2. Viral Diseases (Epizoo exam)
1/48
Earn XP
Description and Tags
viruses - for part 2 in epizoo exam. Husk: IP = time bw. infection + appearance of CS, if animals is infected today - shows signs 5 days later -> IP = 5 days.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
1.Paramyxoviral infectious diseases (Newcastle disease and other avian)
Paramyxoviral viruses cause many important diseases in humans and animals, contagious.
family: Paramyxoviridae, split into subfamilies paramyxovirinae:
Respirovirus → bovine parainfluenza 3, sendai virus
Rubulavirus → newcastle virus (genus avulavirus), Canine parainfluenza virus 2
Morbillivirus → rinderpest, canine distemper virus
and Pneumovirinae:
Metapneumovirus → turkey rhinotracheitis virus
Newcastle disease:
caused by: Avian paramyxovirus type 1 (APMV-1)
species: Chickens. Can infect humans but rare (zoonotic)
Transmission: Inhalation, ingestion, shed virus in feces/resp. secretions. Spread rapidly among birds in confinement.
virus types:
Lentogenic (low) - strains worldwide,
Mesogenic (moderate),
Velogenic (high) - asia, africa, america
Neurotropic → resp. + NS
Viscerotropic → intestinal hemorrhages
CS:
lentogenic/Mesogenic: mild/subclinical, coughing, sneezing, rales, drop in egg production, low mortality
Velogenic: severe, high mortality, depression, anorexia, ruffled feathers, red swollen eyes, head and neck swelling, resp. distress, Nasal discharge, green/watery diarrhea
NS signs: tremors, paralysis, torticollis/twisted neck, circling
PM lesions: Swollen head/Periorbital area, hemorrhages in trachea + pharynx, diphtheric membranes in throat/trachea, hemorhage/ulcers in cecal tonsils and intestines, enlarged & dark spleen, pulmonary edema, ovarian degeneration
Diagnosis: virus isolation from oronasal swabs (dead birds), tracheal/cloacal swabs (live birds), serology (ELISA), molecular: RT-PCR
Treatment/prevention: No treatment, prevention by all-in-all-out system, vaccine, quarantine/reporting, legal import only, disinfection
Turkey Rhinotracheitis (TRT)
In young turkeys, chickens can also be affected - swollen head syndrome
CS: sneezing, frothy nasal discharge, conjunctivitis, swollen infraorbital sinuses, submandibular edema, decr. in egg production, 100% morbidity, mortality is higher in young birds.
2.Paramyxoviral infections ( Rinderpest, PPR, PI, BSV)
part 1: general, genus, transmission, diagnosis - Rinderpest is?
General:
All are spread by aerosols + close contact (respiratory viruses) + fomites (Pi)
They all start with fever, depression/anorexia, nasal and ocular discharge → differ in the main damage.
Resp. → BRSV, PI-3, CPiV-2
Mouth + gut → rinderpest, PPR
Diagnosis: RT-PCR for viral RNA + virus isolation/ID (difficult)
Treatment: Mostly supportive care, ATB only for sec. bacterial infections, Prevention mainly by Vaccination and biosecurity (quarantine, good hygiene).
Rinderpest Virus (“cattle plague”) - ruins the mouth and gut
Species: Large Ru (cattle, buffalo, Yak)
high morbidity, high mortality, NOT zoonotic.
IP: up to 14 days, 4-5 days is typical
CS (hemorrhagic disease):
necrotic mouth lesions (gums, tongue, cheeks),
dry and cracked muzzle,
severe stomatitis-enteritis syndrome
PM: dehydrated, emaciated carcass, severe diarrhea, erosive lesions throughout GIT
Eradicated worldwide in 2011, controlled by vaccination.
Rinderpest - can look like FMD, IBR
2.Paramyxoviral infections ( Rinderpest, PPR, PI, BSV)
part 2 - PPR is?
Peste Des Petis Ruminants (PPR)
Caused by: PPR virus, genus Morbillivirus
Species: Sheep & goats, high morbidity & mortality (worse in goat), OIE-listed, Not zoonotic.
Epizoo: Sub-saharan africa, middle east, Asia
IP: 4-6d (up to 10)
CS: necrotic stomatitis & gingivitis, diarrhea, pneumonia, coughing
PM: necrotic & inflammatory lesions in oral cavity & GIT
PPR and Rinderpest clinically look very similar, needs lab tests to differentiate. Bluetongue, FMD.

2.Paramyxoviral infections ( Rinderpest, PPR, PI, BSV)
part 3 - PI is?
PI → Parainfluenza viruses, Respiratory paramyxoviruses
Bovine Parainfluenza virus-3 (BPiV-3 in cattle) - part of BRD complex. “mild resp. virus → starter for bact. pneumonia in calves”
short course, 3-4 days. usually mild. Immunity is short lived → reinfection is possible.
CS: Cough, dyspnea, lacrimation.
Complication: secondary bacterial pneumonia (Pasteurella Haemolytica) → purulent discharge, severe illness, general malaise
May look like IBR, coronavirus
Canine Parainfluenza virus-2 (CPiV-2 in dogs) - part of kennel cough complex.
Mild or inapparent, 3-14 days.
CS: Cough, conjunctivitis, tonsillitis, sudden serous nasal secretion.
Other agents can mimic Kennel cough, like canine distemper.

2.Paramyxoviral infections ( Rinderpest, PPR, PI, BSV)
part 4: BSV is?
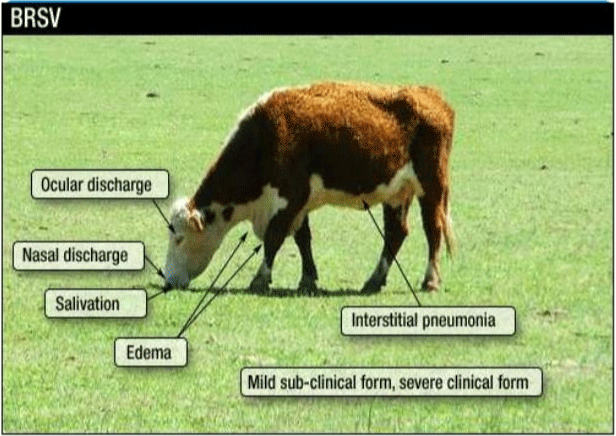
Bovine Respiratory Syncytial virus (BRSV)
family Pneumoviridae, genus Pneumovirus
Species: Mostly cattle, esp. young calves, can also infect sheep/goat
CS: Resp. illness ranging from mild → severe pneumonia. Fever, rapid & open-mouth breathing, dry cough, frothy saliva, decr. milk production
BRSV - can look like IBR, Bovine PI-3
3.Paramyxoviral infection (Canine distemper, NIPAH, and others)
Canine distemper
caused by: Canine distemper virus, genus Morbillivirus
Species: all species of canidae, procyonidae (raccoons), mustelidae (ferrets), felidae (cats)
Transmission: Aerosols, droplets, contact with urine, saliva, blood and feces, contaminated environment, humans & insects can mechanically spread it.
Worldwide
CS: IP is 3-6 days
starts like a cold → becomes systemic → then neurological
general: fever, nasal + ocular discharge, anorexia/lethargy
GI and resp. signs, skin pustules, hard pad disease (hardening of of footpads - hyperkeratosis), enamel hypoplasia (if teeth is still forming)
Neurological signs: muscle twitching + rhythmic jaw movements (chews gum continuosly), seizures, circling, head tilt, nystagmus, paralysis
Diagnosis: RT-PCR-viral RNA, Virus isolation, immunofluorescence
Treatment: no cure → supportive only: fluids, nutrition, antipyretics, analgesics, anticonvulsants + nursing care
Prevention: vaccination (MLV or recombinant vaccines - canarypox vector)
NIPAH - Zoonotic
caused by: RNA virus, family paramyxoviridae, genus Heniparvirus
Species: pigs, horse, dogs, cats. Humans (Severe disease). Fruit bats = reservoir.
Transmission: contact with infected animals - infected bats. bat saliva, urine, feces contaminating food or water.
Epizoo: First outbreak in malaysia 1999, called PRES (porcine resp. & encephalitic syndrome), barking pig syndrome.
CS: in pigs: resp. signs (fever, severe cough, difficulty breathing), and sometimes nervous signs (encephalitis), high morbidity, low mortality (except in piglets), some pigs show no signs.
Humans: asymptomatic → resp. disease → fatal encephalitis.
