Lecture 13: Control/Prevention of Infectious Disease + Vaccine Distribution
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
What diverse priority grouping can vaccine distribution be dependent on
A. Occupation
B. Sickest or most medically vulnerable
C. Stages of life
D. Social vulnerability
E. Procedure applied to whole population (lottery)
How can occupation play a role in priority grouping
1. Healthcare workers (HCW) Professional status & proximity to pandemic-affected patients
2. Vaccine manufacturers
3. Emergency services workers
4. Basic infrastructure (Food distribution, transportation, etc.)
How can stages of life play a role in priority grouping
1. Children
Minimize infection in community
Longest life ahead
2. Adolescence to pre-middle age
Future collective benefit
How can social vulnerability a role in priority grouping
‘Hard-to-reach’ groups
Socially stigmatized (Ex: Homeless, Prisoners, obese)
How can vaccine procedure be applied to whole population
Applied to whole population instead of setting priority groups in advance
Example: lottery system
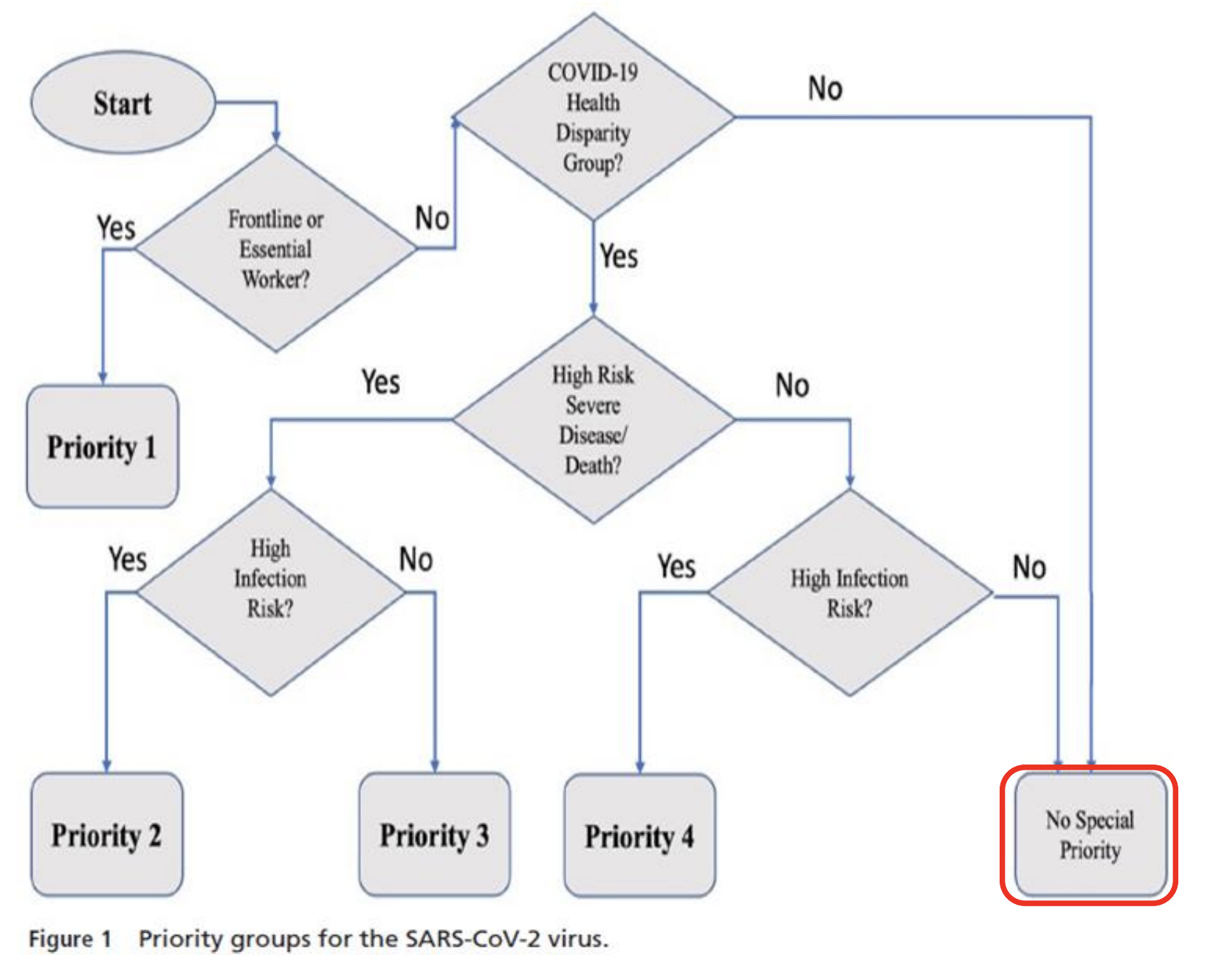
Priority Group 1 for Covid-19 vaccine?
Frontline/essential workers
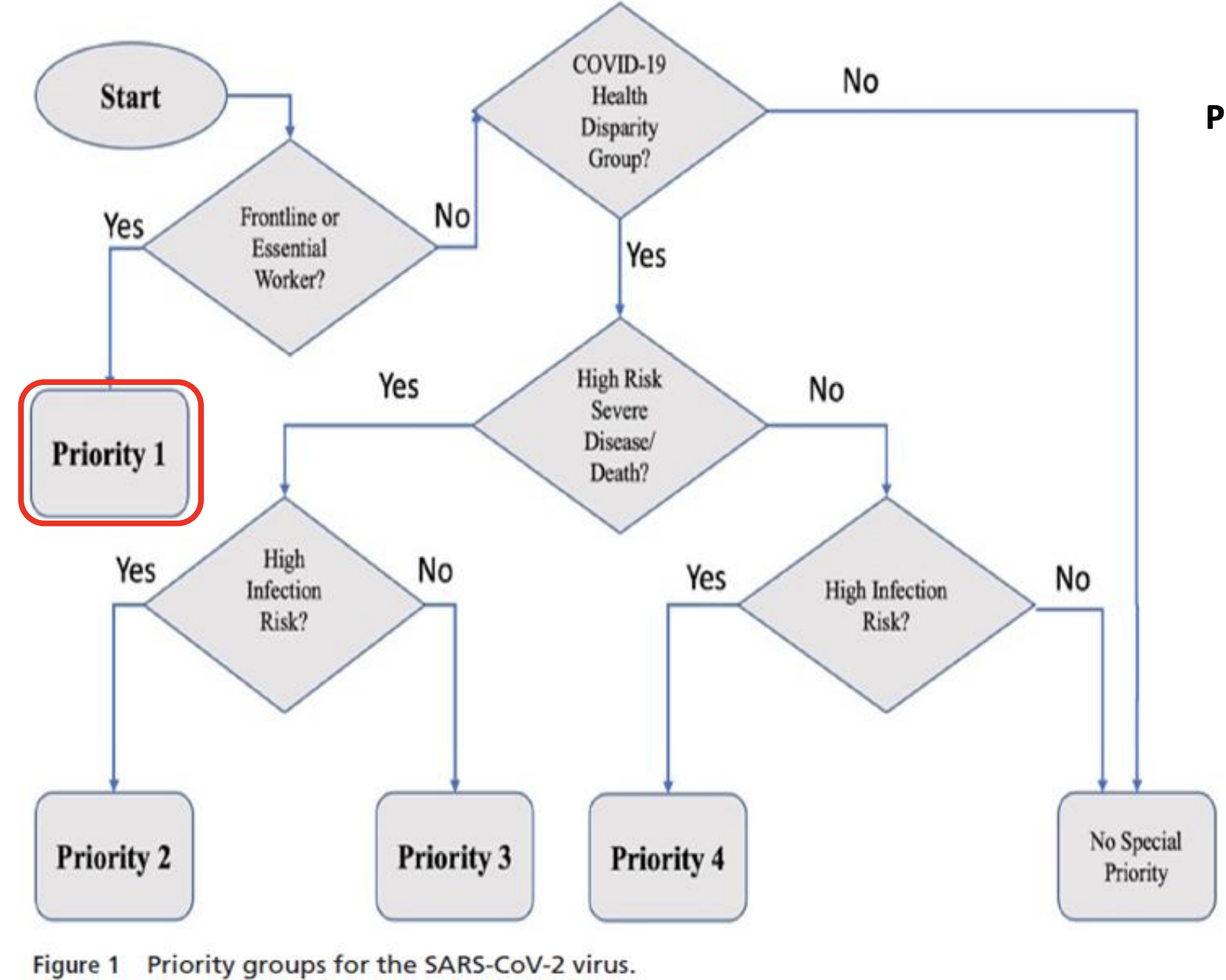
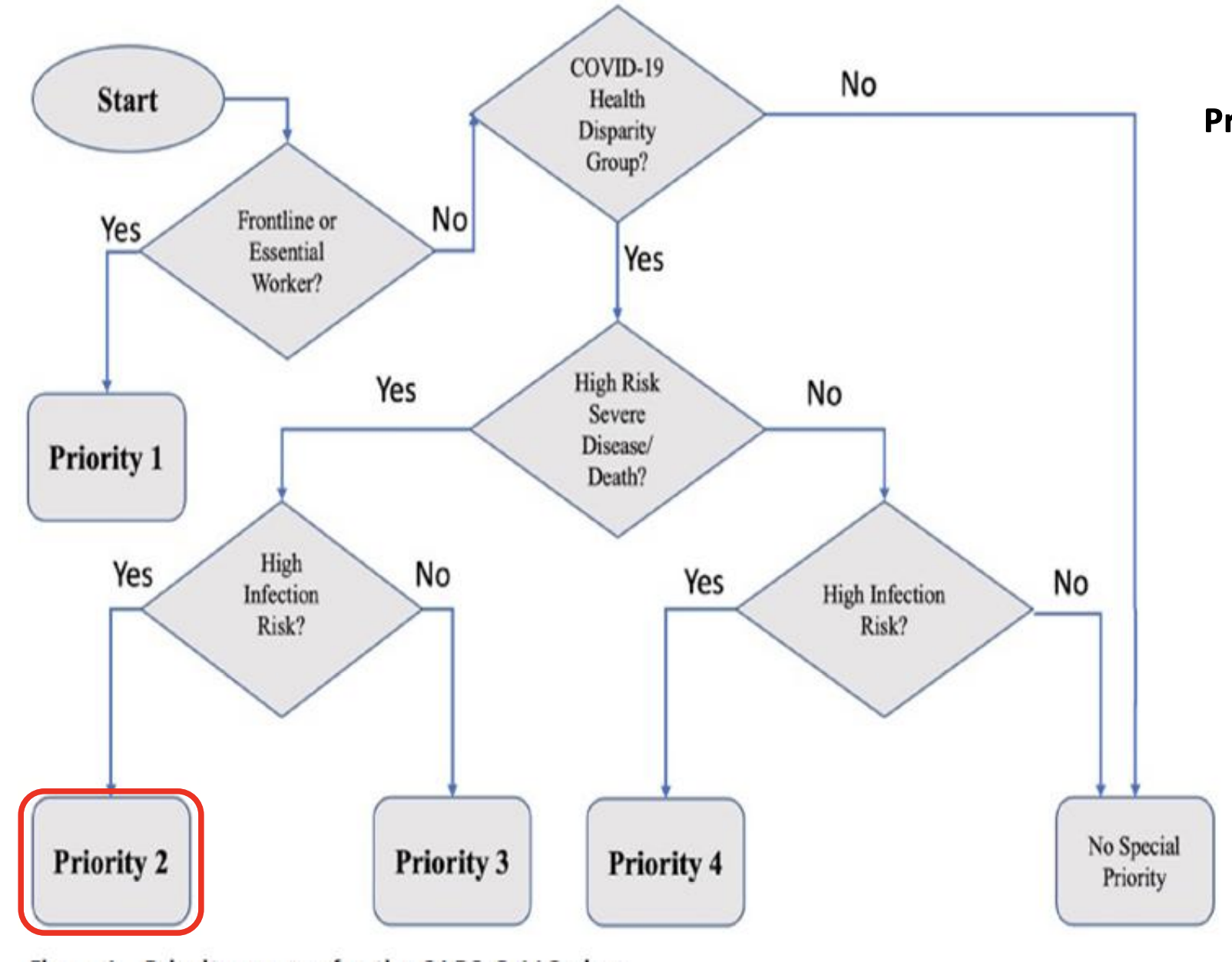
Priority Group 2 for Covid-19 vaccine?
Covid-19 Health Disparity Group
High risk for severe disease
High infection risk
ex:
Age 65+ in nursing home
Racial/ethnic groups with higher risk of infection, severe disease, death
Underlying chronic conditions linked to high risk & live in crowded environments
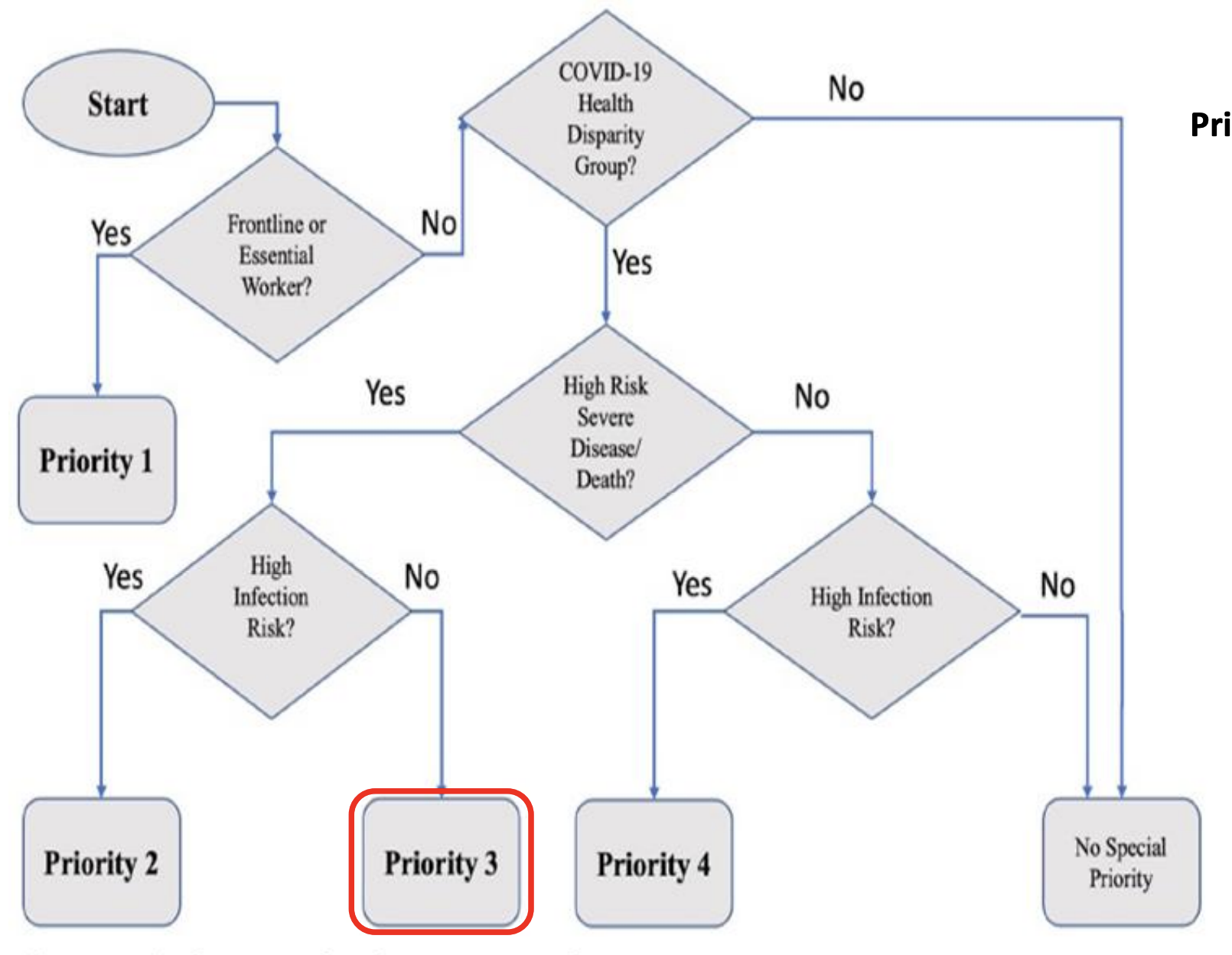
Priority Group 3 for Covid-19 vaccine?
