Dermatology Exam
1/10
Earn XP
Description and Tags
(My answers)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
Which are the most common sites of seborrheic dermatitis and why?
Regions with high sebaceous gland density, especially on a seborrheic background, most commonly on the nasolabial folds, forehead, scalp, and sternal region.
Describe the timing of the patch test and the crescendo reaction:
Apply an adhesive-mounted patch containing minute amounts of standard contact allergens to the sensitized patient’s upper back at time zero (T0). Remove the patch and assess the skin (via Wilkinson scoring system) after 48 hours (T1). In cases of a doubtful reaction (e.g., faint erythema), a second reading is performed at 72 hours (T2) to help differentiate a true allergic response from irritant or adhesive-related effects (e.g., "patch effect"). In case of a true allergic response, there is a progressive increase in reaction severity from the 48 to 72 hours (positive crescendo reaction).
What is the target of Dupilumab?
Dupilumab is a fully human monoclonal IgG4 antibody that antagonizes the IL-4 receptor alpha subunit (IL-4Rα) shared by IL-4 and IL-13 receptor complexes
(This inhibits the signaling of IL-4 and IL-13 cytokines belonging to type 2 (Th2)-mediated inflammation).
Clinical Case: A 16-years old male complains of itching of the face. He has a personal and family history of atopy (allergic rhinitis and asthma). The dermatologic examination revealed an erythema with small vesicles at the level of the armpit, consistent with eczema. A previous treatment with topical corticosteroids had temporary results. The patient is otherwise fine and has no other complaints. Which is the most plausible diagnosis in this patient?
Atopic dermatitis
List 5 differences between ICD (irritant contact dermatitis) and ACD (allergic contact dermatitis):
Pathogenesis: ICD is a localized inflammatory skin response to chemical, physical or biological agents, whilst ACD is a delayed type IV hypersensitivity reaction occurring in sensitized individuals after re-exposure to a specific allergen.
Major complaint: The major complaint, particularly in the acute setting, is burning in ICD, whilst pruritis in ACD.
Margins: For ICD, the margins are sharp, strictly confined to the site of exposure, whilst in ACD they are blurred, spreading to the periphery.
Patch test: In ICD, the patch test is used for exclusion, whilst in ACD it is diagnostic.
Histopathology: In histopathology of ICD, mild spongiosis, necrosis and modest inflammatory polymorphonuclear (PMN) infiltration is seen, as opposed to spongiosis, keratosis and eosinophilic infiltration seen typically in ACD.
The anatomical distribution of eczema according to age in atopic dermatitis?
Infants and young children (0–5 years): typically affects the face, especially the cheeks, with characteristic central facial sparing (periorbital and perioral regions). It also shows a predominantly extensor distribution on the legs and trunk.
In children (6–11 years): the distribution shifts to flexural areas (e.g., elbows and knees). Common features include the "atopic dirty neck" and chronic dry eczema.
In adolescents and adults (>12 years): there is a more variable distribution, often involving skin folds, hands, wrists, feet, eyelids, head and neck, upper trunk, shoulders, and scalp.
Which are the criteria for the diagnosis of atopic dermatitis?
Proposed by Hanifin and Rajka (1980)
Include major and minor criteria
Diagnosis is made when ≥3 major criteria + ≥3 minor criteria are met
The major criteria (4) are:
Pruritus
Typical morphology and distribution
Chronic/chronically relapsing dermatitis
Personal/family history of atopy
The minor criteria:
Xerosis
Ichthyosis
Keratosis pilaris
Palmar hyperlinearity
Positive skin prick test
Elevated serum IgE
Early age of onset —> infants + children
Increased risk of infection —> immunosuppression
Risk of non-specific hand or foot dermatitis
Exacerbation by environmental or emotional stress
Nipple eczema
Cheilitis
Recurrent conjunctivitis
Increased risk to develop cataracts
Dennie-Morgan infraorbital folds
Orbital darkening
Pityriasis alba
Intolerances (wool or food) —> sensitized
White dermographism
Facial pallor or erythema
Anterior neck folds
List 5 pathophysiological mechanisms leading to blister formation:
1) Acantholysis
2) Spongiosis
3) Cytolysis
4) Subepidermal blistering
5) Mechanical blistering
Clinical Case: A 30-year-old man presents to your clinic with a complaint of recurrent blistering lesions located on both elbows and knees. He reports that these skin eruptions have been persistent for approximately two years. His medical history is notable for type 1 diabetes mellitus and autoimmune thyroiditis. He shares that he has had a deep-seated aversion to hospitals since his childhood diagnosis of diabetes, and generally avoids medical facilities unless absolutely necessary. He finally sought medical attention due to intense pruritus, which has become intolerable and is significantly affecting his daily activities. A review of his family history reveals that his maternal grandparents emigrated from Sweden to the UK, reportedly because his grandfather was diagnosed with lymphoma (though the patient is unsure of the specific type). On examination, he appears pale, of short stature, and has a lean build. Nikolsky sign is negative. Multiple erythematous vesicles are observed in a symmetrical pattern on the medial aspects of his buttocks. Direct immunofluorescence testing reveals granular IgA deposits along the apical part of papillae at dermoepidermal junction. What is the most likely diagnosis?
DERMATITIS HERPETIFORMIS, which is a cutaneous manifestation of Celiac Disease
SKIN LESIONS
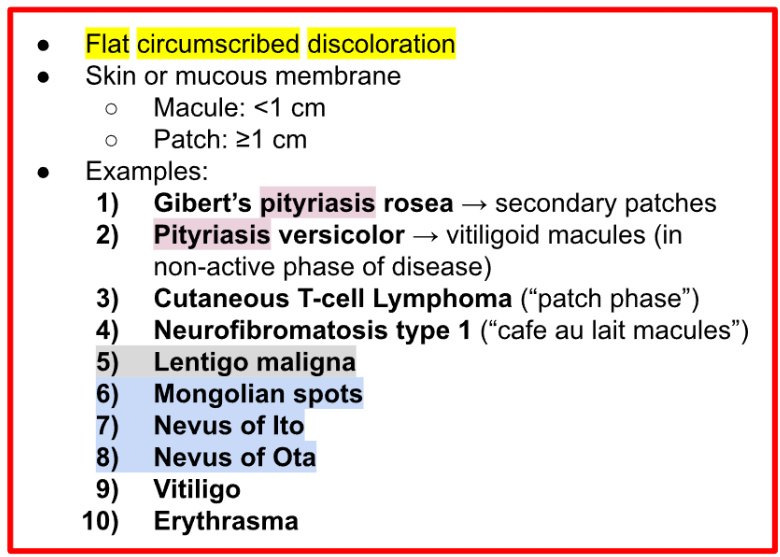
Define macules and patches and list the names of 10 diseases that appear with these lesions.
SKIN LESIONS