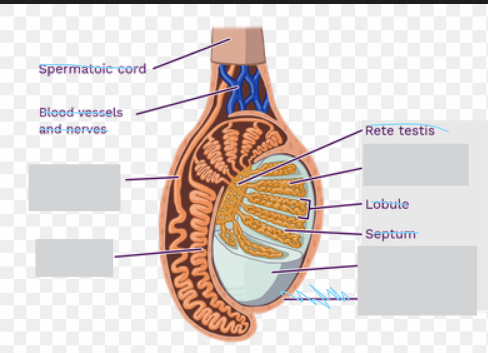
Testes
produce sperm
produce testosterone
Scrotum
sac of skin which holds the testes
sperm need a temperature of 2/3 degrees lower then the body temperature to develop
being situated of the abdominal cavity allows this temperature to be achieved
when cold - muscles in the scrotum contract to bring the testes closer to warmth of the body, heat they relax
Seminiferous Tubules
they produce spermatozoa/sperm through spermatogenesis
Leydig cells in between the tubules produce testosterone
sertoli cells are also located in the testes - nourish developing sperm
List the Sperm Ducts
vasa efferentia (vas efferens sing.)
epididymis
vas deferens
urethra
Vasa Efferentia
carry sperm from the testis to the epididymis
Epididymis
coiled tube where sperm are concentrated
this is because of the reabsorption of fluid secreted by the seminiferous tubule
sperm mature and aquire the ability to swim - do not yet
Vas Deferens
sperm is stored here
passed to urethra
Urethra
connected to the bladder - pass urine
passes sperm from the vasa differentia through the penis
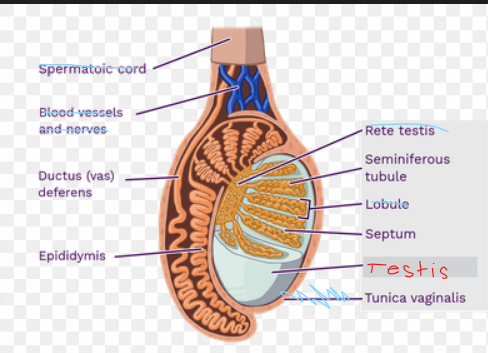
The Glands
seminal vesicles
prostate glands
cowper’s glands - bulbourethral glands
Seminal Vesicles
secrete a thick yellowish alkaline fluid which nourishes the sperm and helps to neutralize acidity of urethra
contains fructose - energy source, along with amino acids, enzymes and flavin (vitamin which provides nutrients to sperm and suppresses the female immune system so it doesn’t attack sperm)
empty into the ejaculatory duct during ejaculation
other chemicals may help sperm penetrate cervical mucus and cause peristaltic movement of the lining of uterus/fallopian tubes which help move sperm toward the ovaries
Prostate Gland
secrete a thin milky white alkaline fluid into urethra during ejaculation which helps to neutralize acidity
Cowper’s or Bulbourethral Glands
clear slightly alkaline fluid which helps to neutralize any acidity of remaining urine in the urethra
produce mucus which acts as a lubricant
produces prostate specific antigen → dissolve cervical mucus
PRODUCES ZN → STABILIZE SPERM DNA
Semen
mixture of sperm and gland secretions discharged during ejaculation
The Penis
contains erectile tissue which becomes engorged with blood when sexually excited - causing penis to become erect
this is bcs the arterioles dilate and accommodate more blood, thus compressing the venules meaning the blood moves into erectile tissue but cannot escape
this raises bp and erects the penis
this is closely related with the excretory system - urogenital system
Ovaries
primary sexual organs - female gametes are made
secrete estrogen and progesterone
outermost layer of the ovaries are made of germinal epithelial cells - produce gamete
middle is made of stroma - contains connective tissue, blood vessels and mature follicles
Oviducts - fallopian tubes
carry ova from ovaries to uterus
end of the tubes closest to the ovary have feathery projections - fimbriae
these move closer to the ovaries during ovulation
cilia lining fimbriae beat and cause a current which draws in the ovum after it is released from the ovary
cilia lining the oviduct beat and smooth muscle contracts causing peristaltic movements moving the ovum down the oviduct to the uterus
site of fertilization
Uterus
size/shape of an inverted pear
embryo implants itself into the wall of the uterus where it will grow during the duration of pregnancy
myometrium - outermost wall of uterus, smooth muscle, contracts strongly during birth
endometrium - many glands and highly vascularized - efficiently exchange nutrients with the placenta
Cervix
narrow entrance to uterus from vagina
plug of mucus blocks it - prevent infection
