Stomach Disorders: PUD, Gastrinoma, Gastric Carcinoma, Gastroparesis
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
lower, duodenum, muscularis, age, H. pylori, NSAID, ETOH
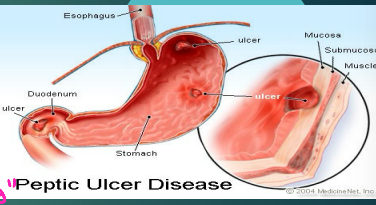
Peptic Ulcer Disease: Background
-Defects in _____ esophagus, stomach or _________, that extend through the ________ mucosa
-Epidemiology/Risk Factors
Incidence increases with ___
_.____ infection (MC)
Chronic _______ use (2nd MC)
Stress
Hypersecretion syndromes
____ use
Meds
Radiation therapy
smoking, NSAID, age, increased, mucosal, increase, gastrin
PUD: Etiology
-H. Pylori infection (95% duodenal, 70% gastric) → _______ increases risk in H. pylori patients
-______ use → prior hx of PUD, dose/duration of therapy, ___, co-therapy with drugs that enhance toxicity
-Alcohol → leads to _________ gastric acid production and _______ injury by breaking down mucosal barrier
-Emotional stress → ________ in ulcer incidence after traumatic events
-Gastrinoma → ______ secreting neuroendocrine tumors
secretion, protection, neutralize, alkaline, inhibits, peristalsis, secretin, pancreas
PUD: Pathophysiology
-Imbalance between the rate of gastric juice ___________ and degree of __________ by the mucosal barrier
-Ability of duodenal juices to _________ gastric acid → duodenal cells secrete _______ mucus and pancreatic juices are alkaline
-Feedback Mechanisms
Acid in duodenum → ______ gastric secretion and ___________ of stomach
Acid in duodenum → secretion of ______ → causes _________ to secrete alkaline juices
less, epigastric, eating, nausea
PUD: Gastric Ulcer
-____ common than duodenal ulcers, seen mostly in 55-65 y/o pts
-Symptoms
Intermittent ________ pain and dyspepsia in a “food-pain” pattern, meaning it is worse after ______
Early satiety
_______/vomiting
Occasional weight loss
20, pain, relieved, nocturnal
PUD: Duodenal Ulcers
-More common, seen in ages __-50
-Symptoms
Intermittent epigastric ____ and dyspepsia that is usually ________ by ingestion of food or antacids (“pain-food-relief” pattern)
________ pain, when acid secretion is maximal
perforation, hematemesis, stools, obstruction, pyloric, epigastric
PUD: Complications
-___________ → suspected if sudden development of severe, diffuse abdominal pain (peritonitis)
-Bleeding → ____________ (red blood or coffee ground emesis), melena (black, tarry ______)
-Gastric outlet __________ → typically with ulcers located in the _______ channel or duodenum. Associated with bloating, N/V, increased __________ pain
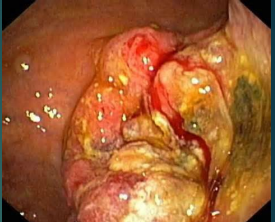
endoscopy, smooth, flat, exudate, lumen, nodular, irregular, malignancy
PUD: Diagnosis
-___________ is the gold standard
Definitively establishes diagnosis
Benign ulcers → ______, regular, rounded edges, with ____, smooth ulcer base filled with _______
Malignant ulcers → ulcerated mass protruding into the _____, folds surrounding ulcer crater are ________, clubbed, fused, or stop short of the ulcer margin, or overhanging, _________ or thickened ulcer margins
-Biopsies should be done on all gastric ulcers for possible ____________
sensitive, duodenal, H. pylori, NSAID, gastrinoma
PUD: Diagnosis, pt. 2
-Barium Swallow
Can identify PUD but less __________
If _______ ulcer discovered and no alarm symptoms, don’t have to have endoscopy but gastric ulcers do
-Other tests
Test for _.______
Ask about _______ use
If those are both negative, then consider other causes like __________

H. pylori, PPI, slower, duodenal, endoscopy
PUD: Treatment
-Lifestyle: eradication of _.______ if needed, withdrawal of offending agents