Diagnosis: difficult to diagnose by CS, confirm by RT-PCR, virus isolation, and virus neutralization test
Treatment&prevention: No vaccine, No specific treatment. Control by biosecurity, keep animals away from fruit trees, reduce bat contact, report outbreaks
4.Parvoviral infectious diseases (Canine, feline, mink)
part 1: Focus on canine, feline
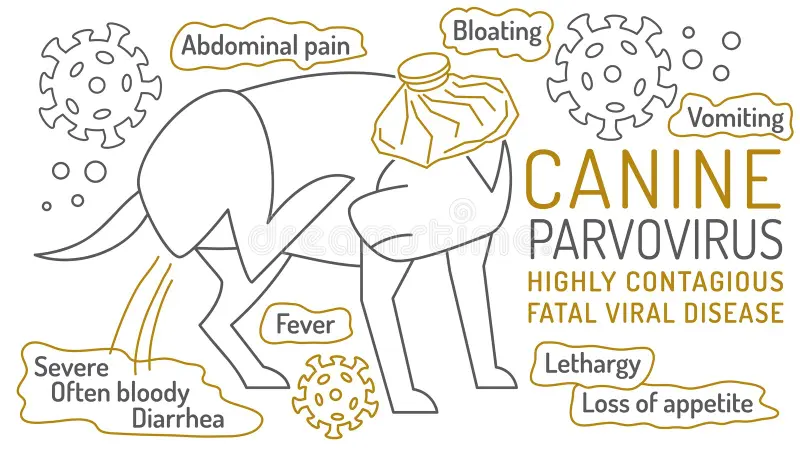
Canine Parvovirus infection (CPV)
Caused by: canine parvovirus type 2 (CVP-2a, 2b, 2c) - Infects rapidly dividing cells. Resistant.
Species: Puppies (esp. unvaccinated), breeds at risk: rottweilers, Dobermans.
Transmission: fecal-oral route, insects/rodents (vectors)
CS: 2 syndromes:
Hemorrhagic enteritis (most common) - malabsorption
Bloody Diarrhea + vomiting → severe dehydration
Loss of intestinal barrier → bacteria enter blood → septic shock
Fever, lethargy, abdominal pain, sudden death
Acute myocarditis (rare) - sudden death in very young puppies
Diff DX: canine distemper, salmonelliosis, hemorrhagic gastroenteritis, canine corona virus
Necropsy: Thymic atrophy, enlarged LN, hemorrhagic Peyer`s patches, pulmonary edema, hydrothorax, hydropericardium, dilation of cardiac chambers
Diagnosis: history & Symptoms, SNAP test, ELISA, PCR
Treatment: supportive care
IV fluids, ATB (prevent sepsis), anti-emetics, glucose support.
Prognosis worse if: intussusception, low protein, no improvement after 4 days
Prevention: Vaccination, colostrum intake, keep puppies indoors until fully vaccinated
Cats get - Feline parvovirus (Panleukopenia) → affects kittens under 1 year, esp. in shelters and multicat homes. Same disease process and canine parvo: vomit, diarrhea, dehydrated.
Feline parvovirus is part of the CORE vaccination for cats.
4.Parvoviral infectious diseases (Canine, feline, mink)
part 2: Focus on mink
Aleutian Disease of Mink
Caused by: Aleutian mink disease virus, Amdovirus
Species: mink with aleutian genotype - has it worst, ferrets infected but usually asymptomatic
Transmission: Feces, urine, saliva, milk. Transmitted by oral, nasal, bites, mosquitoes, often from asymptomatic carriers.
IP: months to years
CS:
Acute: Rare, sudden death
Chronic: behavior changes, poor appetite, decr. activity, weight loss, bloody diarrhea, dark urine, neurological signs (incoordination, convulsions), abortion, death
pathology: spleen, liver, LN, kidney - enlarged. Hemorrhage of MM.
diagnosis: ELISA, PM + Herd history, screening
Treatment & Prevention: No treatment, No vaccine. Control by quarantine, test & remove infected mink.
5.Parvoviral infectious diseases (swine, avian)
part 1: Focus on swine
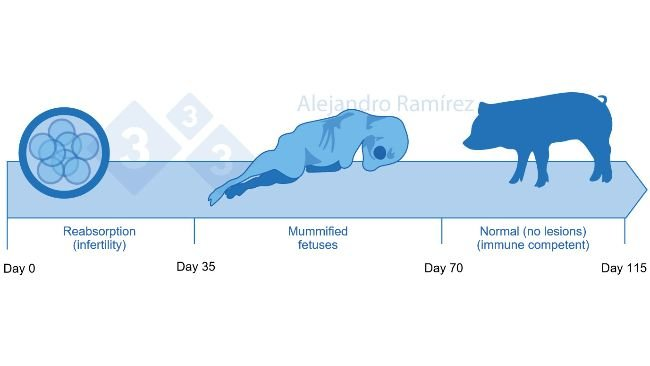
Porcine Parvovirus (PPV)
Species: Pigs = reservoir + source of infection. Enzootic in most herds (seen often in pig population), worldwide.
Transmission: Horizontal (fecal-oral, contaminated feed), vertical (transplacental), fetus is the most infectious source.
CS: Reproductive failure in pigs
clinical syndrome: SMEDI - stillbirth, mummification, embryonic death, infertility
Non-pregnant pigs usually show no signs (possible fever, leukopenia)
Clinical effects by pregnancy stage:
to 2 weeks: virus crosses placenta and kill piglets
to 30 days: embryo death → resorption
30 - 70 days: fetal death → mummification
56-70 days: fetus develops immunity → survives
Diagnosis: History + clinically (SMEDI), lab. Isolation and identification of virus, ELISA, cell culture.
Prevention: vaccination of gilts before breeding. good herd hygiene
5.Parvoviral infectious diseases (swine, avian)
part 2: focus on avian
Avian parvovirus (Chicken & Turkey)
Caused by: Parvovirus (family Parvoviridae)
Transmission: horizontal (fecal-oral route), vertical (from hen → egg)
CS: Malabsorption syndrome
Poult enteritis mortality syndrome (PEMS)
Diarrhea
Feather abnormalities
Inflammation of SI (catarrhal SI enteritis)
Diagnosis: poor flock performance, histopathology - inclusions in epi. cells, PM lesions, PCR - detects viral DNA
Treatment/Prevention: No vaccine, prevention by biosecurity, good hygiene, disinfection, good husbandry
6.Poxviral infectious diseases (Avian and leporid)
part 1: focus on avian
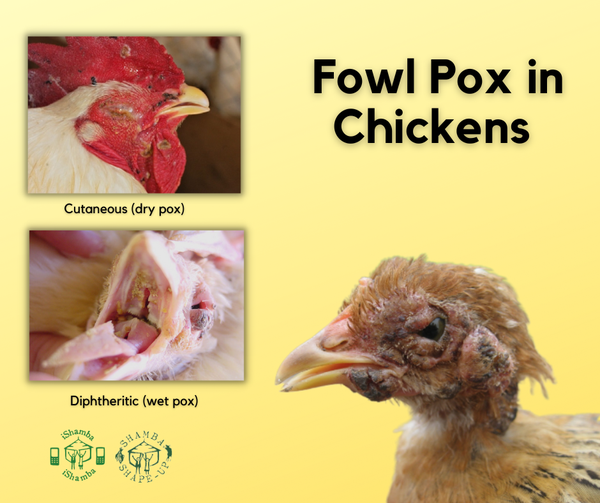
Fowl Pox
caused by Avipoxvirus in poultry
Transmission: Direct contact with skin lesions, aerosols, mosquitoes and biting insects (mechanical vectors), Slow spread in flocks
Clinical forms:
Dry (cutaneous) form: nodules/scabs on un-feathered areas like head, legs, wattle, comb, eyelids. Lesions around nose may cause nasal discharge or closure of eyelids.
Wet (diphtheritic) form: yellow-white cancers/lesions (cheesy exudate) on MM of mouth, pharynx, larynx, trachea. Can cause difficulty breathing and eating. May cause suffocation and death.
Birds may also show both forms at the same time
Diagnosis: By CS, PCR, and skin scrapings
Prevention: Vaccination
6.Poxviral infectious diseases (Avian and leporid)
part 2: focus on leporid
Myxomatosis - Rabbit Poxvirus
caused by Myxoma virus (Myxomatosis Cuniculorum)
Transmission: vector-borne (flea, mosquito) or direct contact
Origin in wild south american rabbits, introduced to Europe (france, 1952), spread widely.
CS: European rabbits → very severe disease, high mortality.
Skin nodules, swelling of eyes (big head disease) and genitals, severe immunosuppression
resp. form may occur without skin lesions
Diagnosis: Virus isolation, serology
Prevention: Vaccination, isolation of infected rabbits, mosquito and flea control

7.Poxviral infectious Diseases (Ruminants and others)
part 1: Name diseases, general
Poxviruses - largest known viruses, causing fever and specific lesions, skin nodules, rash on skin and MM.