Covid-19 Health Disparity Group
High risk for severe disease
No high risk for infection
Underlying chronic conditions linked to higher risk of severe disease/death who can safely socially distance
ex:
High BMI who attend school remotely
65 or older who can work remotely and shelter at home
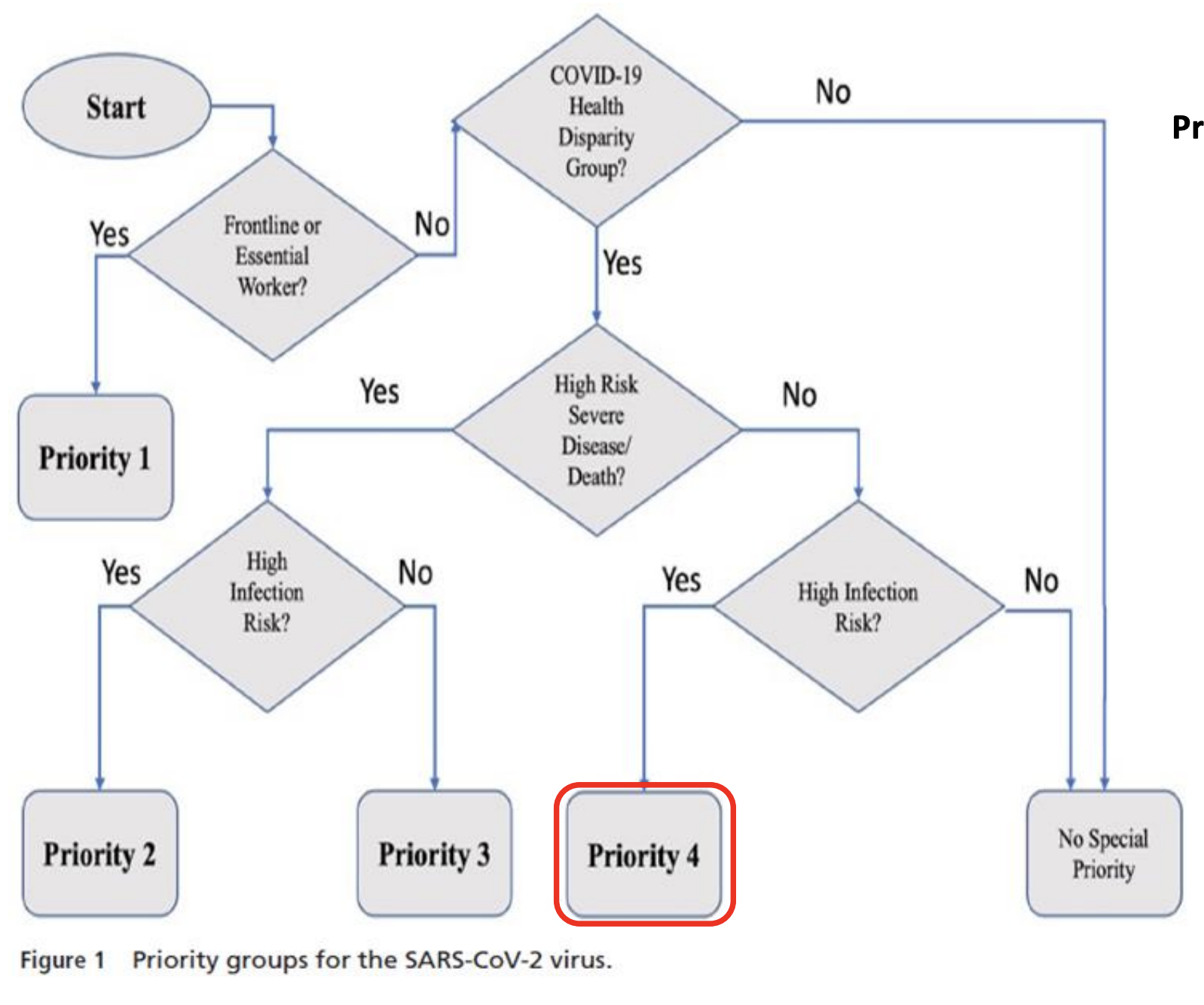
Priority Group 4 for Covid-19 vaccine?
Covid-19 Health Disparity Group
No high risk for severe disease
High risk for infection
ex:
Young, healthy adults working in crowded environments
Young, healthy adults aged 18 – 22 living in college dorms
Healthy adults under age 65 or older living in prisons '
Healthy adults under age 65 or older working in high-exposure environments
Who gets no priority for covid-19 vaccine
Not in Covid-19 health disparity group
Not an essential/frontline worker
OR
In Covid-19 health disparity group
No high risk severe disease/death
No high risk infection
What matters the most when it comes to vaccine distribution
Prevent the most illness
Save the most lives
Benefiting greatest # of people
Maximizing quality of life years saved (QALYS) & minimizing years of life lost (YLL)
Promoting justice, solidarity and trust in government and public health systems
Who is it most important to save when it comes to vaccine distribution
Saving the worst off
Saving those most likely to recover
Saving those most likely to contribute to a flourishing society
Saving those who can most usefully contribute to minimizing impact of pandemic
Targeting those most likely to play significant role in spreading infections (i.e., children)
What do those most likely to get a vaccine have?