ring of muscle can close it
Vagina
muscular tube - contains elastic tissue
stretches during childbirth and during sexual intercourse
two folds of skin surround opening of it labia majora and labia minora
Clitoris
can become erect in response to sexual stimulation
equivalent to male penis
is there a urogenital system in women
no there are separate openings to the excretory and reproductive system
Gametogenesis
production of sperm/ova in the testes and ovaries
involve meiosis which occur from spore mother cells - spermatocyte or oocytes
1. multiplication stage - mitosis to produce many spermatogonia and oogonia
2. period of growth in preparation for first meiotic division
3. maturation stage which the first and second meiotic divisions occur
brief outline of spermatogenesis and oogenesis
germ cell —mitosis—> spermatogonia /oogonia
—growth to prepare for meiosis—→ 1* spermatocyte/oocyte
—meiosis 1——> 2 spermatocyte/oocyte
—meiosis 2—→ spermatid and ootid → sperm and ova
Secondary oocyte must be fertilized to form ova
Describe the process of spermatogenesis
seminiferous tubule has a wall with an outer layer of germinal epithelial cells - aka PGC!
pgc’s undergo mitotic divisions to form the spermatogonia - this occurs in the embryo
spermatogonia undergo more mitotic divisions to produce more spermatogonia - occurs during puberty
spermatogonia increase in size to form primary spermatocytes - these become embedded in the sertoli cells
1 spermatocytes undergo the first meiotic division forming 2 spermatocyte
2 spermatocyte undergo the second meiotic division forming 4 haploid spermatids
spermatids then develop into mature sperm
this takes around 2 months
Sertoli cells
infoldings of the surface membrane seminiferous tubules
carry out the remolding of spermatids → sperm
exchange of nutrients, oxygen and waste substance between developing sperm and blood vessels acting as a barrier between them and any harmful substance in the blood
secrete fluid to carry the sperm through seminiferous tubules - this is then later absorbed in the epididymis where sperm is concentrated and matures and become motile
Sperm
head contains the
nucleus with a haploid number of chromosomes
acrosome - contains hydrolytic enzymes which are involved in the penetration of the layers surrounding ovum
short neck has 2 centrioles, microtubule of one of the centrioles elongate during development and form the axial filament of the flagellum in a 9+2 microtubule arrangement
midpiece - many mitochondria to produce lots of atp needed to bring about beating movement of the tail
tail - activation of tail takes place in vagina, needed to orient spermatozoa and help penetrate oocyte, enable sperm to group up around oocyte
tail movements are insufficient to cover distance from vag to site of fertilization
streamlined → good for locomotion
Hormonal Control of Spermatogenesis
controlled by the hypothalamus and anterior pituitary
Hypothalamus secretes gonadotrophin-releasing hormone (GnRH)
this stimulates the anterior pituitary to secrete gonadotrophins - FSH and LH
Follicle Stimulating Hormone: this stimulates the sertoli cells to convert spermatids → sperm
Luteinizing Hormone: synthesis of testosterone by the Leydig Cells
FSH and LH use a second messenger cyclic AMP - goes to nucleus to stimulate the synthesis of enzymes
Testosterone: stimulates sperm production, stimulates Sertoli cells, affects primary and secondary sexual characteristics
Testosterone - negative feedback, inhibits GnRH (decreasing FSH/LH - decreasing sperm production). It also acts directly on ant pit to reduce LH further
Inhibin; released from the Sertoli cells and reduces secretion of FSH and reduces GnRH