Family: Poxviridae is divided into 2 subfamilies:
Chordopoxvirinae
Orthopoxvirus (cowpox)
Parapoxvirus (Contagious ecthyema)
Capripoxvirus (sheep and goat pox & Lumpy skin disease)
there is also: Leporipoxvirus (Myxomatosis) & Avipoxvirus (fowl pox)
Entomopoxvirinae (insects)
7.Poxviral infectious Diseases (Ruminants and others)
part 2: Sheep and goat pox
Sheep and goat pox
caused by capripoxvirus. OIE notifiable!
Transmission: Aerosols, direct contact, insects, virus present in secretions, excretions and scabs
IP is 8-13 days.
CS: Economic losses, esp. among young animals (highest mortality)
fever, conjunctivitis, rhinitis, enlarged LN, depression, anorexia, dyspnea, nasal discharge, secondary infections common
Skin lesion progression: Starts as pink-red spots in hairless areas (macules/papules), to fluid filled blisters (vesicles/pustules) that become hard, dark scabs/crusts, often leaving scars. These may spread over entire body or localize. Survivors may get necrotic scabs.
Diagnosis: CS, virus isolation - grows on tissue culture of ovine/cap/bo origin, lab confirmation of capripoxvirus by PCR method in combo with clinical history. histopathology - show incl. bodies, serology - virus neutralisation test.
Treatment&prevention: no treatment. ATB for seconary infection + good nursing care. Vaccination in endemic areas.

7.Poxviral infectious Diseases (Ruminants and others)
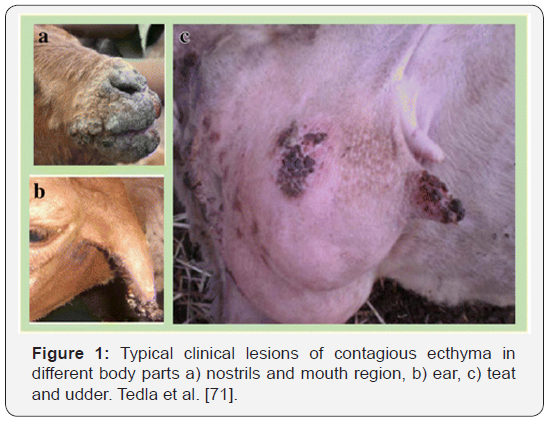
part 3: Contagious ecthyma
Contagious Ecthyma
Caused by Genus Parapoxvirus
Species: Mainly sheep and goat, humans. Zoonotic.
Transmission: direct contact through superficial skin wounds (like cracked lips on sheep), wool, objects (bucket ex.)
IP: 2-3 days
CS: painful blister/scabs on lips, mouth, muzzle, eyelids, ears, feeth and perineum (crusty/sore mouth)
can cause anorexia, starvation, lameness
secondary bacterial infections possible, lesions may go to internal organs
Can resolve spontaneously, mortality is generally low, death occur from secondary infections or failure to nurse.
Diagnosis: CS, skin samples, PCR, Electron microscopy of crust, biopsy
Treatment/prevention: supportive care, vaccine, very resistant to environment.
FMD and bluetongue infection - considered as Diff DX if high morbidity and cs incl. salivation, lameness + fever.
7.Poxviral infectious Diseases (Ruminants and others)
part 4: Cowpox
Cowpox virus (orthopoxvirus) - family Poxviridae
Species: cows, wild rodents & humans. Zoonotic.
Transmission: Direct contact with teat lesions, rarely rodents to humans transmission.
CS:
In cows: Mild fever, papules → pustules → upon breaking, forms red scabs, ulcers. Takes a month to heal.
Humans: red blisters, local edema, fever, lymphadenitis, severe and often fatal in immunosuppressed patients.
diagnosis: History + signs, PCR - from lesion swabs, skin biopsies, histology
Treatment&preventive: Supportive care, ATB for secondary infection, vaccination

7.Poxviral infectious Diseases (Ruminants and others)
part 5: Lumpy skin disease
Lumpy skin disease - Genus Capripoxvirus in cattle
Transmission: Arthropod vectors (mosquitoes, biting flies, midges, ticks), direct contact (minor source), contaminated feed/water by saliva
CS: From mild/not seen to severe
Firm skin nodules on head, neck, udder, perineum + MM
Nodules may become necrotic
spread to resp. + GI mucosa
Also: fever, enlarged LN, Depression, anorexia, fails to produce milk.
Diagnosis: skin scraping + biopsy, transmission electron microscopy, ELISA.
Treatment&prevention: no treatment, slaughter infected animals, movement control, import restriction, vector control. (stable - survives for long periods esp. in dried scabs). vaccine.

8.Prionoses, BSE and scrapie
part 1: focus on what is prionoses, Scrapie?
Prionoses - Prion = infectious proteins (no bacteria, no virus), a misfolded version of normal protein
These cause slow, fatal brain degeneration
Transmissible Spongy encephalopathies (TSEs - group).
Scrapie:
caused by abnormal prion protein (The PrPsc)
Species: Sheep (2-5 years old), spread bw. animals, carrier animals infect others for life
Transmission: Eating placenta/amniotic fluid after lambing, vertical transmission in uterus, environmental contamination
IP: very long, 1-5 years
CS: signs can vary, Behavior → itching → ataxia (generally CNS affected but also outside CNS)
Behavioral changes (stand apart, fixed stare)
Hypersensitive to stimuli
Intense itching (pruritus - due to brain damage) → fleece may be dry, brittle
Ataxia, tremors, teeth grinding, lowered head
Duration - of 3 months to a year, Mortality is 100%
Pathology: Spongiform degeneration of brain, neuronal loss, amyloid plaques (some cases)
Diagnosis: Tonsil biopsy preclinically, CS, epidemiological investigation, brainstem/spinal cord after death, histology (spongy brain), western blot, rapid test.
Treatment: no treatment, control by test & cull positives

8.Prionoses, BSE and scrapie
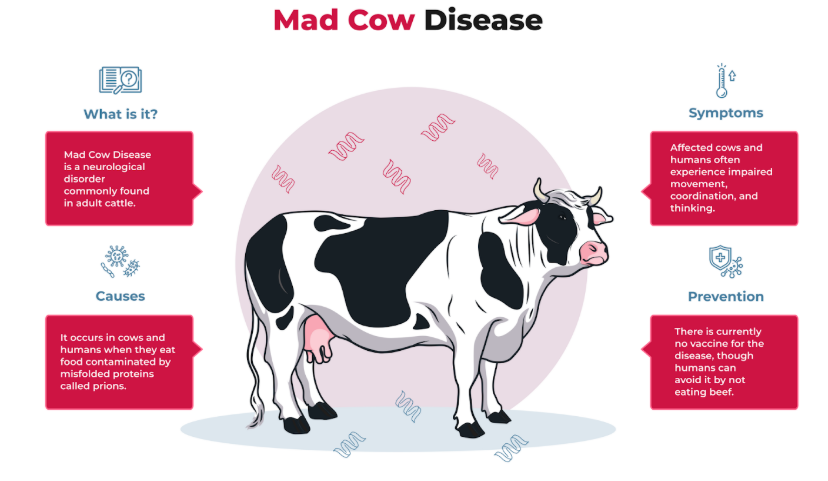
part 2: what is BSE?
BSE - bovine spongiform encephalopathy (Mad cow disease)
Caused by PrP-TSE (abnormal prion protein)
Species: cattle (3-5 years old), zoonotic → humans get variant CJD (creutzfeldt jakob)
Transmission: contaminated meat, recycling of infected carcasses in feed - animal food pellets.
IP: 2.5-8 years, largest epidemic of animal prions disease, cooking/disinfection does not destroy the agent.
CS: behavior → gait → weight loss.
mortality 100%, duration is 1-12 months
Nervousness, aggression, hyperreactivity, tremors, ataxia, lowered head, weight loss, decr. milk production.
Diagnosis: same as scrapie, histology of brain, western blot, rapid prion tests
Treatment/Prevention: No treatment, prevention by banning feed of specific offals of all species, destroy infected animals, and ensure safe recycling practices with carcasses + waste
9.Coronaviral infectious diseases (Bovine, swine, avian)
part 1: family tree, bovine and swine
Coronviruses - RNA viruses, infect resp. and GI epithelium. Affect mammals & birds.
Family: Coronaviridae with genuses:
Genus coronavirinae
Alphacoronavirus - TGE, canine coronavirus, PED (pigs), FIP-virus
Beta - Bovine corona virus (gastroenteritis, bloody diarrhea, winter dysentery resp. disease, fecal oral, no vaccine)
gamma - infectious bronchitis
delta
Genus torovirinae - diarrhea in calves, pigs, horses
Swine - Transmissible Gastroenteritis (TGE) / Swine coronavirus enteritis.
caused by: Coronavirus
Species: Pigs, esp. piglets
Transmission: Fecal-oral, virus shed massively in feces, spreads fast in poor hygiene
Survival: killed by sunlight in hours, survives long in the cold, resistant to disinfectants. Disease is in farrowing houses until sow gets immunity to protect piglets, once lactogenic immunity is no longer being taken in the pigs → infected → virus multiply → pigs shed the virus → contaminated weaner rooms.