rapid digital connection
time to repeatedly refresh link or hold on phone for hours
ability to travel to vaccination site (often by car)
trust in safety and efficacy of vaccine
What are some reasons people w/ high risk for severe illness/death do not seek vaccine
lack of awareness
barriers to vaccine access
concerns about vaccine
Strategies to mitigate disparities
Prioritize to zip codes most severely affected (typically have high index of economic hardship)
Partner with local health care institutions, community organizations, and other trusted sources to promote vaccine awareness & uptake
Prioritize distribution to those who face mobility/transportation barriers
Simplify registration process
How to prioritize distribution to those who face mobility/transportation/time barriers
Deliver vaccine to homebound older person
Vaccination sites near public transportation
Hours of operation accessible to those who work during standard business hours
How to simplify vaccine registration process
Have options that don’t require internet or digital platforms
Accessible to those with limited English proficiency or limited literacy
Should not require nonessential documentation
Options that do not require pre-registration
Various ways a pathogen can be eliminated from an environment
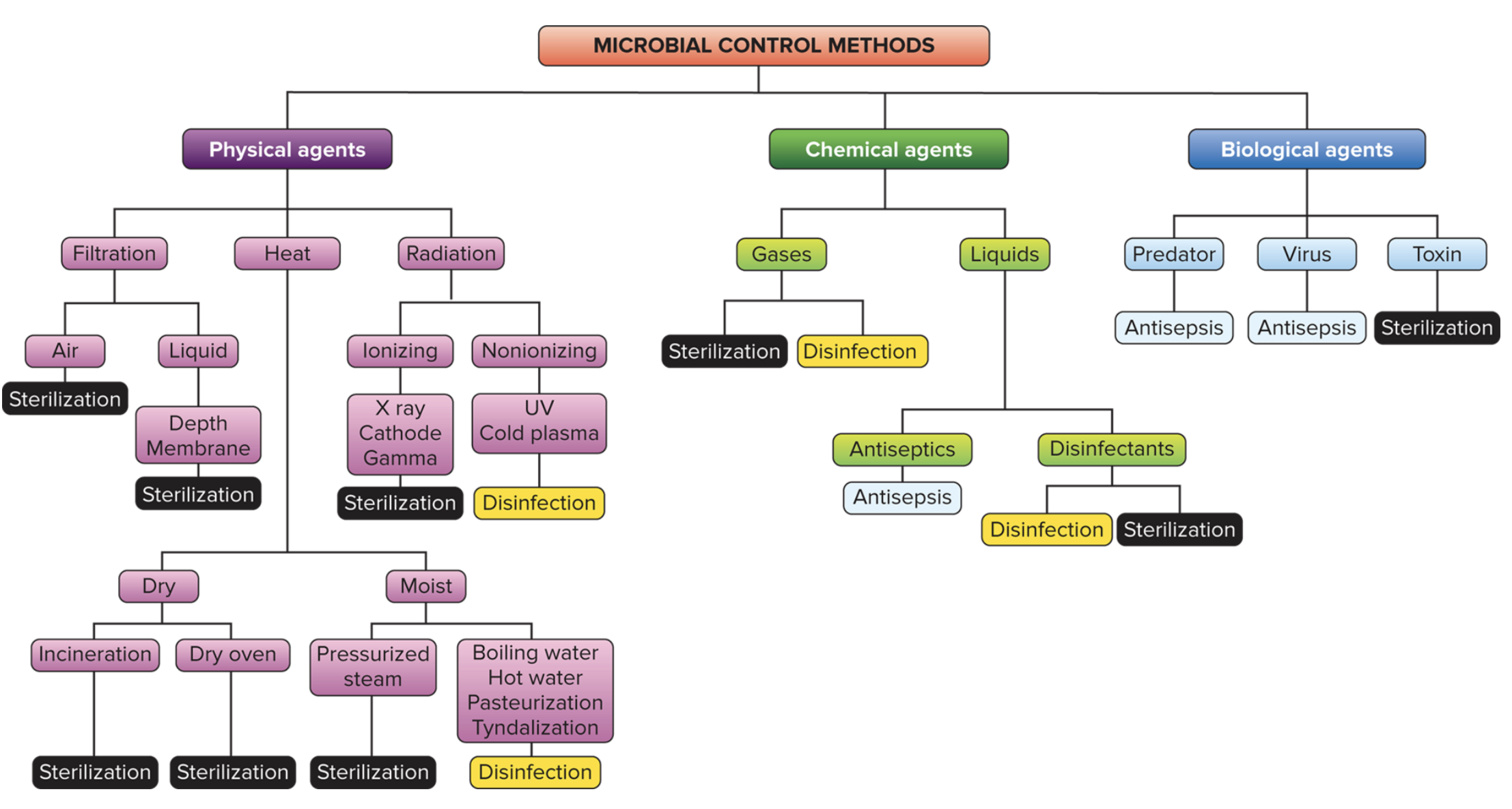
Sterilization
Everything (even non-pathogens) is completely destroyed/removed
Sterilant
Agent that helps w/ sterilization
Ex: chemical agents, like ethylene oxide (C2H4O) can be used to sterilize medical devices
Disinfection
Killing/inhibiting/removing microorganisms that may cause disease on INANIMATE objects
Usually done via chemical agents
Sanitization
Cleaning/disinfecting inanimate objects deemed safe by public health standards
Example: restaurant utensils
Antisepsis
Controlling microbes on living tissue through chemical agents
Antiseptics kill/inhibit pathogen growth
Less toxic than disinfectants
-cide vs -static
-cide = to kill
biocide: an agent that can kill living (can control microorganisms)
Germicide
Bactericide
Fungicide
Viricide
-static: inhibit growth but does not kill
