Viral infections
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
What are the properties of viruses?
Small infectious agents that contain DNA or RNA and exist in a variety of shapes. Each has a central nucelci acid core surrounded by a protein coat, some enclosed within a lipid envelope derived from host cell or nuclear membranes
What does it mean for a virus to be known as an obligate intracellular parasite?
Metabolically inactive outside of hosts - rely on a host cell machinery to synthesise viral proteins and nucleic acids
What does the decision to treat viral infections depend on?
Balances severity of the infection against toxicity and availability of treatment
How do antiviral drugs work?
Interfere with viral replication - can be difficult to treat without harming host cells
What are most viral infections best controlled by?
Vaccinations
What are influenza viruses?
Enveloped orthomyxoviruses with a negative-sense, single-stranded RNA genome divided into 8 segments with allows generation of new strains
What key surface glycoproteins are present in influenza?
Haemagglutinin (HA) and neuraminidase (NA) - key in viral infectivity but also for our prevention and treatment.
How does HA and NA help the influenza virus enter cells?
HA binds to sialic acid receptors on host respiratory epithelial cells - NA facilitates release of new virions and aid in viral spread
How many types of influenza are there?
4 - A, B, C, D.
Why do annual influenza epidemics occur?
Antigenic drift - slow buildup in HA and NA mutations and also caused by genetic reassortment
What are the symptoms of influenza?
Sudden onset of fever, myalgia, headache, cough, sore throat with nasal discharge, arthralgia, significant malaise. Can also have GI upset e.g., diarrhoea and vomiting in children
What are some symptoms in children for influenza?
Irritability, febrile seizures, tachypnoea, croup, bronchiolitis or bronchitis
What can potential complications of influenza be?
Viral pneumonia, secondary bacterial pneumonia, exacerbations of chronic illnesses
Who is more susceptible to complications from influenza?
Older adults, pregnant women, immunocompromised patients and those with chronic medical conditions
What ocular symptoms may be present for influenza?
Photophobia, conjunctivitis, lacrimation and pain upon eye movement
What is complicated influenza indicated by?
Hypoxaemia, dyspneoa, radiological signs of lower respiratory tract infection, central nervous system involvement, or significant worsening of underlying chronic conditions
What is a recognised bacterial complication of flu in older adults and those with cardiorespiratory disease?
Bacterial pneumonia
What does the severity of flu depend on?
Host’s pre-existing immunity and virulence of circulating viral strain
What should treatment of flu be about?
Treating symptoms e.g., antipyretics, rest and fluids
What is coryza?
Acute inflammation of mucous membranes of the nose
What is a febrile seizure?
Convulsion in a child, typically between 6 months and 5 years old, triggered by a fever
What is lacrimation?
Flow of tears
What is tachypnoea?
Abnormally rapid, shallow breathing defined as more than 20 breaths per minute for an adult
What can be used to shorten duration of symptoms in flu?
Neuraminidase inhibitors zanamivir (Relenza) and oseltamivir (Tamiflu)
How do neuraminidase inhibitors work?
Interfere with virus particle release from the host cell and prevents infection of new host cells and spread of respiratory disease - must be used as early as possible
What is the first-line intervention for flu?
Vaccination! All eligible people should receive this
Why are flu vaccines given annually?
Viral mutation and short duration of protection
What groups are offered the annual flu vaccine based on age/comorbidiites?
6 months + clinical risk group, over 65s, children age 2-17 not in risk groups, front-line health and social care workers
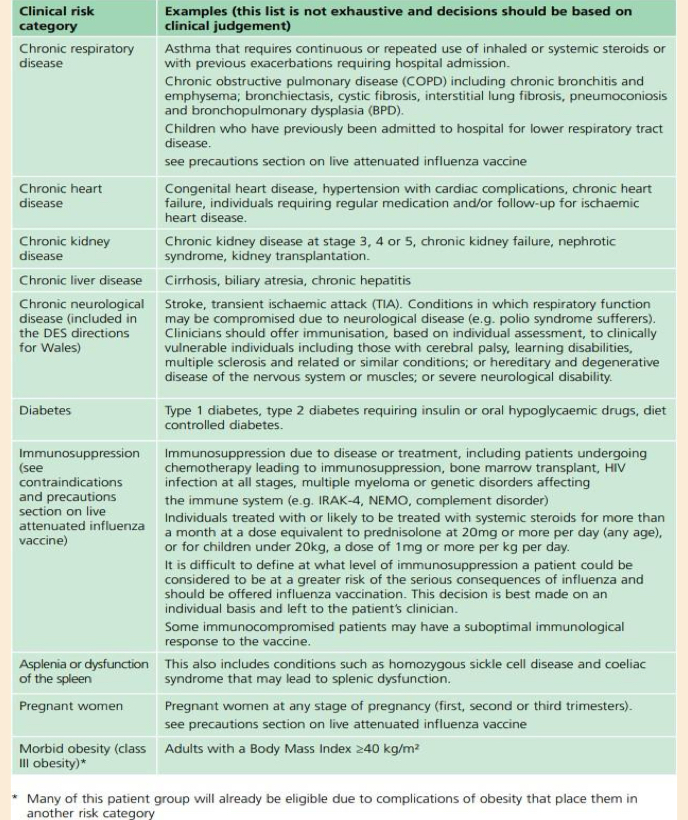
What clinical risk groups are offered a free flu jab?