inhibin is released in amounts proportional to sperm count, high sperm count, high inhibin, to inhibit spermatogenesis
Secondary Sexual Characteristics - Males
deeper voice due to thickening of the larynx caused by testosterone
enlargement of the penis, testes and glands
increased muscle development
growth of pubic hair
Describe the process of Oogenesis
oogonia are produced during fetal development
oogonia undergo mitosis and form primary oocytes which enter prophase I
primary oocyte grows large due to the development of ribosomes, rna, energy stores
primary oocyte is enclosed by a single layer of granulosa cells → PRIMORDIAL FOLLICLE
primordial follicle → Graafian follicle
as the follicle changes the primary oocyte must become an ovum through;
primordial follicle → primary follicle ( granulosa cells multiply around primary oocyte + theca develops over these layer of granulosa cells from stroma)
primary oocyte undergoes meiosis I producing a haploid secondary oocyte and a polar body
antrum develops inside the follicle - now this is a secondary follicle (secondary ooctye inside)
growth of follicle+ secondary oocyte + fully formed antrum → Graafian Follicle
second meiotic division proceeds as far as metaphase II but doesnt continue unless fertilization occurs
FERTILIZATION; secondary oocyte + polar body —→ meiosis II producing the OVUM and a second polar body
1st polar body makes a 3rd polar body - these all disintegrate
Functions of Oestrogen
brings about female secondary sexual characteristics
enlargement of breast
growth of pubic hair
widening of hips
Hormonal Control of the menstrual cycle - preovulatory or follicular phase
hypothalamus secretes GnRH which stimulates the anterior pituitary to release FSH and LH
FSH stimulate primordial follicles to develop - however only one follicle will complete development
as the primary follicle develops the granulosa cells on the follicle being to secrete oestrogen
stimulates thickening of the endometrium lining
inhibits FSH (prevents more follicles from developing)
stimulates secretion of LH at high concentrations toward the midpoint of the cycle
LH stimulates the graafian follicle to rupture - triggering ovulation
→ at this stage oestrogen has an inhibitory effect on the hypothalamus
Hormonal Control During ovulation
occurs during the midpoint of the cycle
graafian follicle at this point is secreting lots of oestrogen
FSH and LH are released in a surge once oestrogen exceeds a threshold limit
LH; causes ovulation release of the secondary oocyte from the graafian follicle - this surge ensures precise timing of ovulation
stimulates remaining graafian follicle to develop into the corpus luteum
ovulated oocyte consists of a secondary oocyte arrested in metaphase II
zona pellucida - glycoproteins secreted by follicle cells
corona radiata - layer of granulosa cells protecting and nourishing the oocyte
→ oestrogen has a stimulatory effect on the hypothalamus
Hormonal Control in the postovulatory or Luteal Phase
Corpus luteum continues to secrete oestrogen and progesterone - these make sure that the lining of the uterus is ready for implantation of a fertilized ovum
oestrogen inhibits FSH and maintains the endometrium
progesterone
stimulates the uterus to maintain its thickening
inhibits LH and FSH
associated with a rise in body temperature just after ovulation
if fertilization DOESNT OCCUR corpus luteum degenerates, hence oestrogen and progesterone levels drop
endometrium lining breaks down - menstruation (prostaglandins help by causing contraction of uterine muscles)
release of fsh and lh is no longer inhibited
ovum dies after the 36hrs of being shed in the oviduct
What happens if fertilization occurs
ovum forms - meiosis II completes