if removed/diluted → effect is gone
bacteriostatic
fungistatic
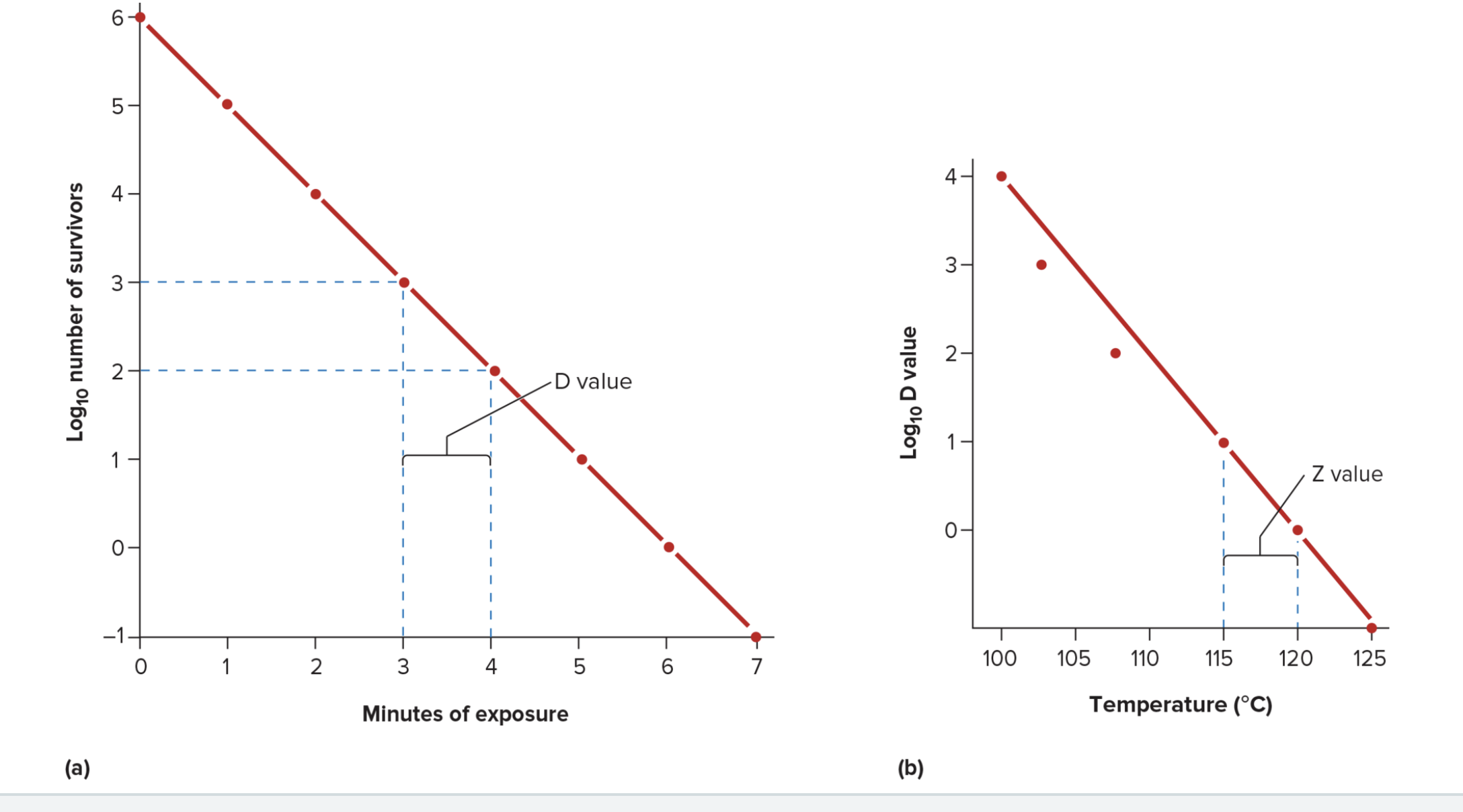
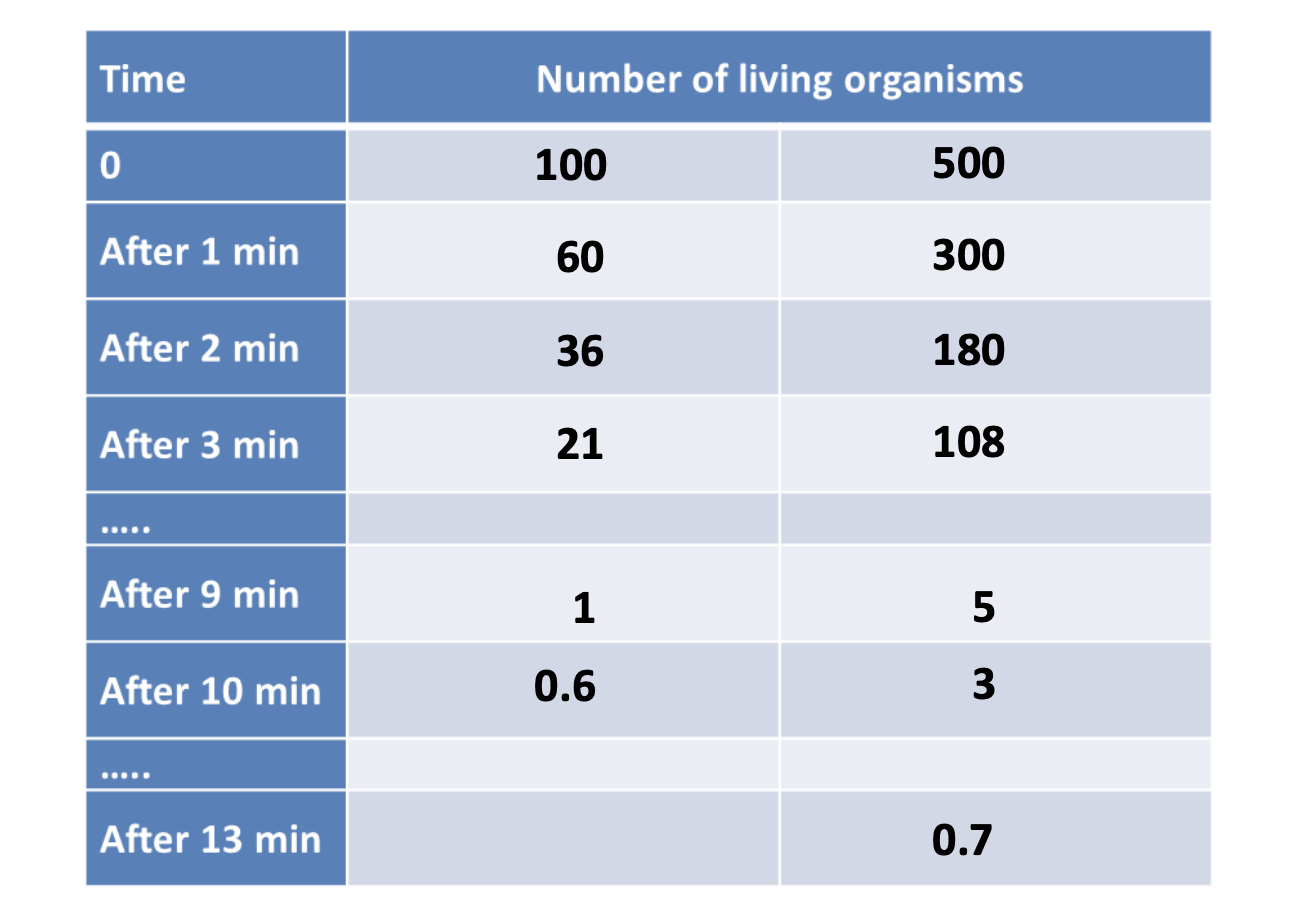
Exponential microbial death
Population decreases by the same fraction at constant intervals
ex: at a particular temp
10% of organisms die in 1st min
10% of living organisms die in 2nd min
10% of living after 2nd wmin will die in 3rd mijn
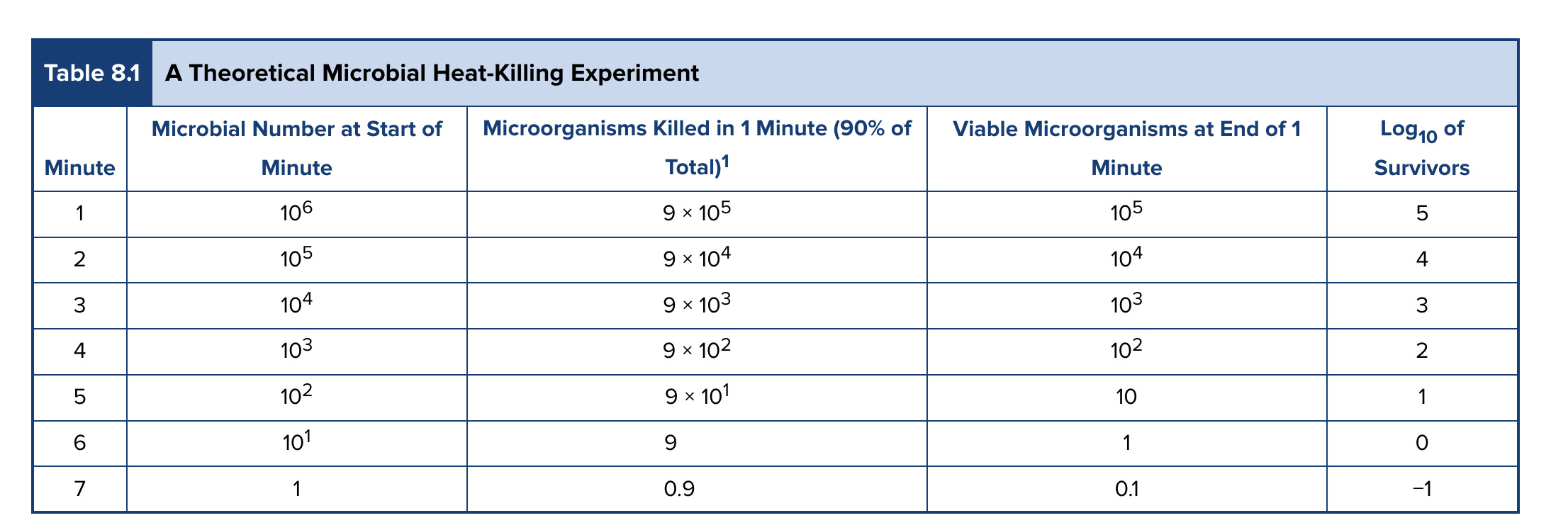
Decimal reduction time (D value)
Time to kill 90% of microorganisms in a sample at a specific time
Types of physical agents for controlling microbes
Filtration
Air
Liquid
Heat
Moist
Dry
Radiation
UV
ionizing
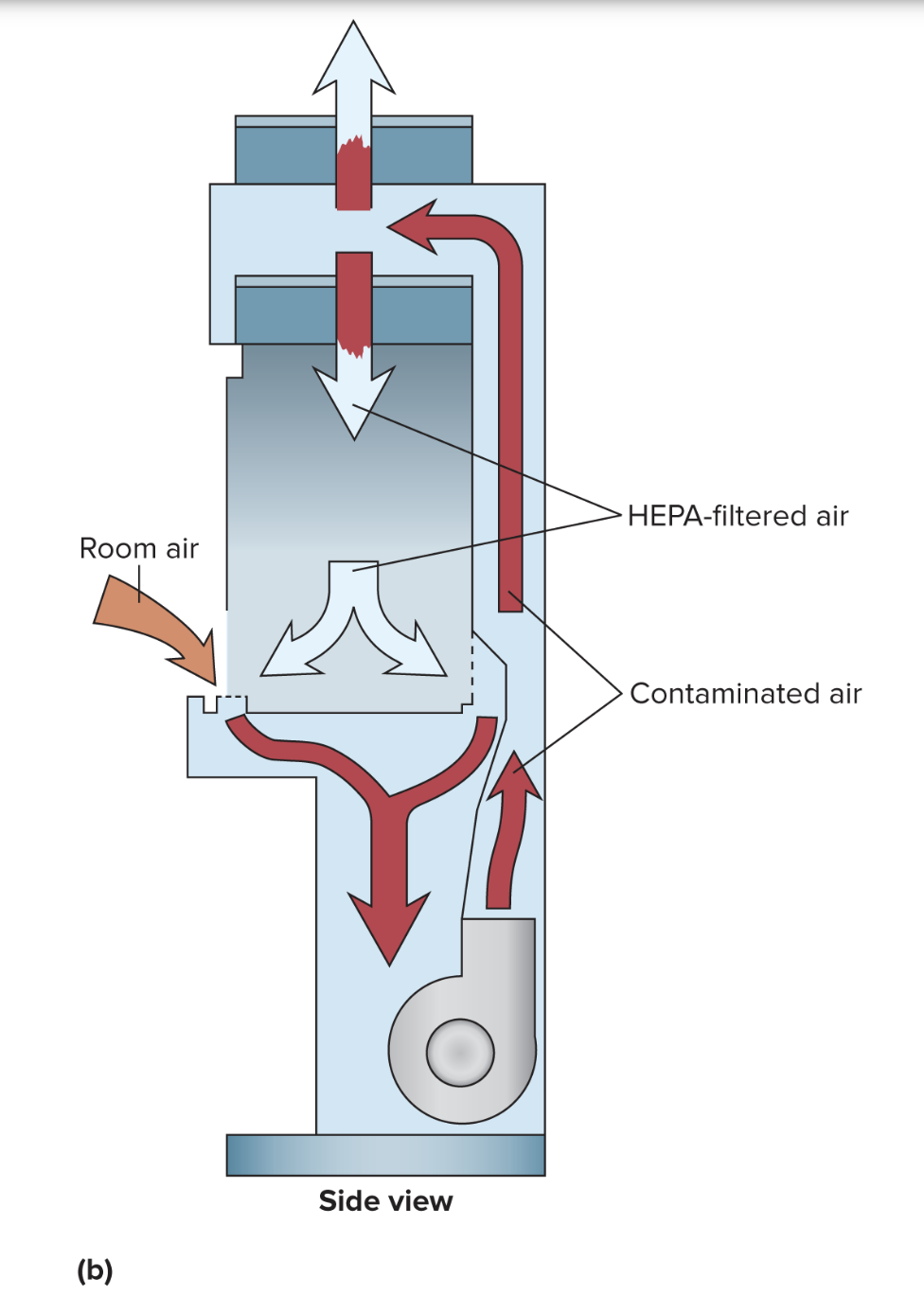
Air filtration
Type of physical agent to control microorganisms
Examples
HEPA filters
high-efficiency particle air
fiberglass
removes 99.97 % of particles ≥ 0.3 µm
also captures nanoparticles (≤0.1 µm, like viruses)
N95
excludes 95% of particles ≥ 0.3 µm
Hospitals/labs
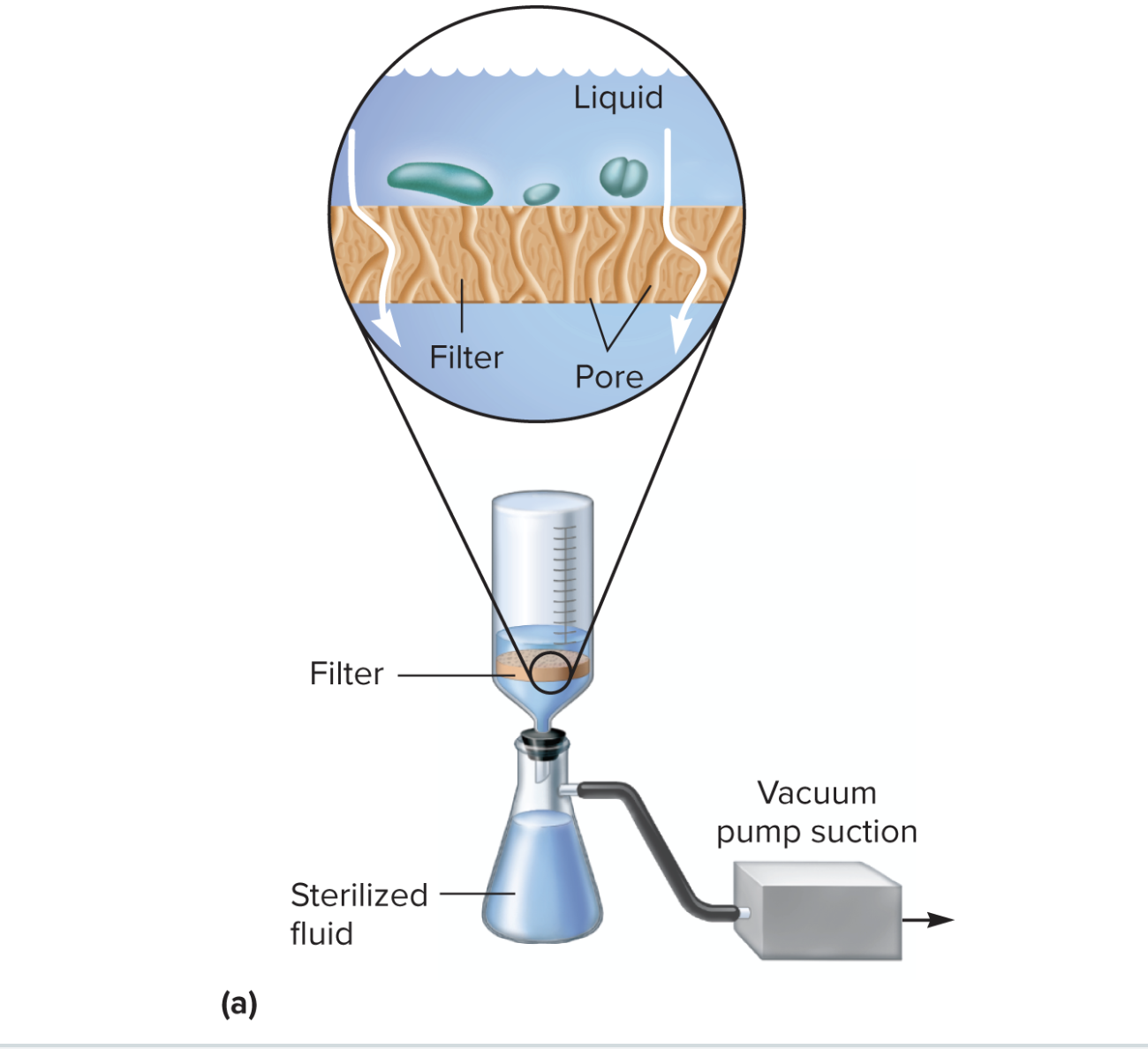
Liquid filtration
Type of physical agent to control microorganisms
Depth filter