Those with chronic respiratory disease e.g., COPD, chronic heart disease e.g., congenital heart disease/heart failure or ischaemic heart disease, CKD stage 3-5/chronic kidney failure, chronic liver disease e.g., cirrhosis, chronic neurological disease, diabetes, immunosuppression, pregnant women, morbid obesity
What property do most flu vaccines have?
InactIvated quadrivalent so cannot cause influenza
What live vaccine is given in flu and who to?
LAIV - given to healthy children, usually as a nasal spray
How is measles prevented?
Vaccine - MMR vaccine
How is measles transmitted?
Respiraotry droplets or aerosol route
What is the period of infectivity for measles?
4 days before until 2 days after onset of the rash - incubation period of 9-12 days
What are the symptoms of measles in the prodrome phase?
A severe cold, Koplik’s spots, fever, cough, coryza, conjunctivitis
What are Koplik’s spots?
Small, blush white papules with a red base, can be found as white/blue papules on gums
What is the rash of measles?
Blotchy, red rash - maculopopular rash
What is a maculopapular rash?
Flat, discoloured spots and raised, small bumps as the papules
What are the symptoms following a prodrome in measles?
Maculopapular rash that starts on the face/hairline before spreading to the trunk and limbs, lasting around 5-7 days, followed by mild skin discolouration, general malaise, fatigue and irritability
What are some complications from measles?
Otitis media, pneumonia - severe include encephalitis, rarely myocarditis or pericarditis
What are some indicators of complications of measles?
Persistent high fever, tachypnoea, dyspnoea, neurological signs e.g., seizures, prolonged or biphasic course
What is the main treatment of measles?
No antivirals so management is supportive care, preventing complications and public health measures E.g., isolating for at least 4 days after rash appears
What are some examples of supportive care for measles treatment?
Ensuing adequate hydration, good nutrition, using paracetamol/ibuprofen to manage fever and discomfort
What monitoring is necessary in measles treatment?
Bacterial pneumonia, otitis media signs as they should be treated with antibiotics or hospital referral necessary if severe signs of illness e.g., hypoxaemia, neurological involvement or CVS issues
What are some high-risk groups for measles?
infants, pregnant women, immunocompromised ndividuals
What should be considered for post-exposure prophylaxis in measles?
Offered to susceptible close contacts - vaccination within 72 ours of exposure is preferred but HNIG reserved unable to be vaccinated
What public health measures should be considered for measles?
Notifying the local health protection team, confirming the diagnosis through appropriate sampling, tracing and safeguarding vulnerable contacts and promoting catchup vaccinations to enhance population immunity
What is the herpes virus?
Family of enveloped DNA viruses that cause latent infections
What happens to the herpes virus after primary infection?
Viral DNA lies dormant in various tissues and can be reactivated
What are examples of herpes viruses?
Herpes simplex virus 1 and 2, varicella-zoster virus, cytomegalovirus, Epstein-Barr virus, human herpes viruses 6-8
What are the most common herpes viruses?
Herpes simplex - hSV-1 commonly presents as cold sores/oral herpes, HSV-2 is associated with genital herpes
What does VSV cause in childhood?
Chickenpox
What does VSV cause in adulthood when reactivated?
Shingles
What groups is CMV (cytomegalovirus) important in?
Pregnancy and immunocompromised patients
What is EBV the cause of?
Infectious mononucleosis
What is herpes simplex virus reactivation triggered by?
Fever, sunlight, intercurrent infections, local trauma, psychological stress, immunosuppression, menstrual cycle
Can HSV1 sometimes cause genital herpes and can HSV2 cause oral/pharyngeal disease?