CS:
Piglets (<7 days old) - watery diarrhea, severe dehydration, up to 100% mortality in 2-3 days, no response to ATB
Weaners & growers: vomit, diarrhea, rapid spread, recovers in ish 5 weeks
Sows: Mild vomiting, diarrhea, recover in 1 week.
Pathology: virus destroy SI epithelial cells, villus atrophy → malabsorption → diarrhea.
Diagnosis: rapid spread + watery diarrhea, FAT test (fluorescent Ab test), virus isolation
Treatment&Prevention: No specifics, supportive therapy only, colostral (lactogenic) immunity protects piglets

9.Coronaviral infectious diseases (Bovine, swine, avian)
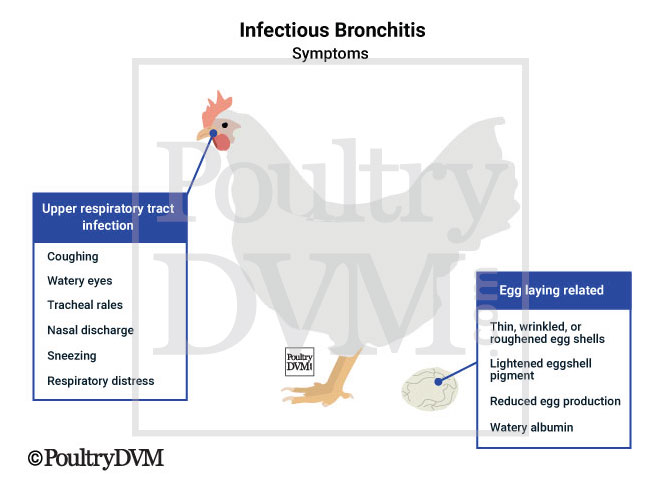
part 2: focus on avian
Infectious bronchitis in chicken
transmission: aerosol droplets, feces, contaminated equipment
CS: very short incubation (18-48h), resp. signs (sneezing, cough, tracheal rales), wet eyes, facial swelling, decr. egg production, poor egg shell quality, red. growth (all depends on severity, age, immune status of flock)
Some strains: cause kidney damage → high mortality (economic loss)
Diagnosis: cannot rely on signs alone due to the similary to mild resp. forms of other resp. agents like Newcastle disease, mycoplasma.
ELISA, HI - hemagglutination inhibition, virus isolation.
Treatment/Prevention: No treatment, although ATB may reduce mortality due to sec. infections, warmth. Vaccination.
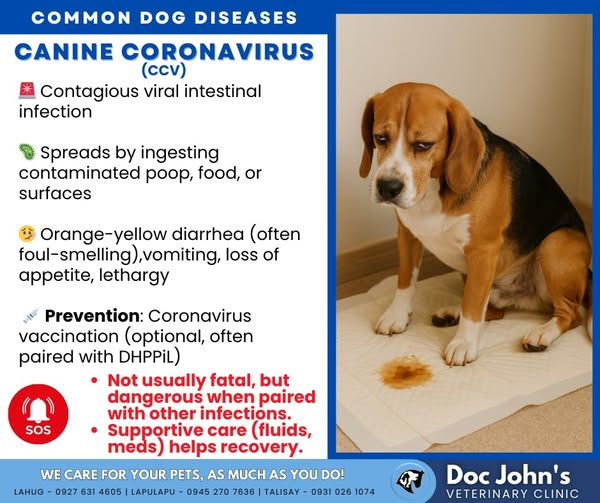
10.Coronaviral infectious diseases (canine, feline)
part 1: focus on canine
Coronaviral infection of dogs
caused by canine corona virus in all breeds, all age categories of dogs
Transmission: Fecal-oral, virus shed in feces for 2 weeks
highly contagious, high morbidity, low mortality, puppies often infected at 2-3 months → develop Ab.
CS: usually mild or inapparent, vomiting, watery diarrhea (sometimes foamy, orange, foul-smelling, can be bloody), mild fever, rare leukopenia, recovery in 1 week.
Danger: Mixed infection with CPV or bacteria like salmonella → fatal
Pathology: virus infects intestinal enterocytes, causes villus damage and malabsorption
Diagnosis: PCR/electromicroscopy on feces, hematology - rule out parvo - as it has severe neutropenia, and canine corona virus does not. Testing Ab has no value (As positive Ab does not equal currently infected)
Treatment/prevention: Supportive care, ATB for secondary infections, vaccination, Good prognosis unless mixed.
10.Coronaviral infectious diseases (canine, feline)
part 2: focus on feline
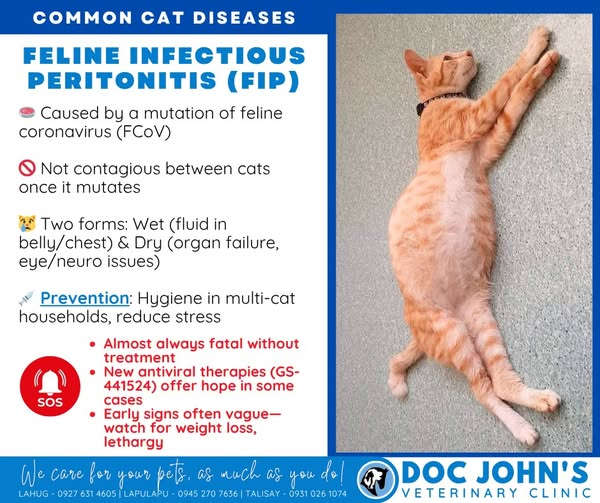
Feline coronavirus & FIP (feline infectious peritonitis)
Caused by feline coronavirus (mutation → FIP), Disease is immune mediated. in cats. (cat is first infected with feline coronavirus - usually mild, in small percentage → virus mutates inside the cat → becomes form that causes FIP)
Transmission: Oronasal, Aerosols, transplacental
Clinical forms:
Mild coronavirus - mild enteritis, mild diarrhea
FIP - Severe, fever, depression, lethargy
Dry FIP: Granulomas in organs (liver, kidney, CNS, eyes) + neurological signs (paresis, paralysis, nystagmus + behavior change)
Wet FIP: Ascites, weight loss, depression, anemia, pleural/pericardial effusion → dyspnea, jaundice, Death
Pathology: virus → tonsils + SI enterocytes, necropsy show abd. enlargement, ascites, enteritis, hepatitis, pleuritis, peritonitis, uveitis, nephritis.
Diagnosis: CS + virus detection, ELISA, IF, rivalta test on effusion: Drop persist = positive.
Treatment/Prevention: No effective treatment, only supportive care + ATB, Vaccination.
11.Rabies and other lyssavirus infection
Rabies + other lyssavirus infection - behave almost the same clinically + epidemiologically as clasical rabies.
Rabies:
Caused by: family Rhabdoviridae, genus: Lyssavirus. Has many species, but the most important is Classical Rabies virus (RABV)
RNA virus, targets nerve cells (neurons)
Species: Infect all mammals, Zoonotic, fatal. Car (fox, wolf, dogs etc.) - carry different rabies viruses, acting as reservoirs, sometimes infecting humans. Highest risk in Africa, asia, north south america.
Urban cycle → dogs
Sylvanian cycle → foxes, raccoons, wolves, coyotes. etc.
Transmission: Bite wounds (Saliva), saliva into cuts or mucosa, rarely aerosols or oral. Saliva becomes infectious before signs appear.
Incubation: few days → several years
Pathogenesis: Enters via bite → replicate in muscle → enters nerve endings via acetylcholine receptors → travels up nerves to brain → encephalitis → death
Clinical forms:
Furious (aggressive behavior) form - stages:
Prodromal (behavior change, fever, dilated pupils)
excitation stage (aggression, biting, hypersensitivity, drooling)
Paralytic (ataxia, convulsions, paralysis, death)
Dumb (paralytic) form: quiet, depressed, muscle tremors, hind limb paralysis, drooling, death
Pathology: encephalitis, Negri bodies (intracytoplasmic inclusions in neurons)
Diagnosis: Fluorescent Ab test -FAT (gold standard), PCR for viral RNA, negri bodies on histology, samples from brain, serology (response to vaccination)
Treatment/prevention: No treatment once signs appear, prevention by vaccination, control stray/reservoir populations, virus is sensitive to disinfectants, UV, extreme pH.
Differential Diagnosis: cause acute, progressive neurological disease, so many other NS issues can look similar, such as viral encephalitis (other viruses - causing inflammation of brain - herpesvirus), other viral encephalitis (west nile), poison - atropine (confusion, dilated pupils), tumors - intercranial, listeriosis (bacterial encephalitis in ru - circling, paralysis, head tilt).