oestrogen and progesterone continue to be produced maintaining the endometrium lining
the ovum then implants itself into the endometrium lining - abundance of nutrients and rich blood supply
How do birth control pills work
contain hormones which resemble progesterone and oestrogen
negative feedback on hypothalamus and anterior pituitary
Copulation
sexual stimulation involves stimulation of the parasympathetic nervous system
penis becomes erect
inserted into the vagina, rhythmic movements produced during sexual intercourse cause friction increase stimulation of cells at the tip of the penis
activates sympathetic nervous system - ejaculation
lubrication - mucus secreted by copwer glands and glands in vag and vulva
clitoris also becomes erect
female orgasm - muscular contractions of both the vagina and uterus
Passage of Sperm to ovum
sperm are deposited at the top of the vagina close to the cervix
cervix is normally blocked by a thick mucus
thins during the first part of the menstrual cycle
release of progesterone after ovulation causes it to thicken once more
contractions of uterus and oviducts - caused by prostoglandins in the semen and hormones such as oxytocin released during copulation + action of cilia lining uterus and oviducts allow the sperm to travel to the oviducts
it takes about 4/8 hours for most sperm to reach oviduct
can survive for 1-3 days - most fertile for 12-24 hours
Capacitation
when sperm undergo a series of physiological changes making it capable of fusing w oocyte
removal of plasma proteins and glycoproteins from outer surface of the sperm by enzymes in the uterus
loss of cholesterol from the membrane - weaking it
increased permeability to Ca2+ ions - increasing beating of the tail and promotes the acrosome reaction
Acrosome reaction
sperm makes contact zona pellucida and the cell surface membrane of the sperm next to the acrosome and membrane of acrosome rupture
hydrolytic enzymes - hyaluronidase and proteases are released from acrosome
allows sperm to digest w zona pellucida
Fertilization
Fusion of the sperm nucleus with the ovum Nucleus to form a diploid cell - zygote
Explain in detail the stages of fertilization
hyaluronidase is released by the acrosome’s and digest a path through hyaluronic acid which holds the follicle/granulosa cells together.
Sperm reach the outer surface of zone pellucida where it binds to specific receptors - these receptors are species specific
Proteins are then released and digest through the zona pellucida
Head of sperm reaches membrane of oocyte, other proteins cause adhesion of sperm to oocyte and fuses with microvilli on oocyte and penetrates cytoplasm
Sperm binding induces Ca2+ to be released and this induces a fertilization membrane to form - zona pellucida thickens and harden through the release of enzymes. - cortical reaction, prevents other sperm from fusing. Furthermore enzymes destroy sperm receptor sites
Ca2+ activates oocyte metabolism and the second meiotic division is completed
Nucleus of sperm swells as chromatin unravels
Male and female pronucleus form - fertilization. New nucleus is diploid and known as a zygote. Undergoes mitosis
Define implantation
the embedding of a blastocyst into the endometrium usually done through protein digesting enzymes
Describe implantation
As the zygote passes down oviduct it undergoes cleavage - mitosis division w out an increase in size due to zona pellucida
Morula is formed
blastocoel forms - cavity filled with liquid from oviduct, at this point the embryo is called a blastula, individual cells are blastomeres and the outer layer of cells is called the trophoblast
In a part of the blastula the trophoblast forms an inner cell mass
Blastula arrives in uterus and the zona pellucida disappears.