Yes - distinctions between the two are not absolute
What is HSV1 the primary cause of?
herpetic gingivostomatitis, herpes labialis (cold sores), ketatoconjunctivitis and leading infectious cause of sporadic viral encephalitis
What are the usual symptoms of primary HSV1 infection?
Asymptomatic
What can the symptoms be in young children for primary HSV1 infection?
Fever, painful vesicular gingivostomatitis, cervical lymphadenopathy
What is painful vesicular gingivostomatitis?
Swollen, inflamed gums and fluid filled blisters/vesicles that may burst into painful ulcers around the mouth
What is cervical lymphadenopathy?
Swollen or enlarged lymph nodes in the neck
What symptoms can present in adults for primary HSV1 infection?
Pharyngitis or tonsilitis
How does HSV1 contact transmit?
Close contact e.g., saliva, viral shedding can occur in symptom absence
What can primary ocular infection of HSV1 lead to?
Severe keratoconjunctivitis, recurrent episodes can lead to corneal scarring
What are the 7 development stages of recurrent herpes labialis?
prodromal (1 day)
Erythema (1-2 days)
Papule (1-2 days)
Vesicle (1-2 days)
Ulcer (1-3 days)
Crust (4-14 days)
Skin re-epithelisation (4-14 days)
What symptoms can HSV2 infections cause?
Painful genital ulceration that can be severe with symptoms lasting 3+ weeks, recurrent infections are milder though and virus shedding
What is the treatment for HSV infections?
Topical, oral and IV antivirals - preparation depends on symptoms, usually aciclovir e.g., encephalitis treated with IV aciclovir
What is chickenpox?
Most common in children aged 4-10, highly infectious
When are people most infectious for chickenpox?
48 hours before the spots appear and 5-6 days after
How is chickenpox spread?
Respiratory droplets - vesicular fluid is also infectious
What are the initial symptoms of chickenpox before a rash appears?
Low grade fever, malaise and sometimes mild flu like symptoms
When does the rash appear for chickenpox?
6 days later - appears behind the ears, face or trunk and spreads further
What are the characteristics for the spots in chicken pox?
Spots are usually erythematous and maculopapular, then turn into vesicles before coming pustules that crust and heal over
How can VSV spread when vesicles rupture in chicken pox?
Direct contact with the fluid or indirect contact with infected clothes, towels or bedding
Why is ibuprofen not used in chickenpox?
Increases risk of skin infections including necrotising fasciitis
What is the usual treatment for chicken pox?
Symptomatic management usually all that is required for healthy children between 1 month-12 years + immunocompetent individuals
What can be used for fever/flu like symptoms in chicken pox?
Antipyretics
What can be used for itchiness in chickenpox?
Oral antihistamines and topical preparations e.g., crotamiton, calamine
What can be used for immunocompetent adults and children over 14 for chickenpox?
Aciclovir (5x a day for 7 days) if they present within 24 hours of rash onset - particularly in those with severe chickenpox or those at risk of complications e.g., smokers and corticosteroid users
What aciclovir treatment may immunocompromised individuals need?
IV therapy TDS 10mg/kg for 5 days
What happens if serious complications are suspected in chickenpox?
Complications e.g., pneumonia, dehydration, encephalitis = admit to hospital for parenteral antiviral treatment
What can virus reactivation of VSV to cause shingles be caused by?
Age, disease, physical or emotional stress, fatigue in immunocompromised
Can you get shingles if you haven’t had chickenpox?
No - but you can catch it from chicken pox
What are the symptoms for shingles?
Onset of a rash with severe nerve pain - tingling, itching or burning, usually unilateral and localised rash on abdomen, chest, face or neck
What do the lesions start as in shingles?
Erythmatous and maculopapular, develop into vesicles and crust over
How is shingles transmitted?
Direct contact - keep the affected area covered
What can be used for treatment of shingles?
Oral antivirals e.g., aciclovir, famciclovir or valaciclovir to prevent complication of post-herpetic neuralgia - should be started 72 hours of the onset of the rash and reduces complications
What can be a complication of shingles?
Post herpetic neuralgia
What is post herpetic neuralgia?
Steady burning, aching pain, jabbing pain or both that can continue for weeks or years
What are some treatments for post herpetic neuralgia?
Capsaicin cream, adjunctive neuropathic pain relief e.g., Amitriptyline low dose, gabapentin, sodium valproate