12.Picornaviral infectious diseases (Foot and Mouth disease)
Footh and Mouth Disease (FMD)
caused by: FMDV - footh and mouth disease virus, genus Aphtovirus. 7 serotypes. No cross-protection bw. these, type O is most common.
Species: All domestic + wild cloven-hoofed animals
Transmission: virus is in all secretions - saliva, milk, urine, feces, semen, breath, vesicle fluid, aborted fetus.
Spread by: direct contact, aerosols, ingestion, contaminated milk, equipment, people, AI
carriers: recovered animals can carry virus in throat > 28 days, african buffaloes have long-term reservoir of SAT serotype (up to 5 years), humans can carry it in the nose for 1-2 days
epizoo: Extremely contagious, endemic in parts of Asia, africa, middle east + south america
survives: in LN + bone marrow - neutral pH, also in cold, moist environments in organic matter, in milk (during regular pasteurization), in frozen tissue.
Destroyed by acidic pH (<6), high heat (UHT)
IP: 2-14 days
General CS: fever, vesicles (blisters) → erosions on: mouth, feet, teats/udder.
Drooling, lameness, depression, anorexia - does not want to move due to pain of erosions. Adults recover in 2-3 weeks mostly.
morbidity 100%, mortality is low in adults, high in young
Specific CS based on species:
Cattle: severe mouth lesions → weight loss, drool, teeth grinding, lip smacking, foot pain/lesions at coronary band & interdigital space, decr. milk production, “hairy panter” heat intolerance after recovery.
sheep/goats: mild oral lesions, lameness can be subtle, decr. milk
pigs: severe foot lesions, claw detachment, vesicles on snout and limbs
Young animals can die from heart failure.
Pathology: “tiger heart” in young - striped myocardial necrosis, erosions on rumen pillars PM.
Diagnosis:
Differential Dx: Vesicular stomatitis, swine vesicular disease, vesicular exanthema, blue tongue, BVD
samples: vesicle, oropharyngeal fluid
Tests: ELISA (Ag), RT-PCR (viral RNA), other: virus isolation - grown then confirmed by ex. ELISA, electron microscopy, snap test, serological (prescribed test in the OIE, alternative test - complement fixation test).
Treatment/prevention: Supportive care only. Prevention by movement control, quarantine, slaughter infected and contact animals, disinfection of premises, vehicles and clothes, safe disposal of carcass, emergency vaccination during outbreaks.
13.Picornaviral infectious diseases (Swine vesicular diseases and others)
part 1: focus on swine vesicular disease
Swine vesicular disease (SVD)
caused by: swine vesicular disease virus, genus: enteroviridae, occurs in domestic pigs
Transmission: Direct contact, contaminated environment, through mucosa, skin breaks, ingestion
CS: can be subclinical, mild, or severe
Vesicles on coronary band, interdigital spaces, sometimes mouth. Vesicles rupture → erosions.
Lameness, hoof detachment, mild fever, weight loss
recovery in 2-3 weeks, but dark horizontal line on hoof may remain
Diagnosis: RT-PCR on vesicle fluid for detection of svd virus RNA. Virus isolation - slower but gold standard.
Treatment/Prevention: no treatment, no vaccine, Control by import restriction and surveillance.
13.Picornaviral infectious diseases (Swine vesicular diseases and others)
part 2: focus on other diseases
Teschen Virus
caused by: porcine teschovirus - 13 serotypes, in Pigs
some strains of serotype PTV-1 can cause CNS disease called Teschovirus Encephalomyelitis
Transmission: fecal-oral, nasal route, virus shed in feces, urine, oral fluid
IP: 1-4 weeks
CS: often without clinical signs
but some strains cause severe CNS disease
Most Typical sign is Neurological dysfunction, most notably ataxia (lack of coordination), swaying gait then progressing to paralysis (Ascending - starting with hindlimbs).
fever, anorexia, depression, teeth grinding, lip smacking, tremors, rigid/stiffness, nystagmus, seizure, opisthotonos
Diagnosis: Sample from brain, RT-PCR, ELISA, complement fixation.
Treatment: supportive only, vaccination.
Duck hepatitis virus
caused by: duck hepatitis virus type 1 in ducklings less than 6 weeks, highly contagious
Transmission: horizontal - bird to bird, by direct contact of fecal-oral.
IP: 18-48h
CS: lethargy, loss of balance
young ducks show spastic paddling + opisthotonus (arched-back posture) immediately before death, which can be within minutes.
Older ducks can be infected, but no signs.
Pathology: enlarged liver with hemorrhage, enlarged spleen + kidney
Diagnosis: virus isolation, PCR
Treatment/prevention: Vaccination & biosecurity controls
14.Retroviral infectious diseases (Enzootic bovine Leucosis, avian leukosis)
part 1: Enzootic bovine leucosis
Retroviruses - RNA → DNA → Tumors
Family: Retroviridae
integrate into host DNA, large group of malignant tumor diseases, like leukemias, lymphomas, sarcomas, Autoimmune diseases
Enzootic bovine Leukosis:
caused by: Bovine Leukemia virus (BLV) in cattle
transmission: Mainly through infected blood, needles, dehorning tools/surgical tools, rectal gloves, AI, contaminated milk, possibly insects.
BLV - occurrence depend on countries, some still have infected animals, others not due to eradication programs.
Outcome: either asymptomatic carrier, persistent lymphocytosis in some, lymphosarcoma in older cows.
CS - most are subclinical, but some develop lymphosarcoma, 3 main forms:
Juvenile form (in young - < 6months): fever, weight loss, enlarged LN, dyspnea, bloat, posterior paresis
Thymic form (6-24months): inv. thymus, cervical mass, dyspnea, bloat, jugular distention
Cutaneous form (1-3yrs old): skin plaques (neck, rump, thighs), may regress then relapse
Lesions - tumors can occur almost everywhere in body, ex. spinal cord → paralysis
Diagnosis: ELISA to detect anti-BLV Ab in blood or milk, cytology/Histology - tumors.
No treatment, prevention by avoiding blood transfer
14.Retroviral infectious diseases (Enzootic bovine Leucosis, avian leukosis)
part 2: avian leukosis
Avian leukosis
caused by Avian leukosis virus (subgroups A to D, J), in chickens
Transmission: Vertical (egg) or horizontal (contact).
Congenital infection → lifelong viremia (fail to make neutralizing Ab) → more tumors.
strict sanitation = reduces transmission
Mortality is high
CS: weak, diarrhea, weight loss, enlarged bursa (palpate), tumors in liver, spleen, bursa. Virus → damage WBC → lead to sec. infections.
Diagnosis: Necropsy (tumors), PCR, Serology
Diff. dx: imp. to differentiate from Marek`s disease! (both cause tumors, but marek cause also nerve involvement - paralysis for ex. + does not have bursa involved as avian leukosis does)
No treatment, imp. to control by sanitation, remove infected
15.Retroviral infectious diseases in cats
Feline Leukemia (FeLV)
caused by Feline leukemia virus (FeLV). 4 subgroups, all start as FeLV-A.
FeLV-A (original form, immunosuppression)
FeLV-B (tumors)
FeLV-C (severe anemia)
FeLV-T (Ly depletion)
species: Cats, young kittens most susceptible
Very common cause of morbidity + mortality in cats, virus dos not survive for long outside host, readily destroyed by disinfectants, soap, heat, drying
Transmission: carriers shed virus in saliva, but also feces, nasal, milk, by infected cats, mainly through friendly contact such as grooming. Biting, blood transfusion
CS: Usually starts in oropharynx → bone marrow infection → viremia.
Most common is non-regenerative anemia, immunosuppression → sec. infections, Lymphoma (mediastinal, peripheral, spinal)
others: Reprod. failure, neurological signs (vocalization, paralysis), eye inflammation (uveitis), other tumors, lymphoma at GI, renal etc.
Pathology: Virus → invade various cells of immune system + blood-forming tissues → cell death or mutation → possible cancer, but may take time (months-years)
Diagnosis: FeLV p27 Ag (snap test), PCR for provirus, IFA (immunofluorescent Ab test)
Treatment&prevention: no cure, supportive care, treat infections, vaccination available.
Feline Immunodeficiency - FIV
caused by: feline immunodeficiency virus, in mostly adult male outdoor cats
Transmission: bite wounds, vertical may occur
FIV looses infectivity quickly outside host, susceptible to disinfectants, soap
CS:
long asymptomatic phase (years), some cats never develop disease
signs due to immune failure: chronic stomatitis, skin and resp. infections, weight loss, anemia, neurological signs
cats remain infected for life
diagnosis: ELISA, Western blot for confirmation
treatment/prevention: No vaccine available, only supportive.