-Pharmacological: ___ drug of choice (omeprazole, pantoprazole), H2 blockers are an option but ______ to heal ulcers, and antacids/sucralfate can heal __________ ulcers but not routinely recommended
-Repeat __________ should be done on all gastric ulcers to document healing
duodenal, gastrectomy, perforated
PUD: Surgical Approaches
-_________ ulcers → vagotomy
-Gastric ulcers → partial __________, Billroth I or II reconstruction
-_________ ulcer → laparoscopy/open patching
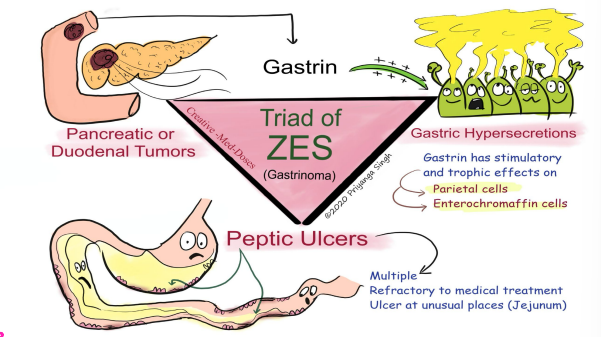
hypersecretion, gastrinoma, duodenal, MEN-1
Zollinger Ellison Syndrome (Gastrinoma): Background
-Gastric acid _____________ from a __________ resulting in severe acid related peptic disease and diarrhea
__________ is the most common or pancreatic neuroendocrine tumors
-Epidemiology
20-50 y/o
Men > women
1/3 associated with ___-_
PUD, loss, bleeding, steatorrhea
Zollinger Ellison Syndrome (Gastrinoma): Symptoms
-___ with multiple refractory ulcers
-Diarrhea, heartburn, and weight ____ are other common symptoms
The diarrhea is specifically __________, which is loose fatty stools
-Complications → ________, stricture, perforation
fasting, pH, 10, 2, secretin, persistent, US, head, duodenum
Zollinger Ellison Syndrome: Diagnosis
-Initial/Screening Tests: _________ serum gastrin concentration and gastric __ measurement
Gastrin levels > __x normal with gastric pH <_ is diagnostic
-Confirmatory: ________ stimulation test
If serum gastrin <10x normal and low gastric pH or differentiate gastrinoma from other processes
__________ gastrin elevation in gastrinoma
-Imaging: somatostatin-receptor scintigraphy, __, CT, MRI, endoscopy
Most found in ____ of pancreas or 1-2nd portion of _________
PPI, somatostatin, resection, liver, bone, chemo, MEN 1
Zollinger-Ellison Syndrome: Treatment
Local Disease
-High dose ___ is first line med
-Octreotide therapy (__________ analog)
-Exploratory laparotomy and _________ (ideal for local disease) → sporadic gastrinoma without metastatic spread
Metastatic Disease
-______ most common, next is ____
-Limited efficacy of treatment options → ____ or surgery
-Screen all pts with ZES for ___ _
adenocarcinoma, antrum, intestinal, differentiated, Asia, >
Gastric Carcinoma: Background
-_____________ most common
-Location
______
Body and fundus
Cardia
Entire organ
-Types
________-type (resembles intestinal cancers in forming glandular structures)
Diffuse-type (poorly ___________ and lacks glandular structures)
-Epidemiology
Highest incidence in East _____, East Europe, and South America
Men _ women
> 40yo
gastritis, salt, smoking
Gastric Carcinoma: Risk Factors
-Chronic _________ (H.pylori infection most common)
-Atrophic gastritis (autoimmune disorder)
-High ____ diet (leads to chronic gastritis)
-Nitrous compounds (preserved foods, tobacco smoke)
-Obesity
-__________, ETOH
-Gastric surgery
loss, anemia, supraclavicular, palpable
Gastric Carcinoma: Symptoms
-Weight ____ (anorexia, nausea, early satiety)
-Abdominal pain (epigastric, vague)
-GI bleed (iron deficiency ______)
Signs of Metastatic Dz
-Left _____________ adenopathy
-Periumbilical nodule
-__________ liver or abdominal mass
endoscopy, biopsy, metastatic, LAD
Gastric Carcinoma: Diagnosis
-___________ → most sensitive and specific for diagnosis
______ needed for confirmation
EUS to determine the local extent of primary tumor
-Chest/Abdominopelvic CT
Performed early after dx is made
Evaluate for _________ disease
-PET Scan → can confirm malignant involvement if CT detected ___
-Laparoscopy → advantage of directly visualizing abdomen
