Gram-negative Cocci
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
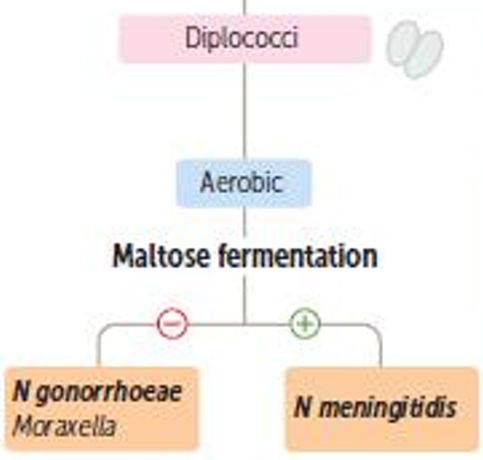
What’s a distinctive biochemical feature between N. gonorrheae and N. meningitidis and Moraxella
N, meningitidis can ferment maltose
N. gonorrheae and Moraxella cannot ferment maltose
What are the reservoirs for N. gonorrheae?
Only humans
What are the documented modes of transmission for N. gonorrheae?
Sexual (any kind)
Vertical (Mother to neonate ocular infection)
Non-sexual transmission not documented
What are the virulence factors of N. gonorrheae?
IgA proteases
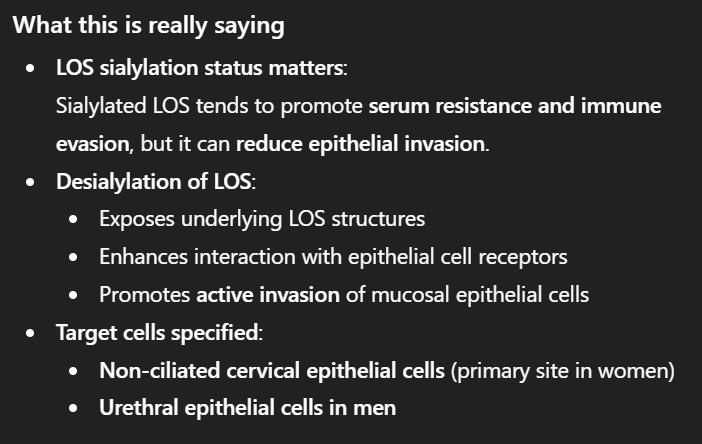
Lipooligosaccharides LOS (Strong endotoxin)
Antigenic variation of pili (shuffle pili genes → Escape IS
What does N. gonorrhoeae cause in men?
If untreated, epididymitis and prostatitis
What does N. gonorrhoeae cause in women?
If untreated: Urethral stricture, salpingitis, tubo-ovarian abscess, PID, Fit-HughCurtis syndrome, Sterility
What does N. gonorrhoeae cause in neonates?
Ophthalmia neonatorum (conjunctivitis) 2-5 days after birth
What if N. gonorrhoeae remains untreated for too long
Bacteremia and septic arthritis
How is N. gonorrhoeae diagnosed in males
We take a urine sample from patients who have not urinated in at least 2 hours, also intraurethral swabs (discharge at the meatus), and intrarectal swab
N gonorrhoeae diagnosis in women
Swabs from: cervix, vagina, urethra, rectal, endometrium, Skene/ Bartholin glands
Common methods of diagnosis in men & women
Oropharyngeal swabs (oral sex)
Blood
Fluid from arthritic joints
Nucleic acid amplification test
What morphological characteristics
IC kidney-beaned shaped Gram-negative diplococci inside Polymorphonuclear cells (Neutrophils and stuff)
N. gonorrhoeae culture medium
Modified Thayer-Martin agar
They are capnophiles and require 5-10% CO2.
They’re also very delicate and autolytic and must be cultured right after specimen acquisition
N. gonorrhoeae Biochemical characteristics
Glc +
Proline arylamidase +
Maltose -
Levulose -
Saccharose - (They are saccharolytic)
Gamma gt -
N. gonorrhoeae treatment (Venereal and neonatal)
Venereal: Single dose IM ceftriaxone, and if chlamydia isn’t yet ruled out, must also add doxycycline
Neonatal: Erythromycin eye ointment → Prevent neonatal blindness
N. gonorrhoeae treatment
Pretty common, β-lactamases
N. gonorrhoeae prevention
Safe sex
Treatment of partner
N. gonorrhoeae vaccine
None, antigenic variation
What are the hosts for N. meningitidis
Only in humans, it normally colonizes the oropharyngeal and nasopharyngeal tracts. Carrier rate is 8-20%
N. meningitidis transmission mode
Respiratory droplets
What are the symptoms of N. meningitidis bacteremia
When N. meningitidis enters the bloodstream, it releases LOS endotoxins in large amounts and causes the following:
Waterhouse-Friderichsen syndrome - acute hemorrhagic adrenal insufficiency
Petechiae
Purpura
Adrenal hemorrhage
DIC
Shock
*Note: While bacteremia may lead to meningitis, patients can easily die from the symptoms before ever getting meningitis (19-70% mortality at this stage)
Explanations
Petechiae and purpura result from endotoxin-induced endothelial injury and DIC, while adrenal hemorrhage causes acute adrenal insufficiency.
DIC leads to microthrombi everywhere + bleeding everywhere → Adrenal glands normally have very high blood flow, and this blocks it → Bilateral adrenal hemorrhage → Hemorrhagic adrenal insufficiency
What are the epidemiological characteristics of meningococcal meningitis?
2nd most common meningitis (King is S. pneumoniae - pneumococcus)
Sporadic in young children
Outbreaks: Occur among adults in crowded living conditions (dorms/army)
How would you describe meningococcal meningitis in children and adults?