16.Retroviral infectious diseases (Equine, ovine)
part 1: focus on ovine
Retroviruses
Maedi-Visna (Sheep Lentivirus)
Caused by: Maedi-visna virus (MVV), genus Lentivirus, infect host for life
species: sheep mainly, sometimes goats
Transmission: colostrum, milk + close contact
IP: very long, 3-4 years - so infected early, but not seen before 2 years of age
Clinical forms: most are subclinical, some develops progressive, untreatable disease syndroms like:
Maedi form (lungs): dyspnea, fatal
Visna form (CNS): hindlimb weakness, ataxia, head tilt, tremors, paresis → paralysis
Other: mastitis, arthritis
Diagnosis: ELISA - for Ab against MVV in blood, AGID (agar gel immunodiffusion) - clinical suspicion in older wasting sheep → 2 years old, slow progressive resp. distress, neurological, mastitis, or arthritis
Treatment/Prevention: no treatment, test, quarantine, cull
16.Retroviral infectious diseases (Equine, ovine)
part 2: focus on equine
Equine infectious anemia
by: retroviral infectious anemia virus - genus Lentivirus in horse.
Transmission: biting insects (horse flies) - remain in blood leukocytes for life, contaminated needles (iatrogenic)
IP: 1w - 45 days
CS: fever, anemia, edema, weight loss, weak, depression, often inapparent (mild - not seen). All infected horses become lifelong carriers. CS - often non-specific.
Diagnosis: Coggins test -AGID, immunodiffusion, ELISA - positives confirmed by coggin
Horses are usually sero-neg. in the first 2-3 weeks, can be longer. Thus coggin may remain negative - as Ab has not reached detectable levels.
Treatment/prevention: no vaccine/treatment, Prevention by control programs.
17.Herpesviral infectious diseases (infectious bovine rhinotracheitis/pustular vulvovaginitis, caprine herpesvirus, equine herpesvirus)
Part 1: Focus infectious bovine rhinotracheitis/pustular vulvovaginitis
Herpesvirus - family herpesviridae, subfam. alphaherpesvirinae, key: lifelong latency + reactivation.
Infectious bovine Rhinotracheitis (IBR) / Pustular vulvovaginitis
Caused by: BoHV-1 (resp. + reproductive) & BoHV-4 (reproductive)
species: Cattle mainly
Transmission: horizontal - sexual contact & AI, aerosols, + vertical - transplacental.
IP: 2-20 days
CS: not life-threatening, but can lead to secondary infections → death
Respiratory: fever (42 degrees), “red nose” (hyperemic necrotic nasal mucosa), cough, nasal discharge, dyspnea
Reproductive: Pustular vulvovaginitis, ulcers, edema, hyperemia, abortion - mummification
Systemic (calves): fever, diarrhea, convulsions, resp. distress
CNS, GIT - epithelial necrosis, loss of cilia, n.trigeminus → trigger CNS inflammation.
diagnosis: PCR in nasal/genital swabs, virus isolation
Treatment/Prevention: vaccination
17.Herpesviral infectious diseases (infectious bovine rhinotracheitis/pustular vulvovaginitis, caprine herpesvirus, equine herpesvirus)
Part 2: focus on caprine and equine herpesvirus
Caprine herpesvirus
caused by CpHV-1, CpHV-2 in goats
Transmission: nasal or genital routes
CS:
Kids (1-2w): affect digestive tract, often fatal
Adults: mild resp. signs, vaginitis, balanoposthitis, possible abortion
Diagnosis: PCR, VNT, histology of aborted fetus (intranuclear inclusions)
Prevention: no specific vaccine
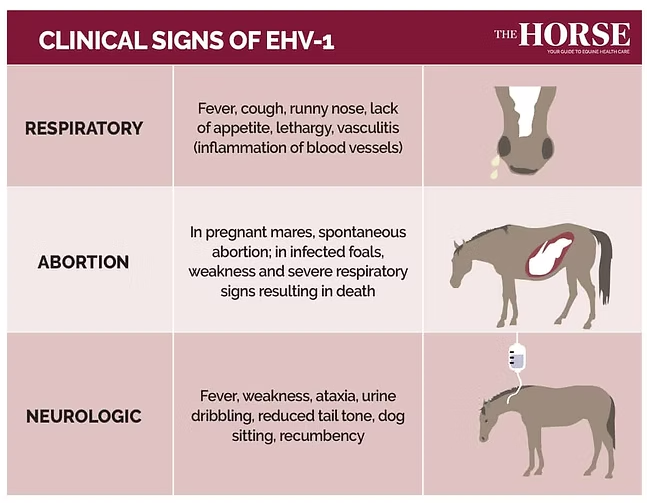
Equine herpesvirus (EHV)
Caused by: EHV-1, EHV-4 in horses
Transmission: aerosols
CS:
Respiratory: fever, nasal discharge, depression, lethargy, not eating
Abortions & Neurological (EHV-1): equine herpes myeloencephalopathy - can be fatal
horse under 3 yrs - sudden-onset, mainly fever + resp. signs
Pathology - infect + multiply in epithelial cells of resp. mucosa
Diagnosis: PCR nasal swab or whole blood
Treatment/prevention: no specific treatment, supportive. vaccination, isolation, hygiene
18.Herpesviral infectious diseases, Aujeszky disease
Aujeszky Disease (Pseudorabies - cause rabies-like signs like aggression, paralysis and death, does not infect humans)
Caused by: Porcine herpesvirus-1 (PHV-1). Belongs to subfam. alphaherpesvirinae, more resistant to temp. + pH than other herpesvirus.
species: Pigs (natural reservoir), while ru, dogs and cats are dead-end-host (fatal CNS disease, no shedding - cannot spread it any further!)
Transmission: pigs - respiratory, oral or transplacental
ruminants - through skin wounds, and dogs/cats get it from eating raw contaminated pork.
virus survives 2-7 weeks in environment, in muscle for 11-36 days.
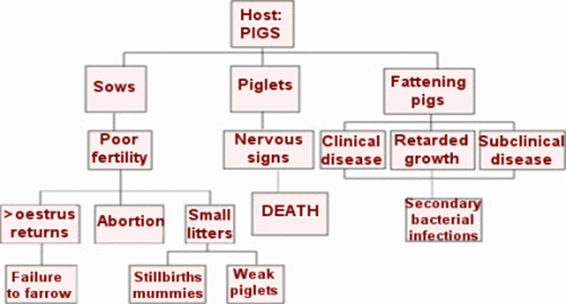
CS: Most typical in pigs, is resp. signs, abortion, high mortality in piglets, + severe NS in piglets.
Persistent + latent infection in pigs, CS vary with AGE:
Newborn: fever, tremors, incoordination, limb paralysis (100% mortality)
3-4 weeks: NS, hoarse voice - pharynx lesion (50-70% mortality)
4w-3 months: resp. + CNS signs, can be complicated with sec. bacterial infections (5-30%)
Adults: fever, resp signs → pneumonia (low mortality)
Pregnant sows: abortion, stillbirth, weak piglets
In non-pig species, most typical sign is intense Pruritus/ITCHING → self-mutilation. “MAD ITCH” + NS.
Ruminants: Anxiety, fever, ataxia, severe local pruritus at entry site, self-mutilation, death in 1-2 days
dogs&cats: Sudden onset, behavior change, aggression, dyspnea, hypersalivation, vomit, diarrhea, paralysis of muscle + rabid behavior, severe itching of head/neck/shoulder, erythema, ulcer, death within 48h
Diagnosis: lab - virus isolation + ID, sample from brain (animal with NS), swabs from tonsils, immunofluorescence, virus neutralization, serology - acc. to OIE, ELISA
Treatment/Prevention: Notifiable disease
vaccination only in enzootic areas (with special permission of state vet - this is because it may interfere with surveillance, trade status and eradication programs, in disease-free regions, vaccination may actually make control harder - as vaccination → hides infection (develop Ab cannot tell if it is from infection or vaccination), and it may not always fix the issue)
test + cull positives, Disinfection (phenol, NaOH)
19.Herpesviral infectious diseases (canine, feline, avian)
part 1: focus on canine
Canine herpesvirus
caused by: CHV-1 in domestic and wild canidae-dogs, esp. puppies (< 2-3 weeks)
Transmission: Direct contact, body fluids/contamianted surfaces, resp. secretions (cough) and vertical (transplacental)
CS:
Puppies: Hypotherma, crying, abd. pain, diarrhea (gray-yellow-green), weight loss, nasal discharge, seizures, sudden death
Most important fatal hemorrhagic disease in puppies less than 2-3 weeks old. Virus cause immunosuppression.