Fibrous or granular material
Thick layers with lots of twisting channels of small diameter
Solution is sucked through & microbial cells ar trapped
Membrane filters
Synthetic materials
Varity pore sizes
~0.2µm in diameter
Removes most vegetative cells
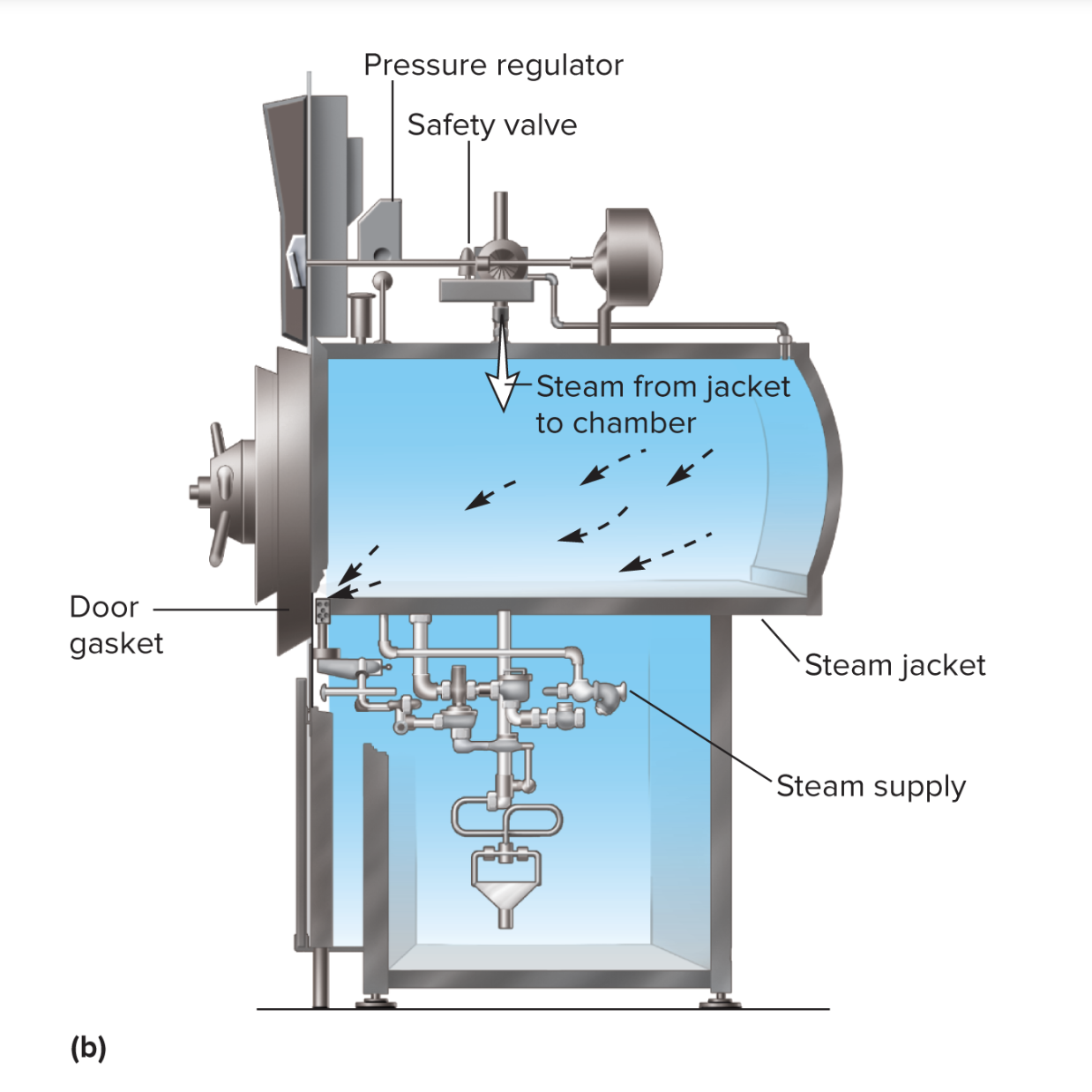
Moist heat as a physical agent for removing microbes
Autoclaves
Water boiled → Steam
Enters chamber & put under pressurew
121 degrees C & 15 lbs of pressure
Pasteurization
Controlled heating at temps well below boiling
Does not sterilize
Kills most pathogens, reducing spoilage
Dry heat as a physical agent for removing microbes
Less effective than moist
Does not corrode metal instruments
Sterilizes powders & oils
Bench top incinerators to sterilize innoculating loops
UV Radiation to control microbial growth
Non-iodizing
260-280 nm
Causes pyrimidine dimer, which is lethal
Pyrimidine = C & T
Limiting factor: Can’t penetrate well
Used in rooms in cabinets to sterilize air or exposed surfaces
Ionizing raditaion to control microbial growth — How many types?