Trophoblast cells make contact with endometrium and begin absorbing nutrients
Due to presence of nutrients trophoblast cells multiply and 6-9 days after fertilization a protein digesting enzyme is secreted by blastula to embed itself in the endometrium - this is implantation
What happens after implantation
Trophoblast cells secrete human chorionic gonadotrophin - HCG and this prevents breakdown of corpus luteum
Corpus luteum continues to secrete progesterone and oestrogen leading to increased growth of the endometrium
Cells of trophoblast differentiate into an inner and outer layer
Outer layer: chorion - chorionic villi, increase SA of contact w maternal blood
Hydrolytic enzymes released by trophoblast cause blood vessels in endometrium to break down and fill spaces between chorionic villi
Exchange of substances occurs through chorionic villi until
Placenta takes over
Describe the development of the extra-embryonic membranes
Trophoblast cells develop into chorion
inner cell mass develops into the amnion and the yolk sac
Amnion - thin protective layer contains amniotic fluid protecting embryo from physical damage
Yolk sac has no function in humans
other cells of the inner cell mass give rise to the embryo- differentiation into endoderm and ectoderm and later on mesoderm - gastrulation
Ectoderm develops into brain and spinal cord 3rd week
Allantois develops - grows out toward chorion and forms an allantochorion which gives rise to placenta
6 weeks - fetus and after gestation period of 38 weeks birth
what is the placenta
composed of cells derived from fetus and mother
Allows exchange of materials
Develops after 12 weeks
Describe the structure of the placenta
→ fetal part
consists of chorionic villi to increase SA
These villi contain branches of umbilical arteries and veins
Umbilical cord is a tough structure and it’s where the umbilical arteries and veins run through
→maternal part
projections from the endometrium
Between this and the chorionic villi there are spaces supplied with arterial blood
Blood flows through spaces from arterioles to venules in the uterus wall
BLOOD NEVER MIXES
Why is it important blood doesn’t mix in the placenta
Relatively high blood pressure of mom isn’t exposed to baby
ABO groups may not be compatible -
Describe the mechanisms of uptake across the placenta
Chorionic villi have microvilli which increase surface area for active transport and diffusion and facilitated diffusion
Cells contain many mitochondria and carrier molecules for active transport
Numerous small vesicles are found inside cells of villi - pinocytosis
Water - osmosis l, glucose - facilitated diffusion, ions - active transport / diffusion , amino acids iron and vitamins - active transport
oxygen diffuses from mom to fetal blood as fetal blood has higher affinity for oxygen