Adults: usually asymptomatic, mild resp. signs, can cause abortions
Pathology: Necropsy - gross change in kidney, random acute necrosis of other organs
Diagnosis: CS, PM examination of puppies, PCR
Treatment/Prevention: No treatment, Isolate pregnant dogs the last weeks of gestation
19.Herpesviral infectious diseases (canine, feline, avian)
part 2: focus on feline
Feline Rhinotracheitis
caused by: FHV-1, feline herpes, in cats
Transmission: Close contact - discharge, sneeze, aerosols, fomites. Very contagious
CS: Cause resp. infection, can be serious - esp. in kennels. Latent infection in adults - CS occur during immunosuppression.
conjunctivitis, sneezing, nasal discharge, ocular ulcers, fever, lethargy, inappatence
can become reinfected, will be carriers for life.
Diagnosis: CS, PCR
Treatment/Prevention: supportive care, hygiene + vaccination (core)
19.Herpesviral infectious diseases (canine, feline, avian)
part 3: Focus on avian
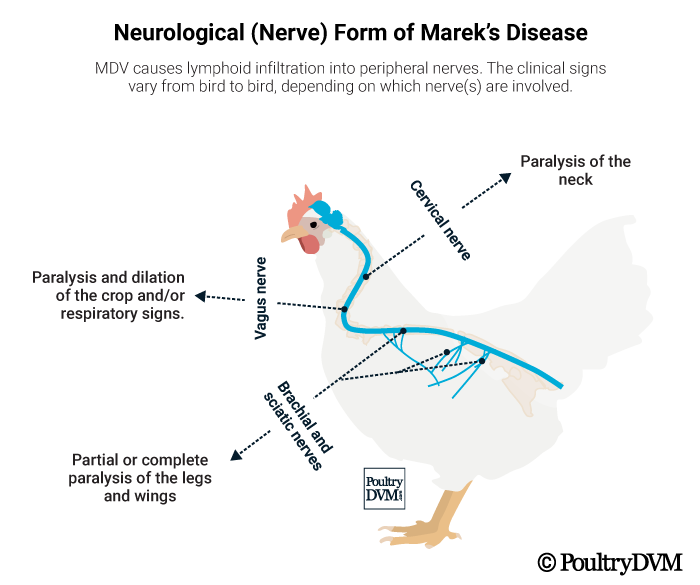
Marek`s Disease:
caused by Gallid Alphaherpesvirus 2, in Poultry
Transmission: Inhalation of infected dust, virus shed from feather follicles, Very contagious
CS: T-Cell Lymphomas + peripheral nerve enlargement (most typical)
Lymphoid tumors, paralysis, grey eye (blindness), death
Acute: depression, paralysis + death
Pathology: PM - enlarged nerves, Lymphoid tumors in various organs, lesions at feather follicles
Diagnosis: Gross Necropsy + histopathology, History + CS
Treatment/Prevention: No treatment. Vaccination.
20.Pestiviral infectious diseases, bovine viral diarrhea
Bovine viral diarrhea:
caused by: BVD virus (BVDV-1 & BVDV-2)
Genus Pestivirus (Flaviviridae - fam.)
Species: cattle, all ages
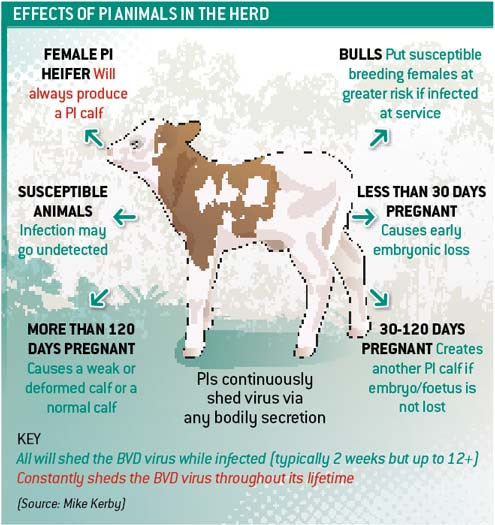
Transmission: Persistently infected (PI) animals = main reservoir. Virus shed in saliva, urine, feces, milk, semen. Direct contact, nose-to-nose, vertical (Transplacental)
Epidemiology: endemic worldwide, maintained by PI animals, highly immunosuppressive
CS: Infection results in a wide variety of CS due to its immunosuppresive effects. Has direct effect on respiratory + fertility, can also lead to persistently infected fetus
Acute form: Fever, depression, diarrhea, dyspnea, decr. milk, thrombocytopenia, lymphopenia
Intrauterine infection: abortions, stillbirth, congenital abnormalities (growth retardation, skeletal, CNS issues)
Infection during gestation outcome depends on gestational age: early (embryo death), mid (congenital defects), later pregnancy (PI calf)
Persistent infection: infected early in utero, infected before immune system is developed → does not recognize virus as foreign → no Ab → carriers + sheds virus for life, often appear normal or stunted (growth retardation), high risk of sec. diseases (mucosal disease later)
Mucosal disease: Profuse diarrhea, weight loss, anorexia, abd. pain, mouth erosions, hypersalivation + lacrimation - most typical signs in this form!, rapid + fatal.
Pathogenesis: Direct contact, aerosol → primary infection of upper resp. system → virus infect leukocytes → viremia, Leukopenia → immunosuppression → secondary infections common
Diagnosis: PCR - for viral RNA in blood, serum or nasal swabs virus isolation - reference method, IF, PI animals are seronegative
Treatment/prevention: no treatment, Vaccination, test and remove positive animals, good biosecurity
21.Classical Swine Fever & African Swine fever
Hog Cholera - Classical Swine fever & African Swine fever
Caused by:
CSF - Genus Pestivirus, fam. Flaviviridae - RNA virus
ASF - Genus Asfivirus, fam. Asfaviridae - DNA virus
Species: Domestic pigs & Wild boards (natural reservoirs) + Warthogs
All age groups are equally susceptible
Transmission: direct contact, fomites (vehicles, clothes), eating garbage with infected meat, wild boar reservoir
Transplacental - only in CSF
Ticks - only in ASF
Virus remain in blood, tissues, secretion + excretions of sick and dead animals.
Recovered animals - chronic infected, acting as carriers
CS - Indistinguishable in the field - both are very similar!
Peracute: Sudden death, few lesions
Acute: often affects whole herd
Fever, depression, loss of appetite, weak, recumbency,
NS: Ataxia, paresis, convulsions
watery diarrhea/constipation,
can vomit bile, resp. distress,
can develop skin hemorrhages (ears, abdomen, inner thighs), or cyanotic discoloration of legs, ears, tail.
abortion
mortality up to 100% - within 3 weeks
Chronic: non-specific CS, weight loss, fever, skin ulcers, arthritis, resp. disease
Pathology: Widespread hemorrhages, swollen LN, “button ulcers” in colon (CSF)
Diagnosis: RT-PCR + PCR, virus isolation in cell culture, Immunofluorescence, neutralization test
samples: tonsils, LN, spleen, kidneys, blood
Treatment: No treatment for either
Prevention/control by:
Vaccine only in CSF
outbreaks → slaughter all affected, disinfection, disposal, surveillance, epidemiological investigation
tick control in ASF
Environmental resistance: Survives months in chilled meat, years in frozen meat, killed by cooking, inactivated by chlorine disinfectants, sensitive to UV and Drying

22.Reoviral Infectious diseases (Bluetongue)
Bluetongue virus (BTV)
Fam: Reoviridae, Genus: Orbivirus. Segmented RNA virus
Species: Sheep (most severely affected), Goat, cattle, buffalo and deer (rest is mild/inapparent affected).
Transmission: Biological vector: (Culicoides) biting midges, mechanical via needles, equipment, virus in blood, semen
Vector-borne → seasonal, climate, dependent. No persistent infection in ru. Morbiditiy in sheep up to 100%, mortality is 30-70% (up to 90 in deer)
IP: 5-10 days
CS: mainly sheep, signs can be asymptomatic, mild or severely ill.
fever, depression
nasal discharge (serous → mucopurulent, crusting)
Hyperemic muzzle, oral mucosa
Facial edema (muzzle, lips, eyelids)
swollen tongue → cyanotic (“blue”)
Oral ulcers → drooling, lameness, dyspnea + pulmonary edema → death
Abortion
Cattle: Often asymptomatic, but viremic for long periods (virus present in the blood)
Pathogenesis: Replicates in LN → vascular endothelial damage→ edema, hemorrhage. Viremia - sheep up to 2 weeks, cattle up to 3 months
Diagnosis:
samples: blood in heparin (alive), spleen, liver and LN (dead animals), keep at 4 degrees, do not freeze (damages the virus)
tests: RT-PCR, Virus isolation, immunofluorescence, Serology
Treatment: No
Prevention: Emergency vaccination, vector control, movement restriction, surveillance
Resistance: inactivated by heat, sensitive to pH <6 or >8, very stable in protein (can survive in blood for years)
MANY DIFF DX: FMD, malignant catarrhal fever, Bovine virus diarrhea, Sheep pox….