3 types
Gamma rays
Electron beams
X rays
Penetrates deep
Damages DNA & produces peroxide
Destroys bacterial endospores & vegetative cells
Uses for ionizing radiation
Medical: antibiotics, hormones, syringes
Foods
Goal of chemical agents? What are some examples of chemical agents?
Be efffective against a wide range of microbes w/o being toxic to humans or corrosive to common material
Examples
Phenol
Soaps & detergent
Alcohol
Oxidizing agents
Joseph Lister
Sprayed phenol (a type of carbolic acid) into wounds, incisions, etc) & noticed it prevented infections
Led to antisepsis in healthcare setting
Phenol & phenolic derivatives
Denature proteins and disrupts plasma membrane
Advantages:
effective in presence of organic material
remains active on surface for a long time after application
Disadvantages:
Bad odor & causes skin irritation
Example of phenol-derivative
Triclosan
Phenol-derived antiseptic
Binds to enoyl-ACP reductase (bacterial enzyme)
Inhibits fatty acid synthesis (important for cell membrane synthesis)
Soaps & detergents
Surfactants (amphipathic)
allows them to break down and lift away dirt, oil, and bacteria from surfaces or skin
Removes microbes, oil
Action of removing microbes increases w/ scrubbing
Alcohols—what does it cause? What can it inactivate/kill?
Disinfectants (inanimate) & antiseptics (living tissue)
Bactericidal
Inactivates viruses
Dissolves/disrupts PM
Ex: ethanol/isopropanol (hand sanitizer)
Oxidizing agents
Strip electrons from molecules
Examples
H2O2 (3% solution) can be used on skin wounds)
Tincture of iodine
Sodium hypochlorite (found in household bleach, swimming pools)
Wastewater treatment (Chlorine/ozone)
What factors affect the effectiveness of antimicrobial agents
Population size
Cell type
High concentrations of antimicrobial agent
Longer duration of exposure
How does population size affect the effectiveness of antimicrobial agents
Fewer organisms = less time needed to achieve sterility
Table shows example of 40% death rate/min
How does cell type affect the effectiveness of antimicrobial agents
Vegetative cells are actively growing and more susceptible to agents
Younger cells are more susceptible than mature
Cells w/ endospores are more resistant
How does concentration of agent & duration of exposure affect the effectiveness of antimicrobial agents
Increased concentration destroys organisms faster (up to a point)
Longer duration of exposure leads to more killed
Phenolic component
Disinfectant screening test to see the effectiveness of a disinfectant
Potency of a disinfectant is compared to phenol
Series of identical dilutions to phenol & experimental disinfectant conducted
Methods of phenolic component test
20ºC water bath for 5 mins so all tubes come to same temp
Inoculated w/ 0.5 ml of test bacteria (Salmonella typhi & staphyloccus aureus
Test after 5, 10, 15 mins of innoculation
Transfer into broth & incubate for 48 hours
Find smallest concentration (highest dilution) that kills all organism after 10 mins
This dilution is used to calculate phenol coefficient
How to calculate phenol coefficient
Reciprocal of test disinfectant dilution divided by reciprocal for phenol
ex:
test infectant dilution = 1/250
phenol dilution = 1/250
250/250=1
test disinfectant has same effectiveness as phenol
test disinfectant dilution = 1/450
phenol dilution = 1/90
phenol coefficient: 450/90=5
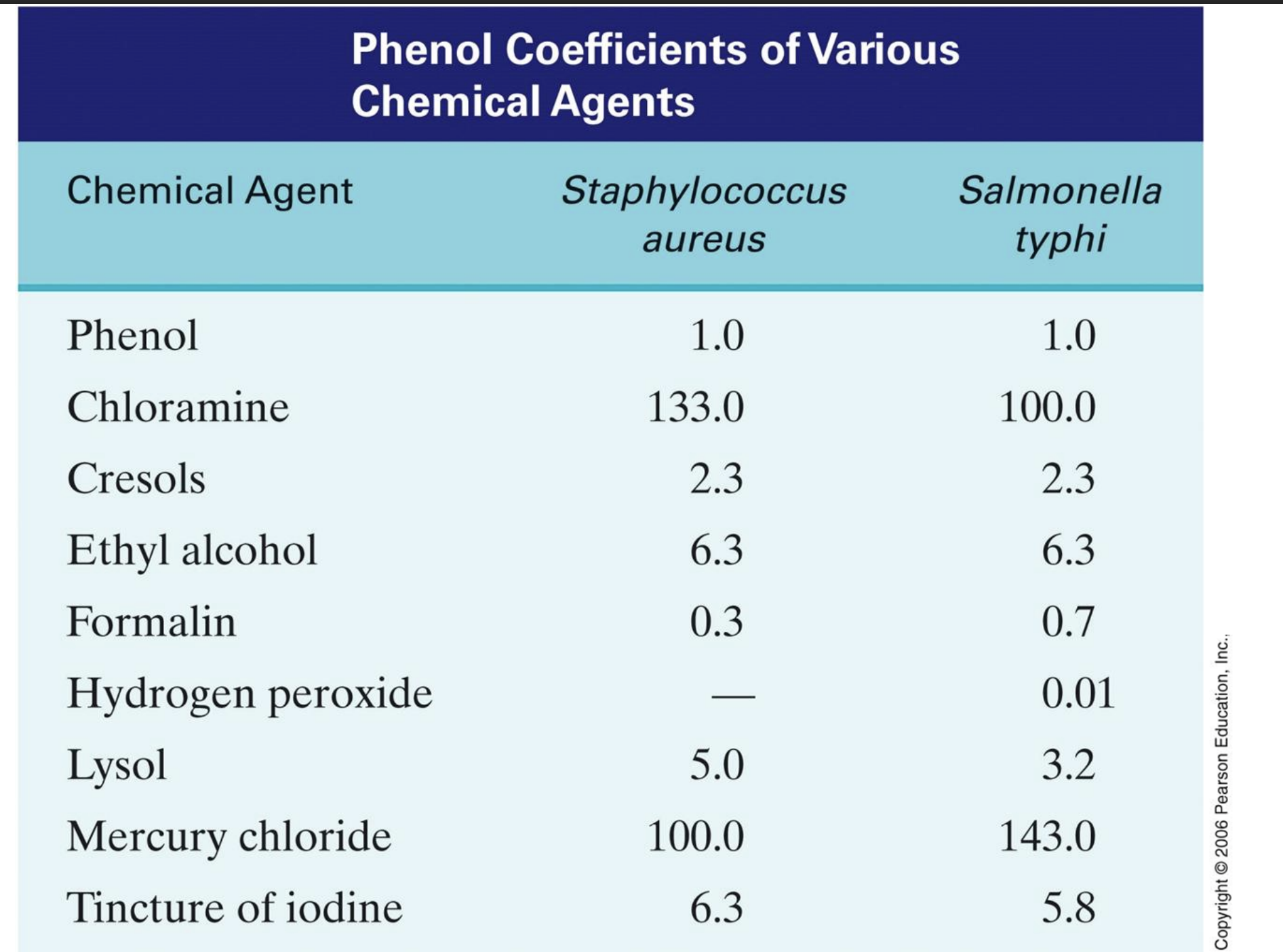
T/F: higher phenol coefficient means a more effective disinfectant under those conditions
True