resection, I-III, mucosal, total, chemotherapy, palliative
Gastric Carcinoma: Treatment
-Curative Surgical _________ (mainstay)
Stage _-___
Endoscopic _______ resection for small, early gastric cancer
Radical surgical resection → _____ or subtotal gastrectomy
-Perioperative ___________ or adjuvant chemoradiation
Associated with improved survival in pts with localized or locoregional cancer who undergo surgical resection
-________ Modalities
Metastases or local invasion of other organs
Surgery and chemo considered not curative
Dumping, immediate, diarrhea, hyperglycemic, surgical, B12
Gastric Carcinoma: Postgastrectomy Considerations
-________ Syndrome → symptoms after a meal due to rapid gastric emptying
Early → _________ symptoms after meal; tachycardia, diaphoresis, abdominal cramping, and __________
Late → symptoms hours after a meal; can become very ____________ → need insulin bolus → hypoglycemia
-Bile reflux → often needs ________ correction
-Vitamin ___ Deficiency → any pt with total gastrectomy or gastric bypass needs supplementation
emptying, absence, autonomic, enteric
Gastroparesis: Background
-Delayed gastric ___________ in the ________ of mechanical gastric outlet obstruction
-Pathophysiology → abnormalities of the _________ nervous system, smooth muscle cells, _______ neurons and GI hormones
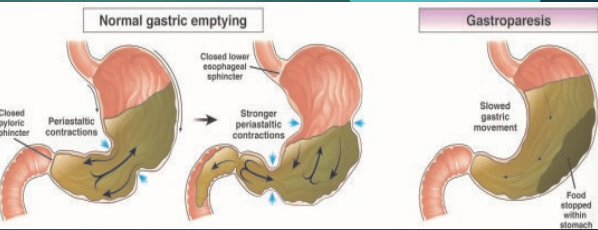
Diabetes, >, autonomic, vagus, narcotics, vagus
Gastroparesis: Etiology
-Idiopathic
-_________ mellitus
Type 1 _ Type 2
Due to __________ dysfunction and/or abdominal intrinsic nervous system, leading to neuropathy involving the _____ nerve and loss of interstitial cells of Cajal
-Iatrogenic → induced by several meds, like _________
-Postsurgical → d/t injury of ____ nerve, fundoplication one of most common
nausea, pain, satiety
Gastroparesis: Symptoms
-___________
-Vomiting
-Abdominal ____
-Early ______
-Postprandial fullness/bloating/weight loss
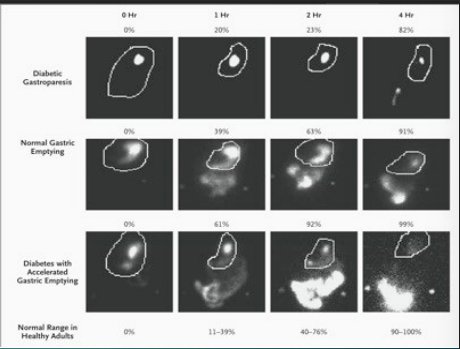
obstruction, endoscopy, motility, imaging, retention, 10, 60
Gastroparesis: Diagnosis
-Exclude mechanical obstruction
Upper __________
CT or MRI enterography → if unavailable, then barium follow through
-Assess gastric ________
Gastric scintigraphy → ingestion of meal followed by ________ immediately after then at 1, 2, and 4 hours
Delayed emptying defined as gastric _________ > __% at 4 hours and/or __% at 2 hours
glucose, myopathic, neuropathy
Gastroparesis: Establish Etiology
-Known underlying disease → no further investigation
-No known underlying disease → consider labs, manometry, and/or autonomic testing
-Laboratory studies → Hgb, fasting ______, total serum protein, TSH, ANA
-Gastroduodenal manometry → __________ vs neuropathic process
-Autonomic testing → preganglionic or central lesion vs peripheral ___________
dietary, fiber, dehydration, Metoclopramide
Gastroparesis: Management
-First Line (Mild) → ________ Modification
Small, frequent meals
Low fat; contain only soluble _____
No carbonated or ETOH beverages
-Hydration and Nutrition
Vomiting and decreased intake can cause hypokalemia, metabolic alkalosis, and __________
Vitamin deficiencies
-Glycemic control
-Pharmacologic therapy
DOC is _____________
Can consider erythromycin IV or antiemetics
venting, decompress, enteral
Gastroparesis: Refractory Symptom Treatment
-Percutaneous endoscopic gastrostomy ______ tube → _________ upper GI tract
-Percutaneous endoscopic jejunostomy tube → ______ nutrition, pts with unintentional weight loss of > 10% of normal body weight
-Surgery → rarely indicated