23.Reoviral infectious diseases (African Horse Sickness)
African Horse sickness virus (AHSV)
Fam: Reoviridae, genus: Orbivirus (Same as Bluetongue)
Species: Horses, donkeys, mules
Transmission: Biological-vector: Culicoides (mosquito), not contagious by contact.
Epidemiology: Endemic in tropical areas of Africa, Seasonal (vector dependent)
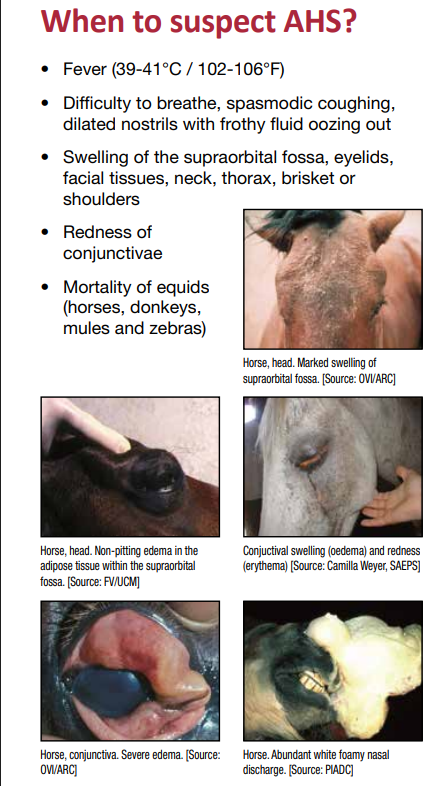
IP: 5-7 days
Clinical forms:
Peracute pulmonary form: fever, dyspnea, pulmonary edema → death, frothy nasal discharge, death within hours, fatal (95%). Seen in unvaccinated horses, foals without colostral immunity
Subacute cardiac form: Fever, subcutaneous edema, swollen head and supraorbital fossae, petectiae on MM (= poor prognosis), fatal (50%)
Mixed form: combo of pulmonary and cardiac signs
Mild/horse sickness fever: low fever, mild signs (usually in zebras, donkeys)
Pathogenesis: Virus from culicoides transmission → virus replicate in LN → widespread viremia, affecting endothelial cells in organs → vascular damage → edema, hemorrhage
Diagnosis: RT-PCR, Serology, CS
Treatment: no treatment, supportive care only
Prevention: Vaccination, vector-control, movement restrictions
in suspicion of AHS - contact vet services, prevent spread by spread midges repellent, keep animals inside, protect buildings with mesh/net, avoid any stress, do not transport animals to other plces,
24.Bunyaviral infectious diseases
Part 1: family tree, general + mention diseases
Bunyavirual disease - Arboviruses
Arboviruses = insects-borne viruses
Birds = often source of infection for mosquitoes → spreads to horses, other animals + people
Family: Bunyaviridae (now often called bunyavirales) - with genuses:
Orthobunyavirus - with virus:
California encephalitis (mosquito)
La Crosse encephalitis (mosquito)
Phlebovirus - with virus:
Rift Valley fever (mosquito)
Orthonairovirus - with virus:
Crimean-Congo hemorrhagic fever (tick)
Diagnosis: PCR, ELISA, Virus isolation
Prevention: Vector control, insecticides
24.Bunyaviral infectious diseases
part 2: Distinguish the diseases
All are zoonotic, can be spread to humans.
California Encephalitis virus (CEV)
Reservoir: Small mammals (squirrels, rodents)
Vector: Mosquitoes (aedes)
Animals are usually asymptomatic, mild neurological signs occassionally.
Humans: Encephalitis (brain inflammation) can be mild to severe
La Crosse Encephalitis virus (USA)
Species: small mammals (chipmunk/squirrel)
vector: Mosquitoes (Aedes)
Animals are asymptomatic, rare encephalitis
Humans: encephalitis, most cases are mild (<1% fatal)
Rift Valley fever
Species: Livestock (cattle, sheep, goats) & camels
Vector: Mosquitoes (Aedes & Culex)
Animals: severe livestock disease, abortions, high young mortality
humans: can get severe fever, hemorrhagic & encephalitis forms rare
Crimean Congo Hemorrhagic fever (CCHF)
species: wild + domestic animals (many mammals)
Vector: Tick (Hyalomma)
Animals: generally asymptomatic in livestock, can get fever, inappatence
Dogs: generally asymptomatic/non-specific or petechia (rare)
Humans: severe hemorrhagic fever, high fatality (up to 40%) - high fever, red eyes, red spots on mouth roof, severe bruising, severe nosebleeds, uncontrolled bleeding at injection sites can develop.
25.Flaviviral infectious diseases
part 1: general, name diseases
Flaviviral diseases
Fam: Flaviviridae, genus: Flavivirus
Vector-borne (mosquitoes, ticks)
Zoonotic (can infect humans) - humans often have no or mild disease, but severe CNS or systemic disease can occur.
No specific antiviral treatment → mainly supportive care
Prevention = vector control and vaccination (where available)
Diseases:
Dengue virus - dengue fever (mosquito)
Japanese encephalitis virus (mosquito)
West nile virus (mosquito)
Tick-borne encephalitis virus
25.Flaviviral infectious diseases
part 2: Dengue virus, Japanese encephalitis virus
Dengue virus - Dengue fever - febrile systemic disease
Host: humans
Vector: Aedes mosquito + transplacental (rarely)
CS: Muscle & Joint pain → break-bone fever.
Non-specific signs, like fever, headache, nausea, vomiting
treatment: supportive, vaccine in endemic areas
Japanese encephalitis virus - “severe viral encephalitis”
Species: Humans, pigs
Vector: Culex mosquito
CS:
Humans: most infections are asymptomatic or very mild
Severe cases → acute viral encephalitis → permanent neurological damage, high mortality, seizures, paralysis
Pigs: Abortion, stillbirth, congenital malformations, piglets → neurological signs and death.
Treatment: Supportive only, vaccination of pigs in endemic areas, vector control, isolation.
25.Flaviviral infectious diseases
part 3: West-nile, tick-brone encephalitis virus
West-Nile virus
species: Wild bird reservoir, horse + human (dead-end hosts)
Vector: culex mosquito
causes large outbreaks, big impact on eq, important zoonotic threat!
CS:
birds: often asymptomatic, may develop NS, death
Horse: fever, ataxia, weak, paralysis, seizures
Humans: flu-like signs
Pathology: Birds get hemorrhage, encephalitis necrosis, horse - encephalomyelitis + neural degeneration
Diagnosis: lgM detection serum or CSF
treatment: No treatment, vaccination for horse in endemic areas
Tick-borne encephalitis virus
Species: wild rodents reservoir,
Accidental: Humans, domestic animals
Vector: ixodes tick, unpasteurized dairy products
CS:
Dogs/Horse: Fever, lethargy, Ataxia & tremors
Humans: often asymptomatic, non-specific signs, CNS signs (meningitis)
diagnosis: Serology with CSF, ELISA
treatment: No treatment, vaccine for humans, not for livestock/pets
26.Togaviral infectious diseases
part 1: focus on general, species, diagnosis, treatment.
Togaviral diseases:
Fam: Togaviridae, genus: Alphavirus
species: Horse (main clinical disease), human (zoonotic), mammals, reptiles, amphibians
birds = reservoir, eq + humans = dead-end host
Transmission: vector-borne (culicoides, aedes, culex mosquito)
Diagnosis: Bloodwork, ELISA, PCR with CSF
treatment/prevention: Supportive care, vaccinate horse (No vaccine in venezuelan), vector-control
Conditions:
venezualan equine encephalitis virus
eastern equine encephalitis virus
Westerrn equine encephalitis virus
26.Togaviral infectious diseases
part 2: diseases, venezuelan, eastern + western
All: depression, fever, CNS signs (severity varies), ataxia, high-public health importance (zoonotic).
Eastern equine encephalitis virus (EEE) - The MOST severe! “sleeping sickness”
Fatal, Inflammation/swelling of brain, rapid onset of severe CNS signs
Ataxia, Head pressing/circling, irregular gait, seizures, rapid progression to death.
highest mortality of all three
Bird → mosquito → horse/human (classic cycle) - eastern & southern USA, central/south america.
Venezuelan equine encephalitis (VEE) - The most INFECTIOUS!
high viremia, CNS signs: ataxia, paralysis and seizures
Mortality can be very high (up to 90%) but more variable, as some subtypes can be mild.
can cause explosive outbreaks
Rodent → mosquito → horse → human (does not rely primarily on birds)
central and south america
Western Equine encephalitis (WEE) - the MILDEST!
Lower mortality
Moderate fever, CNS signs: tremors, incoordination, ataxia, convulsions, paralysis (Less severe)
Bird → mosquito → horse/human (like EEE)
Still standing horse, less severe, slower progression.
western north and south america