What’s its mortality rate?
Rapidly progressive 7-13%
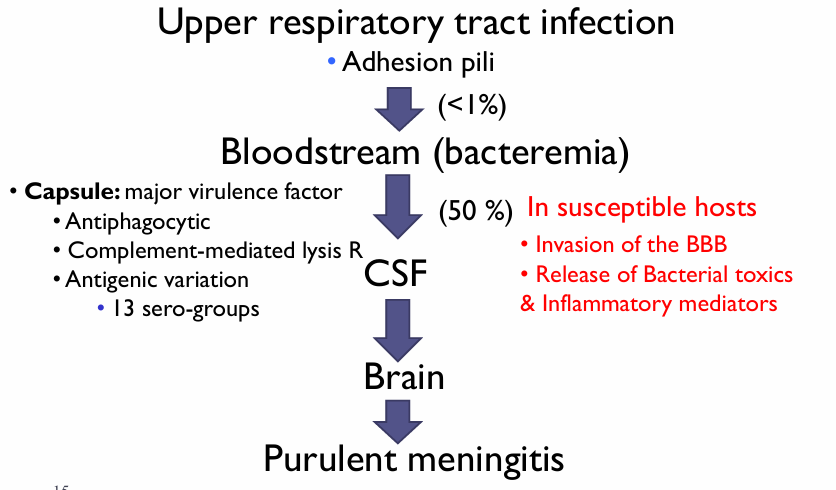
Describe Meningitides’ capsule as a virulence factor
Antiphagocytic
Resistance to complement-mediated lysis
Contributes to antigenic variation (13 serogroups)
Progression to meningitis chart
N. meningitidis invasive serotypes
A, B, C, Y and W135
A, B, C cause 90% of meningococcal diseases
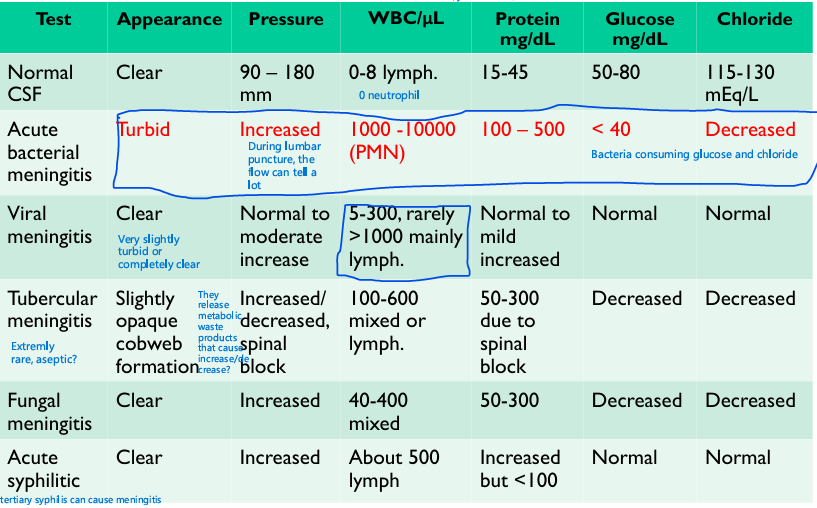
Compare the 6 types of meningitis depending on:
- CSF appearance, pressure, WBC/uL, Protein mg/dL, Glucose mg/dL, Chloride
What’s the best way to diagnose Meningococci
Gram stain on CSF → Find IC and EC encapsulated diplococci with flat adjacent sides
PCR on serum and CSF
Immunofluorescent test kits for CDF available commercially for: NHS
Extra:
Although meningococcal meningitis requires bacteremia, blood tests alone are insufficient because bacteremia may be transient, while CSF directly samples the infected compartment, provides higher diagnostic yield, and distinguishes bacterial meningitis from other causes.
How do we culture meningococci
Modified Thayer-Martin agar
→ Obligate aerobe
→ Capnophile → 5-10% CO2
A patient presents subacute illness, focal neurological deficits, seizures, or a contiguous ENT source, and a history of COM, sinusitis, dental infection, or recent surgery what do you do?
These symptoms fit the clinical presentation of brain abscesses, which is caused by anaerobes.
HOWEVER, we must still rule out meningococci, because missing meningococci is catastrophic, and time-critical, so:
→ The CNS specimen must be split between the aerobic, capnophilic, modified Thayer-Martin, and Robertson’s cooked medium: allows us to cultivate Bacteroide and anaerobic cocci
What are the biochemical characteristics of N. meningitidis
Maltose +
Glc +
Gamma GT+
ONPG -
Neisseria meningitidis treatment and prophylaxis and vaccination
Treatment:
Ceftriaxone
Penicillin G
Prophylaxis:
Rifampicin + Ciprofloxacin/ Ceftriaxone
Vaccination:
Polyvalent vaccine for ACYW135
New vaccine for B group (high-risk individuals)
Where can we find Moraxella catarrhalis?
1-5% of adults carry it in their URT
Children and older adults may have HIGHER frequencies
What clinical conditions can Moraxella catarrhalis cause
Otitis media, sinusitis, bronchitis, pneumonia
How do we culture M. Catarrhalis
Specimen: Sputum / sinus biopsy / Middle ear pus
Morphology: Coccobacilli
Culture: Incubation conditions similar to gonococci, BUT grows on NA and does not require increased CO2
M. catarrhalis Biochemistry
Ox +
Cat +
DNase +
Tributyrin +
What helps us differentiate between M. catarrhalis and Neisseria
Moraxella catarrhalis does not ferment any sugars: Glc - / Lac - / Mal - / Suc -