Carbon dioxide and nitrogenous wastes are diffused to mother
Antibodies can cross the placenta from mother to fetus - passive immunity
Placenta as an endocrine organ
takes over role of corpus luteum in secreting progesterone and oestrogen
HCG - maintain activity of corpus luteum until placenta takes over
Human Placental Lactogen: growth and development of breasts - needed before oestrogen and progesterone can affect the breasts
What are contractions during birth attributed to
decrease in progesterone (progestone inhibits contractions)
oestrogen → because it makes the uterus more sensitive to oxytocin
Describe the Hormonal Control that undergoes during contractions
oestrogen production increases
progesterone levels decrease - baby hypothalamus releases ACTH which stimulates release of cortiocosteroids from adrenals, crosses into mother circulation and this causes a progesterone decrease and an increase in prostaglandins
stretching of uterus by fetus and pressure on cervix by fetal head - oxytocin release
First Stage
cervix starts to dilate
mild contractions, mucus plug is lost and amnion is burst releasing more amniotic fluid
contractions get stronger - POSITIVE FEEDBACK OF OXYTOCIN, more uterus contracts, more stretch receptors are stimulated, more release of oxytocin
contractions spread from top to bottom
cervix dilates
once baby + placenta r expelled stretch receptors arent stimulated so contractions stop
Second Stage of Birth
baby is pushed out of uterus and down vagina - head first
umbilical cord is clamped and cut
Third Stage
placenta detaches from the wall of the uterus and passes it out through the vagina
bleeding is limited by vasoconstriction of the blood vessels of the uterus which supply placenta
Define Lactation
production of milk
Describe the structure of the mammary glands/breasts
special epithelial cells line cells called alveoli - secrete milk
alveoli r surronded by smooth muscle fibers
attached to series of ducts which lead to sinuses (store milk)
passed through separate opening in the nipple
Hormones in development of breasts and milk
progesterone - breasts increase in size
ducts - oestrogen
prolactin produces milk - secreted by ant pit
presence of oestrogen and progesterone inhibits secretion of prolactin, however at birth when oestrogen and progesterone lvls fall - prolactin isnt inhibited
Contents of Human Milk vs Colostrum
milk - fat, lactose, lactalbumin, casein
colostrum - first secretion of breasts, rich in globulin, low in fat, passes antibodies IgA from mom to baby
Suckling Reflex
milk ejection reflex
sucking of baby on breast - nerve impulse to hypothalamus - oxytocin (post pit)
contraction of smooth muscle around alveoli and forces milk outta nipples
release of prolactin is also stimulated - produce milk for next feed
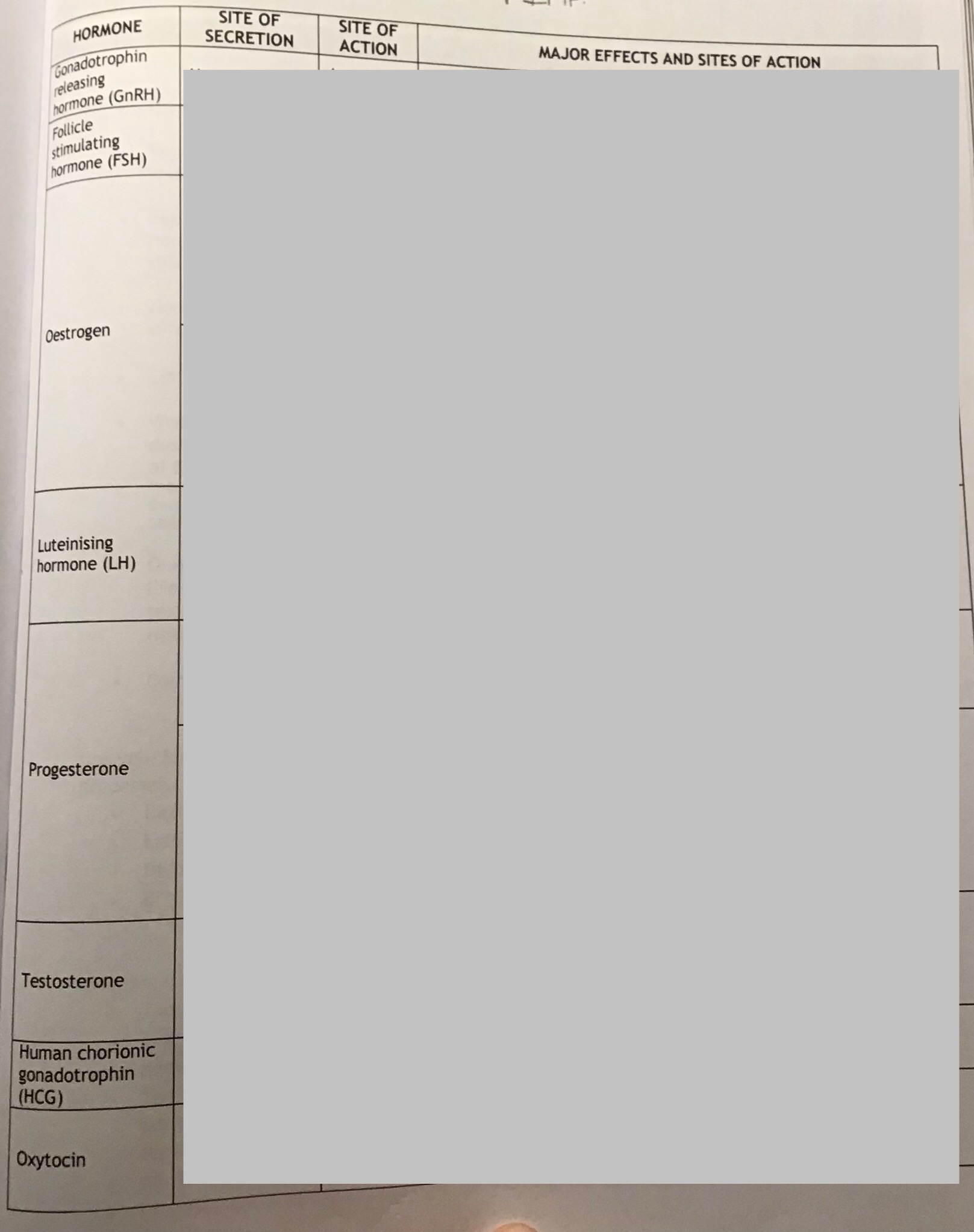
tanti hormone summary V imp
